PEDS Exam 2
1/270
Earn XP
Description and Tags
CU NSG 3030
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
271 Terms
Environmental factors for kids getting cancer
Radiation (xrays, mri)
turf that is cancer causing chemicals
foods
Genetic conditions that predispose kids to cancer
down syndrome
family history
Is there a genetic link?
—
Childhood cancers: _________ embryonic origin, no strong _____________ link, routine screening ____ recommended, few _______________ strategies, metastatic disease at __________, more responsive to treatment, .70% ______ rate
primitive, environmental, not, preventive, diagnosis, cure
Cancers demonstrating the greatest improvement in survival rates:
acute leukemia
CNS tumors
non-Hodgkin’s lymphoma
bone tumors
Wilms tumor
What’s behind the improved outcomes?
COG, POG, clinical trials w/ cancer treatment, transition to multi-modal therapy, provide data to:
improve therapy
decreased morbidity
increase survival of children w/ cancer
Cancers of blood and lymph system
leukemia (all-acute lymphoid leukemia, AML-acute myelogenous leukemia)
lymphomas
Hodgkin’s disease
non-Hodgkin’s lymphoma
Nervous system tumors
neuroblastoma
brain tumors
astrocytoma
medulloblastoma
brainstem glioma
ependyoma
Bone tumors
osteogenic sarcoma
Ewing sarcoma
(PNET) primitive neuroectodermal tumor
Solid tumors
Wilm’s tumor
Rhabdomyosarcoma
Retinoblastoma
Testicular tumors
Warning signs of cancer in children: C.H.I.L.D.R.E.N.
—
Lab/Diagnostic test
CBC (complete blood count)
CMP/BMP
LP (lumbar puncture)
What might a LP test be looking for?
testing cerebral spinal fluid for cancer cell findings —> CSF: finding wbc
child should be under anesthesia
dr might push chemotherapy into their csf space
profolacitally
CBC might look like _____ for a cancer pt.
very low ______ count
Skin findings:
bulging Fontenelle
bruising/petechia
pallor/pale
rash
Heart findings:
increased HR (lump adding pressure)
increased BP (pump harder)
HEENT findings:
swollen lymph nodes
depends on where cancer is…
trouble swallowing
anorexia
dehydration
lungs findings:
Neuro findings:
balance difficulty
difficulty focusing
seizures
double/poor vision
modes of therapy:
surgery
chemotherapy
radiation
biologic response modifiers
bone marrow transplant
Two specific goals of surgery:
1) obtain a biopsy
2) remove all traces of tumor
Surgery may be ________ when cancer has metastasized or advanced. Most used in ______ tumors. Most successful in ____________ tumors.
palliative, solid, encapsulated
Encapsulated tumor has what around it?
cells, they contain it
Chemotherapy can be classified according to the:
primary mechanism of action
Alkylating chemotherapy: 3 types
cyclophosphamide
ifosfamide
cisplatin
Antimetabolites chemotherapy: 2 types
methotrexate
mercaptopurine
plant alkaloids chemotherapy: 2 types
vincristine
vinblastine
Antitumor antibioticsvchemotherapy: 2 types
doxorubicin
daunomycin
Adrenal/gonadal hormones chemotherapy: 2 types
prednisone
dexamethasone
others chemotherapies: 1 type listed
L-asparaginase
many chemotherapeutic agents are ________
vesicants
extravasation can occur if chemotherapeutic agent _______ into surrounding tissue
infiltrates
infusion should be stopped ____________ with any sign of infiltration (pain, stinging, swelling, redness)
immediately
What is a potentially fatal complication of administering chemotherapeutic agents?
anaphylaxis
Anaphylaxis is characterized by:
urticaria
angioedema
flushing
rashes
difficulty breathing
hypotension
n/v
L-asparaginas, bleomycin, cisplatin, etoposide have known ____________ potential
anaphylactic
If a pt is receiving chemo and begins to have these symptoms, what would you do first?
