B2.3 Transport - Paper 2 Questions
1/20
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
Draw and label a diagram of the heart showing the four chambers, associated blood vessels, valves and the route of the blood through the heart
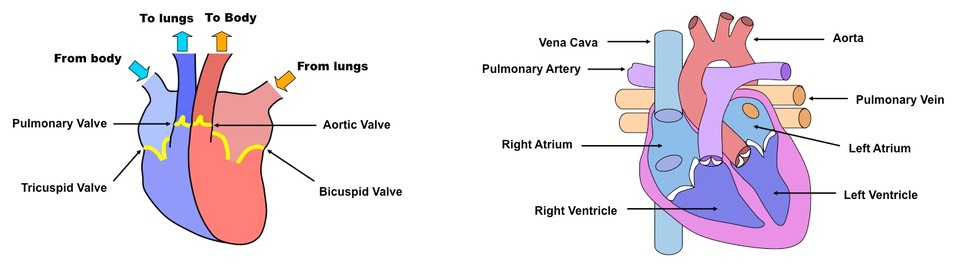
Explain the action of the heart in terms of collecting blood, pumping blood and opening and closing valves
Deoxygenated bbood returning from all parts of the body (except lungs) enter the right atrium via the vena cava - this blood is relatively deoxygenated
The blood passes from the right atrium to the right ventricle and then via the pulmonary artery to the lungs (where blood is reoxygenated)
The blood returns to the left atrium via the pulmonary vein and passes through the left ventricle to the aorta, where it is pumped around the body
The heart valves maintain the one-way flow of blood:
When the atria contract, atrioventricular (AV) valves open
Blood flows from the atria and into the ventricles
When the ventricles contract, the AV valves close and semilunar valves open
This forces blood out of the ventricles and into the arteries
As arterial pressure rises, the semilunar valves close, ensuring the one-way flow of blood
Outline the control of the heartbeat in terms of myogenic muscle contraction, the role of the pacemaker, nerves, the medulla of the brain and epinephrine (adrenaline)
The contraction of the heart tissue (myocardium) is myogenic, meaning the signal for cardial contraction arises within the heart muscle itself
Within the wall of the right atrium are a specialised plexus of nerves called the sinoatrial node (SAN)
The sinoatrial node initiates contraction of the cardiace muscle and acts as a pacemaker, regulating normal sinus rhythm
It stimulates atria to contract and, when excitation reaches the junction between atria and ventricles, stimulates another node (atrioventicular node)
The atrioventricular node (AVN) sends signals via the Bundle of His to Purkinje fibres, which cause ventricular contraction
This sequence always ensures their is a delay between atrial and ventricular contractions, resulting in two heart sounds ('lub dub')
The pacemaker is under autonomic control from the brain, specifically the medulla oblongata (brain stem)
Sympathetic nerves speed up heart rate by releasing a neurotransmitter (noradrenaline) to increase the rate of myocardial contraction
Parasympathetic nerves splow down heart rate by releasing a neurotransmitter (acetylcholine) to decrease the rate of myocardial contraction
Additionally, the heart rate may be increased by the chemical release of the hormone adrenaline into the blood (from the adrenal gland)
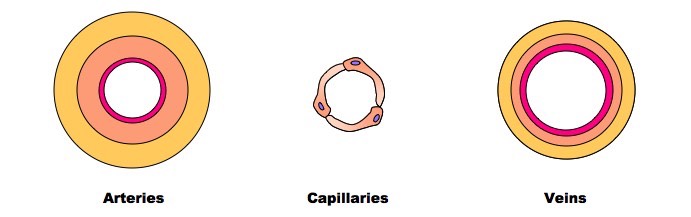
Explain the relationship between the structure and function of arteries, capillaries and veins
Arteries
Arteries carry blood at high pressure (80 - 120 mm Hg)
They have a narrower lumen (to maintain high pressure) surround by a thick wall made of two layers
The middle layer (tunica media) contains muscle and elastin to help maintain pulse flow (it can contract and stretch)
The outer layer (tunica adventitia) contains collagen prevents the artery rupturing due to the high pressure blood flow
Veins
Veins carry blood under low pressure (<10 mm Hg)
They have a very wide lumen (keeps pressure low and allows greater flow of blood)
The walls of tissue surrounding the vein are thin (blood is not travelling in rhythmic pulses)
They have valves to prevent blood pooling at extremities (arteries do not have valves)
Capillaries
Capillaries are involved with material and gas exchange with the surrounding body tissue
Blood pressure in the capillaries is relatively low (~15 mm Hg) and they have a very small diameter (~5 micrometers wide)
Their wall is made up a a single layer of cells to allow for ease of diffusion
Capillaries may contain pores to aid the transport of material
How does the structure of capillaries ensure efficient oxygen and carbon dioxide exchange?
