Exam 2
1/161
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
162 Terms
What is the leading cause of death in individuals 5 - 34 years of age?
car crashes
What are some examples of primary prevention in trauma?
Seatbelts
Helmets
Why is early intervention key in the care of a trauma patient?
first 10 mins-1hr largely determine patient outcome
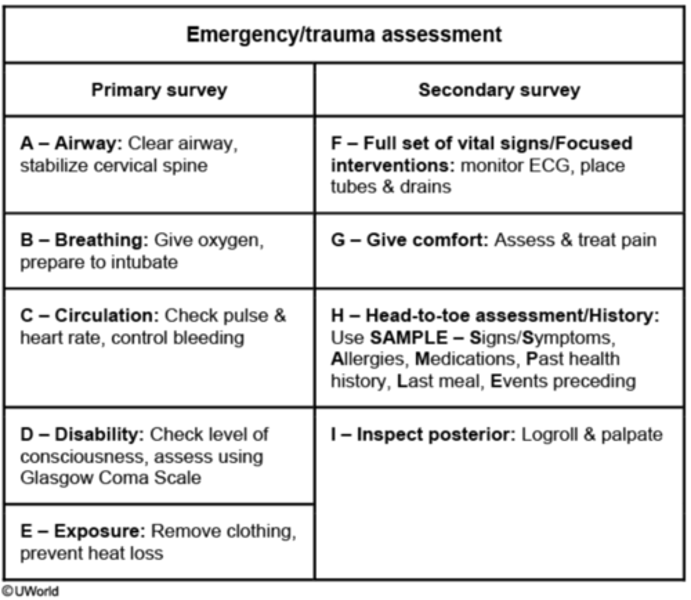
Describe the steps in the trauma primary survey.
What is the role of the nurse in the trauma bay during the primary survey?
Vital signs
IV and drugs
Transfusions
Foley, Gastric tube, etc
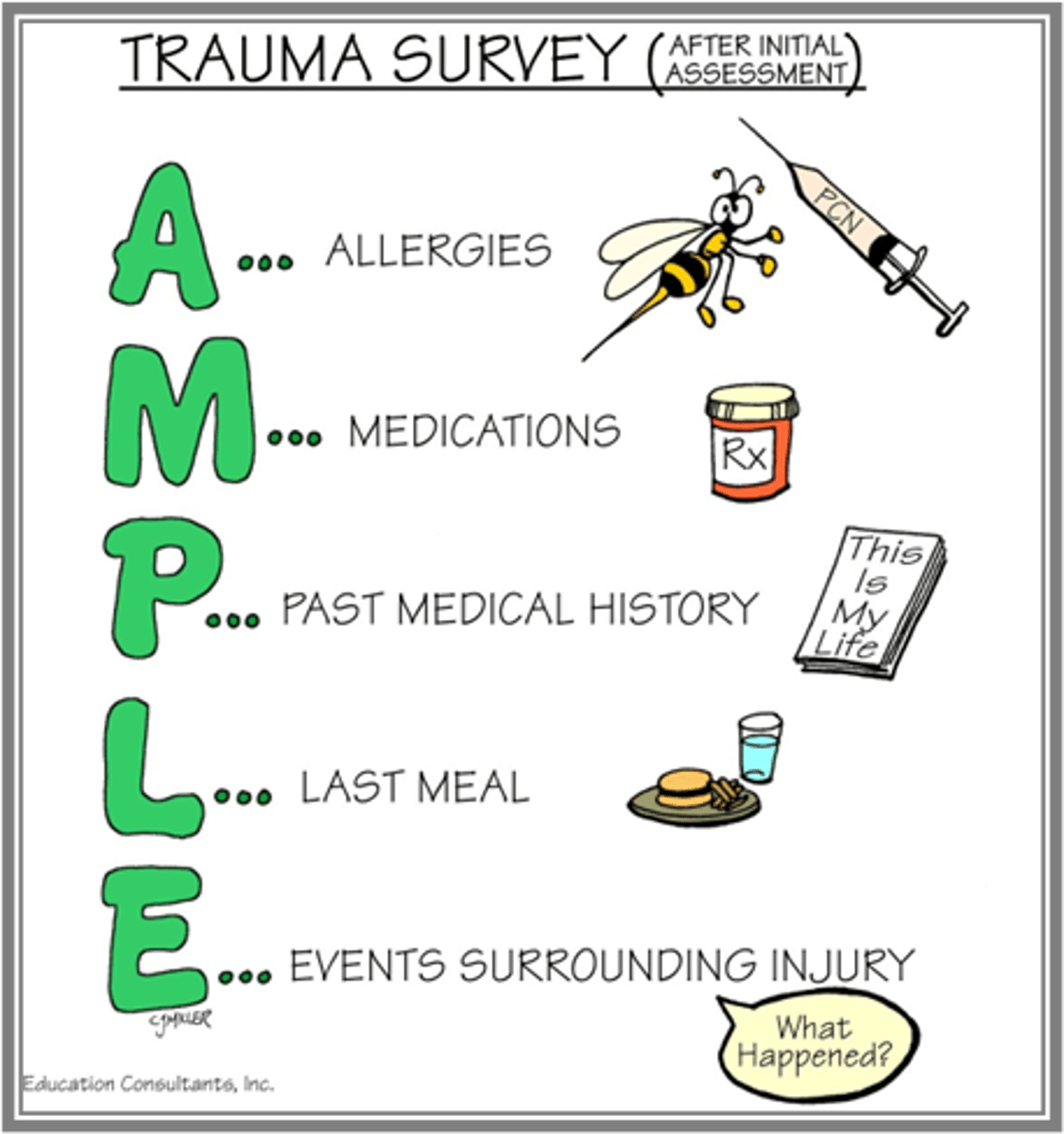
Describe the trauma secondary survey.
Physical Examination
What is the role of the nurse during the secondary survey?
Assessment
repositioning
Documentation
List potential causes of blunt abdominal trauma.
Injury caused by blunt force
-MVC (motor vehicle crash)
-MCC (motorcycle crash)
-Pedestrian vs car
-assault w blunt force
-fall
List potential causes of penetrating abdominal trauma.
Penetrating Ab trauma
-stab wound
-gunshot wound
Emergent management of abdominal trauma
Fast= Assessment in peritoneal bleeding
-in an unstable patient
=+ FAST = OR
=- FAST = CT
-In a stable patient
= + FAST = CT
= - FAST = Stop, repeat FAST, CEUS, CT or Observation
Identify common injuries associated with blunt abdominal trauma.
Liver laceration
Splenic laceration
Renal laceration
Bowel hematoma
Pelvic hematoma
Retroperitoneal hematoma
Management of blunt abdominal trauma
Unstable = SPB
Management of Penetrating Abdominal trauma
Unstable
-OR
Stable
-Stab wound
=CT scan
-GSW
=X-ray
--Through and through -> CT scan
--All other injuries -> OR
Describe the pre-operative nursing management priorities of abdominal trauma.
-Prep for surgery
-Fluid resuscitation
-Protection of ABCs
-Management of Pain
-Frequent abdominal assessments
=Observe for abdominal distention
=palpate for pain and firmness
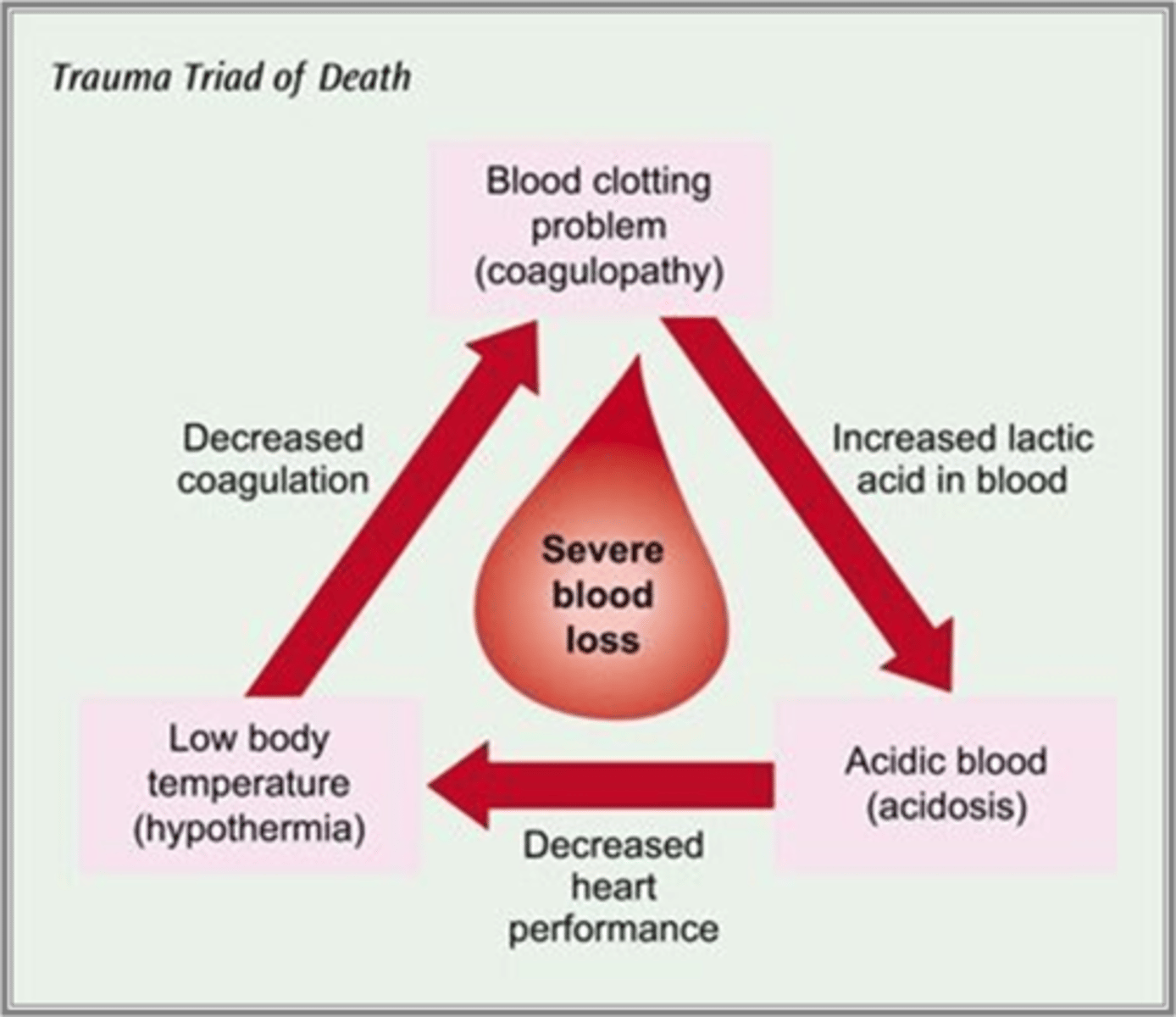
-Prevention of lethal triad
Explain the trauma triad of death.
