(25.3.4) Physiology of Kidney & Step 1 Glomerular Filtration
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
How much is fluid is processed daily by the kidneys?
Approximately 180 L of fluid processed daily BUT → only 1.5 L of urine is formed
Kidney’s filter body’s entire plasma volume 60 times each day
Consume 20-25% of oxygen used by body at rest
Define Filtrate
Produced by glomerular filtration → basically blood plasma - proteins
Urine is produced from filtrate
Define Urine
<1% of original filtrate
Contains metabolic wastes and unneeded substances
List and Define the 3 Major Renal Processes
Three processes are involved in urine formation and adjustment of blood composition:
Glomerular filtration
Produces cell-free and protein-free filtrate
Tubular reabsorption
Selectively returns 99% of substances from filtrate to blood in renal tubules and collecting ducts
Tubular secretion
Selectively moves substances from blood to filtrate in renal tubules and collecting dicts
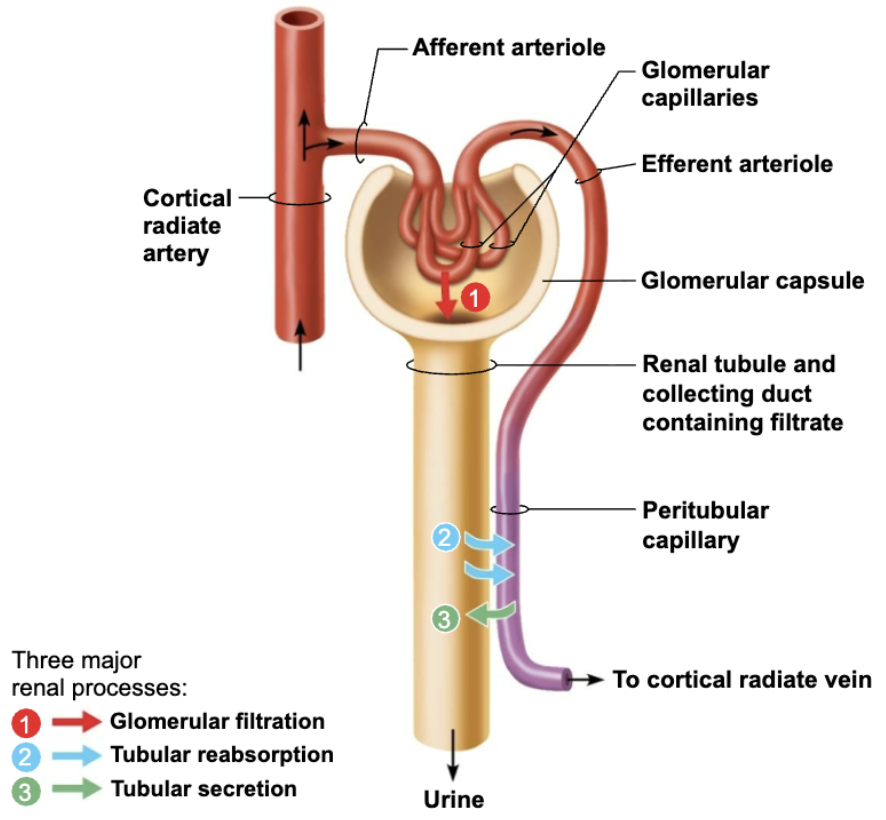
Explain Glomerular Filtration
A PASSIVE PROCESS (no metabolic energy required)
Hydrostatic pressure forces fluids and solutes through filtration membrane → glomerular capsule
NO reabsorption into capillaries of glomerulus occurs
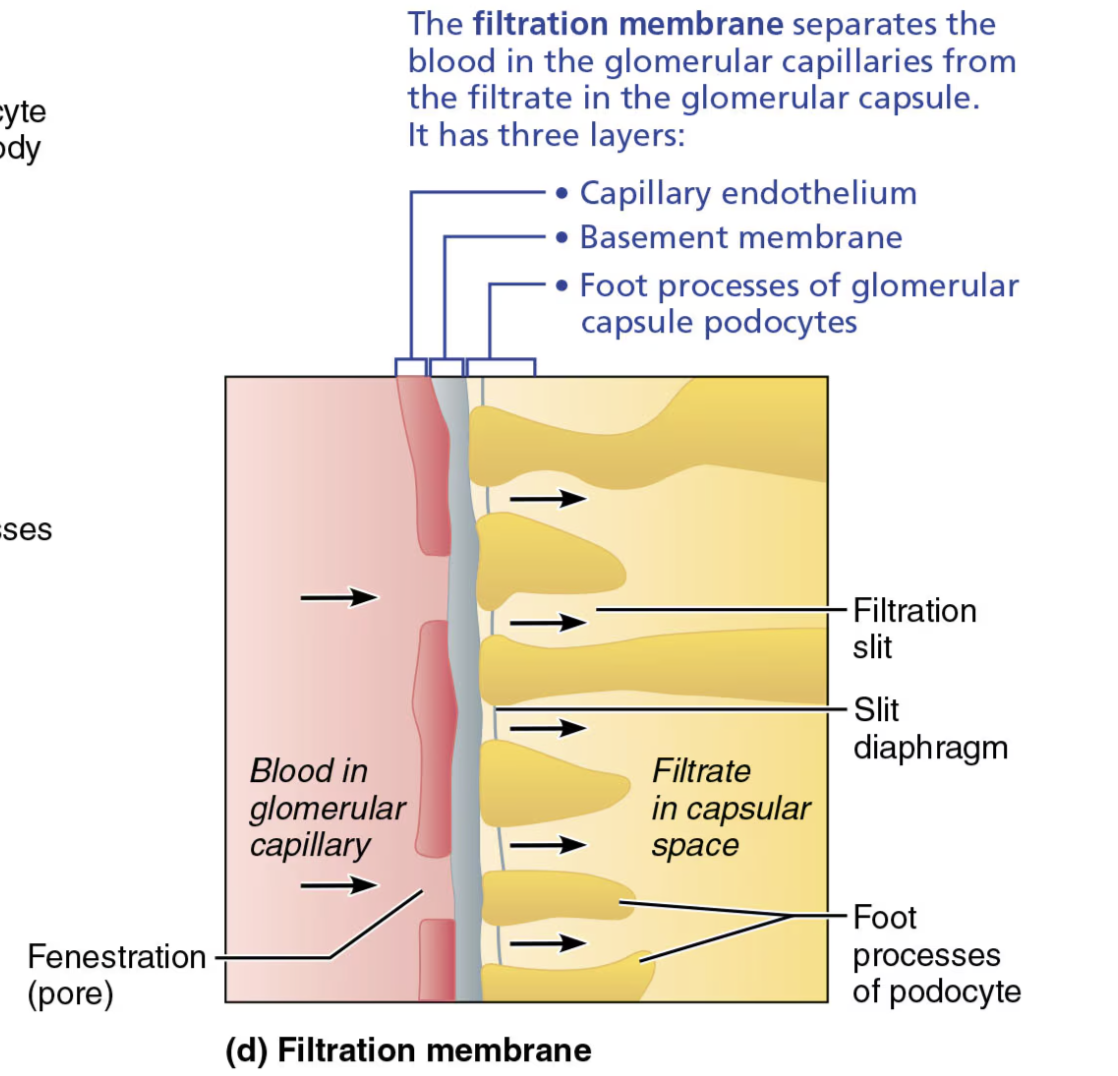
Role of the Filtration Membrane
STRUCTURE
Porous membrane between blood and interior of glomerular capsule
FUNCTION
Allow water and solutes smaller than plasma proteins to pass → NORMALLY NO CELLS CAN PASS
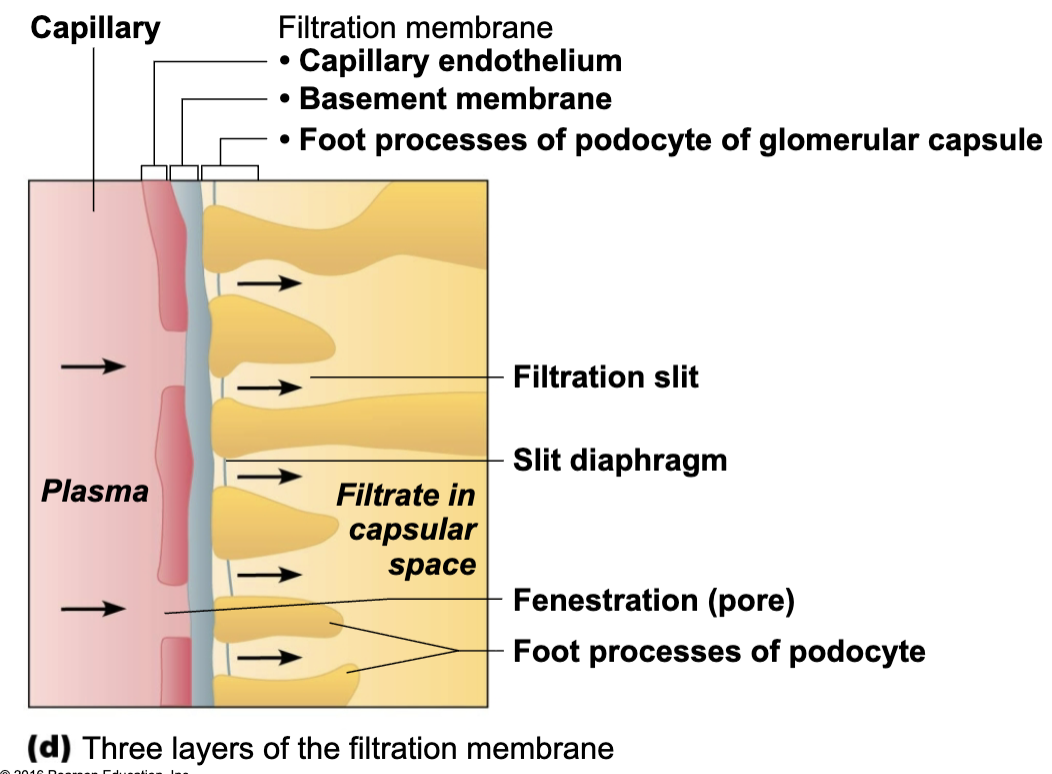
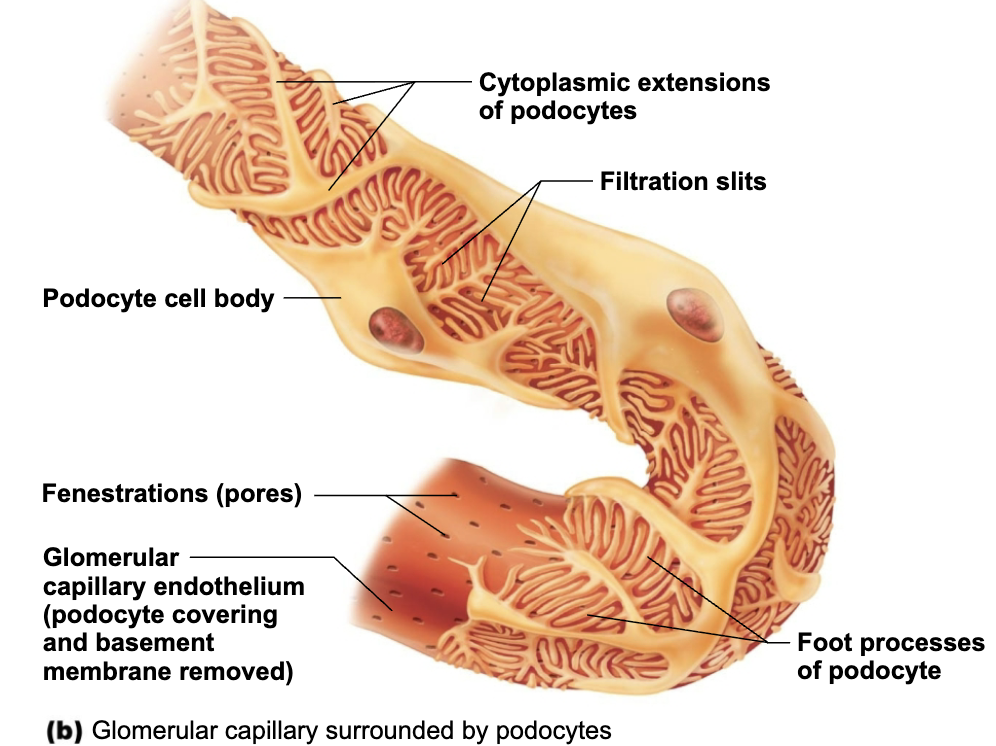
Name and Describe of the Layers of the Filtration Membrane
Fenestrated endothelium
of glomerular capillaries
Basement membrane