The structure of capillaries is finely tuned for the efficient exchange of oxygen and carbon dioxide.
Capillaries have extremely thin walls, often consisting of just a single layer of endothelial cells. This minimizes the distance over which diffusion has to occur, speeding up the exchange process.
The narrow diameter of capillaries ensures that blood moves slowly, giving sufficient time for gases to equilibrate between the blood and surrounding cells.
The vast network and branching of capillaries increase their surface area, providing more sites for exchange.
Some capillaries have fenestrations - microscopic pores that allow larger molecules like proteins to pass through, facilitating rapid exchange between the blood and surrounding tissues.
The combined effect of these adaptations ensures that cells receive the oxygen they need for cellular respiration and can offload waste carbon dioxide efficiently.
Adaptations of arteries
Artery walls consist of three layers:
The innermost layer is an endothelial layer, consisting of squamous epithelium
The endothelium is one cell thick and lines the lumen of all blood vessels. It is very smooth and reduces friction for free blood flow
The middle layer contains smooth muscle cells and a thick layer of elastic tissue
This layer is very thick in the walls of arteries
The layer of muscle:
Strengthen the arteries so they can withstand high pressure
Can contract or relax to control the diameter of the lumen and regulate blood pressure
The elastic tissue helps to maintain blood pressure in the arteries; it stretches and recoils to even out fluctuations in pressure when the heart beats
Further from the heart there is more smooth muscle and less elastic tissue due to smaller fluctuations in blood pressure
The outer layer covers the exterior of the artery and is mostly made up of collagen and elastic fibres
Collagen is a strong protein and protects blood vessels from damage by over-stretching
Along with elastic fibres, it prevents the arterial wall from rupturing as blood surges from the ventricles
Arteries have a narrow lumen which helps to maintain high blood pressure
Arterial blood pressure
Arteries, and to a slightly lesser extent arterioles, must be able to withstand high pressure generated by the contracting heart, and both must maintain this pressure when the heart is relaxed
Muscle and elastic fibres in the arteries help to maintain the blood pressure as the heart contracts and relaxes
Systolic pressure is the peak pressure point reached in the arteries as the blood is forced out of the ventricles at high pressure
At this point the walls of the arteries are forced outwards, enabled by the stretching of elastic fibres
Diastolic pressure is the lowest pressure point reached within the artery as the heart relaxes
At this point the stretched elastic fibres recoil and force the blood onward through the lumen of the arteries
This maintains high pressure throughout the heart beat cycle
Vasoconstriction of the circular muscles of the arteries can increase blood pressure by decreasing the diameter of the lumen
Vasodilation of the circular muscles causes blood pressure to decrease by increasing the diameter of the lumen
Adaptations of veins
They receive blood that has passed through capillary networks, across which pressure has dropped due to the slow flow of blood
The capillaries converge to form venules, which deliver blood to veins
The structure of veins differs from arteries:
The middle layer is much thinner in veins
There is no need for a thick muscular and elastic layer as veins don't have to maintain or withstand high pressure
The walls of veins are flexible, allowing surrounding muscles and tissues to compress them
This facilitates the movement of blood back to the heart
Veins contain valves
These prevent the back flow of blood that can result under low pressure, helping return blood to the heart
Movement of the skeletal muscles pushes the blood through the veins, and any blood that gets pushed backwards gets caught in the valves; this blood can then be moved forwards by the next skeletal muscle movement
Veins have a wide lumen
This maximises the volume of blood that can flow at any one time
Differentiate between the structural features of arteries and veins
Functions: Arteries, responsible for transporting oxygen-rich blood away from the heart (excluding pulmonary arteries). Veins are responsible for returning deoxygenated blood to the heart (except pulmonary veins).
Arteries have thick walls made predominantly of smooth muscle and elastic tissue. These robust walls are essential for withstanding high blood pressures. Veins have thinner walls with less smooth muscle and elastic tissue, resulting in a more compliant structure.