STOP IMMEDIATELY MED/remove IV/PORT
inform physician
When giving meds with known anaphylactic potential
Observe VS closely (q15 minutes for at least an hour)
Emergency equipment at the bedside
Emergency drugs readily available
If a reaction is suspected
Discontinue medication immediately
Flush/aspirate IV line
Ongoing monitoring of VS
Notify MD
Who has published comprehensive guidelines for safe practice issues related to administration of chemotherapy?
The Oncology Nursing Society
Nurses must use safeguards to protect themselves
Prepare drugs in properly ventilated room
Wear disposable gloves and protective clothing
Use precaution to prevent any physical contact with the chemotherapeutic agents
Nurses must know how to care for and maintain central venous access devices
Central line
Port-a-cath
Children might become _______ to port. (think: “Mr. Tubey”)
attached
Radiotherapy
can be used in conjunction w/ chemotherapy and surgery
can be used for curative purpose and for palliative
radiotherapy is _________. Acute side effects are caused by the damage to _________________ cells.
cytotoxic, proliferating
Biologic theerapy:
some may stimulate the body’s immune system (immunotherapy or biological response modifiers therapy)
may use antibodies to target cancer cells directly
may interfere with specific molecules related to tumor growth (targeted therapies)
Goals of treatment
cure or free from disease
developmentally appropriate care
maintain normalcy as much as possible
Complications of treatment
acute adverse effects
pediatric oncologic emergencies
long term effects
managing adverse effects of treatment
head
alopecia
mucositis: ulcerations/sloughing of mucosa anywhere along the GI tract
Pain
local anesthetic w/out alcohol (Benadryl/Maalox) rinse
do not use viscous lidocaine which may depress gag reflex and increase risk of aspiration
morphine PCA may be required
managing adverse effects of treatment
risk of infection:
must maintain excellent oral care
use toothette/soft sponge toothbrush
peridex is effective against candidal and bacterial infections
rectal temperatures and suppositories are avoided for pts with rectal ulcers
alopecia
baldness, fingernails, skin regeneration lost
cancer pts will enjoy sucking on candy, why?
dry mouth
note: chocking hazard. give appropriate to age
Nausea/vomiting can occur after chemotherapy administration or after radiation. What med would you give?
Intervention: Zofran (antiemetic) 30 min-1 hour prior to chemo and every 2, 4, or 6 hours for 24 hours after chemo
GI tract adverse effects of chemotherapy treatment:
N/V/D
constipation-lack of motility or neuropathy
anorexia
anorexia is a ________ effect related to cancer that is nonspecific, aversion to ____from n/v during treatment, response to stress in the __________, depression
physical, food, environment
depression
Intervention: Ongoing assessment of nutritional status
Supplement with high-protein and high-calorie foods
Hyperalimentation as needed to maintain optimal nutritional status
Pediatric oncological emergencies
acute tumor lysis syndrome
hyperleukocytosis
obstruction
overwhelming infection
Direct result of rapid release of _________ contents during death of malignant cells as a result of ________
Usually occurs during ______ ________
Causes ______ abnormalities
Hyperuricemia
Hypocalcemia
Hyperphosphatemia
Hyperkalemia
intracellular, treatment, initial treatment, metabolic
Crystallization of ___ ____ in renal tubules can lead to ___ _____failure and _____
uric acid, acute renal, death
hyperkalemia = ?