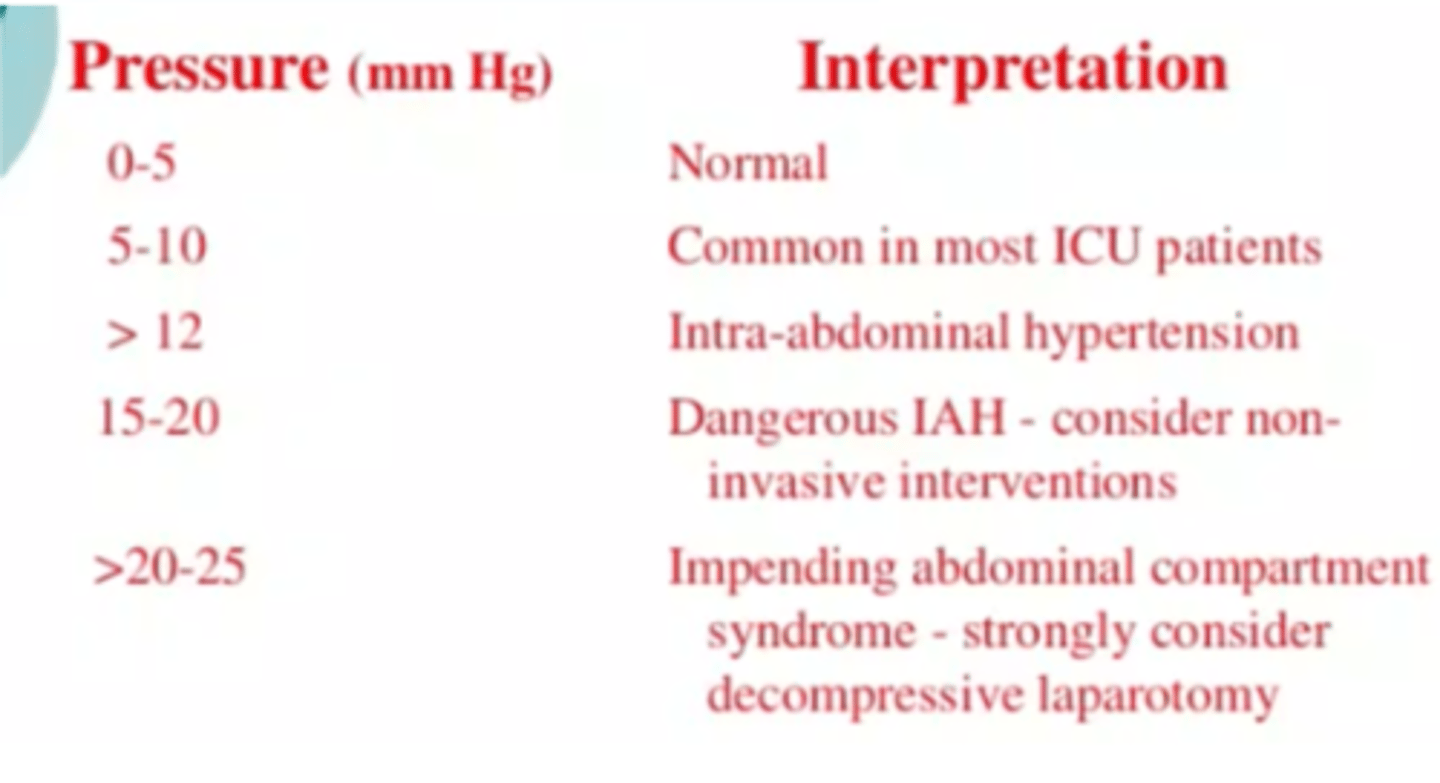
What is the significance of intraabdominal pressure monitoring?
-used to identify children at risk of intra-abdominal hypertension (IAH) and abdominal compartment syndrome (ACS)
-IAH & ACS are most likely to occur in the setting of major fluid resuscitation, severe gut oedema, intra-peritoneal or retroperitoneal bleeding, or ascites
Describe the post-op nursing management associated with abdominal trauma.
Respiratory
Cardiovascular
Hematologic
Gastrointestinal
Surgical site
Respiratory Management
-Airway patency
-monitor vitals
-position patient to ensures optimal lung expansion
-Monitor color and character of secretions
=suction as needed
Cardio management
Maintain hemodynamic stability
-Monitor VS
-Frequent assessment of peripheral vascular system
-monitor mental status
-Provide fluid resuscitation
=Crystalloid
---IV fluids-> LR or NS 20-30 ml/kg
=colloid
---bleeding?-> Give them back what they are losing
-monitor I and o
Vasopressors
signs of decreased perfusion
CNS/Brain
-restless or anxious at first then agitated or confused
Cardiac
-Increased HR and decreased BP
GI
-Decreased motility progressing to then ileus and finally mesenteric ischemia if very low perfusion
Renal
-decreased urine output progressing to oliguria and finally anuria
Skin
-decreased cap refill -> cold extremities and finally mottled cyanotic cold extremities
hematologic managment
Prevent trauma triad of death
-STOP the bleed
-keep the patient warm
=covered
=warm blanket or electric warming blanket
=keep room temp high
-admin fluids
=both crystalloid and colloid and ensure they're warm
-Monitor and maximize oxygenation
GI system
-Abdominal Assessment
• Observe for increasing abdominal distention
• Auscultate for bowel sounds (will likely be hypoactive or absent)
• Palpate
-Trend bladder pressures
• Measures the intra-abdominal pressure
= Considered reliable only when patient is heavily sedated or chemically paralyzed
-Nutrition
• Early involvement of Nutrition Team
• Advocate for 1.5 - 2.5 g/kg/day of protein to start
• Monitor nutritional status with weekly labs (albumin, pre-albumin, c-reactive protein)
• Monitor and replace electrolytes
• Weigh patient daily
• If contraindications to TEN exist, advocate for patient to start TPN within 48 hours of initial damage control procedure.
Incision assessment
• Incision Assessment
• Midline incision with full abdominal closure
• Partial closure (i.e.: fascial closure but skin remains open)
• Open abdomen with ABThera, VAC or other closure device
Indications for open abdomen
• Indications for the open abdomen:
• Damage control surgery
• Abdominal compartment syndrome
• Massive fluid replacement
• Requirement for second-look surgery
• To assess bowel viability or to evaluate and treat continued intra-abdominal contamination
Explain the potential complications in abdominal trauma.
Abdominal Compartment Syndrome
Renal Injury
Infection
What is abdominal compartment syndrome?
• Condition caused by abnormally increased pressure within the abdomen that is associated with organ dysfunction
• Risk factors
=Trauma
= Surgery
= Infection
Abdominal Compartment syndrome clinical manifestations
• Abdominal distention worsening to tense, rigid abdomen
• "Washboard-like"
• Abdominal pain out of proportion to injury
• Tachypnea and/or dyspnea
Abdominal Compartment syndrome treatment
• Need to relieve the pressure!
• EMERGENCY that needs to go to the OR immediately for exploratory laparotomy
Renal injury complications
Causes AKI
• Pre-Renal
• Secondary to impaired perfusion (i.e.: hypovolemic shock)
• Intra-Renal
• Secondary to prolonged hypotension
• Toxins such as antibiotics and IV contrast dye
Renal injury interventions
• Monitor urine output
• Inform provider if patient produces < 0.5 mL/kg/hr
• Obtain labs as ordered
• Monitor creatinine, BUN, and electrolytes
MODS (multiple organ dysfunction syndrome)
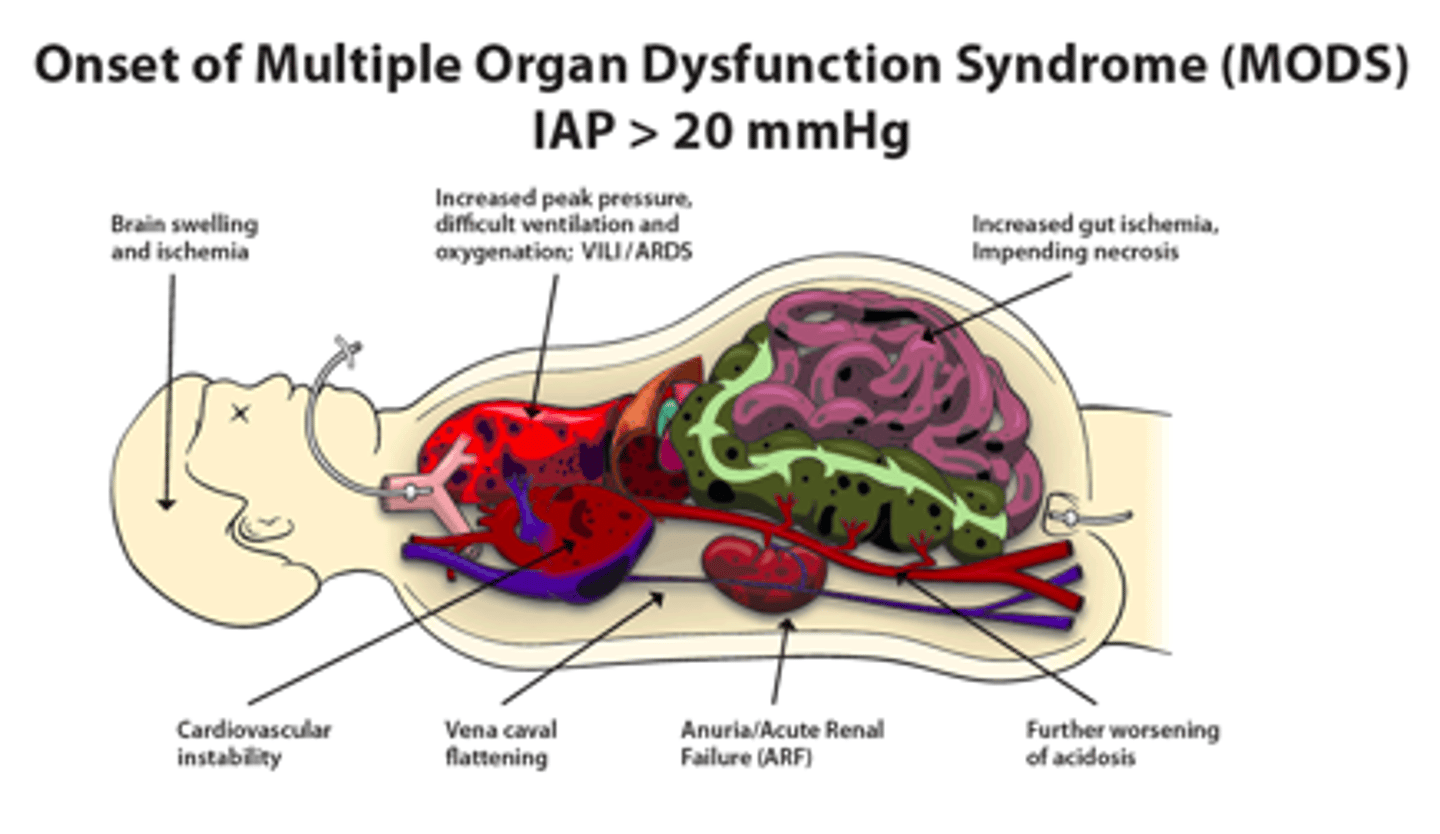
What intraabdominal pressures are most concerning?
Infection complications
• Prevent & Treat
• Monitor for the following signs:
• S - shivering, or fever
• E - extreme pain or general discomfort
• P - pale or discolored skin
• S - sleepy, difficult to arouse, confused
• I - statements such as "I feel like I might die"
• S - shortness of breath
Antibiotics prophylaxis vs treatment
• Prophylaxis example -> Patient had surgery and they're ordered for a 24 hr dose of antibiotics
• Treatment example -> Patient has active or suspected infection, the antibiotics ordered should be intended to actively treat that infection.
