Chapter 7: Neurological examination
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
What is a Neurological Examination?
A series of tests conducted by a neurologist to evaluate the integrity of the nervous system for many reasons, including (but not limited to)
Following trauma or stroke
When there are suspected neurodegenerative changes (ex. Cumulative change in brain from playing sports)
Following exposure to a neurotoxic agent
Localization
Cerebral Hemisphere (Telencephalon)
Internal Capsule
Brainstem (Diencephalon, Mesencephalon, Metencephalon, or Myelencephalon?)
Spinal Cord
Cranial Nerves
Neuromuscular Junction
Muscle
Overview of common components of exam
Patient history
Cranial nerve function
Motor function (e.g., reflexes)
Somatosensory function
Coordination
Mental status
Patient history: Age, education and handedness
Just going to Post-secondary school → less likely to have cognitive impairment later in life, like dementia
Right-handers and left-hemisphere dominance
Patient history (cont’d)
Past medical history
Use of prescription and/or recreational drugs
Family medical history
Disease Process:
Temporal profile: sudden vs. gradual; acute vs. chronic
Change over time: static, improvement, worsening
Identify triggers/relievers of symptoms
Gauge severity of symptoms
Memorize cranial nerves
Oh Oh Oh, To Touch And Feel Very Good Velvet, Ah Heaven
Some say money matters, but my brother says big brains matter more

Olfactory (I)
Damages that cause (I) dysfunction: Ethmoid ridge (bones behind nose), cribriform plate (also another bones with axons, injured → cut axons, and TBI
Damage: Can’t smell
Optic (II)
Standard visual acuity tests for each eye
Visual field confrontation
Papilledema (swelling of optic disk) due to intracranial pressure
Nystagmus
Damages cranial nerves III, IV, VI.
A condition characterized by involuntary, repetitive eye movements, which can cause reduced vision and depth perception
Oculomotor (III)
Eyelid motor
Damage: Ptosis
Ptosis
Damages III
Droopy eyelids, block the view to see
Trochlear (IV)
Moves the eye down and in
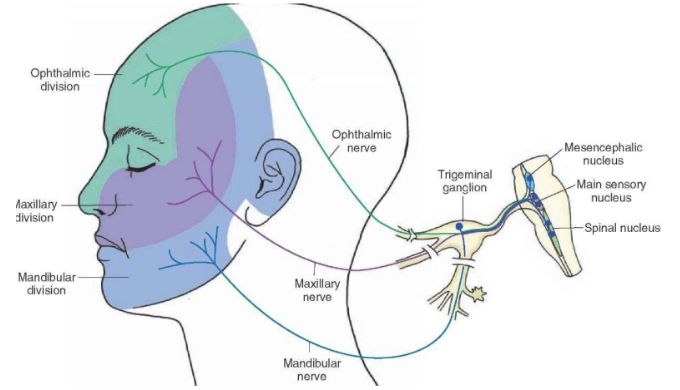
Trigeminal (V)
Facial somatosensation (put cotton, “can you feel”?)
Motor function (feel muscle by clenching teeth)
Reflex (put cotton close to eye, see if they blink)
So test the forehead, cheekbones, chin
Abducens (VI)
Moves eye outward (abduction)
Facial (VII)
Facial expression: Smile, frown, wrinkle their forehead
Taste: Anterior tongue
But we don’t really test taste! We are bad at it. Sick/too hot food → temporarily lose taste
Damage: Bell’s Palsy (temporary facial asymmetries)
Bell’s Palsy
Half droopy face, facial paralysis, impaired taste
Vestibulocochlear (VIII)
Auditory perception (Close one ear, whisper to another ear, “can you hear”?)
Balance
Glossopharyngeal (IX)
Taste and sensation from posterior tongue
Gag reflex, Swallowing, Coughing, Voice
Hard to detect
Vagus (X)
Parasympathetic NS: Motor control of heart, lungs, digestive system, etc.
Outer ear canal sensation
Gag reflex, Swallowing, Coughing, Voice
Hard to detect
Accessory (XI)
Shrugging of shoulders
Head resistance
Hypoglossal (XII)
Movement of tongue (push tongue against your cheek), NOT TASTE, lateral movement of tongue, speech, swallowing
Motor neurons
This motor neuron travels down the spinal cord to muscles
Upper motor neuron (not the last stop) sends signal from motor cortex and brainstem, down to the spinal cord, lower motor neuron receives it, and sends it out to muscles, and causes them to contract
They causes reflex! Like the knee-jerk. This type of assessment test the stretch reflex.
