protein assays and hepatobiliary function tests
1/35
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
chemical measurements should be completed in
1 hour. else freeze the sample to preserve integrity. it should not be refrozen a second time.
refractometric method
measures the refractive index of serum or plasma with a refractometer. used to measure total protein. The refractive index of the sample is a function of the concentration of solid particles in the sample. In plasma, the primary solids are the proteins. This method is a good screening test, because it is fast, inexpensive, and accurate.
biuret photometric method
measures the number of molecules that contain more than three peptide bonds in serum or plasma. This method is commonly used by analytic instruments in the laboratory. It is a simple method that yields accurate results.
dye binding method and precipitation method
not commonly performed. used to measure a small amount of protein in urine and cerebrospinal fluid.
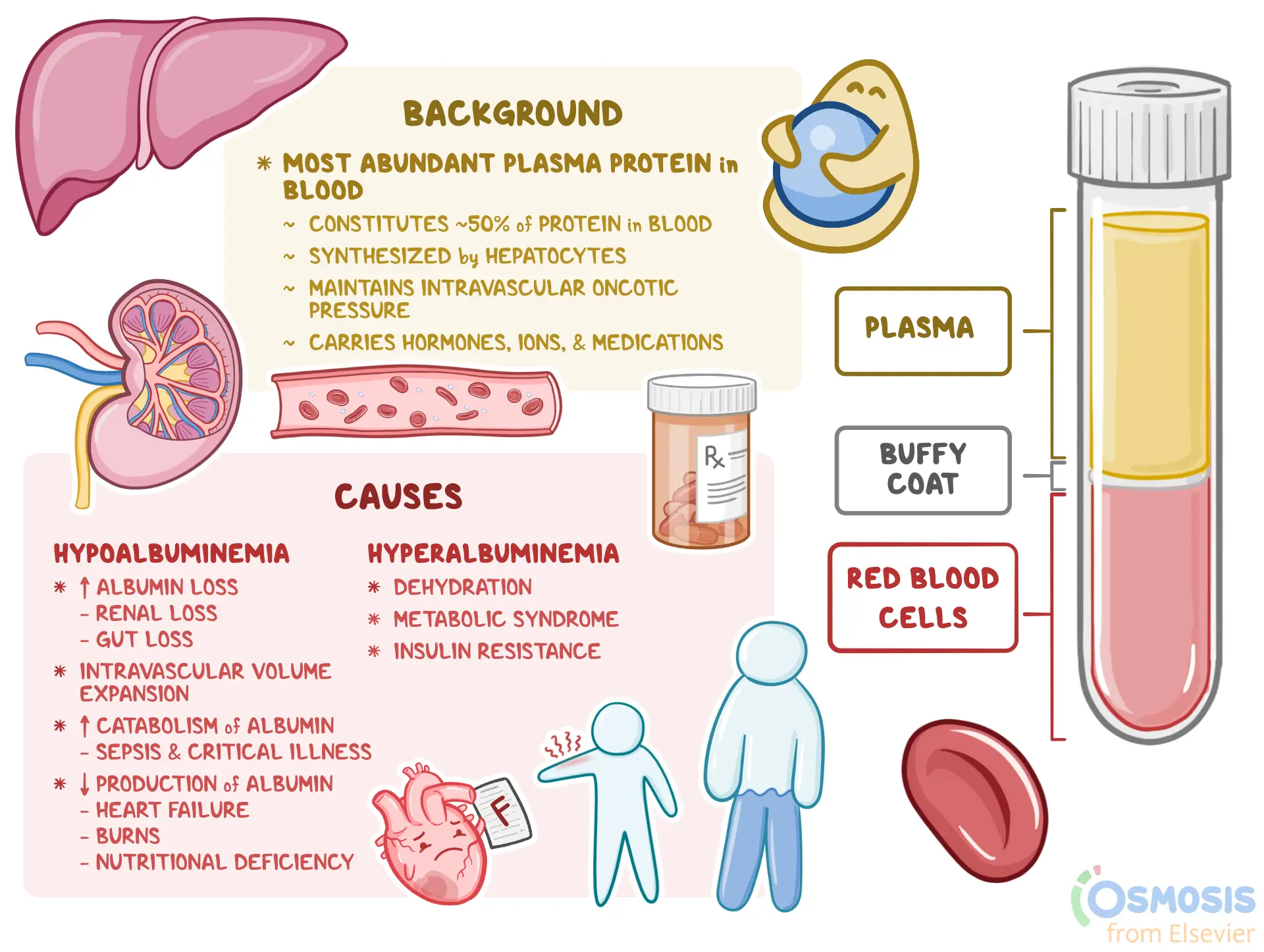
albumin
elevated in dehydration, hemolysis, lipemia, laboratory error. Decreased in protein losing nephropathy, gastroenteropathy, liver failure, malnutrition, exudative skin disease, neonates, external blood loss, chronic effusions, hyperglobulinemia, multiple myeloma. one of the most important proteins in plasma or serum. It makes up 35% to 50% of the total plasma protein in most animals, and any significant state of hypoproteinemia is most likely caused by albumin loss. Hepatocytes synthesize albumin, and any diffuse liver disease may result in decreased albumin synthesis. Renal disease, dietary intake, and intestinal protein absorption may also influence the plasma albumin level. Albumin is the major binding and transport protein in the blood, and it is responsible for maintaining the osmotic pressure of the plasma. The primary photometric test for albumin in veterinary patients is the bromocresol green dye-binding method.

globulins
elevated in dehydration, infection, immune mediated disease, neoplasia. any decreases are unremarkable. The globulins are a complex group of proteins.
Alpha globulins are synthesized in the liver and primarily transport and bind proteins. Two important proteins in this fraction are high-density lipoproteins and very-low-density lipoproteins.
Beta globulins include complement (C3, C4), transferrin, and ferritin. They are responsible for iron transport, heme binding, and fibrin formation and lysis.