high K (potassium)
potassium affects the heart
Medication to reduce uric acid formation and promote excretion of by-products of purine metabolism
Allopurinol

______ Anatomy and Physiology of ____________ system
Bone, Hematological
Coagulation Cascade
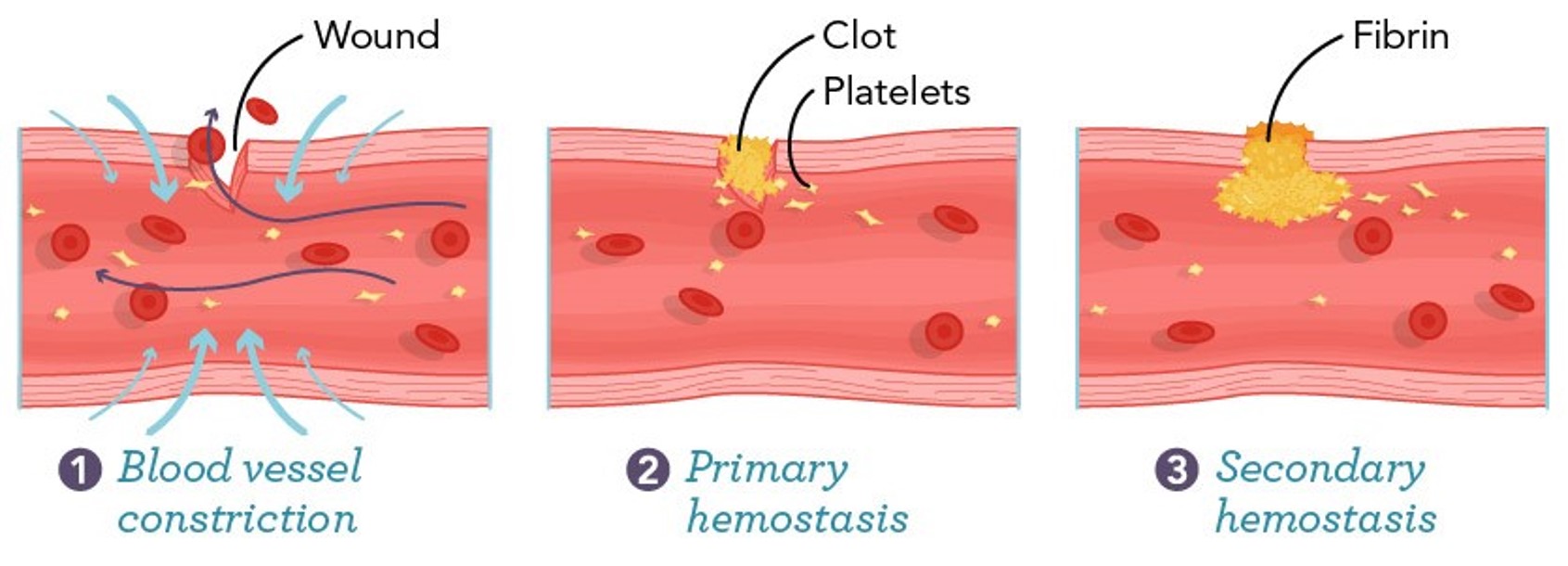
Three steps of the coagulation cascade
blood vessel constriction
primary hemostasis
secondary hemostasis
More detailed order of coagulation cascade (hemostatic cascade) DO NOT NEED TO MEMORIZE :)
injury site
blood vessels constrict
platelets adhere
platelets activate and aggregate
clotting factors are triggered
prothrombin converts to thrombin
fibrin converts to fibrinogen (weak plug - primary hemostasis)
fibrinogen stabilized (clot stabilized bleeding controlled - secondary hemostasis)
Three dif anemias
iron deficiency anemia
sickle cell anemia
beta-thalassemia (Cooley Anemia)
Iron deficiency anemia
Iron Deficiency Anemia
Cause:
Insufficient iron intake (dietary deficiency)
Increased iron needs (pregnancy, growth spurts)
Blood loss (menstruation, gastrointestinal bleeding)
Malabsorption (celiac disease, gastric surgery)
Symptoms:
Fatigue and weakness
Pale skin
Shortness of breath
Dizziness or lightheadedness
Cold hands and feet
Brittle nails
Headaches
For diagnosis and treatment, consult a healthcare professional.
sickle cell anemia
Sickle Cell Anemia
Cause: Sickle cell anemia is caused by a mutation in the HBB gene, which encodes the beta-globin subunit of hemoglobin. This mutation leads to the production of abnormal hemoglobin known as hemoglobin S (HbS).
Symptoms:
Anemia (fatigue, weakness)
Episodes of pain (sickle cell crises)
Swelling in hands and feet
Frequent infections
Delayed growth in children
Vision problems
For management, regular medical care and treatments are essential.
beta-thalassemia (cooley anemia)
Causes of Beta-Thalassemia (Cooley Anemia)
Genetic mutations in the HBB gene affect hemoglobin production.