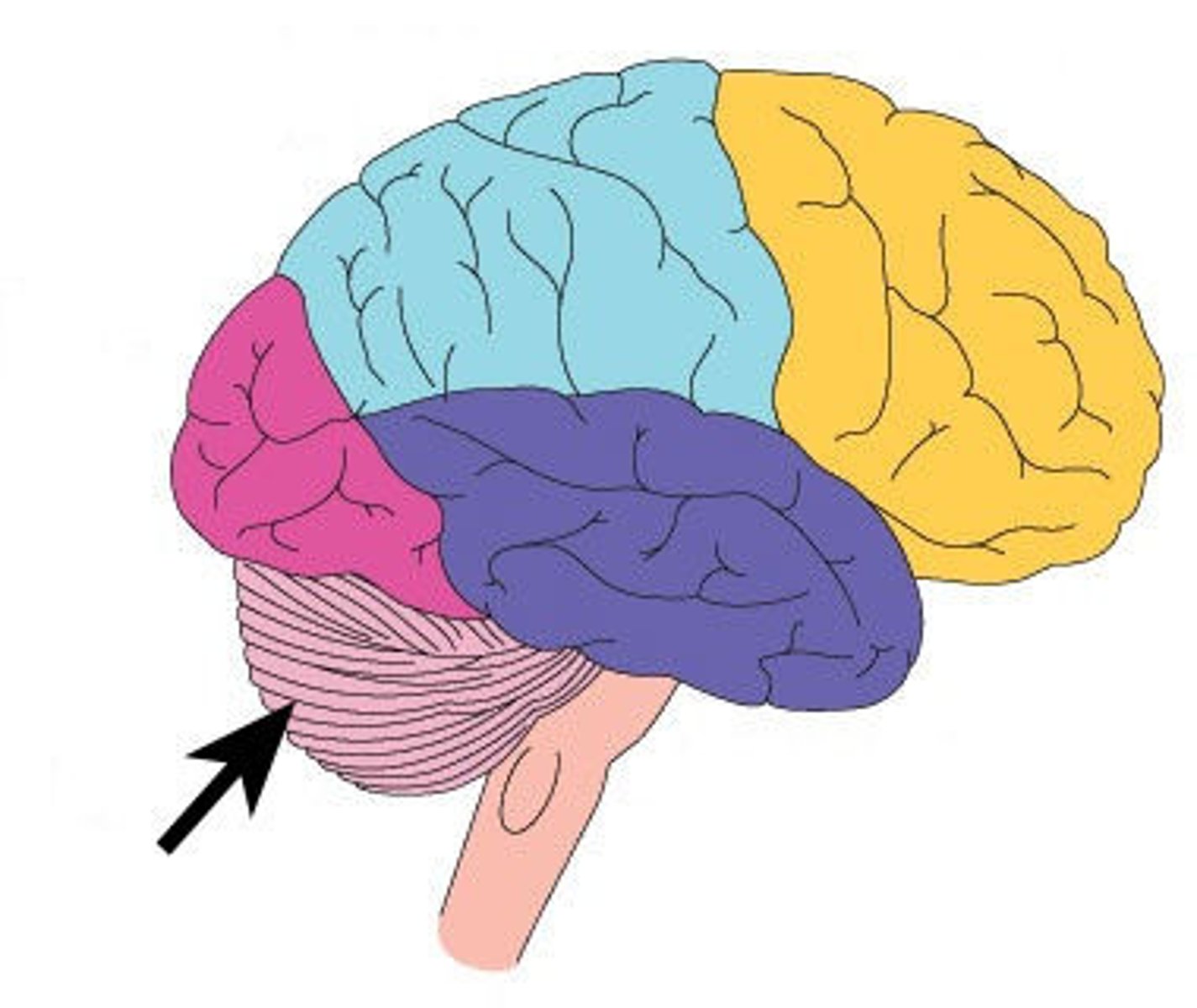
frontal lobe
A) associated with reasoning, planning, parts of speech, movement, emotions, and problem solving
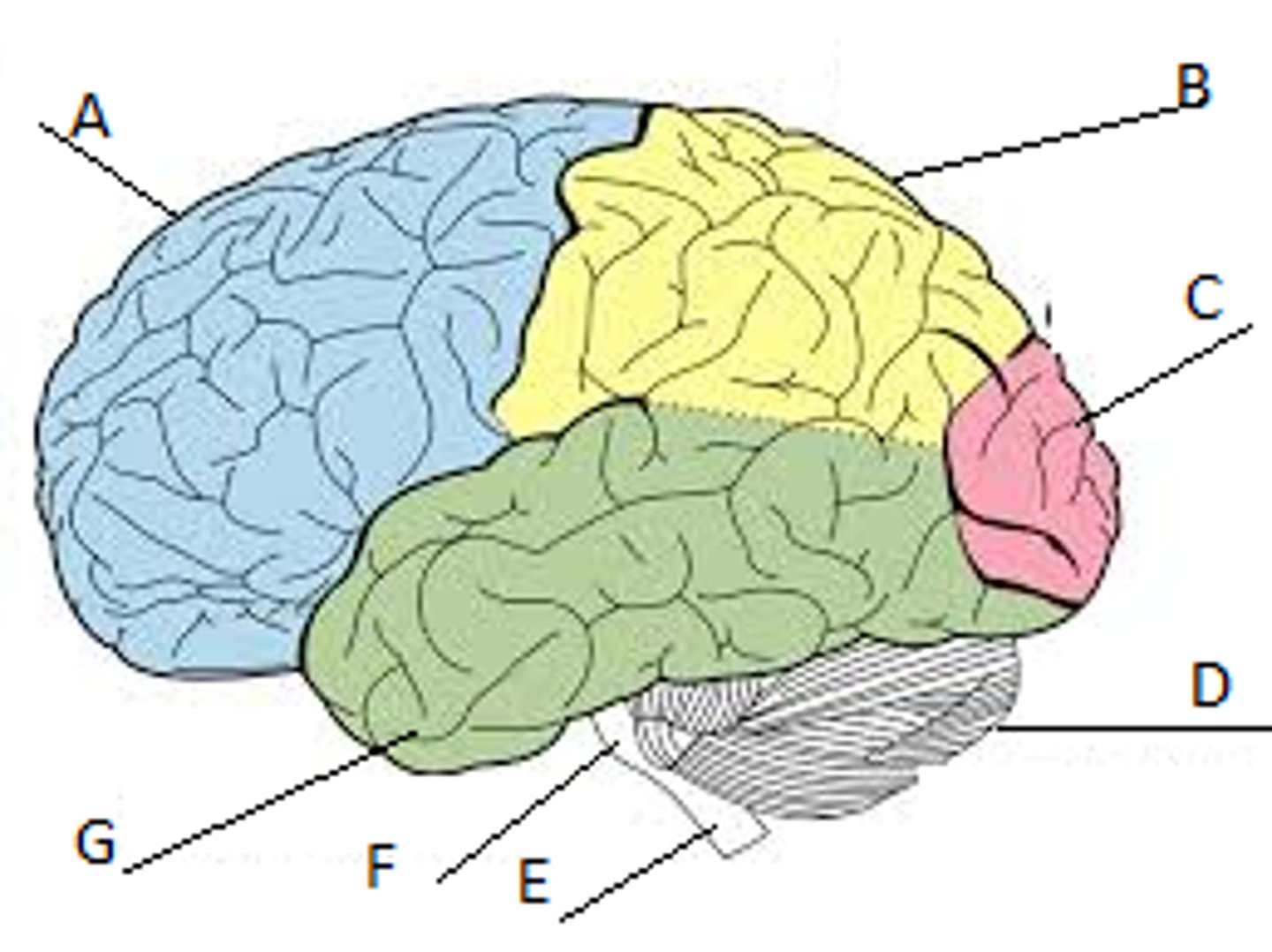
parietal lobe
B) receives sensory input for touch/pressure, body position, taste
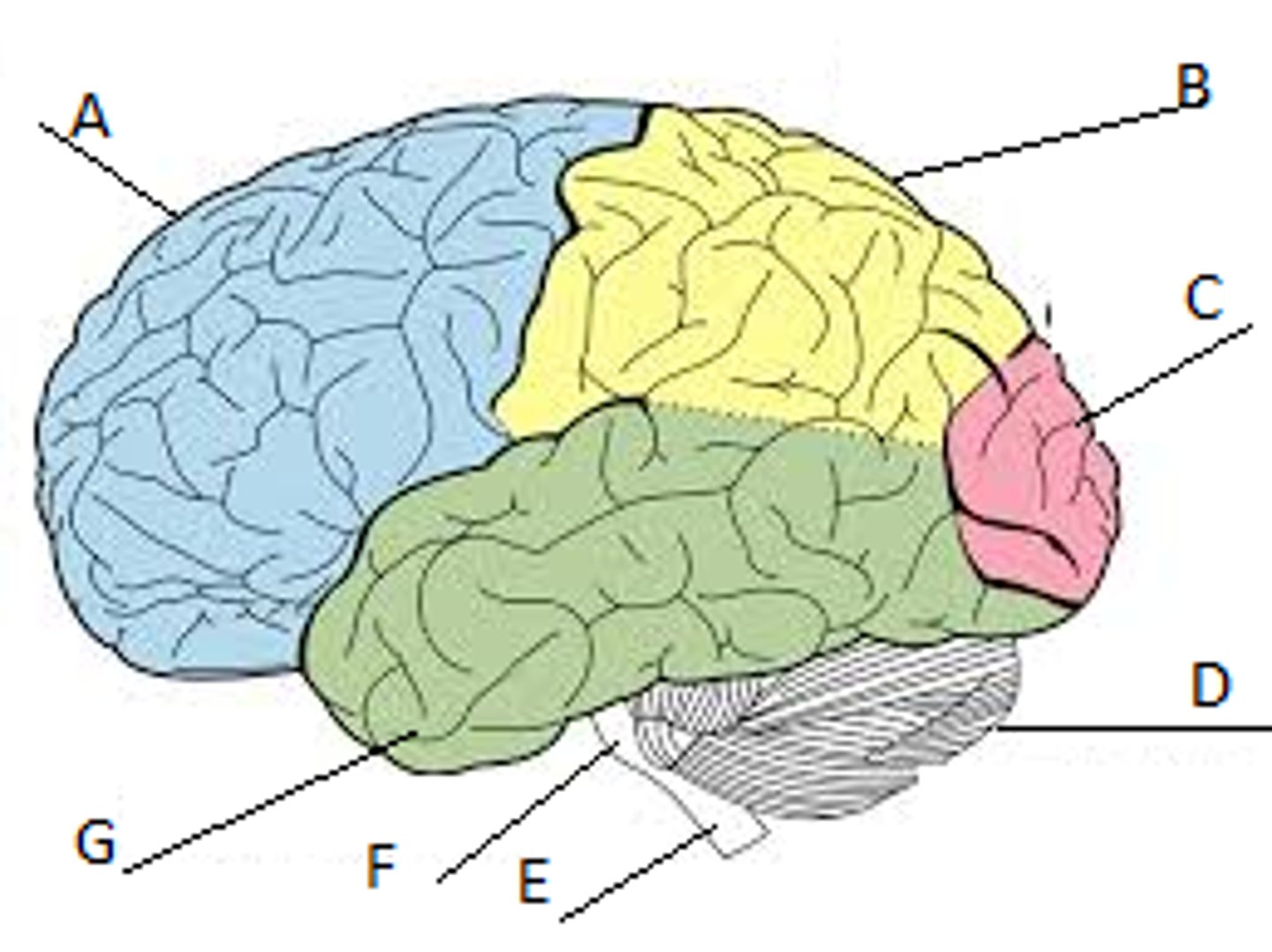
temporal lobe
G) A region of the cerebral cortex responsible for hearing and facial recognition.
