3. small animal med- diseases of the oropharynx
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
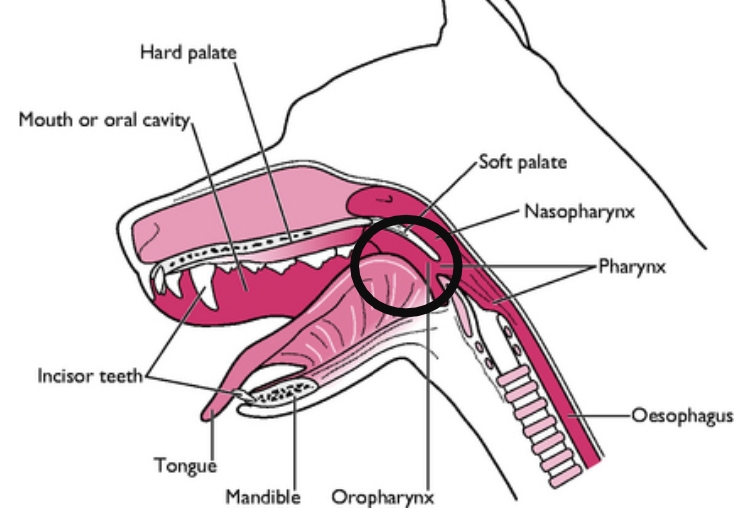
where is the oropharynx located?
caudal portion of oral cavity
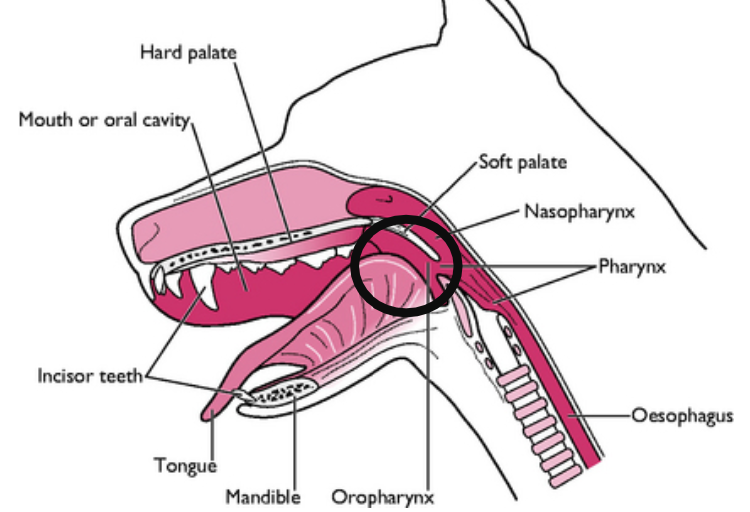
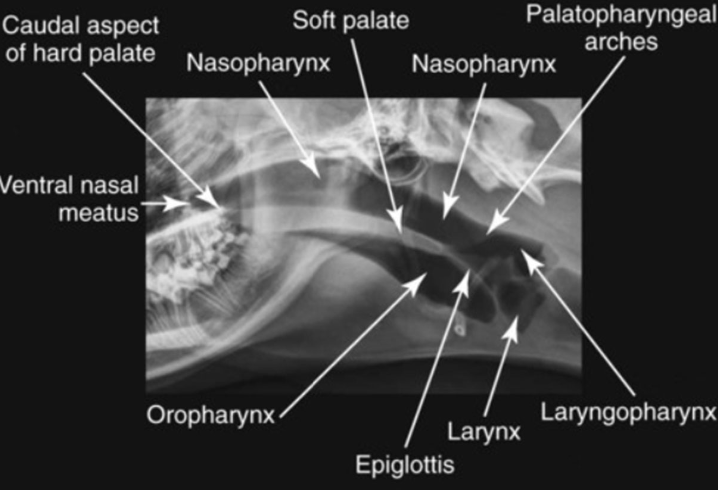
what is the oropharynx bound by?
-soft palate (dorsal)
-root of tongue (ventral)
-tonsillar fossae (lateral)
what is the main clinical sign of disease in the oropharynx?
rergurgitation, vomiting, diarrhea, or dysphagia
dysphagia
what is dysphagia?
difficulty swallowing
occurs with disease of oropharynx or esophagus
what are differentials of dysphagia?