Fused basal laminae of two other layers
Foot processes of podocytes (Visceral layer of glomerular capsule)
with filtration slits → slit diaphragms repel macromolecules
Explain how the filtration membrane" “decides” to let substances into renal tube
Macromolecules “stuck” in filtration membrane are engulfed by glomerular mesangial cells
Allows molecules smaller than 3nm to pass
EX: Water, Glucose, Amino acids, Nitrogenous wastes
Plasma proteins remain in blood to maintain colloid osmotic pressure
Purpose of Plasma proteins in Blood
Plasma proteins remain in blood to maintain colloid osmotic pressure
Prevents loss of all water to capsular space
Proteins in filtrate indicate membrane problem
Explain how Fluid moves out of Glomerulus and into the Renal Tubule
Pressures that Affect Filtration
Outward Pressure → Forces that promote filtrate formation
Hydrostatic pressure in glomerular capillaries (HPgc) is essentially glomerular BP
Chief force pushing water, solutes out of blood
55 mmHg
Reason why HIGH is that efferent arteriole is a high-resistance vessel with a diameter smaller than afferent arteriole
Inward Pressure → Forces inhibiting filtrate formation
Hydrostatic pressure in capsular space (HPcs)
Filtrate pressure in capsule
15 mmHg
Colloid osmotic pressure in capillaries (OPgc)
“Pull” of proteins in blood
30 mmHg
Net Filtration Pressure (NFP) → sum of forces
55 mmHg forcing out minus 45 mmHg opposing = vet outward force of 10 mmHg
PRESSURE RESPONSIBLE FOR FILTRATE FORMATION
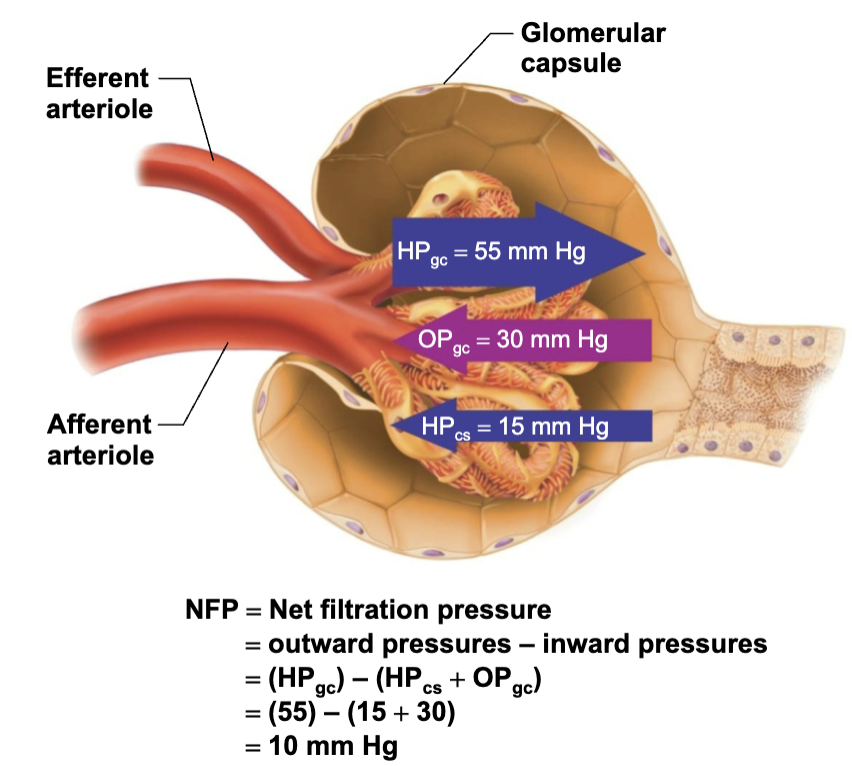
If the osmotic pressure in the glomerular capillaries increased from 28 mmHg to 35 mmHg due to dehydration, would net filtration increase or decrease?
→ Net filtration would decrease.