Inherited in an autosomal recessive pattern.
Symptoms of Beta-Thalassemia
Fatigue and weakness.
Pale or yellowish skin (jaundice).
Shortness of breath.
Enlarged spleen and liver.
Bone deformities, especially in the face and skull.
Delayed growth and development in children.
Iron Deficiency Anemia: pathophysiology
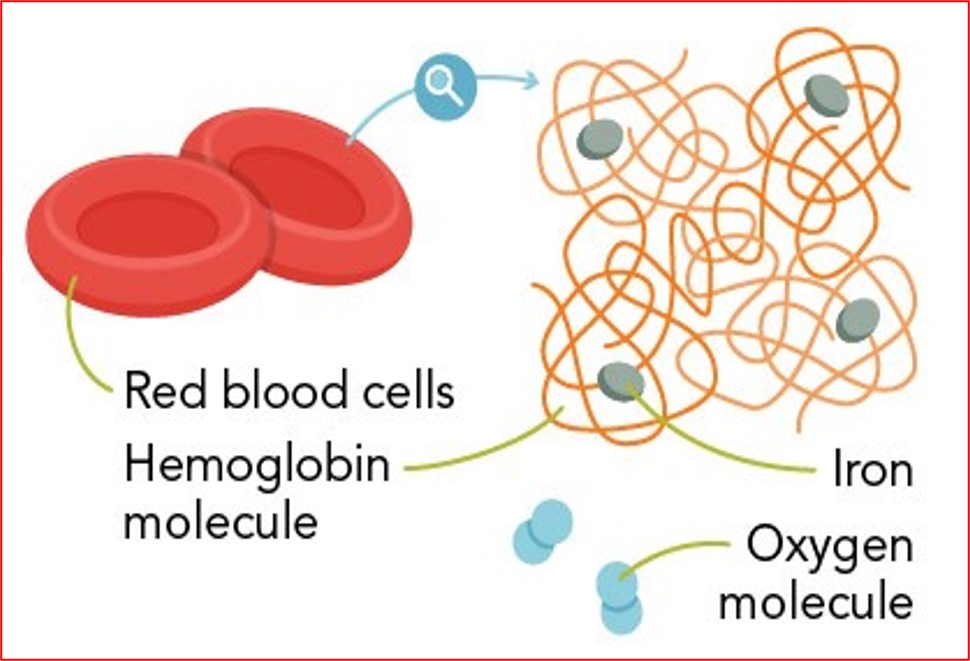
RBCs w/ hemoglobin and iron
Etiology of IDA
infants 9-24 mths
older children
Risk factors of IDA
prenatal
infancy
childhood
adolescents
epidemiology of iron decicient anemia
Epidemiology of Iron Deficiency Anemia
Prevalence: Affects approximately 1.62 billion people globally, particularly in developing countries.
Risk Groups:
Pregnant women
Infants and young children
Adolescents
Vegetarians and vegans
Causes:
Inadequate dietary intake
Malabsorption disorders
Chronic blood loss (e.g., menstruation, gastrointestinal bleeding)
Geographic Variation: Higher rates in regions with poor nutrition and limited access to healthcare.
Key Statistics
Most common nutritional deficiency worldwide.
Significant impact on cognitive and physical development in children.
Clinical presentation of IDA
common manifestations
additional manifestations
common manifestations of iron decicient anemia
Common manifestations of iron deficiency anemia include:
Fatigue and weakness
Pale skin and mucous membranes
Shortness of breath
Dizziness or lightheadedness
Cold hands and feet
Brittle nails
Headaches
Restless legs syndrome
Increased heart rate
If you suspect iron deficiency anemia, consult a healthcare professional for diagnosis and treatment.