Upper motor neuron lesions
Descending Inhibition
Exaggerated reflex (hyperreflexia)
Muscle spasm
Lower motor neuron lesions
Reduce reflex (hyporeflexia)
Lower muscle tone
Descending inhibition
The suppression of reflex activity and muscle tone by signals from the brain and upper motor neurons to the spinal cord. This process helps prevent excessive reflexes.
This is why upper motor neuron lesions → leads to removal of descending inhibition → leads to removal of this reflex suppression → leads to excessive reflex (hyperreflexia)
Key features to examine in motor function
Gross appearance of muscle
Muscle tone, strength
Somatosensory function
Pain
Light touch and proprioception
Testing for Astereognosis
Testing for Graphesthesia
Proprioception
The ability to know where your body parts are in space.
Can be tested by blindfolding you and put your right arm behind your back. If you have this impairment, you will not know where your right arm is when you’re blindfolded
Damage caused by: Cortical strokes
Astereognosis
Inability to perceive the object by touch (ex. hold an eraser, and can’t guess what’s in their hand)
Graphesthesia
Inability to recognize symbols/numbers/letters traced on skin (like back or hand)
Coordination
Quick, alternating movement
Point-to-point movement: Move your finger towards your nose. Cerebellum damage if you can’t do it
Heel-to-shin: Lie on the side, and swing your foot in the air from heel to shin rapidly. Cerebellum damage if you can’t do it
Resistant to sitting/standing
Gait: Walking normally to check smoothness, balance, and symmetry
Coordination: Romberg test
Test cerebellum, vision, vestibular function
But, this test will take out ⅓, which is vision, leaving behind only cerebellum sense, and vestibular sense. So if you have both intact, you’ll do fine, but if you’re missing one (cerebellum OR vestibular) it’ll be very obvious.
The patient stands with feet together, and arms at their sides.
They are asked to close their eyes and maintain balance for about 20-30 seconds.
The examiner observes for swaying, loss of balance, or falling.
MSE: Attention and orientation
Observe the patient’s alertness
Spelling a word backwards
Counting backwards from 20
Auditory vigilance (Ex. ask to raise your hand)
(To check orientation) Current whereabouts (“do you know where are you rn?”), time (“what year it is rn?”)
Damage: Contralateral neglect, anosognosia
Why MSE test attention first?
If you have a problem with this (like not knowing where you are), it’ll affect every test you do.
Regions involved in MSE attention and orientation
Focal cortical and subcortical regions
Origin may be diffused (e.g. toxin)
Contralateral neglect
Inability to draw their attention to the left side of the world, and it’s not sensory impairment. (Drawing test, or not eating the food on the left side on the plate)
Most likely, Right parietal lobe damage (so while left hemisphere mostly controls the language aspect, the right hemisphere mainly controls attention!)
Anosognosia
Failure of individual to self-reflect that they have a disorder/dysfunction
(ex. seen in many Schizophrenic patients—they don’t realize that they’re hallucinating)
Usually goes away in a couple of months
Often caused by damage to the right parietal lobe, affecting self-awareness and perception.
Not the same as denial! They’re not aware, not refusing to accept it
MSE: Language
Fluency
Naming
Repetition
Prosody: Stress in speech
Comprehension
Reading
Writing
Damage: Praxis: “Pick up a pen to pretend that to be a knife, and slice a cheese” The dysfunction in this, they can’t do it according to the instruction
Regions involved in MSE language
Broca’s area: Speech production (motor planning structure)(in temporal lobe)
Wernicke’s area: Speech comprehension (in frontal lobe)
Praxia
The ability to pretend that an object and do another role
“Pick up a pen to pretend that to be a knife, and slice a cheese”
The dysfunction in this (apraxia), they can’t do it according to the instruction
Receptive aphasia
Wernicke’s aphasia: Fluent, Comprehension impairment, Nonsense speech. Also problems comprehending their speech and other ppl’s speech
Expressive aphasia
Broca’s aphasia: If the broca is broken, then no words are spoken!.