Explain Effect and Cause of Anuria
EFFECT
Abnormally low urinary output (less than 50ml/day)
CAUSE
May indicate that glomerular BP is too low to cause filtration
Renal failure and anuria can also result from situations in whicj nephrons stop functioning
EX: Acute nephritis, Transfusion reactions, and crash injuries
Define Glomerular Filtration Rate (GFR)
GFR = Volume of filtrate formed/minute by both kidneys
Normal = 120-125 ml/min
Name and Describe the Factors GFR is directly proportional to
Net Filtration Pressure (NFP)
Primary pressure is glomerular hydrostatic pressure
Total surface area available for filtration
Glomerular mesangial cells control by contracting
Filtration membrane permeability
Much more permeable than other capillaries
Role of GRS
Constant GRS is important as it allows kidneys to make filtrate and maintain extracellular homeostasis
The rate of kidney filtrate formation would normally be dependent upon all of the following factors except__________.
A.) systemic blood pressure
B.) filtration membrane integrity
C.) blood calcium level
D.) renal artery/arteriole diameters
→ C.) blood calcium level
Systemic blood pressure
Filtration membrane integrity
Renal artery/arteriole diameters
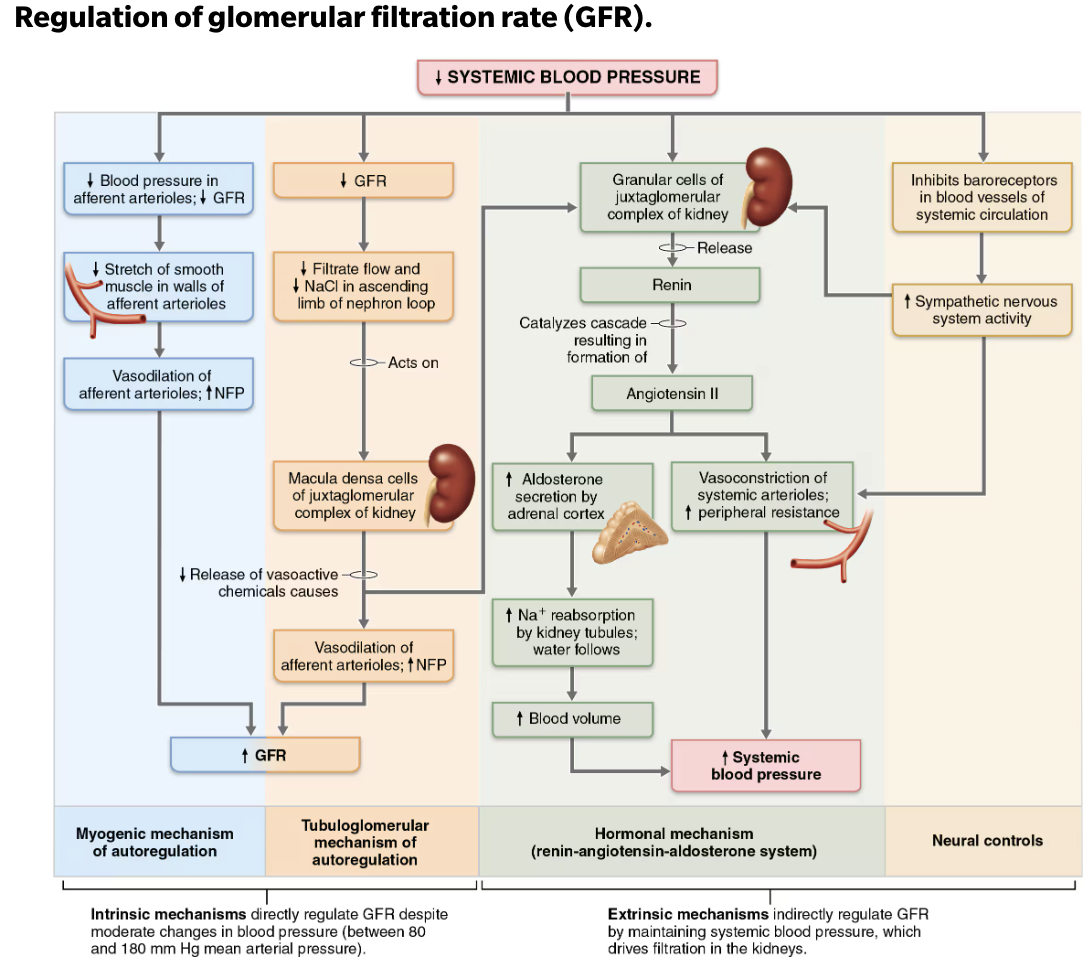
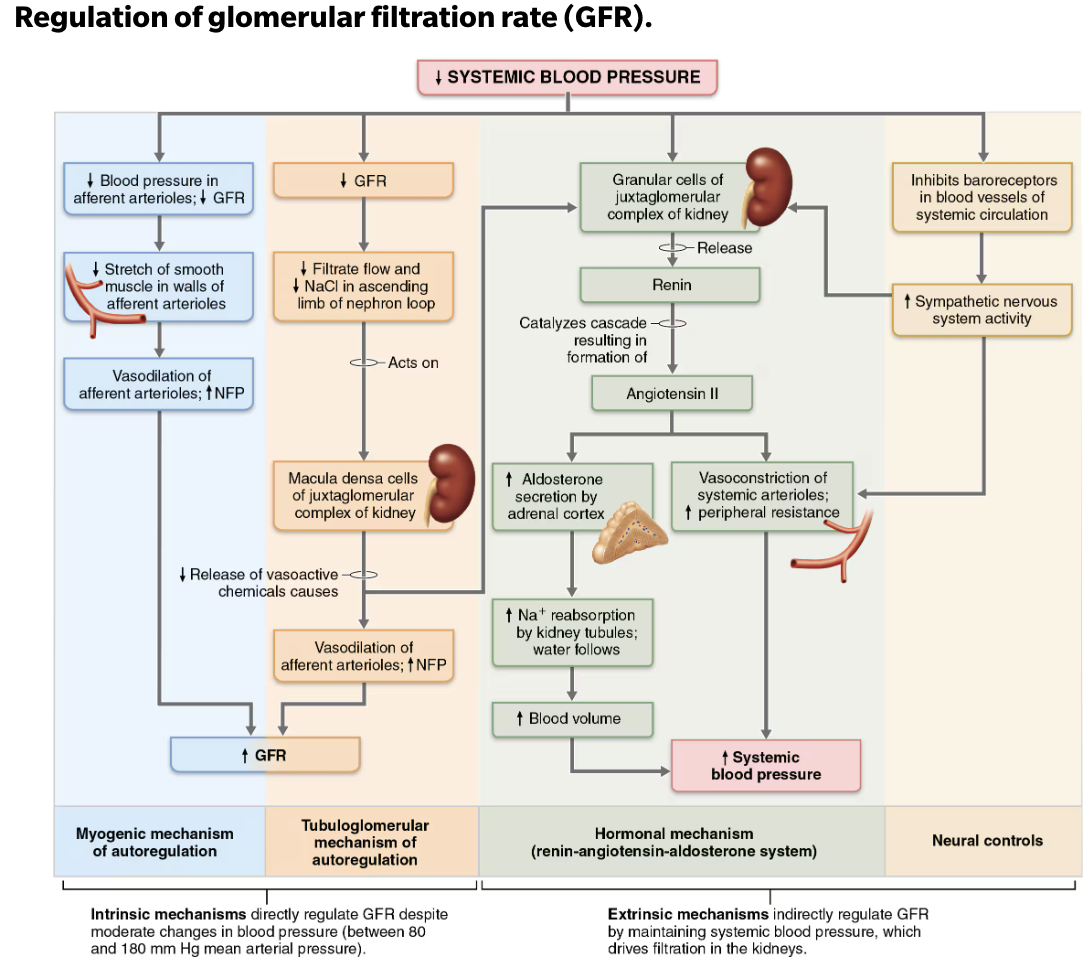
Name Two Types of Controls of GFR
Intrinsic controls→ maintain GFR in kidney
Constant GFR is important as it allows kidneys to make filtrate and maintain extracellular homeostasis
Renal auto-regulation
Extrinsic controls → maintain systemic BP
GFR affects systemic blood pressure
Nervous system and Endocrine mechanisms
T/F: Increased GFR causes increased urine output, which lowers blood pressure, and vice versa
→ TRUE
Define Intrinsic Controls
Maintains nearly constant GFR when MAP is in range of 80-180 mmHg
Auto-regulation ceases if out of that range
Two types of renal auto-regulation
Myogenic mechanism
Tubuloglomerular feedback mechanism
Explain how Myogenic Mechanism works to regulate glomerular filtration
