Depressive Disorder - PSR
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
Depressive Disorders and Bipolar Disorders
DSM IV-TR combined the Depressive Disorders and Bipolar Disorders into one category, Mood Disorders assuming these disorders were on a Spectrum of Mood Disturbance.
This is not true in DSM 5 or 5-TR.
Mood disorder is no longer a DSM diagnosis.
Depressive Disorders in DSM 5
From APA paper Highlights of Changes from DSM IV-TR to DSM 5:
DSM 5 contains several new depressive disorders, including
disruptive mood dysregulation disorder and
premenstrual dysphoric disorder.
To address concerns about potential over-diagnosis and overtreatment of bipolar disorder in children, a new diagnosis, disruptive mood dysregulation disorder, is included for children up to age 18 years who exhibit persistent irritability and frequent episodes of extreme behavioral dys-control.
From APA paper Highlights of Changes from DSM IV-TR to DSM -5:
Based on strong scientific evidence, premenstrual dysphoric disorder has been moved from DSM-IV Appendix B, “Criteria Sets and Axes Provided for Further Study,” to the main body of DSM-5.
Finally, DSM-5 conceptualizes chronic forms of depression in a somewhat modified way.
What was referred to as dysthymia in DSM-IV now falls under the category of persistent depressive disorder, which includes both chronic major depressive disorder and the previous dysthymic disorder
Facts from Washington University School of Medicine
Of the estimated 17.5 million Americans who are affected by some form of depression, 9.2 million have major or clinical depression
Two-thirds of people suffering from depression do not seek necessary treatment
80% of all people with clinical depression who have received treatment significantly improve their lives
The economic cost of depression is estimated at $30.4 billion a year but the cost in human suffering cannot be estimated
Women experience depression about twice as often as men
By the year 2020, the World Health Organization (WHO) estimates that depression will be the number two cause of "lost years of healthy life" worldwide
Major Depression is 1.5-3.0 times more common among first-degree biological relatives of those with the disorder than among the general population
NIH Statistics
Depressive disorders NIH Statistics on Depressive Disorders
Often co-occur with anxiety disorders and substance abuse.
Major Depressive Disorder is the leading cause of disability in the U.S. for ages 15-44 & affects approximately 14.8 million American adults
Signs of Depressive Illness
feeling worthless, helpless or hopeless,
sleeping more or less than usual,
eating more or less than usual,
having difficulty concentrating or making decisions,
loss of interest in taking part in activities
decreased sex drive,
avoiding other people,
overwhelming feelings of sadness or grief,
feeling unreasonably guilty,
loss of energy, feeling very tired,
thoughts of death or suicide.
Signs of Depression
Most widespread psychological disorder
25 to 30% of college students have symptoms of depression
