UKMLA: Dermatology
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
Acne: Which bacteria can cause it?
Propionibacterium acne’s
Acne: What is the classification?
Non-inflammatory→ blackheads and whiteheads
Inflammatory→ papules, pustules and nodules
Severe→ nodules (cysts), scars, acne fulminans and acne conglobata
Acne Fulminans: What is the presentation?
Painful cysts, fever, fatigue→ review urgently in 24 hours
Teenager males mostly affected
Acne Conglobata: What is the presentation?
Uncommon presentation of severe nodular/cystic acne with interconnecting sinus tracts and extensive scaring
Acne: What is the management of mild-moderate acne?
2 of the following topical treatments:
Benzoyl peroxide
Clindamycin
Tretinoin/adapalene
Acne: What is the management of moderate-severe acne?
12 week course of:
Topical tretinoin/adapelene + benzoyl peroxide
Topical azelaic acid with oral lympecycline or doxycycline (tetracycline antibiotics)
Give trimpethoprim and erythromycin in pregnant women
Acne: What is the management of severe acne?
Isotretinoin but:
Screen for mental health disorders before as it can worsen it
Start females of contraception as it is teratogenic
Make sure the patient is aware it can cause blistering and skin peeling
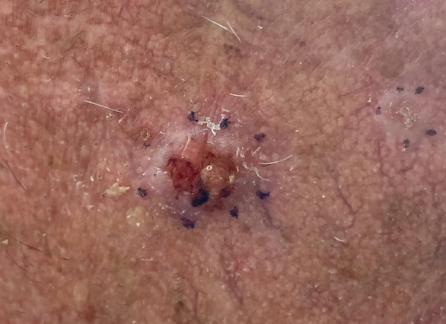
Actinic Keratosis: What is it?
Pre-malignant skin condition that leads to squamous cell carcinoma
Actinic Keratosis: What is the cause?
Actinic keratoses are thought to arise due to sun exposure leading to DNA damage within the keratinocytes
Actinic Keratosis: What is the typical presentation?
Thick papule or plaques with rough, surface
Occurs on sun-exposure area of skin

Actinic keratosis: What are the risk factors?
Type I or II skin (fair, burns easily)
History of sunburn or extensive sun exposure
Outdoor occupation or hobbies
Immunosuppression
Actinic Keratosis: What is the management?
5-Fluorouracil (a cytotoxic agent)
Non-steroidal anti-inflammatory drugs (NSAIDs)
Imiquimod (an immune response modifier)
Patient education on sun-protective measures is also an essential part of management
Alopecia: What is trichotillomania?
Hair-pulling disorder
Alopecia: What is alopecia arteta?
Autoimmune cause of patchy hair loss
Alopecia: What is androgenetic alopecia?
Diffuse thinning of the scalp hair
Alopecia: What is telogen effluvium?
Temporary hair loss due to excessive shedding of resting hair (e.g. after child-birth or weight loss)
Alopecia: What is the management?
Wig
Topical steroids → clobetasol propionate
Minoxidil
Dithranol (skin stain)
BCC: What is the pathophysiolgy?
Originates from basal keratinocytes
DNA damage due to UV radiation
Most common skin cancer
BCC: What is the classification?
Nodular→ most common, shiny pink nodule
Sclerosing→ firm, scar-like plaque
Superficial→ scaly red patches (mistaken for eczema or psoriasis)
BCC: What are the symptoms?
Very slow growing
Local destruction can occur
Usually painless and ulcerates
Flesh coloured nodules with central depression, pearly surface, rolled edge, and telangiectasia
They can can necrose and ulcerate in the centre ('rodent ulcer)
BCC: What are the investigations?
Excision biopsy with 4mm margin
If lesion is 2cm diameter or on ear/lip/face/genitals/hand/feet etc or patient is immunocompromised or had BCC before→ excision biopsy with 6mm margin
BCC: What is the treatment?
Almost always treated surgically with excision using a 4mm margin (6mm for high-risk lesions)
Micrographic surgery for poorly-defined areas
Radiotherapy
Other options: curettage and cautery, topical 5-fluorouracil, topical imiquimod, cryotherapy for low-risk lesions
Cellulitis: What is the pathophysiology?
The most common offending organisms are Streptococcus pyogenes or Group A beta-haemolytic streptococci
Cellulitis: What are the risk factors?
Breaks in the skin
Chronic lymphadenopathy
Obesity
Diabetes
Immunosuppression
IV drug use
Previous history of cellulitis
Cellulitis: What are the symptoms?
Generally caused by Streptococcus and/or Staphylococcus organisms.
Erythema
Calor (heat)
Swelling
Pain
Poorly demarcated margins
Systemic upset: fever, malaise
Lymphadenopathy
Rarely blisters and pustules (severe disease)
Often evidence of breach of skin barrier e.g. trauma, ulcer etc.
Cellulitis: What is the Eron classification?
Class 1→ no systemic toxicity or uncontrolled comorbidities
Class 2→ systemically unwell
Class 3→ acute confusion, tachycardia, tachypnoea, hypotension, or unstable comorbidities
Class 4→ sepsis or necrotising fasciitis
Cellulitis: What are the investigations?
Blood tests - FBC (high WCC), CRP, U+E (may be AKI if severe infection), blood cultures
Wound swab if there is an open wound
US to check for abscess
Cellulitis: What is the management?
Class 1→ flucloxacillin
Class 2→ admit
Class 3 + 4→ admit for IV antibiotics
Patients with infection near eyes or nose→ co-amoxiclav (or metronidazole and clarithromycin if allergic)
Chicken Pox: What is the virus name?
Varicella-zoster virus HHV3
Chicken Pox: What is the infectious period?
1-2 days before rash appears and until 5 days until after rash appears.
Onset to symptoms is 14 to 16 days from exposure
Chicken Pox: What are the symptoms?
Raised,red itchy spots
Fluid-filled vesicles
Within 5 days, it crusts over