Intrinsic Control
Local smooth muscle contracts when stretched:
INCREASED BP causes muscle to stretch, leading to constriction of afferent arterioles
Restricts blood flow into glomerulus
Protects glomeruli from damaging high BP
DECREASED BP causes dilation of afferent arterioles
Both help maintain normal GFR despite normal fluctuations in BP
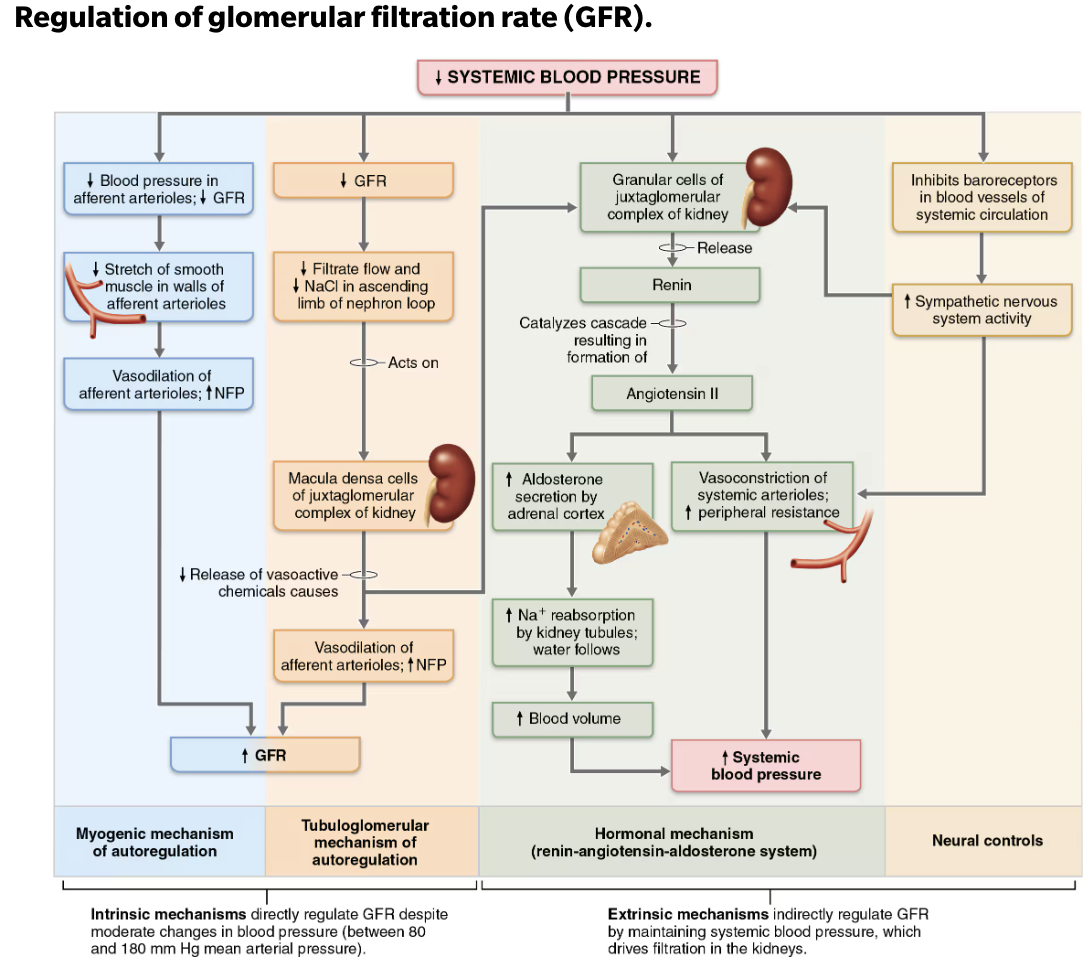
Explain how Tubuloglomerular Feedback Mechanism works to regulate glomerular filtration
Intrinsic Control
Flow-dependent mechanism directed by macula densa cells → Responds to filtrate NaCl concentration
If GFR INCREASES → filtrate flow rate INCREASES
Leads to DECREASED reabsorption time → causing HIGH NaCl levels in filtrate
Feedback mechanism causes constriction of afferent arteriole → which LOWERS NFP and GFR, allowing more time for NaCl reabsorption
Opposite mechanism for DECREASED GFR
When the macula densa detects an increase in NaCl concentration in the renal filtrate, what happens to the glomerular filtration rate (GFR)?