1. functional: secondary to neurological disease or muscular disturbance (neuromuscular dz)
2. structural: stricture, traumatic injury, foreign bodies, neoplasia
if an animal cannot keep down liquids, suspect ___ disease.
functional
if an animal cannot keep down solids, suspect ___ disease.
structural
what are the 2 classifications of dysphagia?
1. oropharyngeal dysphagia
2. esophageal dysphagia
what is oropharyngeal dysphagia?
difficulty with prehension and abnormal transport through the upper esophageal sphincter
what is esophageal dysphagia?
abnormal transport of bolus through the esophagus and lower esophageal sphincter into the stomach
what history questions should you ask owners for animals presenting with dysphagia?
-age of onset (congenital or acquired)
-frequency of signs
-duration of signs
-temporal pattern
-difficulty with solids vs liquids
-recent doxy/clind or anesthesia (esophageal stricture)
-weakness/painful or stiff gait/exercise intolerance (polymyositis)
If dysphagia is within seconds after eating it is likely ___.
oropharyngeal
If dysphagia is within seconds to HOURS after eating it is likely ___.
esophageal
what should be included in your PE in patients with dysphagia?
-palpation of pharynx and neck (masses, asymmetry, pain)
-thoracic auscultation (aspiration pneumonia?)
-look for muscle atrophy, especially around head
-full neuro exam
-sedated laryngeal exam with doxapram (respiratory stimulant)
-sedated oral exam
-watch pet eat food/liquid
what diagnostic imaging can be done for dysphagia?
1. head, cervical, chest rads
2. contrast radiography
3. barium contrast videofluoroscopy
4. endoscopy
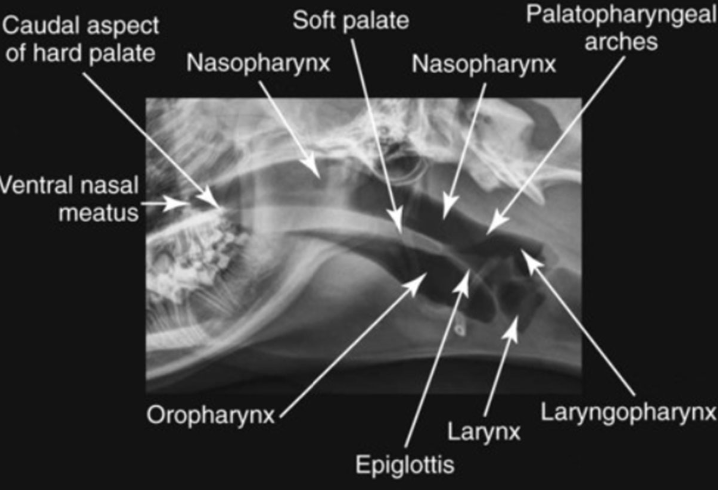
what may be seen with head/cervical/chest rads in patients with dysphagia?
rads look for structural disease, abnormal findings may include:
-dilated esophagus
-mass effect
-metallic foreign body
-air pockets (anaerobic bacteria)
what is the best use of contrast radiography?
search for structural causes of dysphagia in esophagus
how are contrast rads taken?