Study showed 20 percent of all students surveyed thought about suicide,
9 percent had attempted suicide,
20 percent injured themselves.
Older persons and Depression
Between 1 and 2 percent of people over age 65 living in the community, i.e., not living in nursing homes or other institutions, suffer from major depression and about 2 percent have dysthymia (persistent depressive disorder in DSM 5-TR)
Depressive Symptoms
Disorders of
Mood or emotion
Thought or cognition
Motivation
Physical or somatic symptoms
Emotional symptoms
Sadness
Worse in morning
Anxiety
Anhedonia
Numbing
Flat affect
Dullness
Irritability
Cognitive Symptoms
Negative view of self
low self-esteem
feelings of inferiority
distorted beliefs about achievement
self-blaming & guilt
Negative view of future
hopeless of future
future actions ineffective
belief that negative future is unable to be changed by action
Motivational Symptoms
Lack of response initiation
Psychomotor retardation
Inability to make decisions
Difficulty choosing alternatives
Somatic symptoms
Loss of appetite
Weight loss
moderate to severe depression
Sleep disturbance
normally in early morning awakening
Weakness & fatigue
Loss interest in self
erectile difficulty
lack of arousal
Other Physical Complaints
Headache
Backaches
Gastrointestinal symptoms
Yeast infections
Upper respiratory infections
Shoulder aches
Accidents
Beck’s Triad
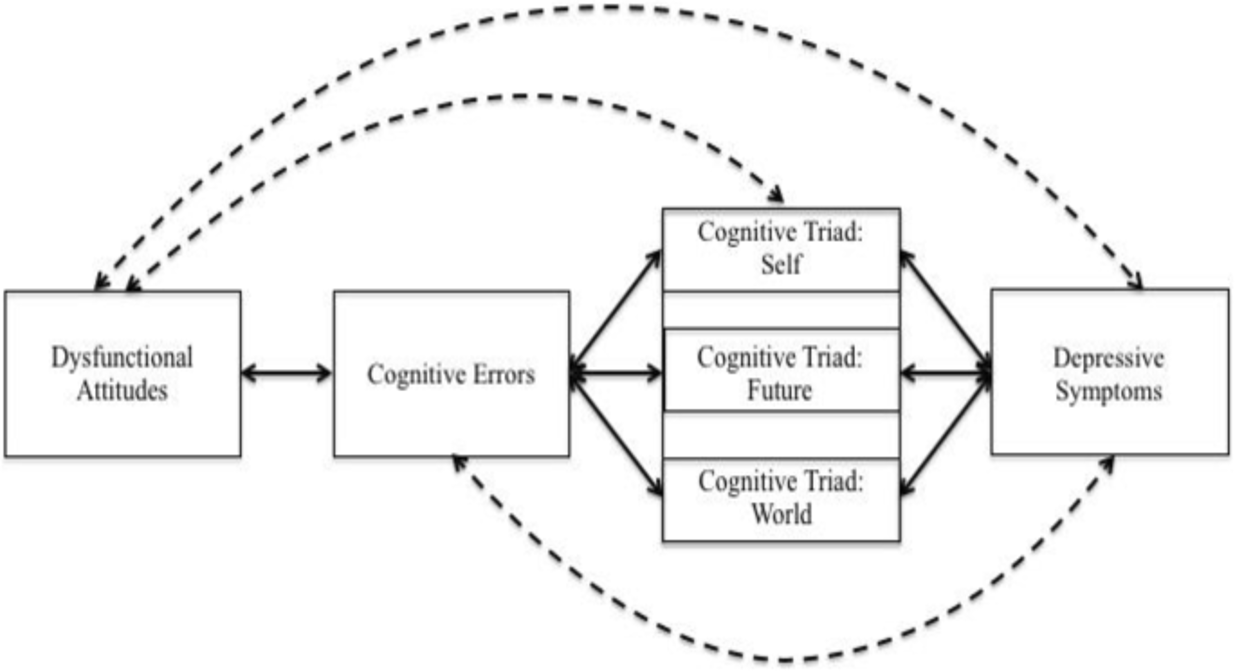
The APA note that CBT is based on a number of beliefs, including the following:
Unhelpful ways that people think can lead to psychological problems.
If people learn unhelpful behavior, this, too, can lead to psychological issues.
People can learn more beneficial ways of thinking and behaving.
New habits can relieve symptoms of mental and physical conditions and allow people to act in better ways.
DSM 5: Depressive Disorders
Disruptive Mood Dysregulation Disorder
Major Depressive Disorder
Persistent Depressive Disorder
Premenstrual Dysphoric Disorder
Substance/medication-induced Depressive Disorder
Depressive Disorder due to another medical condition
Other specified Depressive Disorder
Unspecified Depressive Disorder
DSM 5-TR: Depressive Disorders
Common feature of all of these disorders is the presence of sad, empty, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s ability to function. What differs is duration, timing, or presumed etiology.
DMDD is intended to capture children with frequent temper tantrums and irritability, in part to prevent the overdiagnosis of bipolar disorder in youth with prepubertal onset of these symptoms. Often, such presentations result in a diagnosis of bipolar disorder or oppositional defiant disorder
Disruptive Mood Dysregulation Disorder (F34.8)
The core feature is chronic, severe persistent irritability.
The severe irritability has two features
(a) frequent temper outbursts due to frustration, occurring three or more times per week for a year in two contexts,
(b) chronic persistent irritable angry mood present between temper outbursts.
The irritable mood must be characteristic of the child most of the day, every day, and noticed by those in the environment.