→ GFR decreases
Define Extrinsic Controls
Purpose is to regulate GFR to maintain systemic BP
Will OVERRIDE renal intrinsic controls if blood volume needs to be increased
Two types of renal auto-regulation
Sympathetic Nervous System
Renin-Angiotensin-Aldosterone Mechanism
Explain how Sympathetic Nervous System works to regulate glomerular filtration
Extrinsic Control
Under normal conditions @ rest
Renal blood vessels dilated
Renal auto-regulation mechanism prevail
Under abnormal conditions, such as extremely low ECF volume (low BP)
Norepinephrine is released by sympathetic nervous system and epinephrine is released by adrenal medulla causing
Systemic vasoconstriction → increases BP
Constriction of afferent arterioles → decrease GFR
Blood volume and pressure increases
Sympathetic Nervous System
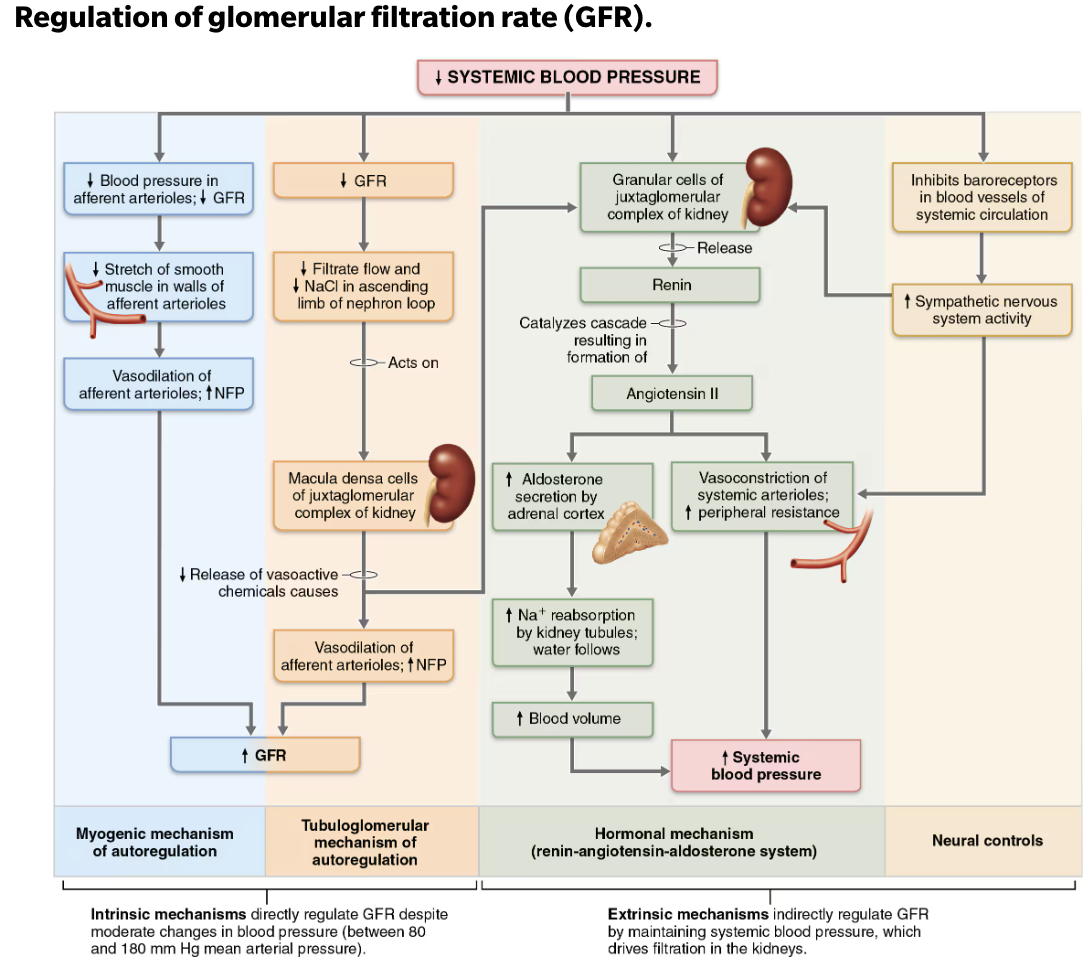
Explain how Renin-Angiotensin-Aldosterone Mechanism works to regulate glomerular filtration
Extrinsic Control
Main mechanism for increasing BP
Three pathways to renin release by granular cells
Direct stimulation of granular cells by sympathetic nervous system
Stimulation by activated macula densa cells when filtrate NaCl concentration is low
Reduced stretch of granular cells