Bone Neoplasms
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
130 Terms
What is the cell of origin of osteoma (benign)
Osteocyte
What are the categories of neoplasms?
Benign and malignant
Name the benign bone neoplasms
Osteoma
Osteoblastoma
Cementoblastoma
Name the malignant bone neoplasms
Osteosarcoma
Chondrosarcoma
Ewing sarcoma
What is the cell of origin of osteoblastoma?
Osteoblast
What is the cell of origin of cementoblastoma?
Cementoblast
What is the cell of origin of osteosarcoma?
Osteoblast
What is the cell of origin of Chondrosarcoma?
Chondroblast
What is the cell of origin of Ewing sarcoma?
Under debate; primitive neuroectodermal cells
What is an osteoma?
A benign bone tumor that continues to grow (vs. exostosis)

What are characteristics of osteoma?
Primarily involve the craniofacial skeleton such as paranasal sinuses

In which population would you find osteoma?
Young adults as asymptomatic, solitary lesions

If you have multiple osteoma, what is that called?
Gardner syndrome

Where would you find osteoma?
Mandibular body is most common but it can be found anywhere

What is the treatment of osteoma?
None if small and asymptomatic, conservative surgical excision for large and symptomatic

Which of the following is correct for osteoma?
Typically small, slow-growing and found in the skull
All of the following are part of Gardner syndrome EXCEPT
Cafe au lait spots
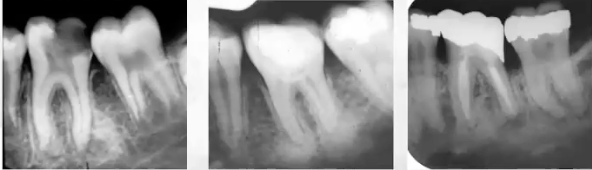
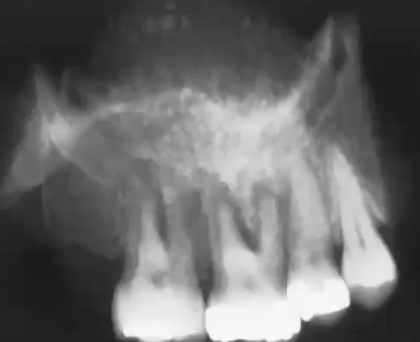
Pano of osteoma
Well circumscribed radiopaque lesion

Radiographic image of osteoma
What is the mode of transmission for Gardner Syndrome?
Autosomal dominant; mutation chromosome #5 (APC)
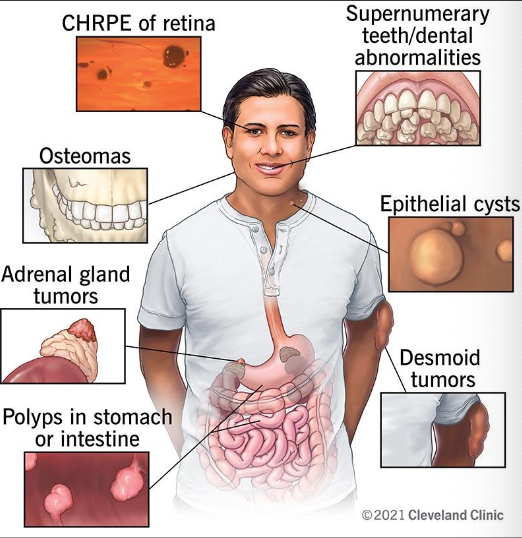
What are the clinical features of Gardner Syndrome
Colorectal (adenoma) polyps which can become malignant (100% if not treated)
Multiple osteoma
Epidermoid cyst of skin
20% have supernumerary teeth
Thyroid carcinoma
Pigmented ocular fundus (90%)
Prognosis: guarded, close follow up
Epidermoid cyst of skin seen in
Gardner Syndrome

Epidermoid cyst of skin
(Back)