Criteria:
A. Severe temper outbursts verbally or behaviorally at least three times a week
B. Temper outbursts inconsistent with developmental level
C. Temper outbursts occur, on average, three or more times per week.
D. Mood between outbursts is persistently irritable and angry most of the day, nearly every day and observed by others.
E. Criteria A-D are present for 12 months and in that time individual not had 3 months without symptoms
F. Criteria A-D present in two of three settings and severe in one.
Not made before six years old or after 18 years
Symptoms begin before age ten
I. Never been period more than day when criteria not met
J. Do not occur exclusively with MDD or explained by other mental disorder
Cannot coexist with ODD, Intermittent Explosive Disorder, or Bipolar Disorder, but can with ADHD, MDD, CD and Substance Use Disorder
If DMDD, no ODD
Ever manic episode, no DMDD
Prevalence & Course-DMDD
Prevalence unclear, must have onset before age 10. Not be applied to children younger than 6 years.
Only use with clients 6-18 years.
Male predominance of condition.
Conversion from sever, non-episodic irritability to bipolar disorder are low.
Children diagnosed with DMDD more likely to develop unipolar depression and/or anxiety disorder.
Major Depressive Disorder
Symptoms must be present every day to be considered present, with the exception of weight change and suicidal ideation with depressed mood most of day, every day
At least one of these symptoms present (2 weeks)
depressed mood
loss of interest or pleasure
Criteria
A. Five or more of following symptoms are present during the same 2-week period and represent a change in function— (Criteria A)
Five or more
Depressed mood most of day, nearly every day or observation
Children or adolescents may be irritable mood
Marked diminished pleasure in activities nearly every day
Significant weight loss or weight gain (5% month), decreased or increased appetite nearly every day
Children, failure to make expected weight gain
insomnia or hypersomnia, nearly every day
Psychomotor agitation or retardation every day
Fatigue or loss of energy nearly every day
Feelings of worthlessness or excessive/inappropriate guilt
Diminished ability to concentrate, think or indecisive
Recurrent thoughts of death, suicidal ideation (no plan), or attempt or plan for suicide.
B. Symptoms cause clinically significant distress or impairment in social, occupational or other function (Criteria B)
C. Not attributable to effects of a substance or medical disorder (Criteria C)
E. There has never been a manic or hypomanic episode
Rule out Mixed Episode
Rule out Substance Disorder effects
Rule out General Medical Condition
Specifiers
Recurrent episode must have interval of 2 months
Mild
Few if any symptoms in excess of those required to make the diagnosis are present, intensity is distressing, but manageable, minor impairment in functioning
Single episode---(F32.0)
Recurrent--------(F33.0)
Moderate
In between mild and severe
Single episode--- (F32.1)
Recurrent---------(F33.1)
Severe
Symptoms in excess of what is required for diagnosis, intensity is seriously distressing, unmanageable, symptoms markedly interfere in function
Single episode----- (F32.2)
Recurrent---------- (F33.2)
Specify
With psychotic features
Mood congruent: inadequacy, guilt, disease, death
Mood incongruent: does not involve depressive themes
Single episode---(F32.3)
Recurrent--------(F33.3)
In partial remission
Symptoms present, but full criteria not met, or 2 months without sig. symptoms
Single episode---(F32.4)
Recurrent--------(F33.41)
In full remission
Past 2 months no signs or symptoms
Single Episode---(F32.5)
Recurrent---------(F33.42)
Unspecified
Features of MDD
MDD associated with high mortality, mostly by suicide.
Depressed individuals admitted to nursing homes die in first year.
Molecular studies indicate genetic variants (neurotrophic factors and pro-inflammatory cytokines).
Abnormalities in neural systems supporting emotional processing, reward seeking, and emotional regulation in adults occur in persons with MDD.
MDD Prevalence
12-month prevalence at 7% with differences by age group. (higher in 18-29 year olds)
Higher prevalence in women, peaks in adolescence & stabilizes.
More atypical symptoms in women than men & more often in non-Hispanic Whites.
Peak onset in the 20s with variable course.
Persistent Depressive Disorder (F34.1)
This disorder represents a consolidation of DSM IV-TR defined chronic major depressive disorder and dysthymic disorder