Chicken Pox: What is the management?
Prevent itching
Oatmeal baths
Chlorpenamine to relieve itching
Paracetamol
If pregnant or neonate-. IV aciclovir
PEP for immunocompromised patient is oral aciclovir 7-14 days after exposure
Contact Dermatitis: What are the two types?
Irritant→ exposure to chemicals or solvents
Allergic→ delayed type 4 hypersensitivity reaction
Contact Dermatitis: Which immune cells are involved?
T cells mediate the delayed type 4 hypersensitivity reaction.
Contact Dermatitis: What are the symptoms of irritant contact dermatitis?
Burning
Pain
Stinging
Contact Dermatitis: What are the symptoms of allergic contact dermatitis?
Itchy
Eczematous rash
Occurs 24-48 hours after exposure
Contact Dermatitis: What is the investigation?
Patch testing
Contact Dermatitis: What is the management?
Emolient use
Topic steroids
Anti-histamines
Folliculitis: What is the cause?
Staph aureus
Folliculitis: What is the name of the type of folliculitis common in immunocompromised patients?
Eosoniophilic folliculitis→ requires biopsy for investigation!!
Folliculitis: What are the signs and symptoms?
Papules
Pustules
Never on hands or soles of feet
Folliculitis: What is the management?
Topical antibiotics and chlorhexidine scrub

Hemangiomas: What are they?
A common benign vascular tumour that occurs in infancy
Hemangiomas: What is the typical clinical presentation?
Occurs in infancy or pregnancy
Typically affects head/neck
Common in females
Grows over time
Hemangiomas: What is the management?
Leave the lesion and do nothing
Propranolol if it needs intervention e.g. near the eye
Hemangiomas: What is the conservative management?
Leave the lesion and do nothing
Impetigo: What is it?
Contagious infection of the epidermis
Occurs in infants and school-age children (typically 0-4 years old)
Impetigo: What is the pathophysiology?
Caused by staphylococcus aureus (80%), group A haemolytic streptococcus (10%)
The bacteria produces exotoxins that target desmoglein-1
Impetigo: What are the risk factors?
Pre-existing skin conditions
Immunosuppression
Direct contact with infected individual
Crowding, humidity and poor hygiene
Impetigo: What is the classification?
Bullous→ fluid filled lesions greater than 1cm
Non-bullous→ no fluid filled lesions
Impetigo: What are the symptoms?
Erythematous macule
Superficial erosion with golden crust
Sores (non-bullous)
Blisters (bullous)

Impetigo: What is the management?
Local non-bullous→ hydrogen peroxide 1% cream for 5 days
Widespread non-bullous→ oral flucloxacillin for 5 days or fusidic acid cream for 5 days
Bullous→ antibiotics for up to 7 days
Children should be off school until all lesions are healed or until 48 hours after starting treatment.
Measles: What is the cause?
Measles morbillivirus (paramyxovirus)→ transmitted via droplets (nose, throat or mouth)
Measles: What is the epidemiology?
Affects anyone at any age
Caused by measles morbillivirus→ single stranded, RNA virus
7-21 days incubation period
Infectious from 4 days before rash appears until 4 days after the rash appears
Measles: What are the symptoms?
Prodromal symptoms (pyrexia and cough)
Fever over 40 degrees
Coryzal symptoms
Conjunctivitis
Koplik spots→ small grey discolourations in the mouth
Rash appears behind ears then spreads to trunk and limbs over 3-4 days

Measles: What is the investigation?
Oral fluid sample for:
Measles RNA 1-3 days after rash onset
Measles-specific IgM/IgG → 3-14 days after rash
Measles: What is the management?
Analgesia
Fluids
Vitamin A
Stay off school for at least 4 days after rash appears
Stay away from pregnant women and immunocompromised people
Measles: How can it be prevented?
MMR vaccine
Necrotising Fasciitis: What is the classification?
Type 1→ polymicrobial (most common)
Type 2→ monomicrobial (e.g. strep or staph)
Type 3→ rare but associated with contaminated seafood or seawater exposure
Type 4→ rare but fungal associated with burns or trauma
Necrotising Fasciitis: What is gas gangrene?
Caused by clostridium perfingens → characterised by crepitus on auscultation