Gamma globulins (immuno-globulins) are synthesized by plasma cells, and they are responsible for antibody production (immunity). The immunoglobulins (Ig) that have been identified in animals are IgG, IgD, IgE, IgA, and IgM.
Direct chemical measurements of globulin are rarely performed. Globulin concentration is normally estimated by determining the difference between the total protein and albumin concentrations.
albumin/globulin ratio
High total protein with a normal A/G ratio
Dehydration
High total protein with low A/G ratio
Hyperglobulinemia
A/G ratio of 1
Hemorrhage
An alteration in the normal ratio of albumin to globulin (A/G) is frequently the first indication of a protein abnormality. The ratio is analyzed in conjunction with a protein profile. The A/G can be used to detect increased or decreased albumin and globulin concentrations. Many pathologic conditions alter the A/G. However, if the albumin and globulin concentrations are reduced in equal proportions, such as with hemorrhage, no alteration in A/G will be present. The A/G is determined by dividing the albumin concentration by the globulin concentration.
In dogs, horses, sheep, and goats, the albumin concentration is usually greater than the globulin concentration (i.e., the A/G is more than 1.00).
In cattle, pigs, and cats, the albumin concentration is usually equal to or less than the globulin concentration (i.e., the A/G is less than 1.00).
Fibrinogen
Elevated in
Acute inflammatory disease
Decreased in
DIC
Severe liver disease
Fibrinogen is synthesized by hepatocytes. It is the precursor of fibrin, which is the insoluble protein that forms the matrix of blood clots, and it is one of the factors necessary for clot formation. If fibrinogen levels are decreased, blood does not form a stable clot or does not clot at all. Fibrinogen makes up 3% to 6% of the total plasma protein content. Because it is removed from plasma by the clotting process, no fibrinogen is found in serum. Fibrinogen assays are performed as part of a coagulation profile but may be a useful tool as part of the chemistry profile. Acute inflammation or tissue damage may elevate plasma fibrinogen levels and has been used to detect subclinical inflammation in horses. The fibrinogen value is calculated by subtracting the total plasma protein value of the heated tubes from that of the unheated tubes. This protein measurement of the heated tubes should be lower because fibrinogen has been removed from the plasma. Some automated analyzers may also provide fibrinogen values.