Criteria
A. Depressed mood most of day for more days than not for at least 2 years.
Children or adolescents irritable mood and duration of one year
B. Presence depressed of
Poor appetite or overeating
Insomnia or hypersomnia
Low energy or fatigue
Low self-esteem
Poor concentration
Feelings of hopelessness
C. During the 2-year period never been without A and B symptoms for more than 2 months (1 year children)
D. Criteria for major depressive disorder may be continuously present for 2 years
E. No manic or hypomanic episodes
F. No cyclothymia, schizoaffective or other schizophrenia spectrum disorders
G. Not a substance or medical condition
H. Distress in social, occupational or other areas of functioning.
During the 2-year period never been without A and B symptoms for more than 2 months
Specifiers
Partial remission (see MDD)
in Full remission (see MDD)
Early Onset (before 21)
Late onset (after 21)
Mild
Few if any symptoms in excess of those required to make the diagnosis are present, intensity is distressing, but manageable, minor impairment in functioning
Moderate
Between mild and severe
Severe
Symptoms in excess of what is required for diagnosis, intensity is seriously distressing, unmanageable, symptoms markedly interfere in function
Specify:
With pure dysthymic syndrome
Full criteria for major depressive episode have not been met in preceding 2 years
With persistent major depressive episode
Full criteria for major depressive episode have been met through out preceding 2 years
With intermittent major depressive episode
Full criteria for major depressive episode been met currently, but been periods of 8 weeks in the preceding 2 years with symptoms below threshold for major depressive episode
With intermittent major depressive episodes, without current episode
Full criteria for major depressive episode are not currently met, but one or more major depressive episode in preceding 2 years
Only specifiers for PDD
Anxious distress
Two of following
Keyed up or tense
Unusually restless
Difficulty concentrating because of worry
Fear of something awful happening
Feeling loss of control
Atypical features
Mood reactivity
Mood brightens to positive events
Two following
Weight gain or increased appetite
Hypersomnia
Leaden paralysis
Heavy, leaden feelings in extremities
Reaction sensitivity
History of rejection sensitivity
Specify level of severity
Mild: Two symptoms
Moderate: Three symptoms
Moderate-severe: Four to five symptoms
Severe: Four to five symptoms and motor agitation
Premenstrual Dysphoric Disorder (N94.3)
Criteria
A. In majority of menstrual cycles, at least five symptoms present in final week before onset of menses, improve in a few days after onset of menses, minimal or absent in week post menses
B. One or more of following: Criteria B
Marked emotional liability
Marked irritability or anger or increased interpersonal conflicts
Marked depressed mood, feelings of hopelessness, self-deprecation
Marked anxiety, tension, feelings of being on edge or keyed up
C. One or more of following to reach a total of 5 symptoms when combined with above: Criteria C
Decreased interest in usual activities
Subjective difficulty in concentration
Lethargy, fatigability, lack of energy
Marked change in appetite, overeating, or food cravings
Insomnia or hypersomnia
Overwhelmed or out of control feelings
Breast tenderness, swelling, joint/muscle pain, bloating, weight gain
Symptoms A-C must be met most menstrual cycles that occurred in preceding year
D. Symptoms of significant distress or interference in functioning
E. Not just exacerbation of another disorder
F. Criterion A should be confirmed by daily ratings during two cycles
G. Not substance abuse or medical condition
Substance/medication-induced Depressive Disorder
A. Persistent disturbance in mood
B. Evidence from history of the following
1. Evidence of symptoms developing after intoxication, withdrawal or exposure to medication
2.Medication can produce those symptoms
C. Not better explained by depressive disorder not substance induced
D. Does not occur in delirium
E. Causes clinically significant distress
Diagnosis made instead of diagnosis of substance intoxication or withdrawal only when symptoms predominate and are severe
Specify
Mild
Moderate
Severe
Onset during intoxication
Onset during withdrawal
Substances that induce depressive disorders
Alcohol
Phencyclidine
Other hallucinogens
Inhalants
Opioids
Sedative, hypnotics, anxiolytics
Amphetamine
Cocaine
Other
Depressive Disorder Due to another Medical Condition
Essential feature is prominent and persistent period of depressed mood or markedly diminished interest or pleasure in all activities that is due to the direct physiological effects of another medical condition.