In relation to their overall size, arteries have a narrower lumen which supports these high pressures and aids the forward propulsion of blood. Vein’s lumen is broader, facilitating the flow of blood at reduced pressures. Crucially, veins incorporate valves to prevent blood backflow, ensuring a unidirectional movement towards the heart.
Veins have valves which are essential in preventing backflow. These structures ensure unidirectional blood flow towards the heart, especially in areas like the legs where blood must overcome gravity.
Arteries have elastic properties - the walls are not rigid; their elastic nature helps maintain a consistent blood pressure, absorbing the force from each heartbeat and then using this stored energy to keep blood flowing during the heart's relaxation phase.
What are the key differences between arterioles and arteries in terms of structure and functions?
Both arterioles and arteries are components of the arterial system, but they have distinct differences in structure and function.
Arteries are larger vessels responsible for transporting oxygenated blood from the heart to various body parts. Arterioles, on the other hand, are smaller branches of arteries that lead to capillaries.
They have thick walls comprising significant amounts of muscle and elastic tissue to handle high pressures. They have relatively thinner walls than arteries but play a crucial role in regulating blood flow into capillary beds.
By constricting or dilating, arterioles can control the volume of blood that reaches specific tissues, thereby helping to regulate blood pressure and distribution according to the tissue's metabolic demands.
Why is it essential for veins to have valves, especially in legs?
Valves in veins are pivotal structures that ensure unidirectional blood flow back to the heart.
Given that veins, especially those in the legs, operate under low pressures and have to work against gravity to return blood to the heart, the role of these valves becomes paramount. When leg muscles contract, they compress the veins, pushing the blood upwards. Valves prevent the backflow of this blood, ensuring that it consistently moves towards the heart.
Without these valves, the efficiency of venous return would be compromised, leading to pooling of blood in the lower extremities, which can further result in complications like varicose veins.
Why do arteries possess more elastic tissue compared to veins?
Arteries are responsible for carrying blood away from the heart, which means they are exposed to high pressures with each heartbeat.
The elastic tissue in their walls allows them to stretch and expand when the heart contracts, helping absorb this pressure.
Then, during the relaxation phase (diastole) of the heart, the arteries recoil, using the stored energy to maintain a consistent and forward flow of blood.
In contrast, veins operate under much lower pressures and thus don't require as much elasticity. Their primary challenges, such as preventing backflow, are addressed by other adaptations like valves.
How do fenestrations in capillaries differ from gaps in the lymphatic system’s thin-walled ducts?
Fenestrations in capillaries and gaps in the lymphatic system's thin-walled ducts both serve to allow the exchange or movement of substances, but they have different structural characteristics and functions.
Capillary fenestrations are tiny pores in the endothelial cells of certain capillaries. These fenestrations enhance permeability, facilitating the transfer of larger molecules like proteins between the blood and surrounding tissues.
In contrast, the gaps present in the lymphatic system's thin-walled ducts are larger and are designed to allow excess tissue fluid and larger cells, such as immune cells, to enter the lymphatic system from the surrounding tissues. These gaps ensure the effective drainage of lymph, which eventually returns to the blood circulation.
Plants have developed efficient methods for transport of water and organic materials. Distinguish between the xylem and phloem of plants.
Plasma membrane in phloem/sieve tubes but not in xylem/vessels (xylem/vessels are dead/acellular whereas phloem/sieve tubes are alive)
xylem vessels have thicker walls than phloem
xylem vessel walls are lignified whereas phloem walls are not
phloem vessels have sieve plates whereas xylem vessels have no cross walls
xylem/vessels are wider/larger than phloem/sieve tubes
companion cells in phloem but not in xylem
Outline the structural adaptations of capillaries that facilitate the efficient exchange of materials with surrounding tissues.
They possess an extensive surface area due to their vast branching, allowing a rapid and efficient exchange rate.
The diameter of capillaries is slender, ensuring a slowed blood flow which provides more time for the effective transfer of substances.
Their walls are incredibly thin, often composed of just a single layer of endothelial cells, which minimises the diffusion pathway.
Additionally, some capillaries feature fenestrations, which are microscopic pores that enable larger molecules, like proteins, to traverse, further boosting the exchange efficiency between blood and nearby tissues.