Acute-phase proteins
Elevated in
Inflammation prior to an inflammatory leukogram
Decreased in
Responses to treatment
primarily produced by hepatocytes immediately following injury or inflammation. There are about 30 recognized acute-phase proteins, and different species produce different ones at different levels. In addition to serum amyloid A (SAA), significant acute-phase proteins of domestic animals include C-reactive protein (CRP), fibrinogen, haptoglobin (HP), ceruloplasmin, a1-acid glycoprotein (AGP), and major acute-phase protein (MAP). Albumin and transferrin are referred to as negative acute-phase proteins because their plasma concentration decreases following injury or inflammation. Although serum electrophoresis can aid in identifying increased levels of acute-phase proteins, measurements of specific acute-phase proteins is more useful. Most of the acute-phase proteins of significance in domestic animals are measured with immunoassays, although a chemical test is available for measurement of haptoglobin. A handheld portable analyzer is available for measurement of SAA in horses. SAA is a major acute-phase protein of many species of mammals and is of particular importance in cats, cattle, and horses. Serum amyloid levels rise within hours following injury or inflammation. The magnitude of the increase can aid in determining the presence of specific disease states. For example, in healthy cats, SAA is generally below 20 mg/L. Increases in SAA are correlated to specific disease states in cats (Table 20.1). SAA values are used to differentiate infectious disease from noninfectious disease in horses and to track response to therapy. CRP is a biomarker for inflammation produced in the liver. Levels of CRP rise dramatically in a variety of disease states, including cardiac disease, sepsis, and neoplasia. The response occurs within 6 hours after the inflammatory event or trauma and peaks in 24 to 48 hours. The levels of CRP drop rapidly as the triggering event is treated.
Hepatobiliary Assays
The liver is the largest internal organ. It is complex in structure, function, and pathologic characteristics. It has many functions, including the metabolism of amino acids, carbohydrates, and lipids; the synthesis of albumin, cholesterol, plasma proteins, and clotting factors; the digestion and absorption of nutrients related to bile formation; the secretion of bilirubin and bile; and elimination, such as the detoxification of toxins and the catabolism of certain drugs. These functions are controlled by enzymatic reactions. The gallbladder is closely associated with the liver, both anatomically and functionally. Its primary function is as a storage site for bile. Malfunctions in the liver or gallbladder result in predictable clinical signs of jaundice, hypoalbuminemia, problems with hemostasis, hypoglycemia, hyperlipoproteinemia, and hepatoencephalopathy. Hepatic cells exhibit extreme diversity of function and are capable of regeneration if damaged. As a result, more than 100 different types of tests are available to evaluate liver function.
Usually liver disease has progressed significantly before clinical signs appear. Some liver function tests are designed to measure substances that are produced by the liver, modified by the liver, or released when hepatocytes are damaged. Other liver function tests measure those enzymes that have altered serum concentrations as a result of cholestasis. Liver cells also compartmentalize the work so that damage to one zone of the liver may not affect all liver functions. Liver function tests are usually performed with serial determinations and several different types of liver tests completed to assist with verifying the functional status of the organ. No single test is superior to any other for detecting hepatobiliary disease. New tests are being developed to allow for the detection of hepatic disease before the liver is severely damaged.
hepatocyte function tests
Many substances are taken up, modified, produced, and secreted by the liver. Alteration in the ability to perform these specific functions provides an overview of liver function. Tests of hepatocyte function that are performed in veterinary practice include bilirubin and bile acids. Other substances produced by hepatocytes are less-sensitive indicators of liver function, because test results may not show abnormalities until two thirds to three fourths of liver tissue is damaged. These less-sensitive tests include albumin and cholesterol.
Enzymes released from damaged hepatocytes- alanine transaminase, aspartate transaminase, iditol dehydrogenase, glutamate dehydrogenase.
Enzymes associated with cholestasis- alkaline phosphatase, gamma glutamyltranserase.