Colorectal Polyps seen in Gardner Syndrome
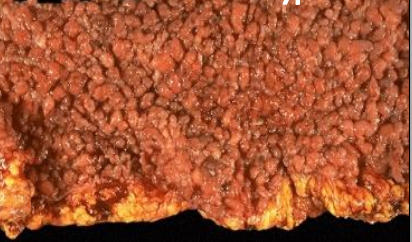
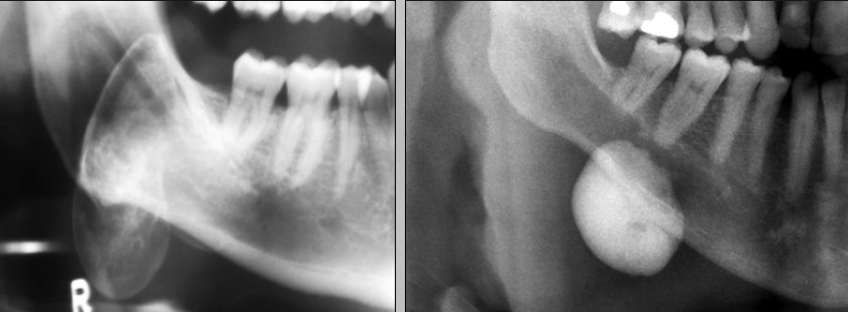
Pano of patient with gardner syndrome

Pano of patient with Gardner Syndrome has supernumerary teeth
Seen in 20% of patients and cleidocranial dysplasia (more common)

What is an osteoblastoma?
A benign bone tumor that arises from osteoblasts and is rare
What is the difference between an osteoid osteoma and osteoblastoma?
Osteoid osteoma is SMALLER than 2 cm, nocturnal and relieved by aspirin
Osteoblastoma is LARGER 2-4 cm and not relieved by aspirin, pain and swelling
In which demographic would you find osteoblastoma?
85% occur before age 30
Where would you find osteoblastoma?
Mostly in the posterior region over the anterior; and in the mandibular than the maxilla
What is the treatment for osteoblastoma?
Surgical excision
What would you look for radiographically in osteoblastoma?
Well-defined or ill-defined radiopaque lesion (can be mixed RO and RL)

Which of the following statements about osteoblastoma is FALSE
Relieved by aspirin

What is cementoblastoma
A benign odontogenic neoplasm of cementoblasts
In which demographic would you see cementoblastoma?
75% occur before the age of 30
Pain and swelling are present in 2/3

Where would you find cementoblastoma?
75% arise in the mandible, almost always in the molar/premolar region
Typically, only affect permanent teeth (especially 1st mandibular molars)

What are the radiographic features of cementoblastoma?
Radiopaque mass that is fused to one or more tooth roots
Outline of the root or roots is usually obscured
Surrounded by a thin radiolucent rim

What is the treatment of cementoblastoma?
Surgical extraction of the tooth and calcified mass
Recurrence is 20%

Which of the following is INCORRECT for cementoblastoma?
Radiolucent mass
What is ossifying fibroma?
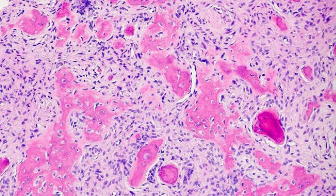
A true bone neoplasm with significant growth potential composed of fibrous tissue that contains a variable mixture of bone & cementum (central vs. peripheral)
—> Large tumors result in painless swelling


Where would you find ossifying fibroma?
Mandible > maxilla

What would you find radiographically in ossifying fibroma?
Well-defined, unilocular
Can be completely radiolucent, or more commonly mixed RL-RO
Depends on amount of calcified material
Root divergence or resorption of roots can occur
Characteristic downward bowing of the inferior cortex of the mandible
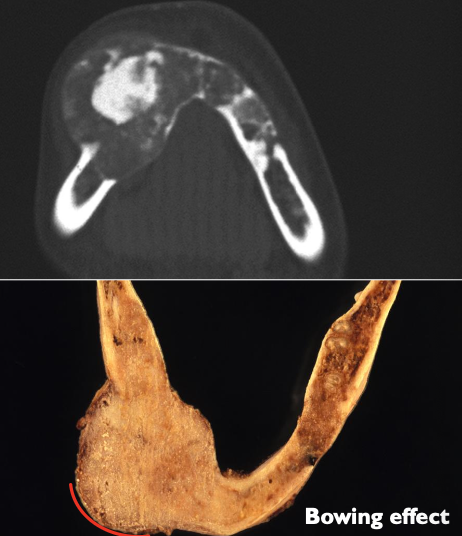
Histological image of ossifying fibroma

What is osteosarcoma?
A malignant bone neoplasm; there are two kinds: primary, and secondary such as Paget disease or radiation
In which demographic would you find osteosarcoma
M > F
Bimodal age distribution
Between 10-20 (more common)
After 50