Not fluent, No comprehension impairment, Affects speech production, making speech slow, labored, and grammatically limited. No comprehension impairment
Global aphasia
Not fluent, Dysfunction in both speech production AND speech comprehension. “Tunnel tunnel tunnel tunnel tunnel tunnel tunnel”
Why can the guy in the video can count 1-10, but can’t say any other things else than tunnelๆๆๆ? Cuz it’s smth we learn to do since a very young age, and this shows how basal ganglia works!—habits and skills
Alexia
Problem with reading. After brain injury
Agraphia
Problem with writing. After brain injury
MSE: Memory
Digit span 1-9 (>5 digits, you’re fine)
Pointing span: Point to different corners of the room, then ask the patient to point to those corners in order
Verbal, visual object learning
Past public/personal events
Factual knowledge
Regions involved in MSE memory
Medial temporal structures (ex. hippocampus), thalamus, basal forebrain (Alzheimer’s), prefrontal cortex (ex. pointing span)
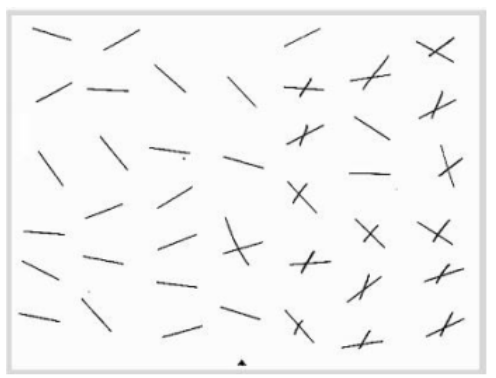
MSE: Visuospatial function
Line cancellation: Cross through all the lines you see
Copy geometric designs
Judgment of line orientation
Object/face/color recognition
Damage: Agnosia, prosopagnosia
Region involved in MSE visuospatial function
Ventral side of temporal lobe (e.g. fusiform gyrus) — damage: birdwatchers can’t recognize diff types of birds anymore
Agnosia
Inability to recognize or interpret sensory information, despite having intact sensory functions (e.g., normal vision or hearing)
Prosopagnosia
Failure to recognize faces
MSE: Executive functions
Ability to multi-task, adjust ur thoughts and behaviors accordingly, make decisions for long-term outcomes, etc.)
Judgment (ex. If you see an envelope on the side of the road, next to the mailbox, they can’t judge what to do with the letter) (Ex. Misjudgment that you shouldn’t go for your friend’s crush)
Cognitive/behavioral flexibility
Luria 3-step (fist-edge-palm on the table repeatedly—test flexibity)
Drawing loops (like drawing 8), alternating patterns
Oral trail making test (A1, B2, C3, D4)
Perseverative behavior
Inflexibility. When a person gets "stuck" on a response and has difficulty shifting to something new
Glasgow Coma Scale (GCS)
A clinical tool developed at the University of Glasgow. It provides a practical method for assessing a patient's level of consciousness in response to defined stimuli
GCS: Purpose and usage
Assessing Severity: Determining the extent of a patient's neurological impairment.
Monitoring Progress: Tracking changes in consciousness over time.
Guiding Treatment Decisions: Informing medical interventions based on the patient's responsiveness
GCS: Evaluating three specific responses
Eye Opening (E) (4 scales): Assesses arousal and awareness.
Verbal Response (V) (5 scales): Evaluates coherence and orientation.
Motor Response (M) (6 scales): Measures purposeful movement and response to stimuli.
GCS: Eye Opening (E)
4: Spontaneous
3: To sound
2: To pressure
1: None
Verbal Response (V)
5: Orientated
4: Confused
3: Words
2: Sounds
1: None
Motor Response (M)
6: Obeys commands
5: Localizes pain: Moves hand toward pain source
4: Normal flexion (withdrawal): Withdraws from pain, but not directed
3: Abnormal flexion: Arms bend abnormally across the body
2: Extension: Arms extend rigidly
1: None
GCS: Interpretation of scores
13-15: Mild brain injury
9-12: Moderate brain injury
8 or less: Severe brain injury
A lower GCS score means…
A deeper level of unconsciousness and a more severe brain injurt
GCS: Structured assessment approach (4 steps)
Check: Identify any factors that might interfere with the assessment (e.g., sedation, paralysis).
Observe: Look for spontaneous behaviors in eye opening, verbalization, and movements.
Stimulate: Apply verbal and physical stimuli if there is no spontaneous behavior.
Rate: Assign scores based on the observed responses.