Hepatocyte function tests- bilirubin, bile acids
Bilirubin
· Elevated in
· Prehepatic conditions
· Hemolytic anemia
· Cholestasis
· Intrahepatic conditions
· Duodenal perforation
· Ruptured gallbladder
. Decreased in
· Unremarkable
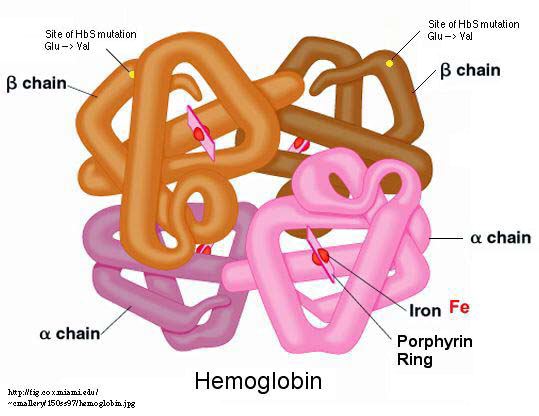
Bilirubin is an insoluble molecule derived from the breakdown of hemoglobin by macrophages in the spleen. The molecule is bound to albumin and transported to the liver. The hepatic cells metabolize and conjugate the bilirubin to the molecule bilirubin glucuronide. This molecule is then secreted from the hepatocytes, and it becomes a component of bile. Bacteria within the gastrointestinal system act on the bilirubin glucuronide and produce a group of compounds collectively referred to as urobilinogen. Urobilinogen is broken down into urobilin before being excreted in the feces. Bilirubin glucuronide and urobilinogen may also be absorbed directly into the blood and excreted by the kidneys. Bilirubin can also be broken down with exposure to light. It is important that samples be protected from light to ensure accurate results. Measurements of the circulating levels of these various populations of bilirubin can help to pinpoint the cause of jaundice. Differences in the relative solubility of each of these molecules allow them to be individually quantified. In most animals, the prehepatic (bound to albumin) bilirubin comprises approximately two thirds of the total bilirubin in serum. Increases in this population indicate problems with uptake (hepatic damage). Increases in conjugated bilirubin indicate bile duct obstruction.
Assays can directly measure total bilirubin (conjugated bilirubin plus unconjugated bilirubin) and conjugated bilirubin. Conjugated bilirubin is sometimes referred to as direct bilirubin, because test methods directly measure the amount of conjugated bilirubin in the sample. Unconjugated bilirubin is sometimes referred to as indirect bilirubin, because its concentration is indirectly calculated by subtracting the conjugated bilirubin concentration from the total bilirubin concentration of the sample. Bilirubin is assayed to determine the cause of jaundice, to evaluate liver function, and to check the patency of bile ducts.
Blood levels of conjugated (direct) bilirubin are elevated with hepatocellular damage or with bile duct injury or obstruction.
Blood levels of unconjugated (indirect) bilirubin are elevated with excessive erythrocyte destruction or defects in the transport mechanism that allow bilirubin to enter hepatocytes for conjugation.
acute pancreatitis
SAA 56.9 in cats
Feline infectious peritonitis (FIP)
SAA 29.4 in cats
Hyperthyroidism
SAA 16.5 in cats
Diabetes Mellitus
SAA 14.9 in cats
Lymphoma
SAA 13.7 in cats
Chronic renal Failure
SAA 8.7 in cats
Bile Acids
· Elevated in
· Hepatocellular disease
· Cholestatic disease
· Portosystemic shunt
· Decreased in
· Delayed gastric emptying
· Malabsorptive disorders
· Rapid intestinal transport
· Ileal resection
Bile acids serve many functions. They aid in fat absorption by enabling the formation of micelles in the gastrointestinal system and modulate cholesterol levels via bile acid synthesis. Bile acids are synthesized by hepatocytes from cholesterol, and they are conjugated with glycine or taurine. Conjugated bile acids are secreted across the canalicular membrane, and they reach the duodenum by way of the biliary system. The gallbladder stores bile acids (except in the horse since they don’t have gallbladders) until contraction associated with feeding. When bile acids reach the ileum, they are transported to the portal circulation and travel back to the liver. Approximately 90% to 95% of the bile acids are actively resorbed in the ileum, and the remaining 5% to 10% are excreted in the feces. The reabsorbed bile acids are carried to the liver, where they are reconjugated and excreted as part of the enterohepatic circulation of bile acids.