-start with lateral cervical (include oropharynx) and 3-view chest rads
-give liquid barium by mouth
-if suspected perforation, use nonionic iodinated contrast agent
-avoid sedation
-take repeated lateral views of neck and thorax after swallowing or soon after swallowing (right lateral recumbency)
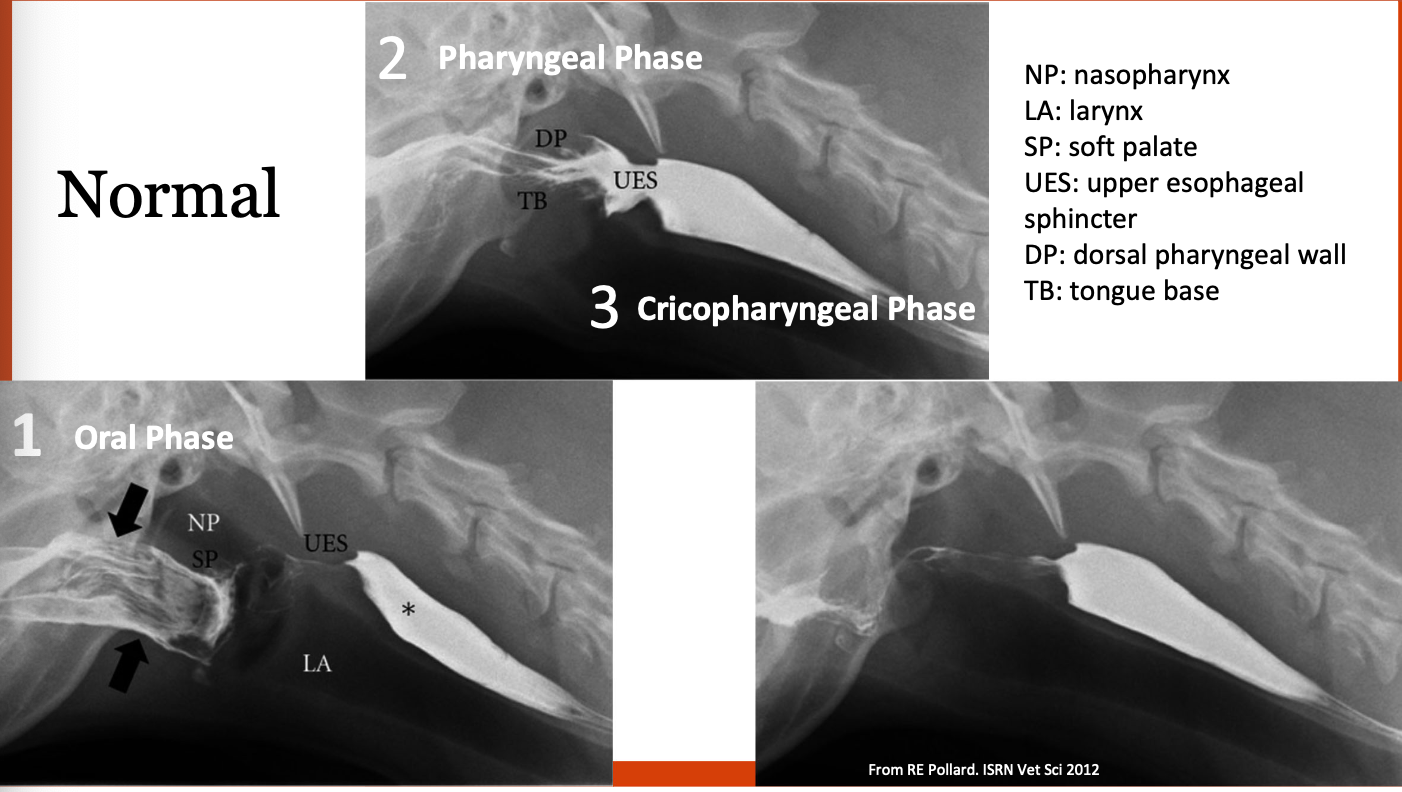
what does barium contrast videofluoroscopy evaluate?