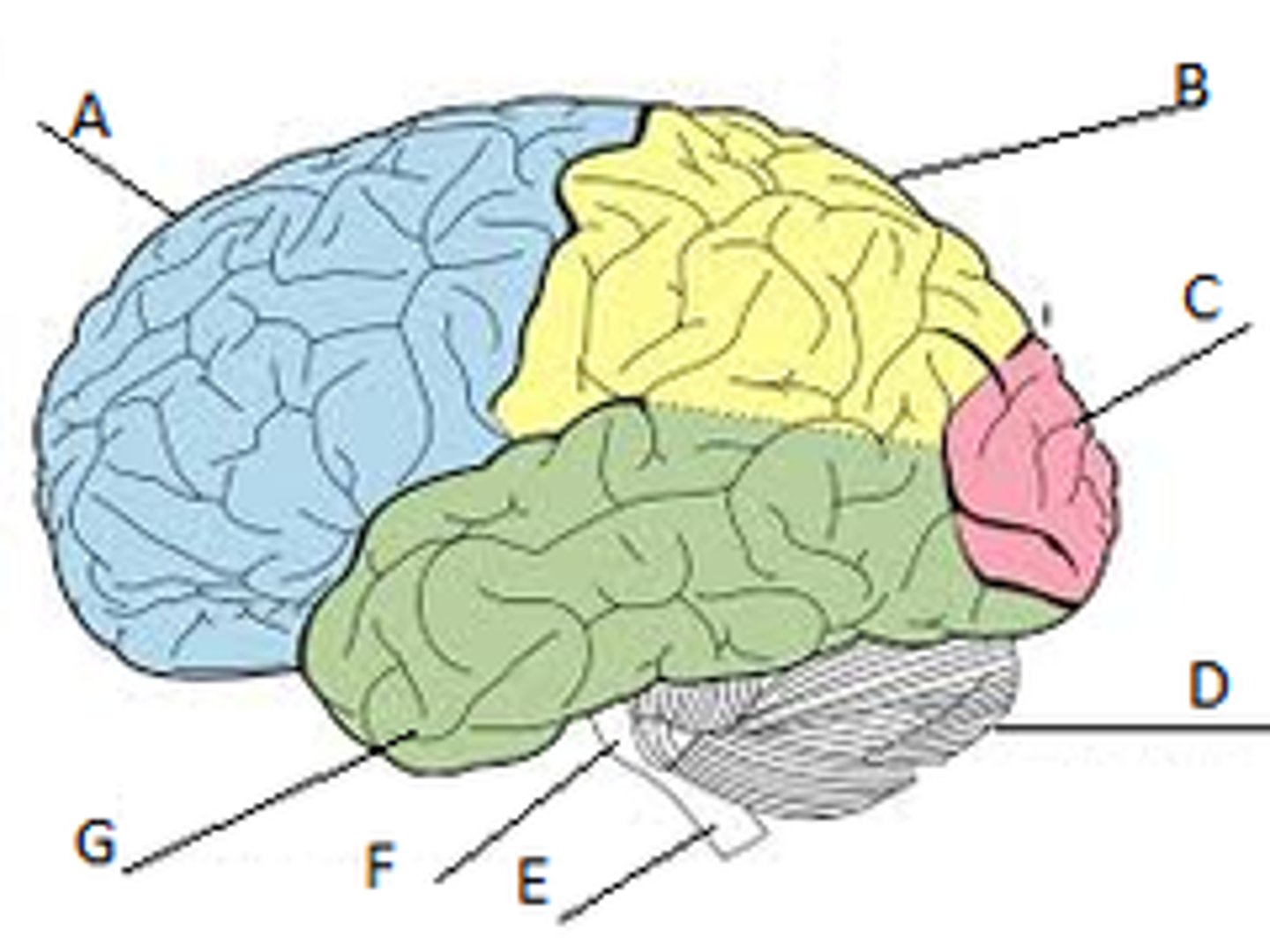
occipital lobe
C) A region of the cerebral cortex that processes visual information
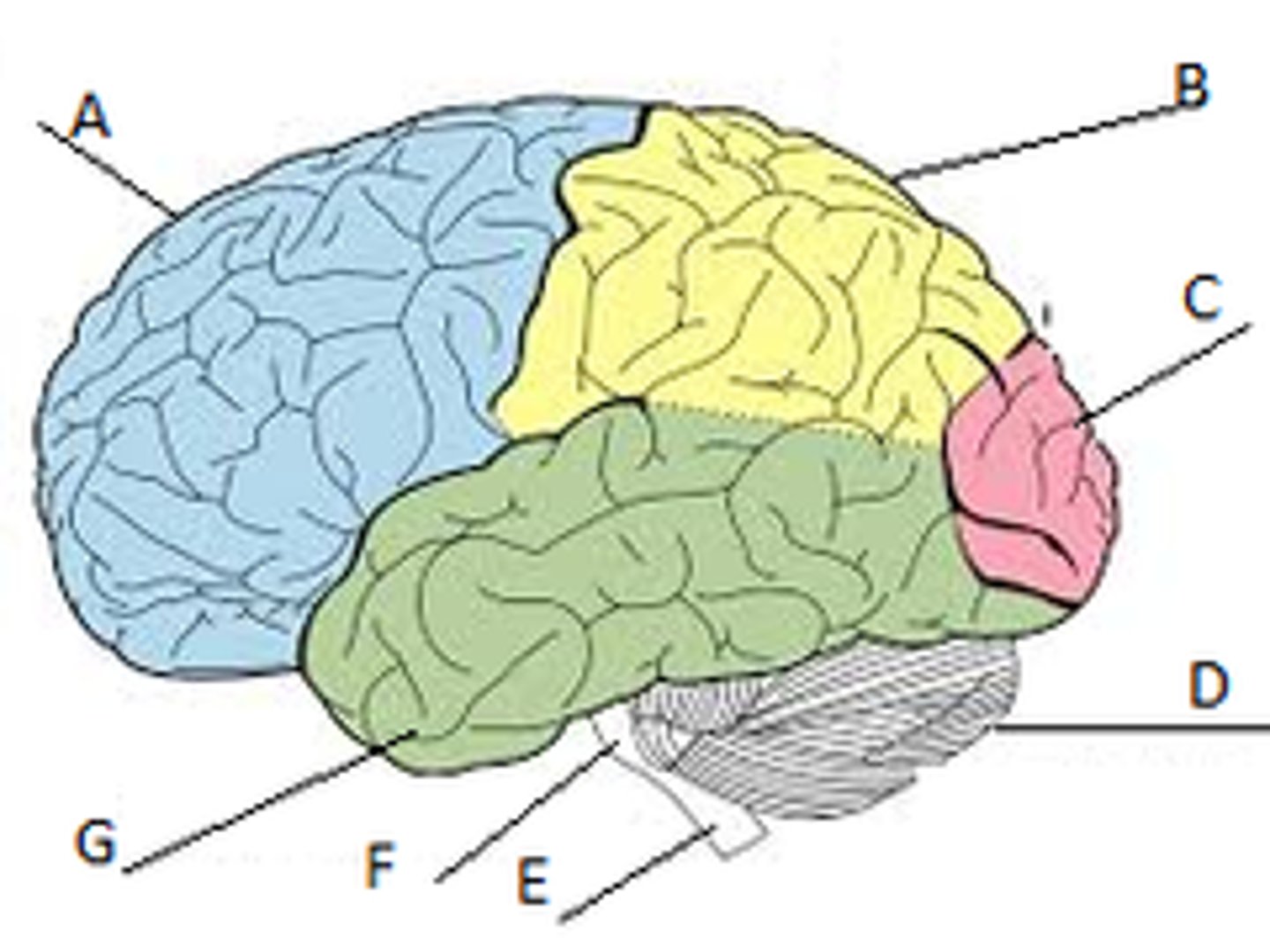
Cerebellum
A large structure of the hindbrain that controls fine motor skills/coordination.
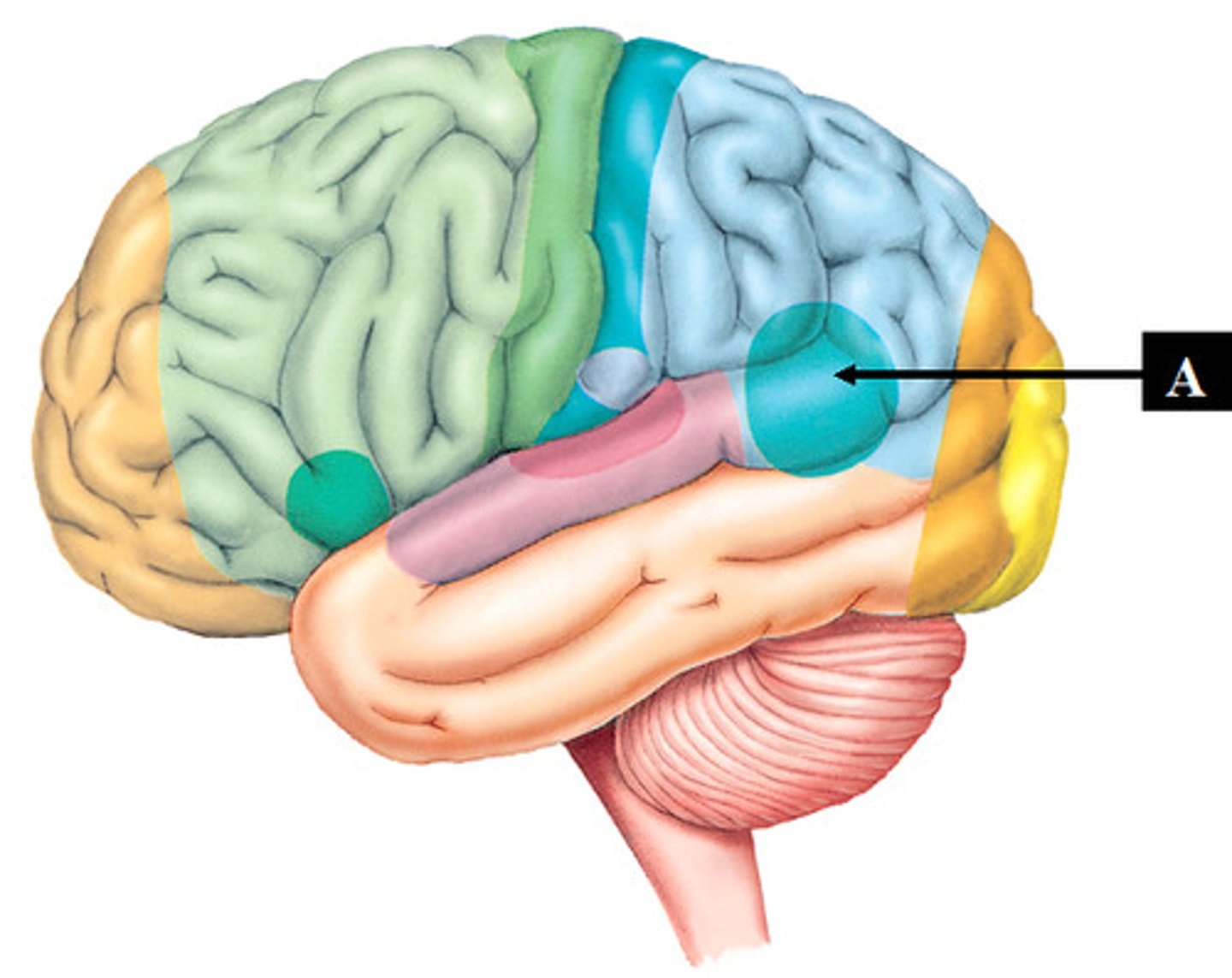
Wernicke's area
a brain area involved in language comprehension, expression, and reading; usually in the left temporal lobe
What counts as brain trauma?
• Penetrating
• Concussion
• Acceleration & Deceleration
• Diffuse Axonal Injury
• Hematomas & Hemorrhages
• SDH
• Epidural Hematoma
• ICH, SAH
What is a non-traumatic brain injury?