Spillover bile acids
that escape from the enterohepatic circulation may be detected in normal animals; serum concentrations of bile acids correlate with portal concentrations. As a result, postprandial serum bile acid (SBA) concentrations are higher than fasting concentrations. Any process that impairs the hepatocellular, biliary, or portal enterohepatic circulation of bile acids results in elevated SBA levels. The great advantages of SBA determinations as liver function tests are that they evaluate the major anatomic components of the hepatobiliary system and that they are stable in vitro. The SBA level is normally elevated after a meal, because the gallbladder has contracted and released increased amounts of bile into the duodenum. Paired serum samples performed after 12 hours of fasting and 2 hours postprandial are needed to perform the test. The difference in the bile acid concentration of the samples is reported. In horses, a single sample is tested. Inadequate fasting or spontaneous gallbladder contraction can increase fasting bile acid levels. Exposing the patient to even the aroma of food can result in spontaneous gallbladder contraction. Prolonged fasting and diarrhea can decrease bile acids.
Elevated Spillover Bile Acids levels
usually indicate liver diseases such as congenital portosystemic shunts, chronic hepatitis, hepatic cirrhosis, cholestasis, or neoplasms. Bile acid levels are unspecific with regard to the type of liver problem that exists and are therefore used as a screening test for liver disease. Bile acid levels may detect liver problems before an animal becomes icteric. They may also be used to follow the progress of liver disease during treatment. Increased bile acid concentrations can also result from extrahepatic diseases that secondarily affect the liver.
A decreased bile acid concentration may be seen with intestinal malabsorptive diseases.
In horses, increased bile acid concentrations can be the result of hepatobiliary disease or decreased feed intake.
The reference ranges for bile acids in cows are widely variable. Bile acid testing is not a sensitive indicator of disease in cows.
Bile acids may be determined by several methods, and the most commonly used is an enzymatic method. The 3-hydroxy bile acids react with 3-hydroxisteroid dehydrogenase and then with diformazan. Color generation is measured by end point spectrophotometry. Lipemic postprandial samples must be cleared by centrifugation to avoid interference with spectrophotometry. A bile acid test that uses immunologic methods (e.g., enzyme-linked immunosorbent assay) is now available for use in the veterinary clinic.
cholesterol
Elevated in
· Postprandial
· Primary hyperlipidemia
· Endocrine disorders
· Cholestasis
· High cholesterol diets
· Nephrotic syndrome
· Protein losing nephropathy
· Idiopathic
· Decreased in
· Liver failure
· Malabsorption
· Maldigestion
· Protein losing enteropathy
· Portosystemic shunt
· Lymphangiectasia
· Starvation
· Hypoadrenocorticism
· Neoplasia
a plasma lipoprotein that is produced primarily in the liver, and it is also ingested in food. Cholestasis causes an increase in serum cholesterol in some species. However, large differences exist in the lipoprotein profiles of different species, and the clearance of lipoproteins is not well characterized in most veterinary species. A number of automated analyzers are available that provide cholesterol and other lipoprotein values. Hyperlipidemia is often secondary to other conditions. Primary hyperlipidemia is rare, and it is associated with inherited conditions in some breeds.
A cholesterol assay is sometimes used as a screening test for hypothyroidism. Thyroid hormone controls the synthesis and destruction of cholesterol in the body. Insufficient thyroid hormone (hypothyroidism) results in hypercholesterolemia, because the rate of cholesterol destruction is relatively slower than the rate of synthesis. Other diseases associated with hypercholesterolemia include hyperadrenocorticism, diabetes mellitus, and nephrotic syndrome. Dietary causes of hypercholesterolemia are rare but may include high-fat diets and postprandial lipemia.
Cholesterol by itself does not cause the grossly lipemic plasma that is seen after eating; triglycerides are also usually present. The administration of corticosteroids may also cause an elevated blood cholesterol concentration. Fluoride and oxalate anticoagulants may elevate enzymatic method results.