Evidence from medical results depressive disorder is result of a medical condition
Not explained by another mental disorder
Not part of a delirium
Causes distress and impairment
Specify
With depressive features--------------- (F06.31)
With major depressive –like episode (F06.32)
With mixed features--------------------- (F06.34)
Other Specified Depressive Disorders & Unspecified Depressive Disorder
Recurrent brief depression
Short-duration depressive episode
Depressive episode with insufficient symptoms
(F32.8) & (F32.9)
Recurrent brief depression
Concurrent presence of depressed mood and four other symptoms of depression for 2-13 days one per month, not menstrual cycle for 12 months. No other criteria met
Short-duration depressive episode (4-13 days)
Depressed affect and 4 of the 8 other symptoms of major depressive episode, distress for more than 4 days, but not more than 14. No other criteria met
Depressive episode with insufficient symptoms
Depressed affect and one of the 8 symptoms for 2 weeks. No other criteria met
Specifiers for Depressive Disorders
Specifiers
With anxious distress:
Two of following
Keyed up or tense
Unusually restless
Difficulty concentrating because of worry
Fear of something awful happening
Feeling loss of control
Specify level of severity
Mild: Two symptoms
Moderate: Three symptoms
Moderate-severe: Four to five symptoms
Severe: Four to five symptoms and motor agitation
With mixed features
At least three present nearly every day
Elevated, expansive mood
Inflated self-esteem or grandiosity
More talkative than usual or pressured speech
Flight of ideas or racing thoughts
Increased energy or goal directed activity
Increased involvement in activities with painful consequences
Decreased need for sleep, yet rested
Mixed symptoms observed by others
If meet criteria for mania or hypomania, bipolar disorder
Not substance or medical disorder
With melancholic features
One of following:
Loss of pleasure
Lack of reactivity to pleasure
Three or more of following
distinct quality of depressed mood
depression worse in morning
early morning awakening
marked psychomotor retardation or agitation
significant anorexia
excessive or inappropriate guilt
Near complete absence of pleasure. Psychomotor changes and distinct quality of mood differs from non-melancholic depressive episode
Specifiers for Depression
Atypical features
Mood reactivity
Mood brightens to positive events
Two following
Weight gain or increased appetite
Hypersomnia
Leaden paralysis
Heavy, leaden feelings in extremities
Reaction sensitivity
History of rejection sensitivity
Psychotic features
Delusions and hallucinations present
Mood congruent psychotic features
Content of delusions/hallucination are consistent with the depressive themes or manic themes
Mood incongruent psychotic features
Content of delusions/hallucination are not consistent with the depressive themes or manic themes
With seasonal pattern
Seasonal pattern of at least one type of episode
Time of the year and onset of mania, hypomania, depressive episode
Full remission when seasons change
Last 2 years, temporal relationship to remission
Seasonal mania or depression outnumber any other mania or depression
With peripartum onset
Onset during pregnancy or postpartum
Present with or without psychotic features
Infanticide most often associated with postpartum psychotic episodes
Once woman has had postpartum episode with psychotic features recurrence at 30 to 50%
Specify if
Partial or full remission
Level of severity
Mild
Moderate
Severe
Childhood Mood Disorders
Seven to 14 percent of children will experience an episode of major depression before the age of 15. Twenty to 30 percent of adult bipolar patients report having their first episode before the age of 20.
Out of 100,000 adolescents, 2,000 to 3,000 will have a mood disorders, of which eight to 10 will commit suicide.
Research indicates that depression onset is occurring earlier in life today than in past decades. (NIH)
Early-onset depression often persists, recurs, and continues into adulthood. Depression in youth may also predict more severe illness in adulthood. (NIH)
Children in Depression
Somber, almost ill appearance.
Frequent complaints of physical problems for which no medical difficulties can be found.
Lack of bounce and enthusiasm characteristic of non-depressed peers.
Tearfulness for no little or no identifiable reason.
Spontaneous irritability, not just when they do not get their way.
Frequent negative self-statements.
Self-injurious or self-destructive behaviors at times.
Anhedonia (i.e., experiencing little pleasure from things which most peers enjoy).
Elementary Child
Disruptive behavior.
Academic difficulties or declining school performance.
Frequent problems with peers.
Increased irritability and aggression compared to peers and to their own non-depressed state.
Suicidal threats & ideation
Anhedonia
Statements that they hate themselves and everything around them.
Sleeping too much.
Rapid, unpredictable emotional changes.
Physical complaints
Headaches
Stomach aches
Nausea
Vomiting
Adolescent Depression
About 20 percent of teens will experience teen depression before they reach adulthood.
Between 10 to 15 percent of teenagers have some symptoms of teen depression at any one time.
About 5 percent of teens are suffering from major depression at any one time
As many as 8.3 percent of teens suffer from depression for at least a year at a time
Most teens with depression will suffer from more than one episode. 20 to 40 percent will have more than one episode within two years, and 70 percent will have more than one episode before adulthood. Episodes of teen depression generally last about 8 months.