• Non-traumatic:
• Tumor
• Stroke: Ischemic and Hemorrhagic
• Infection: meningitis, ventriculitis
• Seizures
• Encephalitis (inflamed brain)
• Anoxic
ASSESSMENT
• ABC...DE (disability, exposure/environment) if trauma
• Neurological Exam
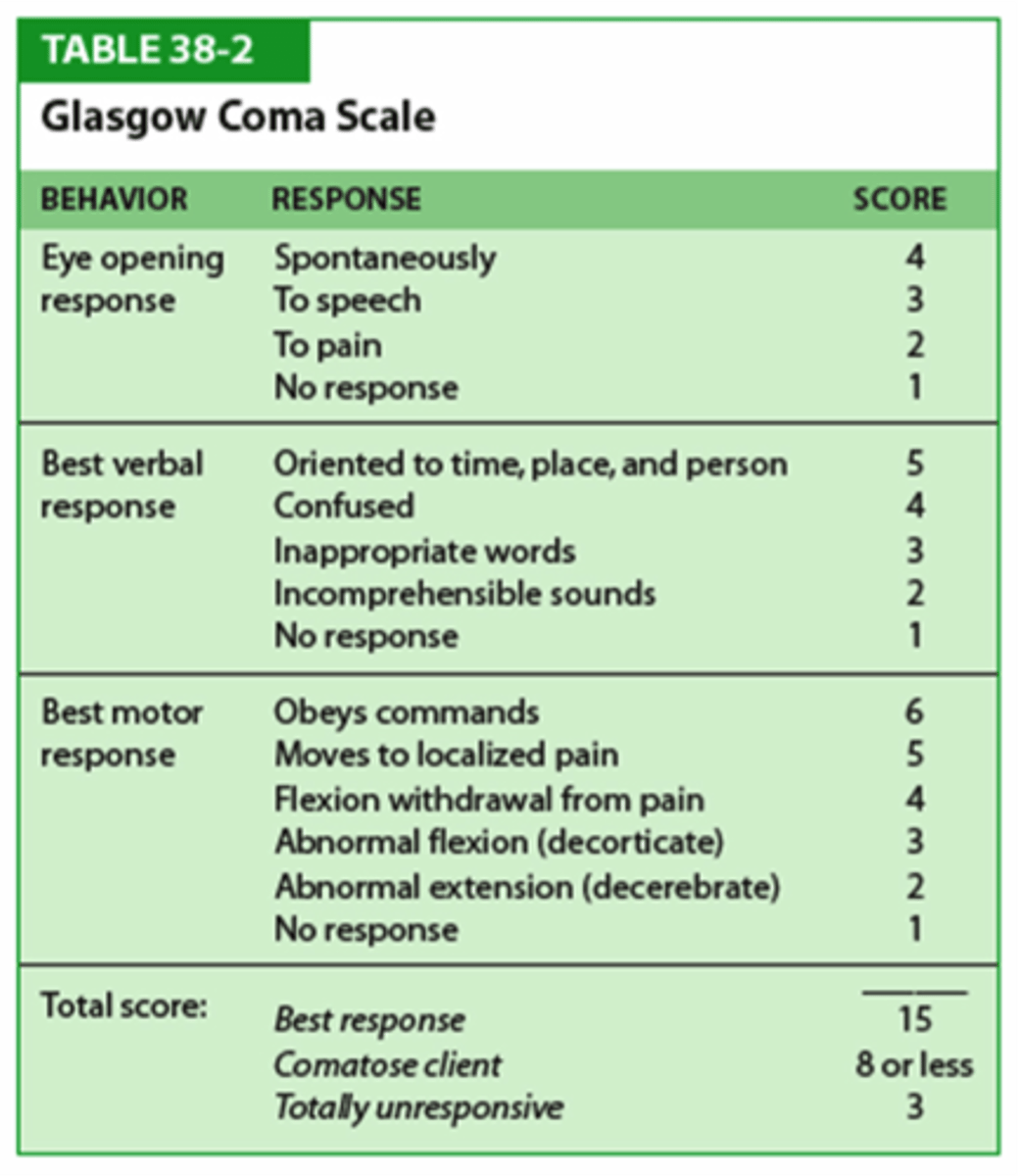
• GCS (GCS
GCS
less than 8, intubate
OBJECTIVE level
Cranial nerves
1-12
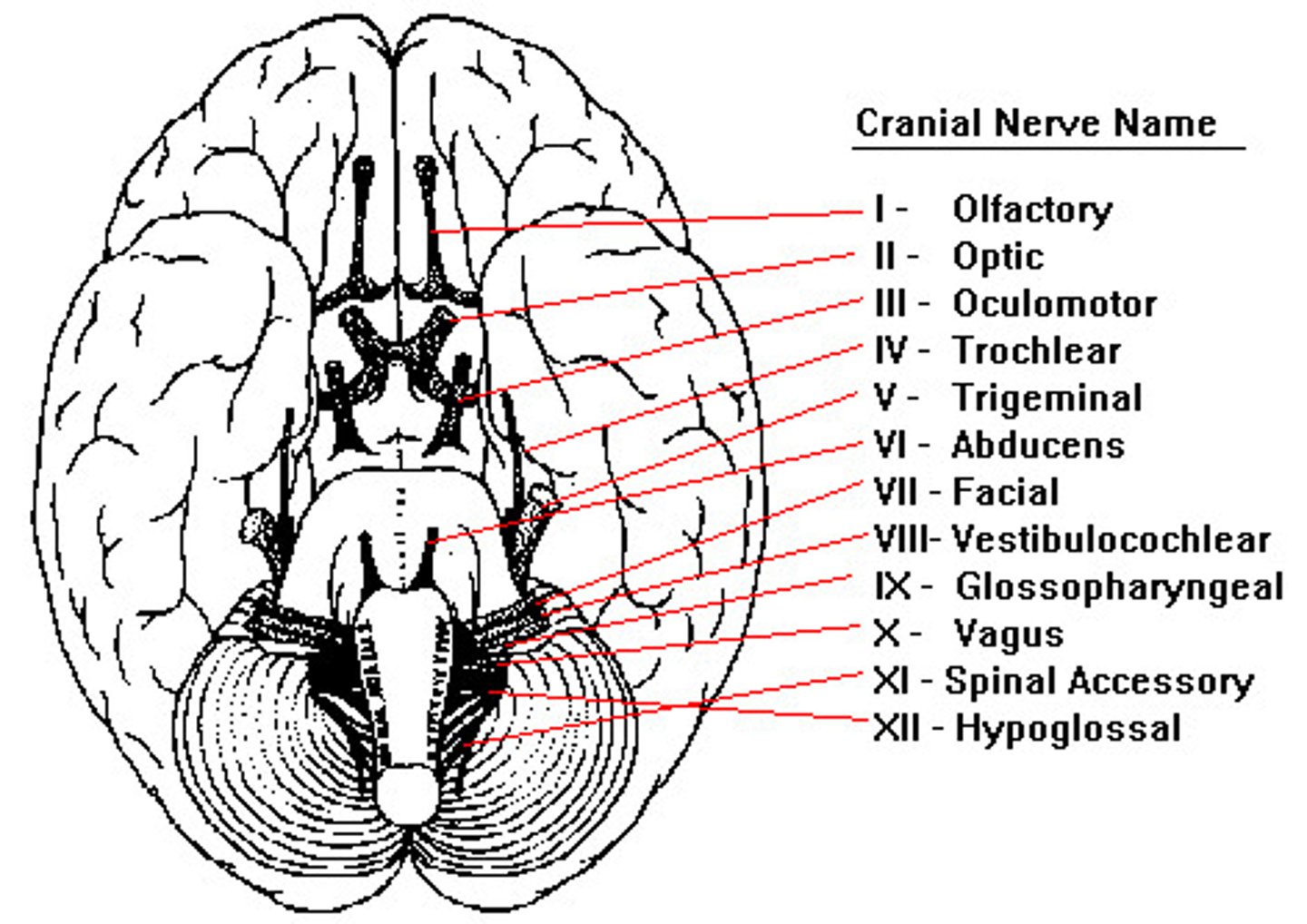
Pupil dilation warnings
• Pupils: CN II & III = midbrain
• Unilateral dilated pupil= mass effect on temporal lobe, or possible epidural hematoma, increased ICP
• Bilateral fixed/dilated= Cerebral herniation and brain stem injury...bad
How does POSTURING= SEVERE BRAIN DAMAGE?
Decorticate (Flexor) Posturing- Damage to cerebral hemispheres
Decerebrate (Extensor) Posturing-deeper brain structures, including midbrain, pons, brain stem
Battle's sign
Bruising behind the ears, indicative of a basilar skull fracture

Raccoon eyes
Bruising around the eyes, indicative of a basilar skull fracture

Symptoms of Brain Injury
MILD
• LOC for secs to mins or none but state of being dazed/disoriented
• Headache
• N/V
• Fatigue
• Speech problems
• Dizziness
MODERATE TO SEVERE
• LOC for several mins to hours
• Headache
• Repeated N/V
• Seizures
• Dilation of one or both pupils
• Clear fluids from nose or ears
• Weakness
• Agitation
• Slurred Speech
• Coma (GCS
What are some compensatory mechanisms of cerebral compliance? Why is this important to know?
-capability to buffer an intracranial volume increase while avoiding a rise in intracranial pressure (ICP).
-The autoregulatory response to Cerebral Perfusion Pressure (CPP) variation influences cerebral blood volume which is an important determinant of compliance.