Enzymes released form damaged hepatocytes
When hepatocytes are damaged and enzymes leak into the blood, a detectable rise in the blood levels of enzymes associated with liver cells occurs. These components, which are commonly referred to as the "leakage enzymes," include the transferase enzymes alanine transaminase (alanine amino-transferase) (ALT) and aspartate transaminase (aspartate aminotransferase) (AST), as well as the dehydrogenase enzymes
iditol dehydrogenase (sorbitol dehydrogenase) (ID) and glutamate dehydrogenase (GLDH). Transaminases catalyze the reactions that transfer amine groups from amino acids to keto acids during the production of new amino acids. The enzymes are therefore found in tissues that have high rates of protein catabolism. Although other transaminases are present in hepatocytes, the only readily available tests are for ALT and AST. Dehydrogenases catalyze the transfer of hydrogen groups, primarily during glycolysis. Transaminases and dehydrogenases are found either free in the cytoplasm of hepatocytes or bound to the cell membrane. The serum levels of these enzymes vary in different species, and most have nonhepatic sources
Alanine Transaminase
Elevated in
. Liver inflammation
· Liver infection
. Toxins·
Neoplasia
Drugs
Endocrine
Liver trauma
Hypoxia
Feline hepatic lipidosis
Copper storage discases
Liver lobe torsion
Hepatocellular regeneration
Cirrhosis
. Decreased in
· End-stage liver disease
· Unremarkable
In dogs, cats, and primates, the major source of ALT is the hepatocyte, where the enzyme is found free in the cytoplasm. ALT is considered a liver-specific enzyme in these species.
Horses, ruminants, pigs, and birds do not have enough ALT in the hepatocytes for this enzyme to be considered liver specific. Other sources of ALT are renal cells, cardiac muscle, skeletal muscle, and the pancreas. Damage to these tissues may also result in increased serum ALT levels. The administration of corticosteroids or anticonvulsant medications may also lead to increases in serum ALT. ALT is used as a screening test for liver disease, because it is not precise enough to identify specific liver diseases. No correlation exists between the blood levels of the enzyme and the severity of hepatic damage. Increases in ALT are usually seen within 12 hours of hepatocyte damage, and peak levels are seen at 24 to 48 hours. The serum levels will return to reference ranges within a few weeks unless a chronic liver insult is present.
Aspartate Transaminase
AST is present in hepatocytes, which are found free in the cytoplasm as well as bound to mitochondrial membrane. More severe liver damage is required to release the membrane bound AST. AST levels tend to rise more slowly than do ALT levels, and they return to normal levels within a day provide chronic liver insult is not present. AST is found in significant amounts in many other tissues, including erythrocytes, cardia muscle, skeletal muscle, the kidneys, and the pancreas. A increased blood level of AST may indicate nonspecific liver damage, or it may be caused by strenuous exercise or intramuscular injection. The most common causes of increased blood levels of AST are hepatic disease, muscle inflammation of necrosis, and spontaneous or artifactual hemolysis. If the AST level is elevated, the serum or plasma sample should examined for hemolysis. Creatine kinase activity should also be assessed to rule out muscle damage before attributing an AST increase to liver damage.
Iditol Dehydrogenase (sorbitol dehydrogenase)
· Elevated in
· Artifact
· Hepatic injury
· Decreased in
· Unremarkable
The primary source of ID is the hepatocyte. Smaller amounts of the enzyme are found in the kidney, the small intestine, skeletal muscle, and erythrocytes. ID is present in the hepatocytes of all common domestic species, but it is especially
useful for evaluating liver damage in large animals such as sheep, goats, swine, horses, and cattle. Large animal hepatocytes do not contain diagnostic levels of ALT, so ID offers a liver-specific diagnostic test. The plasma level of ID rises quickly with hepatocellular damage or necrosis. ID assay can be used in all species to detect hepatocellular damage or necrosis, thereby eliminating the need for other tests (e.g., the ALT assay). The disadvantage of ID analysis is that ID is unstable in serum, so its activity declines within a few hours. If testing is delayed, samples should be frozen. ID tests are not readily available to the average veterinary laboratory. Samples to be sent to outside laboratories should be packed in ice for transport.