Acting-out behavior (missing curfews, unusual defiance)
Appetite changes (usually a loss of appetite but sometimes an increase)
Criminal behavior (such as shoplifting)
Depressed or irritable mood
Difficulty concentrating
Difficulty making decisions
Episodes of memory loss
Excessive sleeping or daytime sleepiness
Excessively irresponsible behavior pattern
Excessive or inappropriate feelings of guilt
Failing relations with family and friends
Faltering school performance
Substance abuse or use
Temper (agitation)
Thoughts about suicide or obsessive fears or worries about death
Weight change
Loss of interest in activities
Persistent difficulty falling asleep or staying asleep
Plans to commit suicide or actual suicide attempt
Preoccupation with self
Reduced pleasure in daily activities
Adolescent Suicides
9 of 10 adolescents who suicide give warnings
Depression
Substance use & abuse
Withdrawal
Decreased activity & attention
Lack of concentration
Sleep & appetite change
Suicidal ideation
Verbal & written suicidal cues
Giving away possessions
Low feelings of self worth
Relationship breakup
Gender identity crises
Low grades
Drop in grades
Suicide in friends or relatives
Drugs most common implement of death
Guns most frequent method for completed suicide
Hanging second method
Differences in males & females
Males die 5X more often, women think about & attempt 3X more often
Older Adults with Depression
Recent NIMH studies show that 13 to 27 percent of older adults have subclinical depressions that do not meet the diagnostic criteria for major depression or dysthymia (persistent depressive disorder in DSM 5) but are associated with increased risk of major depression, physical disability, medical illness, and high use of health services.
Depression in elderly people often goes untreated because many believe depression is a normal aging
Elderly people have challenges through loss, medical vulnerability and mortality of self and others.
Elderly people and families mistake symptoms of depression
Depression signs may be thought to be signs of:
dementia
Alzheimer’s disease
arthritis
cancer
heart disease
Parkinson’s disease
stroke
thyroid disorders
Symptoms in older persons differ from symptoms in other populations.
Depression in older persons is at times characterized by:
memory problems
confusion
social withdrawal
loss of appetite
weight loss
vague complaints of pain
inability to sleep
irritability
delusions
hallucinations
Older depressed individuals often have severe feelings of sadness, but these feelings frequently are not acknowledged or openly shown
Sometimes, when asked if they are depressed, the answer is “no.”
Some general clues that someone may be experiencing depression are:
persistent and vague complaints
help-seeking
moving in a slower manner
demanding behavior
Suicide is more common among the elderly than in any other age group. In studies of older adults who committed suicide, nearly all had major depression, typically a first episode, though very few had a substance abuse disorder.
Suicide among white males aged 85 and older was nearly six times the national U.S. rate (65 per 100,000 compared with 11 per 100,000) in 1996, the most recent year for which statistics are available.
Suicide in Elderly
National Institute of Mental Health
Older Americans are disproportionately likely to die by suicide.
Of every 100,000 people ages 65 and older, 14.3 died by suicide in 2007. This figure is higher than the national average of 11.3 suicides per 100,000 people in the general population.
Non-Hispanic white men age 85 or older had an even higher rate, with 47 suicide deaths per 100,000
American Association of Suicidology
The elderly made up 12.5% of the population; they accounted for almost 15.7% of all suicides.
The rate of suicide for the elderly for 2007 was 14.3 per 100,000.
There was one elderly suicide every 97 minutes. There were about 14.9 elderly suicides each day, resulting in 5,421 suicides in among those 65 and older.
Elderly white men were at the highest risk with a rate of approximately 31.1 suicides per 100,000 each year.
Suicide
From the Span USA website:
“More than 34,500 Americans die by suicide each year (CDC)
There is 1 suicide every 16 minutes and 89 suicides per day (CDC)
24% of the general population has considered suicide at some time in his/her life (Linehan et al., 1982)”
Suicide is the:
11th leading cause of death overall in America (CDC)
3rd leading cause of death for young Americans between the ages of 10-24 (CDC)
Each suicide produces at least six, and as many as hundreds of “survivors,” or people left behind to grieve.
Suicide Rates by Age
In 2016, the highest suicide rate (19.7) was among adults between 45 and 54 years of age.
The second highest rate (19.0) occurred in those 85 years or older.
Younger groups have had consistently lower suicide rates than middle-aged and older adults.
In 2016, adolescents and young adults aged 15 to 24 had a suicide rate of 12.5.