Describe normal cerebral metabolism.
Cerebral O2 consumption in normal, conscious, young men is approximately 3.5 ml/100 g brain/min
What is traumatic brain injury (TBI)?
A traumatic insult to the brain capable of producing physical, intellectual, emotional, social, and vocational changes.
What are classifications of TBI?
• Open (Penetrating) vs. Closed (Closed-head)
• Primary (moment of initial injury) vs. Secondary (complications)
• Mild, Moderate, Severe TBI
What are types of TBIs?
• Concussion
• Acceleration & Deceleration
• Diffuse Axonal Injury
• Hematomas & Hemorrhages
• SDH
• Epidural Hematoma
• ICH, SAH
Penetrating injury
• Penetrating injury= A head injury in which the dura mater (outer layer of the meninges) is breached
• Less common than closed head trauma but worse prognosis
• Penetrating- foreign object penetrates and remains lodged
• Tangential- foreign objects glances off skulls driving bone fragments into the brain
• Perforating- "Through and through"
• **Most common is GSW (40-60% of GSW die before reaching the hospital; 51% who do will survive)
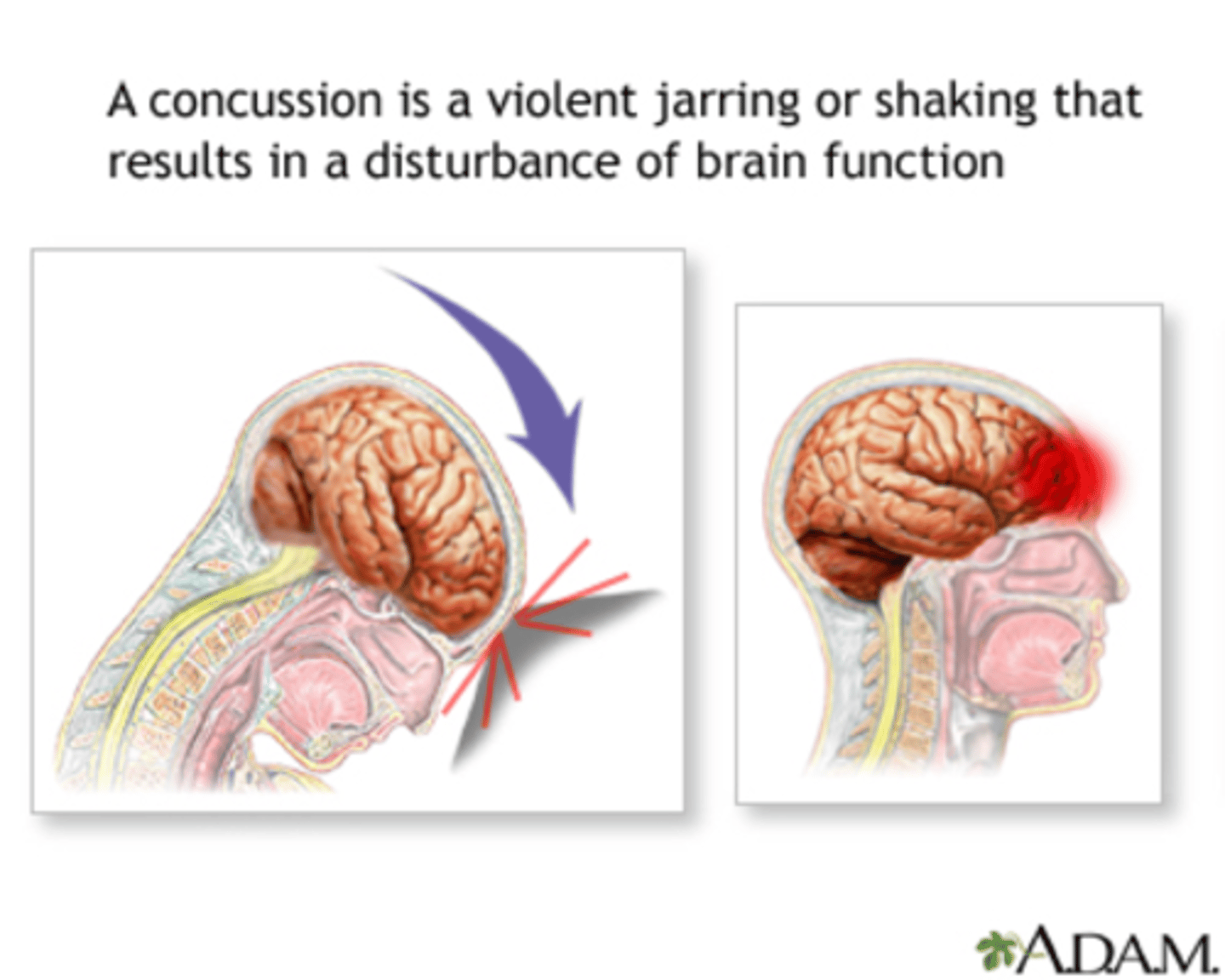
Concussion Injury
• Low velocity injury resulting in functional deficit without pathological injury
• Most common symptoms is headache
• Neuroimaging is typically normal
• Recovery from symptoms within 7 days to 6 weeks
• Balance and coordination may be affected
• CDC estimates 1.6-3.8 Million sports related concussions annually in the US
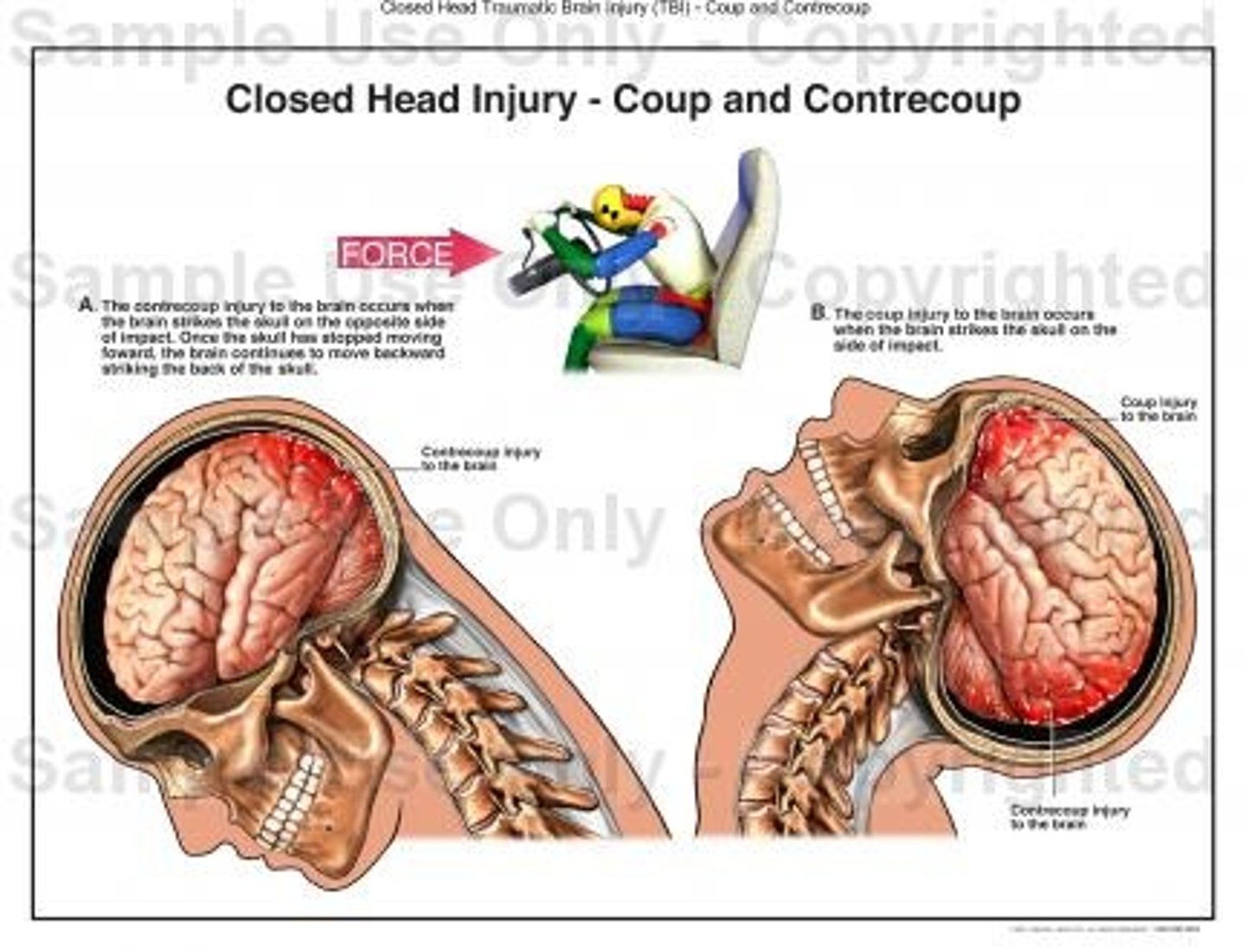
ACCELERATION & DECELERATION INJURIES
• Coup: Site of impact with blunt object
• Contrecoup: Opposite the area of impact
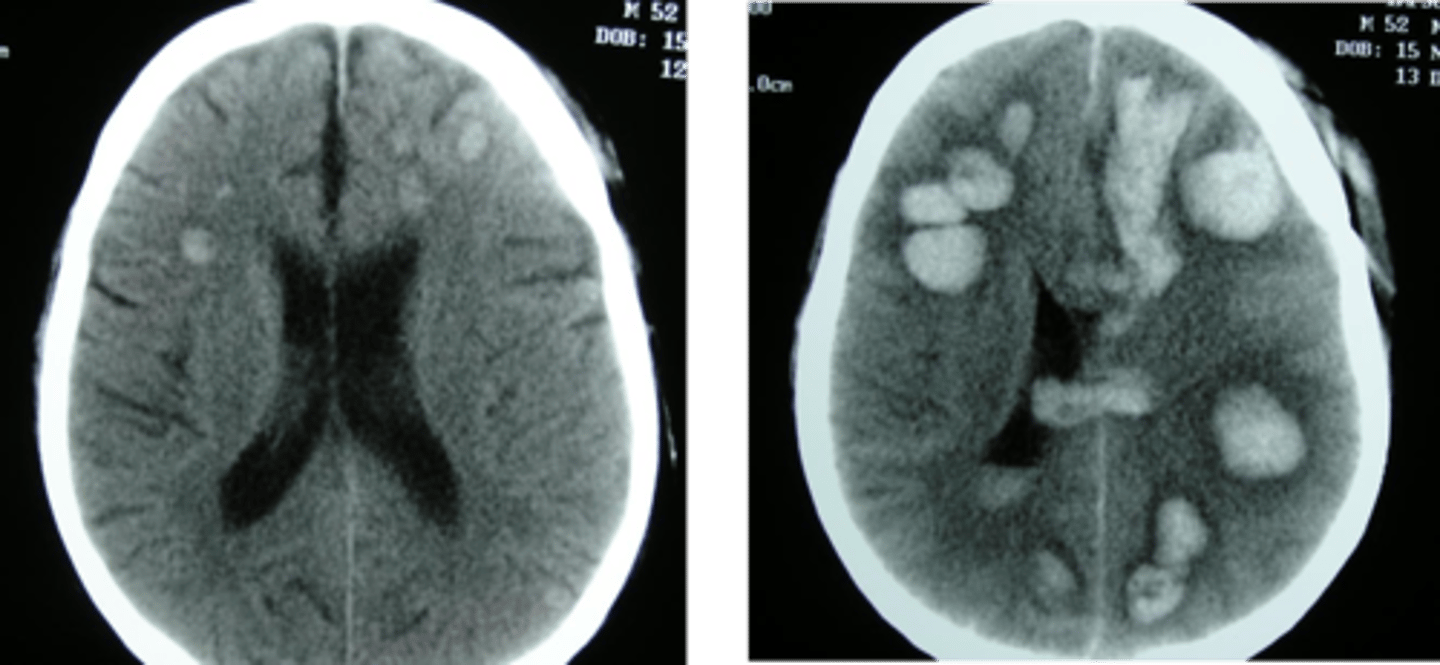
DAI (DIFFUSE AXONAL INJURY)