Glutamate Dehydrogenase
· Elevated in
· Liver injury
· Decreased in
· Unremarkable
GLDH is a mitochondrial-bound enzyme found in high concentrations in the hepatocytes of cattle, sheep, and goats. An increase in this enzyme is indicative of hepatocyte damage or necrosis in cattle and sheep. GLDH could be the enzyme of choice for evaluating ruminant and avian liver function, but no standardized test method has been developed for use in a veterinary practice laboratory.
enzymes associated with cholestatsis
blood levels of certain enzymes become elevated with cholestasis (bile duct obstruction), metabolic defects in liver cells, the administration of certain medications, and as a result of the action of certain hormones, especially those of the thyroid. These enzymes are primarily membrane bound. The exact mechanism that induces increased levels of these enzymes when cholestasis is present is not well documented
Alkaline PHosphatase
· Elevated in
. Liver conditions
· Gall bladder condition
. Steroids
· Growth
· Decreased in
· Unremarkable
Alkaline phosphatase (AP) is present as isoenzymes in many tissues, particularly osteoblasts in bone, chondroblasts in cartilage, the intestine, the placenta, and cells of the hepatobiliary system in the liver. The isoenzymes of AP tend to remain in circulation for approximately 2 to 3 days, with the exception of the intestinal isoenzyme, which circulates for just a few hours. A corticosteroid isoenzyme of AP has been identified in dogs with exposure to increased endogenous or exogenous glucocorticoids. Because AP occurs as isoenzymes in these various tissues, the source of an isoenzyme or the location of the damaged tissue may be determined by electrophoresis and other tests that are performed in commercial or research laboratories. In young animals, most AP comes from osteoblasts and chondroblasts as a result of active bone development. In older animals, nearly all circulating AP comes from the liver as bone development stabilizes. The assays that are used for AP in a practice laboratory determine the total blood AP concentration. AP concentrations are most often used to detect cholestasis in adult dogs and cats. Because of wide fluctuations in normal blood AP levels in cattle and sheep, this test is not as useful for detecting cholestasis in these species.
Gamma Glutamyltransferase
· Elevated in
· Cholestasis
· Drugs
· Hepatocellular disease
. Decreased in
. Laboratory error
· Lipemia
· Hemolysis
Gamma glutamyltransferase (GGT or gGT) is sometimes referred to as gamma-glutamyl transpeptidase. GGT is found in many tissues, including renal epithelium, mammary epithelium (particularly during lactation), and biliary epithelium, but its primary source is the liver. Cattle, horses, sheep, goats, and birds have higher blood GGT activity than dogs and cats. Other sources of GGT include the kidneys, the pancreas, the intestine, and the muscle cells. The blood GGT level is elevated in patients with liver disease, especially in those with obstructive liver disease.
Other Tests of Liver Function
A large number of additional tests may help the veterinarian to develop a diagnosis and a prognosis. Many of these tests are biochemical tests that are associated with other organs as well, and thus they are not specific for liver disease. For example, blood glucose is generally associated with pancreatic function. However, the liver aids in the modulation of glucose values, and liver disease often results in hyperglycemia or hypoglycemia. Additional tests to assess liver function (e.g., dye excretion, caffeine clearance) are primarily performed only in research settings.
plasma protein functions
. Help form the structural matrix of all cells, organs, and tissues
· Maintain osmotic pressure
· Serve as enzymes for biochemical reactions
· Act as buffers in acid-base balance
· Serve as hormones
· Function in blood coagulation
. Defend the body against pathogenic microorganisms
· Serve as transport/carrier molecules for most constituents of plasma
protein assays
not specifically considered liver function tests though majoirty of plasma proteins are produced by the liver. Some are produced by the immune system (reticuloendothelial tissues, lymphoid tissues, and plasma cell). More than 200 plasma proteins exist. most assays are performed on total protein, albumin, and fibrinogen.
Total protein
elevated in
dehydration
hyperglobulinemia
hemolysis
lipemia
decreased in
hemorrhage
hypoalbuminemia
· Liver failure
· External plasma loss
· GI fluid loss
· Malassimilation
· Starvation
· Overhydration
· Glomerular loss
· Cancer cachexia
total plasma proteins include fibrinogen values, whereas total serum proteins measure everything else but. used for determine an animals hydration level. dehydrated have higher concentration.
hyperproteinemia
elevated protein due to dehydration.
hypoproteinemia
decreased total protein due to overhydration. used for edema, ascites, diarrhea, weight loss, hepatic and renal disease, and blood clotting problems.