1. What is the difference between Autoimmunity and Autoimmune Disease?
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
What is the difference between Autoimmunity and Autoimmune Disease?
Autoimmunity: An immune response against a "self" antigen (can occur without disease).
Autoimmune Disease: Clinical tissue damage or disturbed function resulting from that response.
What is "Immunological Tolerance"?
The state where the immune system is non-reactive to self-antigens. Disease occurs when this tolerance breaks down.
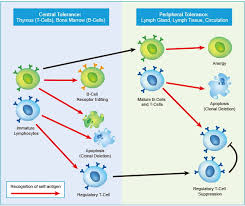
What are Central and Peripheral Tolerance?
Central: Deletion of self-reactive T and B cells during development in the thymus/bone marrow.
Peripheral: Back-up mechanisms (like T-reg cells or Anergy) that silence self-reactive cells that escaped the thymus.
What is the significance of the HLA-B27 allele?
It is strongly associated with Ankylosing Spondylitis. People with this gene are much more likely to develop the disease, showing the genetic link to autoimmunity.
What is "Molecular Mimicry"?
When an infectious agent (virus/bacteria) has antigens that look like "self" proteins, the immune system attacks the infection, then mistakenly attacks the body (e.g., Rheumatic fever after Strep throat).
What are the four mechanisms of tissue damage in Autoimmunity?
Type II: Antibodies against cell surfaces (e.g., Haemolytic anaemia).
Type III: Immune complex deposition (e.g., SLE).
Type IV: T-cell mediated destruction (e.g., Type 1 Diabetes).
Inhibition/Stimulation: Antibodies block or trigger receptors (e.g., Graves’ Disease).
What is Systemic Lupus Erythematosus (SLE)?
A systemic autoimmune disease characterized by Anti-Nuclear Antibodies (ANA). It affects multiple organs including skin, joints, and kidneys.
What is the "Butterfly Rash
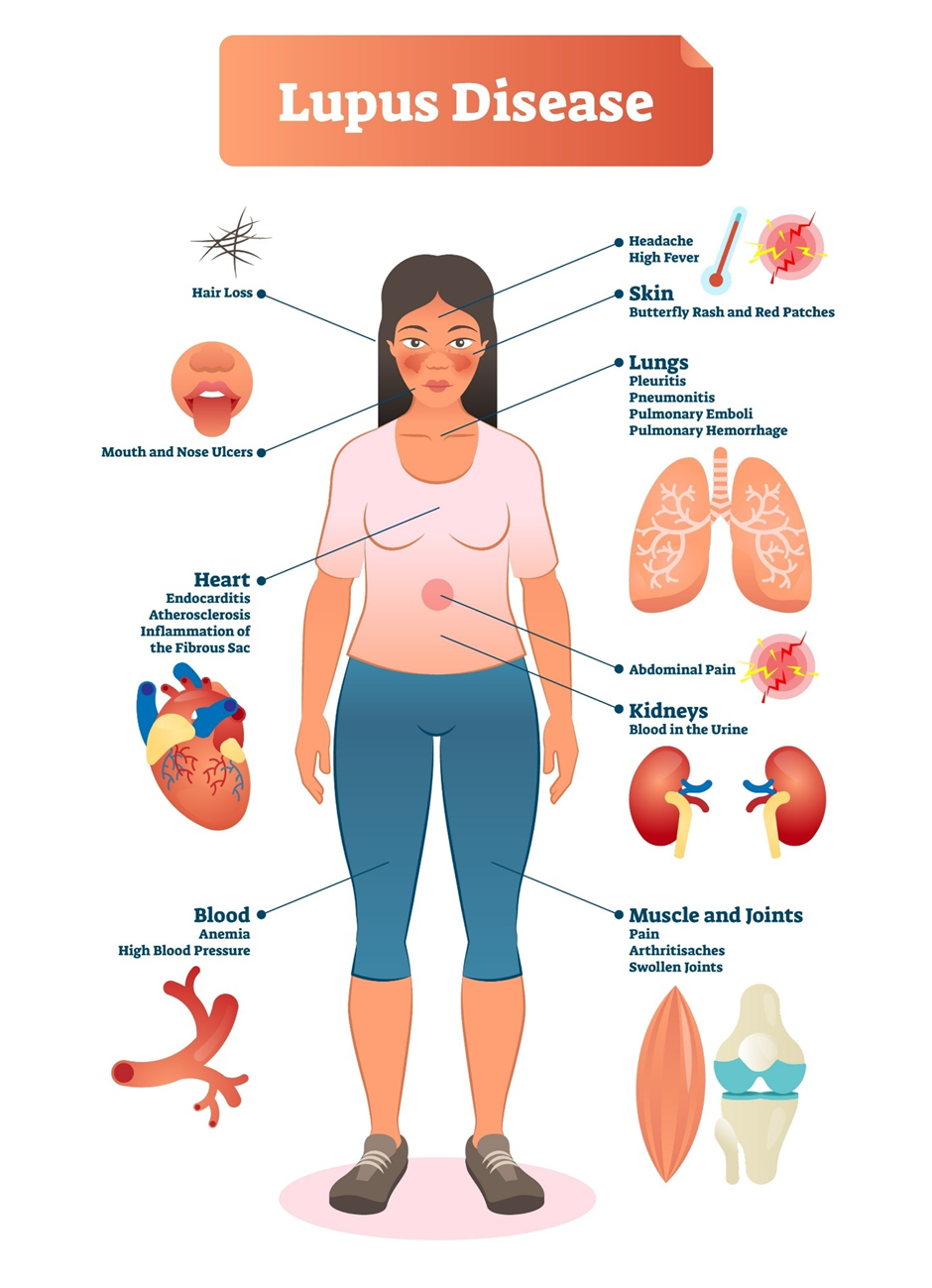
A classic clinical sign of SLE: a malar rash across the cheeks and bridge of the nose, often worsened by sunlight (photosensitivity).
What is the role of Immune Complexes (Type III) in SLE?
DNA and anti-DNA antibodies form complexes that become trapped in small blood vessels, triggering the complement system and causing inflammation in the kidneys (Glomerulonephritis) and joints.
How is SLE diagnosed in the lab?
High titers of ANA (Screening) and more specifically Anti-dsDNA or Anti-Smith (Sm) antibodies. Low Complement levels (C3, C4) indicate active disease.
What is Multiple Sclerosis (MS)?
A chronic autoimmune disease of the Central Nervous System, where the immune system attacks the Myelin Sheath of nerve fibres.
Which cells drive the damage in Multiple Sclerosis?
Primarily TH1 and TH17 cells which cross the blood-brain barrier and release cytokines (IFN-$\gamma$, TNF) that activate macrophages to destroy myelin.
What is the "Inflammatory Phase" of MS?
T-cells and B-cells (plasma cells) enter the brain; B-cells produce myelin-specific antibodies that trigger the Membrane Attack Complex (MAC) to damage nerve cells.
What is the suspected link between EBV and MS?
The Epstein-Barr Virus (EBV) is a prime candidate for triggering MS, possibly by altering immunoregulatory pathways years before symptoms start.
What is "Epitope Spreading"?
As the immune system damages tissue, it "sees" new self-antigens it didn't see before, leading to a broader and more aggressive immune response over time.
How are autoimmune diseases generally treated?
Immunosuppression: Steroids, Ciclosporin, or Biologicals (like Anti-TNF) to dampen the immune response. Plasmapheresis can be used to physically remove harmful antibodies.