Necrotising Fasciitis: What is fournier’s gangrene?
Necrotising fasciitis of the perineum
Necrotising Fasciitis: What are the bedside investigations?
Bedside:
Wound swab to identify pathogens
Blood gas may show metabolic acidosis; hyperglycaemia and raised lactate common
Necrotising Fasciitis: What is the management?
Broad-spectrum IV antibiotics within the first hour; commonly used include tazocin, meropenem, clindamycin, and linezolid.
Surgical debridement
Necrotising Fasciitis: What are the differentials?
Cellulitis: Localised erythema and swelling, but lacks rapid progression and severe systemic illness.
Deep vein thrombosis: Localised pain and swelling, limited skin changes, and patients are not systemically unwell.
Osteomyelitis: Fever, pain, and swelling but usually more chronic and does not progress rapidly.
Psoriasis: What is the diagnostic feature?
Psoriasis is a chronic autoimmune disease characterised by well-demarcated, erythematous, scaly plaques.
Psoriasis: What are the 5 different types?
Chronic plaque psoriasis (most common, knees, elbow, scalp, lower back)
Flexural psoriasis→ smooth without scales in flexures and skin folds
Guttate psoriasis→ small, tear-drop shaped after strep infection in young adults
Psoriasis: What are the risk factors?
Skin trauma
Streptococcus, HIV infections
B-blocker, anti-malarials, lithium, NSAIDS
Steroid withdrawal
Stress
Alcohol + smoking
Cold/dry weather
Psoriasis: What are the signs?
Nailbed pitting → superficial depressions in the nailbed
Oncyholysis → separation of nail plate from nailbed
Subungual hyperkeratosis→ thickening of the nailbed

Psoriasis: What is the management?
Corticosteroid + vitamin D
Vitamin D only 2x daily
Corticosteroid only 2x daily
Phototherapy UVA
If the above doesn’t help then give either methotrexate, cyclosporin (urgent help, pregnant or female of childbearing age) or acitretin
Scabies: What is the cause?
Sarcoptes scabei mite → causes type 4 hypersensitivity reaction 30 days after initial infection
Scabies: What are the symptoms?
Intensely itchy rash
Worse at night
Affects flexures of wrist, axilla, abdomen and groin
Superficial burrows can be seen
Scabies: What is norwegian/crusted scabies?
Scabies in immunocompromised patients e.g. HIV

Scabies: What is the management?
Topical permethrin 5% for 12 hours, repeat in 7 days ( Apply to cool and dry skin, to the whole body → allow lotion to dry before dressing and leave it on for 12 hours before washing off→ repeat after 7 days)
Crotamiton cream to relieve itching
Treat everyone from the same household, on the same day
Scabies: What is the management of Norwegian scabies?
Oral ivermectin + treat household members
Can use in combination with permethrin for maximum effect
Shingles: What is the cause?
Reactivation of varicella zoster virus in the nerve ganglia after chickenpox
Shingles: What is the epidemiology?
Affects the elderly
If a young adult is affected, investigate for an underlying immune condition
Shingles: What are the symptoms?
Tingling feeling
Erythematous papules within a few days→ fluid filled vesicles→ bursts and crusts
Painful rash

Shingles: What is the management?
Valaciclovir 1g 3x a day for 7 days
IV antivirals in hospital if immunocompromised
Avoid contact with vulnerable people e.g. pregnant women
Manage pain via NSAID or amitriptyline if still in pain
Shingles: How can it be prevented?
Shingles vaccine→ offered to people in their 70’s as a one-off vaccine
SCC: What is the pathophysiology?
Originates in epidermal keratinocytes
Pain, tenderness or bleeding
Grows over few weeks or months
SCC: What is the presentation?
Keratinised
Scaly horn or plug (bump)
SCC: Which lesions can develop into SCC?
Actinic keratosis
Marjolin ulcer→ due to previous injury e.g. burns or scars
Bowen’s disease→ precancerous lesion which is defined by irregular, red, keratinised scaly plaques
SCC: What is the treatment?
Almost always treated surgically with excision using a 4mm margin (6mm for high-risk lesions)
Micrographic surgery for poorly-defined areas
Radiotherapy
Other options: curettage and cautery, topical 5-fluorouracil, topical imiquimod, cryotherapy for low-risk lesions
Topical Steroids: Which is the least potent?
Hydrocortisone
Topical Steroids: Which is mildly potent?
Alclometasone
Topical Steroids: Which is moderately potent?
Mometasone
Topical Steroids: Which is very potent?
Betametasone and Fluticasone
Topical Steroids: Which is the most potent?
Clobetasol→ “dermovate”