• Long connecting fibers in the brain (axons) are sheared as the brain accelerates and decelerates
• Causes injury to many places in the brain
• Patients are often in a coma without obvious lesion on CT scan; punctate hemorrhages can be seen on MRI
• Poor outcomes
Bleeds
• Epidural (EDH)
• Subdural (SDH)
• Subarachnoid (SAH)
• Intracerebral (ICH)
• Intraparenchymal (IPH) & Intraventricular (IVH)
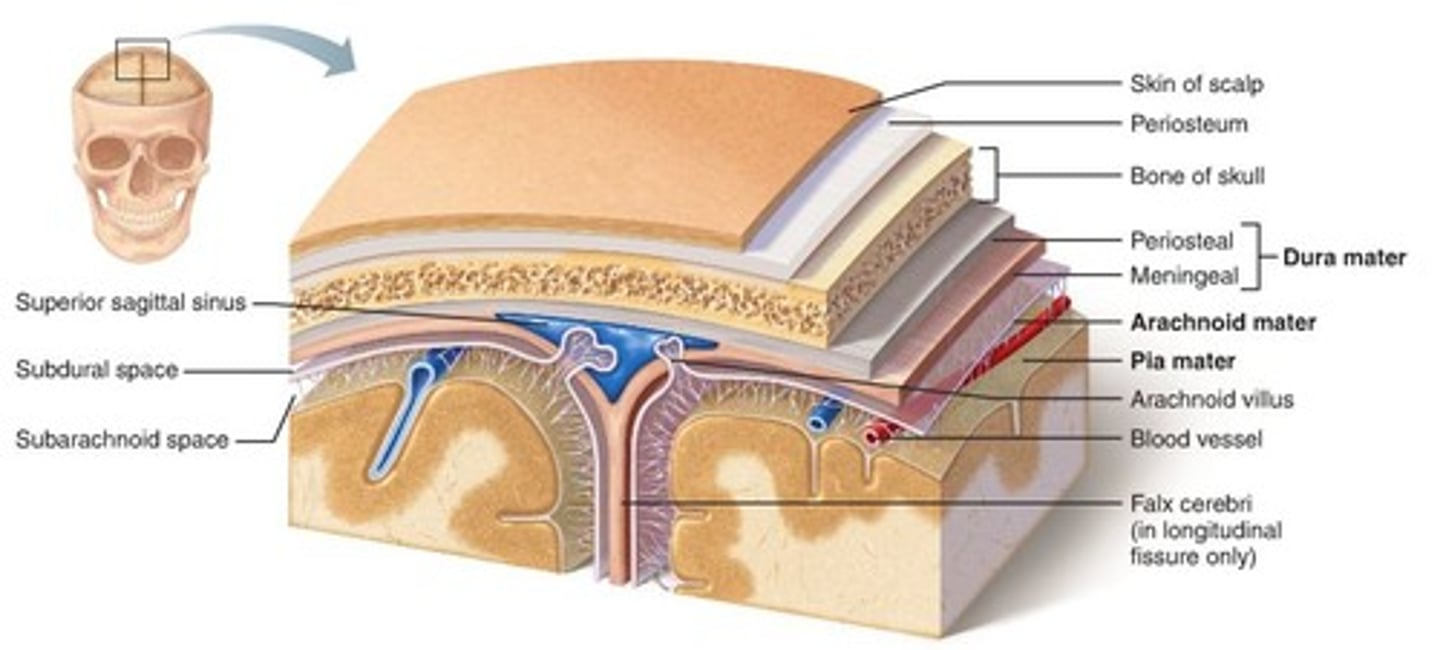
CEREBRAL HEMORRHAGES (HEMATOMAS)
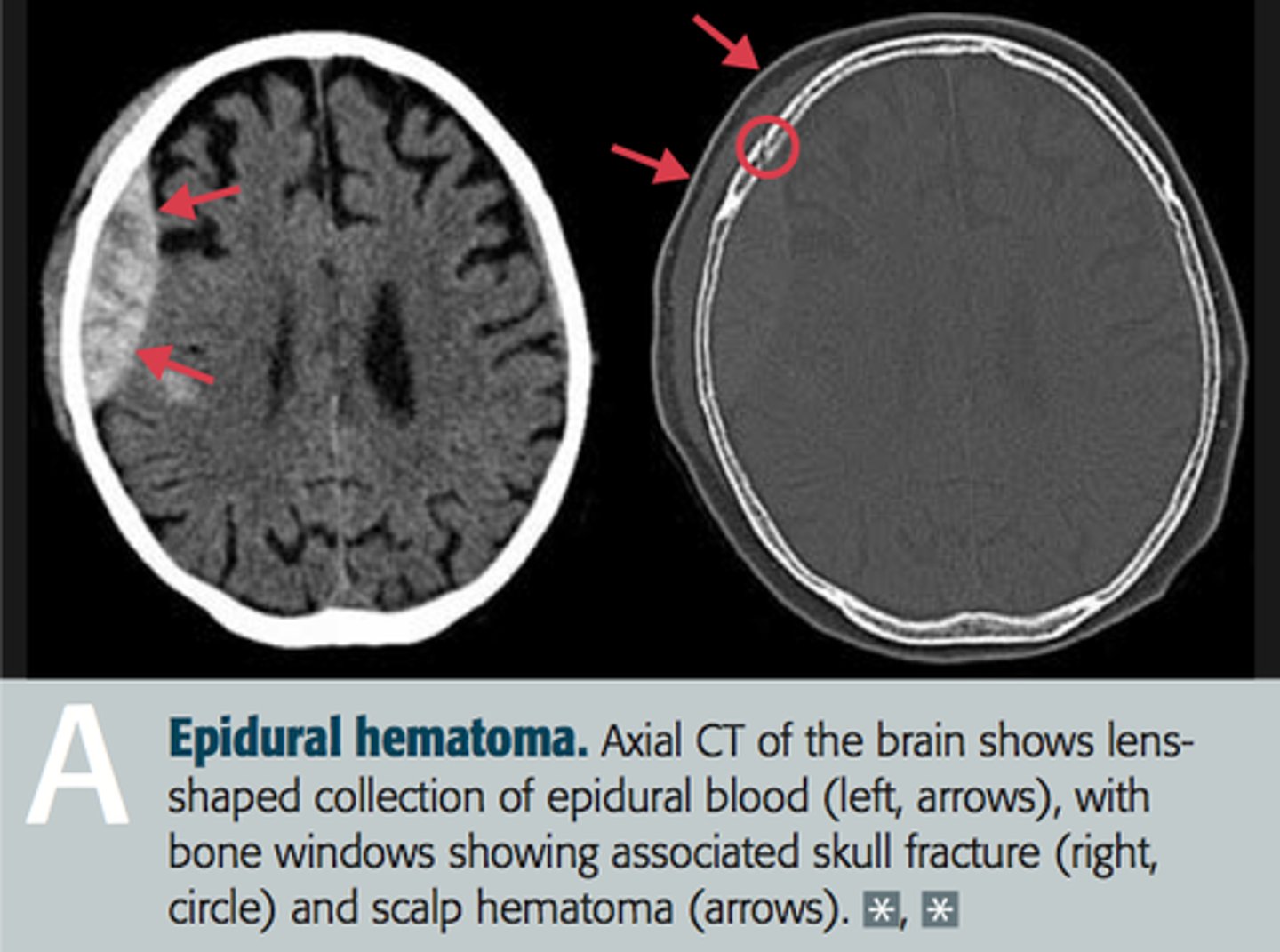
• Epidural Hematomas-
• between skull and dura
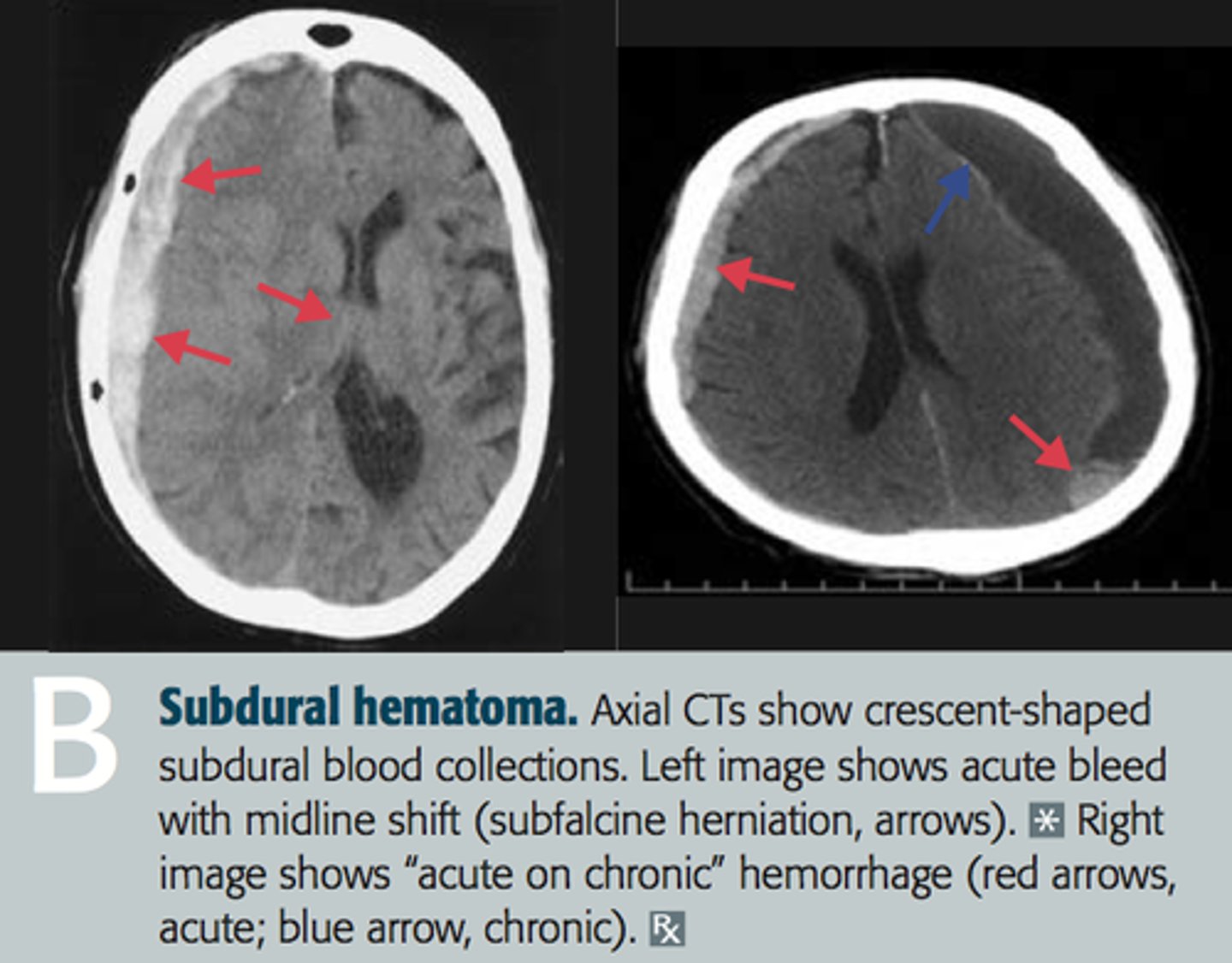
• Subdural Hematomas-
• between dura and arachnoid
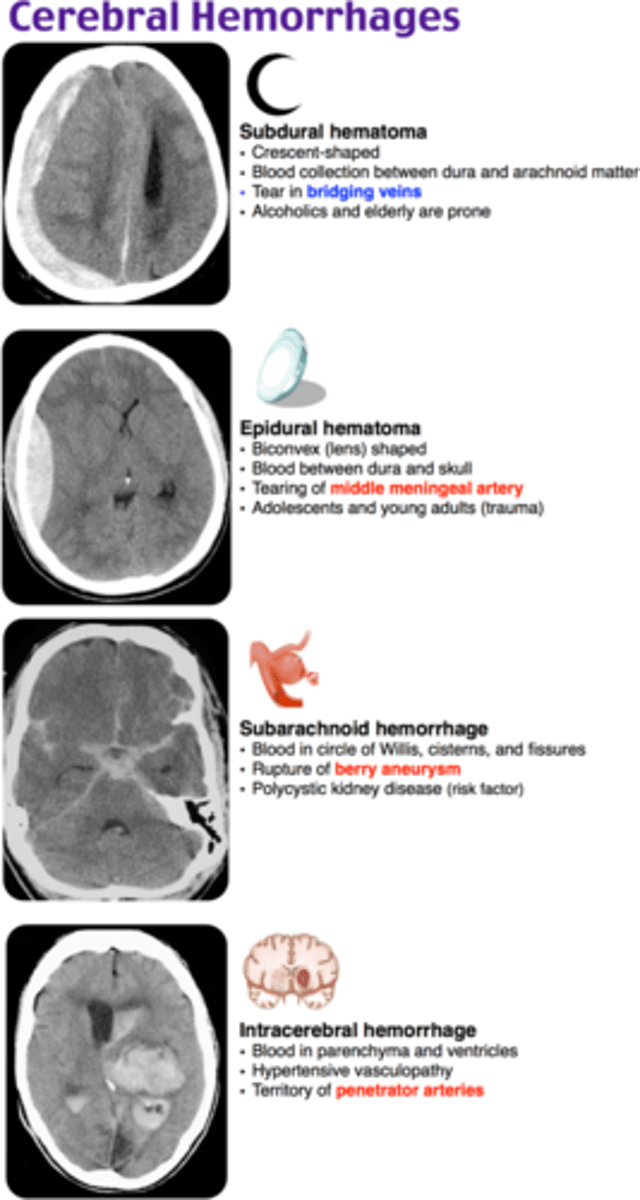
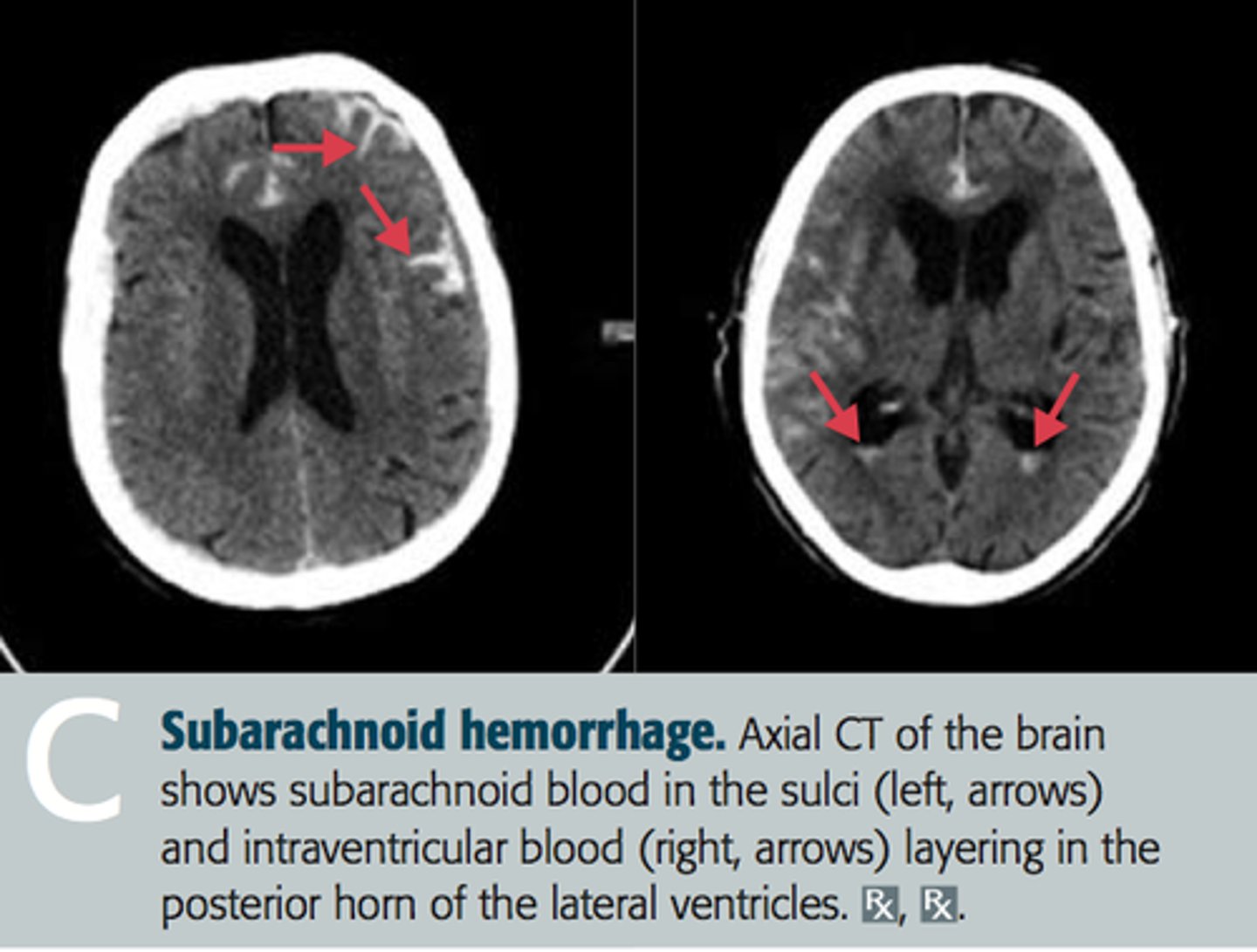
subarachnoid hemorrhage
• Bleeding into the space between the surface of the brain (pia mater) and the arachnoid (one of the 3 coverings of the brain)
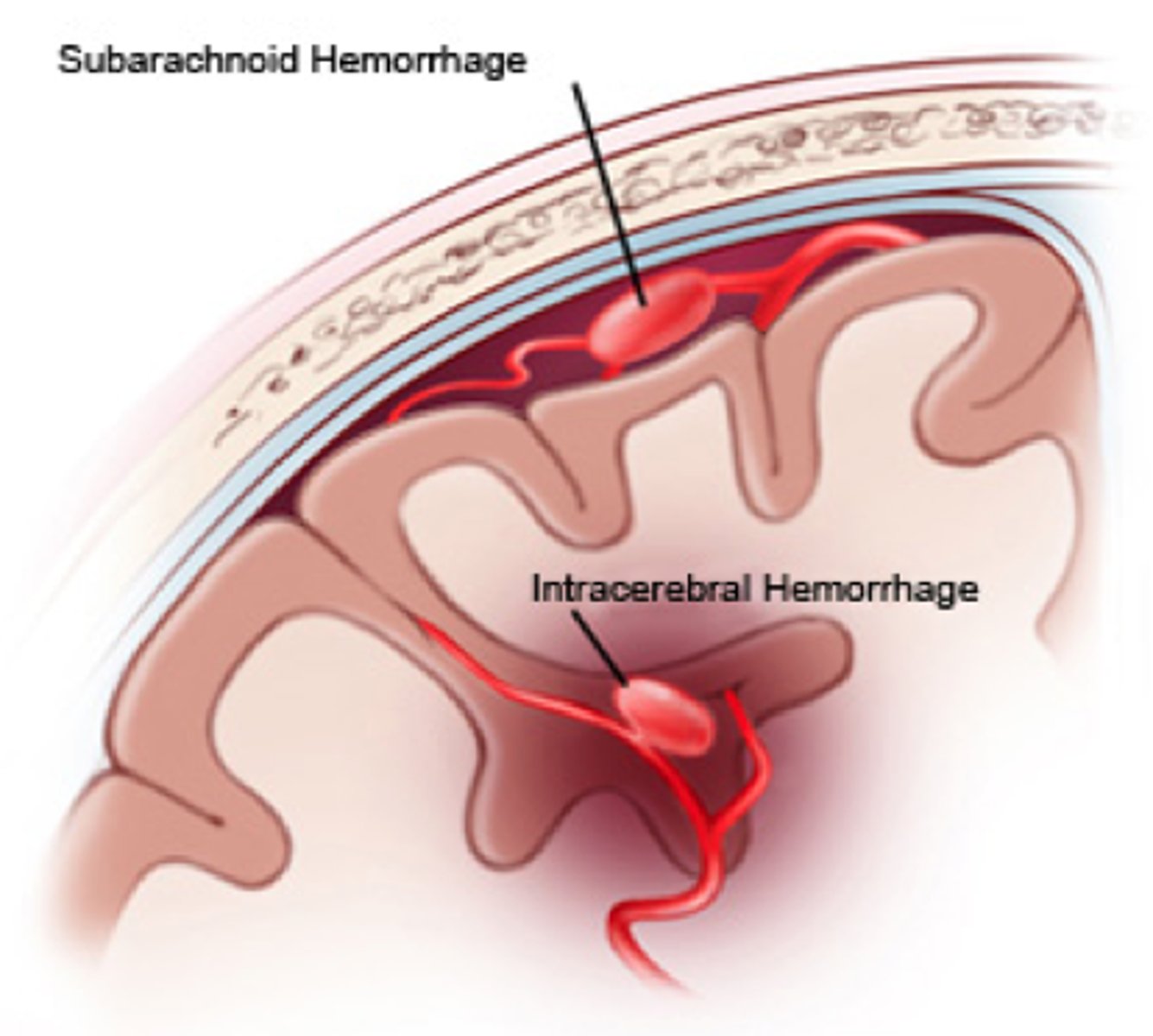
Intracerebral Hemorrhage
• Intraparenchymal- bleeding within the brain tissue itself
• Intraventricular- bleeding into the ventricles
EPIDURAL HEMATOMA
• Close neuro observation:
• lucid initially to unconsciousness
• Potential surgery
• Typically arterial
• Quickly decompensates
SUBDURAL HEMATOMA
• Typically venous
• Close neuro observation:
• gradually increasing headache and confusion
• Potential surgery
• Seizures
• ?Drain
SUBARACHNOID HEMORRHAGE
• Traumatic
• Close neuro observation on admission
• Most common cause of SAH
• Occurs in ~35% of TBI, typically in combination with other hemorrhage
• Rarely causes vasospasm
• FYI: Non-Traumatic
• Close neuro observation for 14 days
• Hunt Hess & Fisher Scale
• Strict BP management
• Angiogram: ?Aneurysmal (75-80%)