evaluates for functional cause of dysphagia
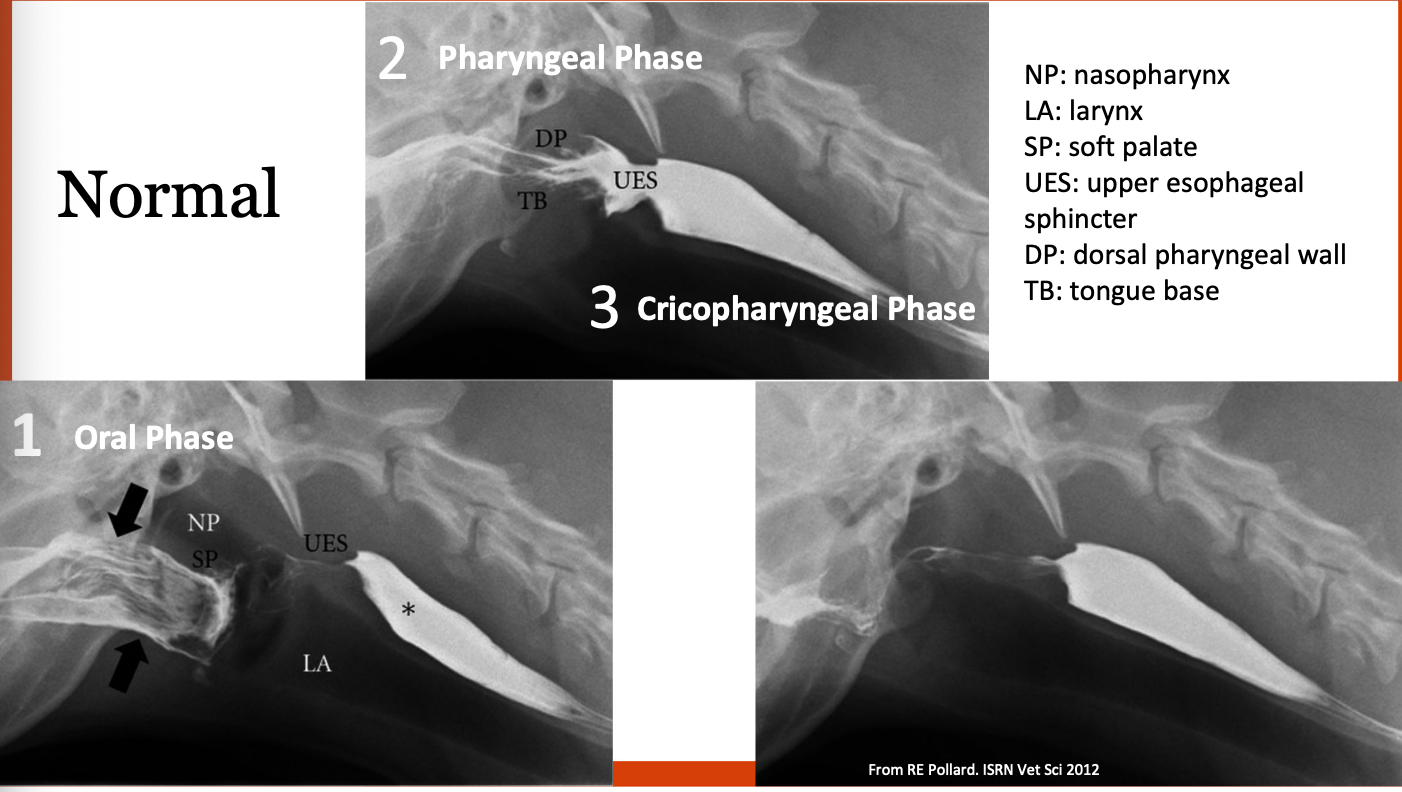
what is the procedure for barium contrast videofluoroscopy?
-fast for 12 hours
-survey rads of thorax/cervical region to rule out gross abnormalities
-give 3 foods with contrast: liquid, slurry, kibble
-visualize prehension of food, swallowing, esophageal motility
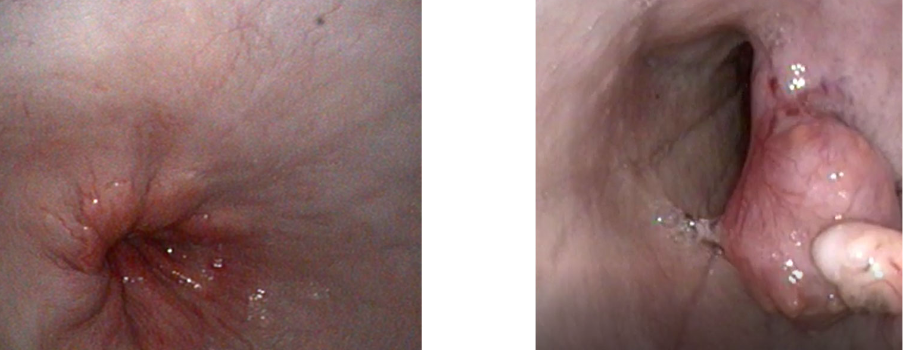
what does endoscopy of the esophagus evaluate?