Where might you find osteosarcoma?
Distal femur and proximal tibia
Jaws 8% of all osteosarcomas, occur at a later age (30s)
Max = Mand (posterior)
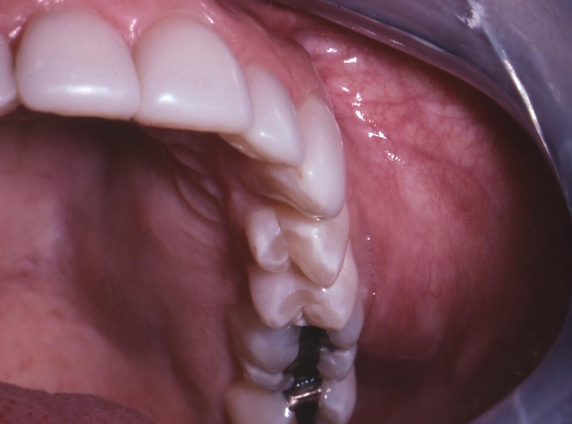

Clinical features of osteosarcoma
Swelling and pain, paraesthesia, loosening of teeth

What is the treatment of osteosarcoma?
Surgery and chemotherapy
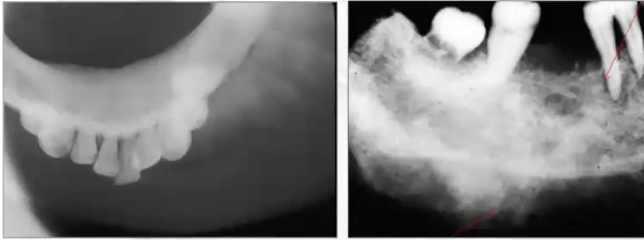
What are some radiographic features of osteosarcoma?
May be RO, RL or mixed
Ill-defined (MOTH EATEN) peripheral borders
Spiking resorption causing tapered roots
Codman’s triangle
Sunburst appearance (25%)


What is codman’s triangle?
Triangular elevation of periosteum

In which condition do you see Codman’s triangle
Osteosarcoma

Which radiograph will be able to best show osteosarcoma?
A sunburst appearance (d/t bony projections on the surface of the lesion) would be best appreciated using an occlusal x-ray

What is an important early finding of osteosarcoma?
Symmetrical widening of PDL space around one or more teeth
Which of the following radiographic features is NOT typically associated with osteosarcoma?
Radiolucent halo rim

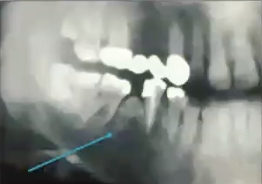
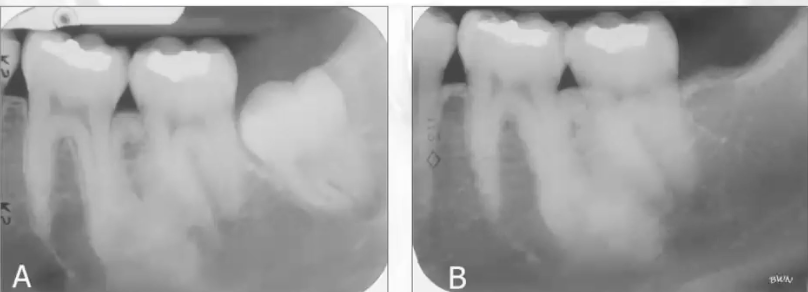
What is this pano showing?
Expansion, subtle sunburst appearance, spiking resorption of 1st molar; seen in osteosarcoma

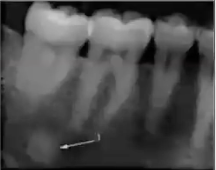
What is this PA showing?
Widening of PDL seen in osteosarcoma
What is this PA showing?
Calcification filling the sinus, widened PDL, spiked appearance of roots seen in osteosarcoma

What is this PA showing?
Osteosarcoma resembling focal cemento-osseous dysplasia
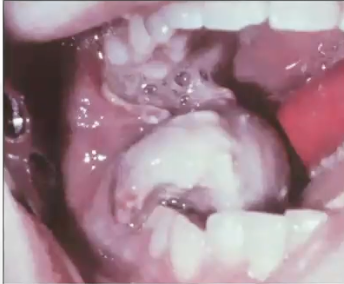
What is this image showing?
Bone destruction seen in osteosarcoma - cortical plate is destroyed
What are some benign features of osteosarcoma?
Uninterrupted
Solid
Continuous
What are some malignant features of osteosarcoma?
Interrupted
Onion skin
Sunburst (sun ray)
Codman’s

What is chondrosarcoma
A malignant bone tumor of cartilage
What is the most common location of chondrosarcoma?
Long bones (3% arise in the head and neck)