Lab testing and diagnostic testing of IDA
complete blood count
additional testing
expected CBC findings for iron decicient anemia
Expected CBC Findings for Iron Deficiency Anemia
Hemoglobin (Hb): Decreased
Hematocrit (Hct): Decreased
Mean Corpuscular Volume (MCV): Decreased (microcytic)
Mean Corpuscular Hemoglobin (MCH): Decreased
Mean Corpuscular Hemoglobin Concentration (MCHC): Decreased
Red Cell Distribution Width (RDW): Increased
Reticulocyte Count: Often decreased or normal
These findings indicate a reduction in red blood cell production and size due to insufficient iron.
additional testing for iron decifient animia (besides cbc)
Additional Testing for Iron Deficiency Anemia
Serum Ferritin: Measures stored iron in the body.
Serum Iron: Assesses the amount of circulating iron.
Total Iron-Binding Capacity (TIBC): Evaluates the blood's capacity to bind iron with transferrin.
Transferrin Saturation: Percentage of transferrin that is saturated with iron.
Reticulocyte Count: Indicates bone marrow response to anemia.
Peripheral Blood Smear: Examines the shape and size of red blood cells.
treatment and therapies for iron deficiency anemia
Treatment and Therapies for Iron Deficiency Anemia
Iron Supplements: Oral iron supplements (ferrous sulfate, ferrous gluconate) are commonly prescribed.
Dietary Changes: Increase intake of iron-rich foods (red meat, poultry, fish, lentils, beans, spinach).
Vitamin C: Consuming vitamin C-rich foods (citrus fruits, tomatoes) can enhance iron absorption.
Intravenous Iron: For severe cases or when oral supplements are ineffective.
Address Underlying Causes: Treat any underlying conditions causing the deficiency (e.g., gastrointestinal bleeding).
Regular Monitoring: Follow-up blood tests to monitor hemoglobin and iron levels.
iron deficiency anemia effect on overal health
Iron Deficiency Anemia and Overall Health
Iron deficiency anemia can lead to:
Fatigue: Reduced oxygen transport causes tiredness.
Weakness: Decreased energy levels affect daily activities.
Cognitive Impairment: Impacts concentration and memory.
Immune Function: Increased susceptibility to infections.
Heart Problems: Can lead to rapid heartbeat or heart failure in severe cases.
Addressing iron deficiency is crucial for maintaining overall health.
considerations for the pediatric population (concerning iron deficiency anemia)
Considerations for Pediatric Population Regarding Iron Deficiency Anemia
Age-Specific Needs: Infants and toddlers require higher iron intake due to rapid growth.
Dietary Sources: Encourage iron-rich foods (e.g., meat, beans, fortified cereals).
Absorption Factors: Vitamin C enhances iron absorption; avoid calcium-rich foods during iron intake.
Screening: Regular screening for at-risk populations (e.g., premature infants, low-income families).
Supplementation: Consider iron supplements if dietary intake is insufficient, under medical guidance.)
Dietary recommendation of iron (when iron deficient)
Causes of Iron Deficiency Anemia
Inadequate dietary intake of iron
Blood loss (e.g., menstruation, gastrointestinal bleeding)
Increased iron requirements (e.g., pregnancy, growth spurts)
Malabsorption disorders (e.g., celiac disease)
Symptoms
Fatigue and weakness
Pale skin
Shortness of breath
Dizziness or lightheadedness
Cold hands and feet
Additional Testing
Serum ferritin
Serum iron
Total iron-binding capacity (TIBC)
Transferrin saturation
Dietary Recommendations
Consume iron-rich foods: red meat, poultry, fish, lentils, beans, tofu, and fortified cereals.
Pair with vitamin C sources (e.g., citrus fruits) to enhance absorption.
self-care skills for iron deficiency anemia
Self-Care Skills for Iron Deficiency Anemia
Dietary Changes: Increase intake of iron-rich foods (e.g., red meat, beans, lentils, spinach).
Vitamin C: Consume vitamin C-rich foods (e.g., citrus fruits) to enhance iron absorption.
Avoid Inhibitors: Limit intake of calcium and tannins (found in tea and coffee) during iron-rich meals.
Supplements: Consider iron supplements as advised by a healthcare provider.
Regular Check-ups: Monitor iron levels through blood tests as recommended.