can identify/look for esophageal disease, foreign bodies, strictures
what are clinical signs of oropharyngeal dysphagia?
occur while eating:
-retching
-gagging
-repeat swallowing
-food coming from nose
-exaggerated swallowing movements and foods will usually drop from mouth within seconds of prehension

what occurs during the oral phase of swallowing?
movement of the food bolus from the tongue to the pharynx
what are functional vs structural differentials for dysfunction of the oral phase of swallowing?
functional: cranial nerve 5 (trigeminal), 7 (facial), and 12 (hypoglossal) dysfunction
structural: skull fractures, oral masses or FBs
what occurs during the pharyngeal phase of swallowing?
transport of bolus from oropharynx to UES (located behind larynx)
what are functional vs structural differentials for dysfunction of the pharyngeal phase of swallowing?
functional: cranial nerve 5, 7, 9 (glossopharyngeal) and 10 (vagus) dysfunction--> pharyngeal paresis/paralysis
structural: pharyngeal abscess/FB/mass
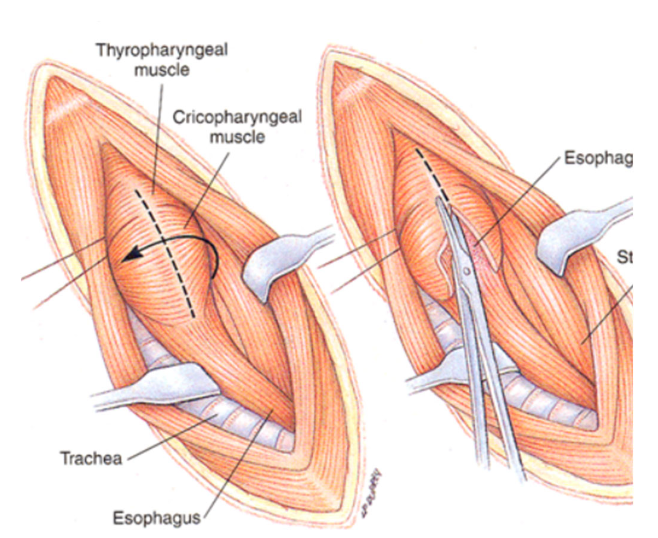
what occurs during the cricopharyngeal phase of swallowing?
relaxation of the UES (ie cricopharyngeal muscle)
what are functional differentials for dysfunction of the cricopharyngeal phase of swallowing?
cricopharyngeal achalasia
cricopharyngeal asynchrony
what cranial nerves are important for prehension, swallowing, esophageal motility, and laryngeal function?
CNs 5, 7, 9, 10, 12
what are clinical signs of neurogenic dysphagia?
-dropped jaw
-facial paralysis or reduced facial sensation
-atrophy of temporalis or masseter muscles
-drooling
-unable to prehend food
-tongue deviation
-choke/cough while eating
-larpar
-megaesophagus
what is cricopharyngeal dysphagia?
congenital or acquired neuromuscular disorder of the upper esophageal sphincter (UES), usually congenital in young dogs
dachshunds and goldens are predisposed
can be achalasia or asynchrony

True or false? With cricopharyngeal dysplasia, the dysphagia will only be seen with solid foods.
False. Dysphagia seen with liquids as well as it is a FUNCTIONAL disorder.
what is cricopharyngeal achalasia?
failure of the UES to relax
what is cricopharyngeal asynchrony?
lack of coordination between the UES relaxation and pharyngeal contraction
how is cricopharyngeal dysphagia diagnosed?
swallow contrast videofluoroscopy
when diagnosed, rule out myopathy or polyneuropathy
(ddx: myasthenia gravis - AChR antibody titers; autoimmune myositis - CK, muscle bx; hypothyroidism - serum total thyroxine, TSH)
how is cricopharyngeal dysphagia treated?
-surgical myotomy of cricopharyngeal muscle (unilateral); less successful with asynchrony
-injection of botulinum toxin into muscle (temporary for 3-4 months), if positive response, may respond favorably to surgery
-gastrostomy tube