What are some clinical features of chondrosarcoma?
Painless mass or swelling of jaw is most common
Extensive infiltration, poorly defined borders, RL and RO varies
± root resorption
Symmetrical PDL widening

What is the treatment of chondrosarcoma?
Complete resection (resistant to chemo and radiation)

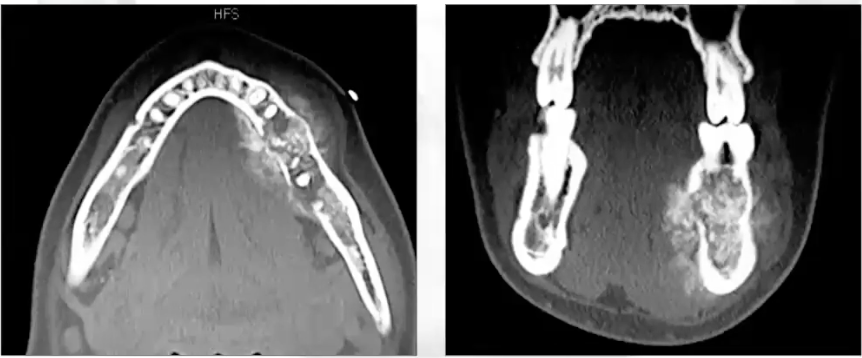
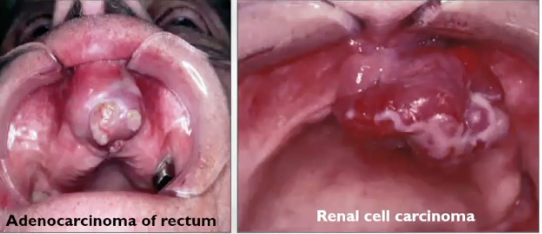
What is this image showing?
Huge expansion and swelling in left mandible area seen in chondrosarcoma

What is this radiograph showing
Mixed radiolucent and radiopaque lesion seen in chondrosarcoma; lacks a well-defined border
What is ewing sarcoma?
A primary malignant tumor of bone, it is highly lethal and known to metastasize (it is the 3rd most common osseous neoplasm)
What gender does ewing sarcoma affect the most?
White male, 80% less than 20 years old
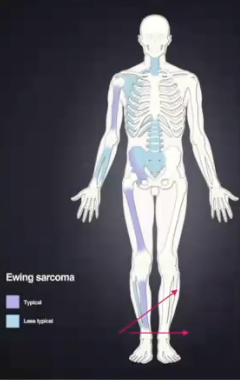
Where would you find ewing sarcoma?
Long bones, jaws are only involved 2% mand > max
What are some clinical features of ewing sarcoma?
Intermittent pain
Swelling
Loosening of teeth

What are some radiographic features of ewing sarcoma?
Irregular defined borders (moth eaten)
Onion skin periosteal reaction like “Garre’s osteomyelitis”
Sunray appearance “like osteosarcoma”
What is the treatment for ewing sarcoma?
Combined surgery, chemo, and radiation
What is Post Radiation Bone Sarcoma?
Sarcoma arising in a bone that has been previously subjected to radiation therapy and is a well-recognized phenomenon
What is the most common type of post radiation bone sarcoma?
Osteosarcoma (50%)
When do post radiation bone sarcoma develop?
Postirration sarcomas may develop 3 years after radiation, but the average is 15 years after therapy
What is metastatic disease?
It is more common of a carcinoma than a sarcoma
What is the difference between carcinoma and sarcoma?
Sarcoma = origin is mesenchymal stem cells (bone, cartilage, adipose tissue, fat, skeletal muscle, smooth muscle)
Carcinoma = origin of the epithelium (most common is squamous cell carcinoma)
If metastatic disease does occur, where will it be?
2/3 are in bone (80% mandible > maxilla)
1/3 in soft tissue (most commonly gingiva)
Common origin of gnathic metastasis:
Breast
Lung
Thyroid
Prostate
Kidney
What are some common symptoms of metastatic disease?
Pain
Swelling
Loosening of teeth
Paresthesia (numb chin)