Sports concern for anemia
bruising/bleeding
Promoting social and personal development for IDA
play
socialization
effected by limiations
social limitaions of iron deficient anemia
Social Limitations of Iron Deficient Anemia:
Fatigue and Weakness: Affected individuals may struggle with daily activities, impacting work and social interactions.
Stigma: There may be misconceptions about the condition, leading to social isolation.
Economic Impact: Increased healthcare costs and potential loss of income due to illness.
Educational Challenges: Students may face difficulties in concentration and performance in school.
Mental Health: Increased risk of anxiety and depression due to chronic health issues.
Client education for iron deficiency anemia
Causes of Iron Deficiency Anemia
Inadequate dietary intake of iron
Blood loss (e.g., menstruation, gastrointestinal bleeding)
Increased iron requirements (e.g., pregnancy, growth spurts)
Malabsorption disorders (e.g., celiac disease)
Symptoms
Fatigue and weakness
Pale skin
Shortness of breath
Dizziness or lightheadedness
Cold hands and feet
Brittle nails
Additional Testing
Serum ferritin
Serum iron
Total iron-binding capacity (TIBC)
Transferrin saturation
Dietary Recommendations
Increase intake of iron-rich foods: red meat, poultry, fish, beans, lentils, tofu, spinach, and fortified cereals.
Pair iron sources with vitamin C-rich foods (e.g., citrus fruits) to enhance absorption.
Client Education
Importance of adhering to dietary recommendations.
Understanding symptoms and when to seek medical help.
Discussing potential side effects of iron supplements.
Importance of follow-up testing to monitor iron levels.
What foods are rich in iron?
Foods Rich in Iron
Red Meat: Beef, lamb, and pork
Poultry: Chicken and turkey
Seafood: Oysters, clams, and sardines
Legumes: Lentils, beans, and chickpeas
Nuts and Seeds: Pumpkin seeds, cashews, and almonds
Leafy Greens: Spinach, kale, and Swiss chard
Fortified Foods: Cereals and bread
Dried Fruits: Apricots, prunes, and raisins
These foods can help increase iron intake, essential for blood health.
How would you explain the importance of eating iron rich foods to a parent/guardian of a child who has begun eating solid foods?
Eating iron-rich foods is crucial for a child's growth and development, especially as they transition to solid foods. Iron supports healthy brain development, boosts the immune system, and helps prevent iron-deficiency anemia, which can lead to fatigue and developmental delays. Foods like lean meats, beans, spinach, and fortified cereals can provide essential iron. Pairing these with vitamin C-rich foods enhances iron absorption. Ensuring a balanced diet will promote overall health and well-being for your child.
Pathophysiology of sickle cell anemia
Pathophysiology of Sickle Cell Anemia
Sickle cell anemia is a genetic disorder caused by a mutation in the HBB gene, leading to the production of abnormal hemoglobin (HbS).
Red Blood Cell Deformation: Under low oxygen conditions, HbS polymerizes, causing red blood cells to become rigid and sickle-shaped.
Vaso-occlusion: Sickle-shaped cells can obstruct blood flow in small vessels, leading to ischemia and pain.
Hemolysis: The abnormal cells have a shorter lifespan (10-20 days), resulting in chronic hemolytic anemia.
Complications: Increased risk of infections, acute chest syndrome, and organ damage due to reduced blood flow.
Management includes pain relief, hydration, and blood transfusions.
sickle cell anemia causes _________ molecules to stick to one another and clump ________.
hemoglobin, clump
Airplane concerns for anemia
dehydration
sitting for hours
pain
decreased O2
high altitude
treatment of anemia
fluid
IV/meds
AVOID NSAIDs
give analgesics
threat O2
compression stockings
antibiotics
NEVER GIVE BLOOD THINNERS
function of platelets
clot
function of WBCs
protect
function of RBCs
carries oxygen/nutrients
Lab values given in exam
don’t need to memorize pg. 784 :)
Hemoglobin
iron needs to “hem” oglobin
Greatest reason for iron deficiencies
malnutrition
solution: supplement/proper nutrition
Microcytic/hypochromic
fuller on outside, not on inside