Explain the processes that cause water to move from the roots of plants to their leaves.
water moved in xylem vessels under tension
tension generated when water evaporates from cell walls (in mesophyll) in a process called transpiration
transpiration is loss of water vapour from leaf (surface)/stomata
cohesivity/cohesion in water due to hydrogen bonding/attractions between water molecules
cohesion ensures that chain/column of water (molecules) does not break/remains continuous
transpiration stream is a column/flow of water in xylem from roots to leaves.
Distinguish between the different phases of the cardiac cycle in the atria and in the ventricular muscle.
Action potential of atrium precedes the ventricle
atrium has a shorter phase 2 and ventricle has a longer phase 2
atrium action potential falls abruptly in phase 2 when ventricle shows a plateau
phase 3 falls more abruptly in ventricular action potential
ventricular phase is overall longer than atrial phase.
Compare and contrast the single circulation of bony fish and the double circulation of mammals [3]
Similarities:
both mammals and fish have a closed circulation
blood is pumped by a heart and circulated in a continuous system of tubes under pressure
circulatory system consists of a heart, arteries, veins and capillaries.
Differences:
bony fish have a single circulation (blood enters and leaves the heart once): blood enters from the body and then leaves to the gills, where blood is oxygenated, and then moves to the rest of the body where oxygen is delivered to tissues. mammals have a double circulation(blood travels through heart twice)
heart in mammals has four chambers whereas bony fish have two
in mammals, the heart is divided into right and left sides: blood flows from the right side of the heart to the lungs, then back to the left side of the heart; the role of the right side of the heart is to pump deoxygenated blood to the lungs; oxygenated blood in mammals is separated from deoxygenated blood, whereas in fish the oxygenated and deoxygenated blood mix/no separation
mammalian circulatory system can pump blood to the body/systemic circulation under high pressure and blood to lungs/pulmonary circulation under lower pressure.
Outline the control mechanism of the heart rate [5]
The heartbeat originates in part of the muscle wall of the right atrium, called the sinoatrial node (SAN) or pacemaker
from here, a wave of excitation (electrical impulses) spreads out across both atria
in response, the muscle of both atrial walls contracts simultaneously (atrial systole). this stimulus does not spread to the ventricles immediately, due to the presence of a narrow band of non-conducting fibres at the base of the atria
these block the excitation wave, preventing its conduction across to the ventricles
the stimulus is picked up by the atrioventricular node (AVN), situated at the base of the right atrium
after a delay (of 0.1s ~ 0.2 s), the excitation is passed from the AVN to the base of both ventricles by tiny bundles of conducting fibres (the Purkinje tissue)
when stimulated by the bundles of His, the ventricle muscles start to contract from the base of the heart upwards (ventricular systole)
the delay that occurs prevents the atria and ventricles from contracting simultaneously
after every contraction, cardiac muscle has a period of insensitivity to stimulation (the refractory period)/a period of enforced non- contraction/diastole
in this phase, the heart begins, passively, to refill with blood
medulla (oblongata of brain) can change/increase/decrease the rate; through nerves/named example of nerve/autonomic/sympathetic/parasympathetic nervous system
one nerve increases the rate and the other decreases it
epinephrine increases heart rate/force of contraction
epinephrine prepares the body for vigorous activity/is part of fight or flight response.
Outline how root pressure is generated in xylem [5]
Endodermal cells of the root contain a waterproof substance (suberin) that blocks the apoplast pathway, directing water through the symplast pathway. this ensures water flows into the xylem and not out, enabling the plant to control water movement
endodermal cells pump salts into the xylem. this lowers the water potential of the xylem/increases solute concentration, enabling water to move down a water potential gradient
a positive pressure potential is created, moving water and dissolved minerals a short distance up the xylem.
Explain the formation and reuptake of tissue fluid [7]
Tissue fluid is a mixture of water and solutes, forced out of the blood by ultrafiltration and it surrounds body cells
tissue fluid is forced from capillaries through small gaps in the endothelium/wall of capillary, under hydrostatic pressure
at the arteriole end of the capillary bed, the force applied to the blood by the heart creates sufficient hydrostatic pressure to overcome osmotic water uptake
at the arteriole end, blood pressure is significantly higher than at the venule end
as blood flows through the capillary bed there is progressive loss of hydrostatic pressure and so osmotic movement of water/osmotic water uptake into the capillary can occur
as a result, lower pressure in the venules allows tissue fluid to drain back into capillaries; not all tissue fluid is returned to the blood circulation by this route - some enter the lymph capillaries.