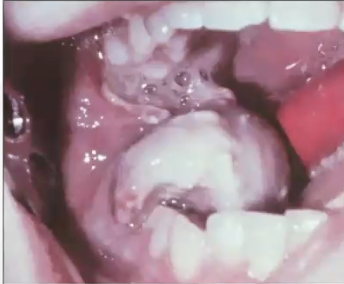
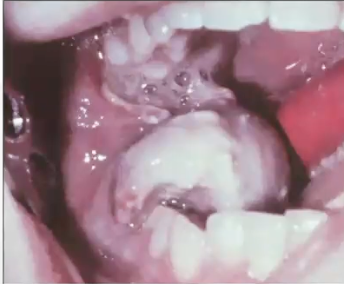
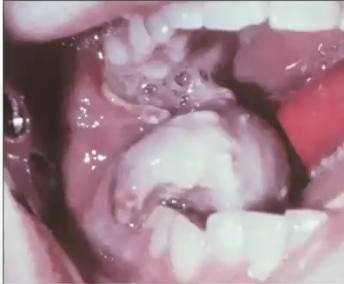
What is this
Metastatic nasopharyngeal carcinoma
What is this?
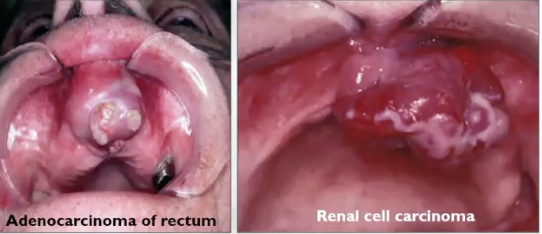
Widening of PDL and ill-defined RL seen in metastatic disease

What is this?
Metastatic small cell carcinoma of the lung
What is this?
Periapical granuloma (not to be confused with metastatic small cell carcinoma of the lung)
Which of the following statements about metastatic disease to the head and neck is FALSE?
Most common location is gingiva

What is focal osteoporotic bone marrow defect?
Area of hematopoietic marrow that produces a radiolucency

What is the cause of focal osteoporotic bone marrow defect?
Unknown, incidental finding

What is the incidence of focal osteoporotic bone marrow defect?
75% in adult women, typically in posterior mandible

What can focal osteoporotic bone marrow defect be confused with?
Intraosseous neoplasm

What are some clinical features of focal osteoporotic bone marrow defect?
No jaw expansion
It is NOT pathology, but the x-ray features may look like it
Multilocular radiolucency
May minic botryoid cyst, OKC, ameloblastoma

What is the treatment for focal osteoporotic bone marrow defect?
None, bx to rule out pathology
What is idiopathic osteosclerosis?
Focal area of increased radiodensity that is of unknown cause and cannot be attributed to anything else
Where might you find idiopathic osteosclerosis?
90% in the mandible (molar/premolar) and the tooth is VITAL
What are some clinical and radiographic features of idiopathic osteosclerosis?
No decay or pulpal involvement, tooth is sound
Sometimes associated with a tooth
Asymptomatic
No cortical expansion
Radiolucent lesion, no radiolucent rim
What is the treatment for idiopathic osteosclerosis?
Follow-up
What is this?
Idiopathic osteosclerosis after 10 years follow-up
What should be included in your differential diagnosis for idiopathic osteosclerosis?
Condensing osteitis, which is associated with decay or pulpal involvement (infection)
Focal cemento-osseous dysplasia, which can have a radiolucent rim + clinical features (gender, age, location)
Do not confuse with cementoblastoma, which will be fused with the tooth and have a radiolucent halo
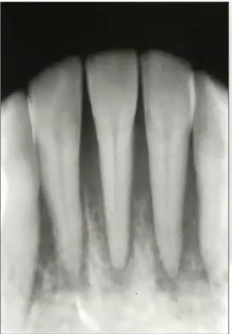
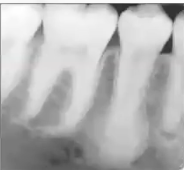
Radiographic example of idiopathic osteosclerosis
Tooth is sound; bone scar enostosis
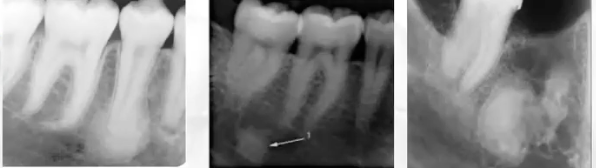
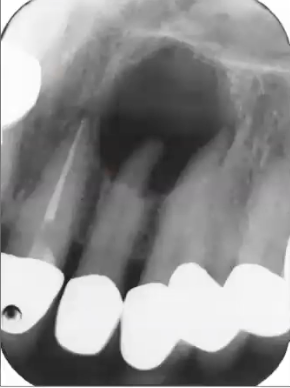
Radiographic example of condensing osteitis
Focal (chronic) sclerosing osteomyelitis —> large restoration, caries, and infection