• Vasospasm watch with associated delayed cerebral ischemia - TCDs, Angios, Nimodipine, euvolemia, 14 days in ICU
• Hydrocephalus: CSF diversion?
INTRACEREBRAL HEMORRHAGE (ICH)
• IPH & IVH
• Causes:
• Trauma
• HTN
• Amyloid
• Ruptured AVM
• Bleeding disorders
• Cocaine
• Bleeding Tumor

Describe potential complications/secondary injuries of TBIs.
-Cerebral Edema & Herniation
• Monro Kellie Doctrine**
• Mannitol, HTS
• ICP monitoring & EVD (CPP =MAP- ICP; goal >60)
• Hemicraniectomy
-Seizures
• Prophylactic antiepileptic medications as well as aggressive treatment of seizures
-Hydrocephalus
• CSF diversion (EVD/LD drain)
-Alterations of neuroendocrine function of hypothalamus and pituitary system
• Due to cerebral edema
• SIADH: Low Serum Sodium; Low or normal urine output
• DI: High Sodium!!; High urine output (clear)
Why is it important to monitor intracranial pressure (ICP)?
MONRO-KELLIE HYPOTHESIS
• Brain Parenchyma, CSF and Blood are in a fixed box (the skull); an increase in one causes a decrease in one or both of the remaining two
• In an injured brain this autoregulation can be disrupted or the injury is so severe leading to increased intracranial pressure and potentially brain herniation
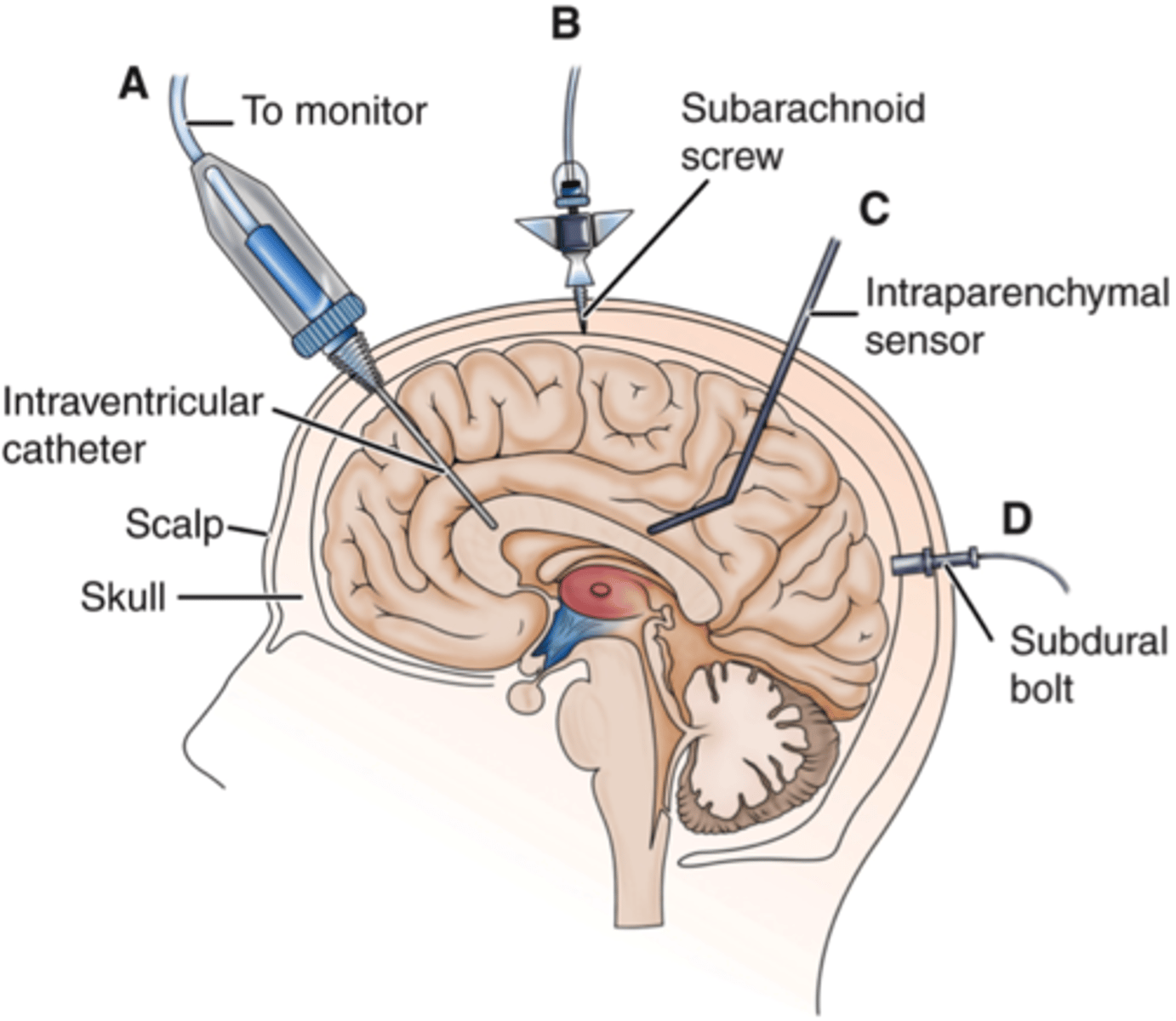
How would you assess ICP?
• ICP Multimodality Monitors: EVD, bolt (ICP, brain O2, perfusion, micro dialysis)
TREATMENT & MANAGEMENT OF INTRACRANIAL HYPERTENSION
• Mostly Supportive Therapy! Close monitoring!!
• Nursing Interventions
• Elevate HOB >30 (ideally as high as you safely can)
• Minimize hip flexion (reverse Trendelenberg)
• Ensure proper neck alignment
• Hyperventilate (should be a rescue measure; not to exceed 15 min)
TREATMENT OF TBI
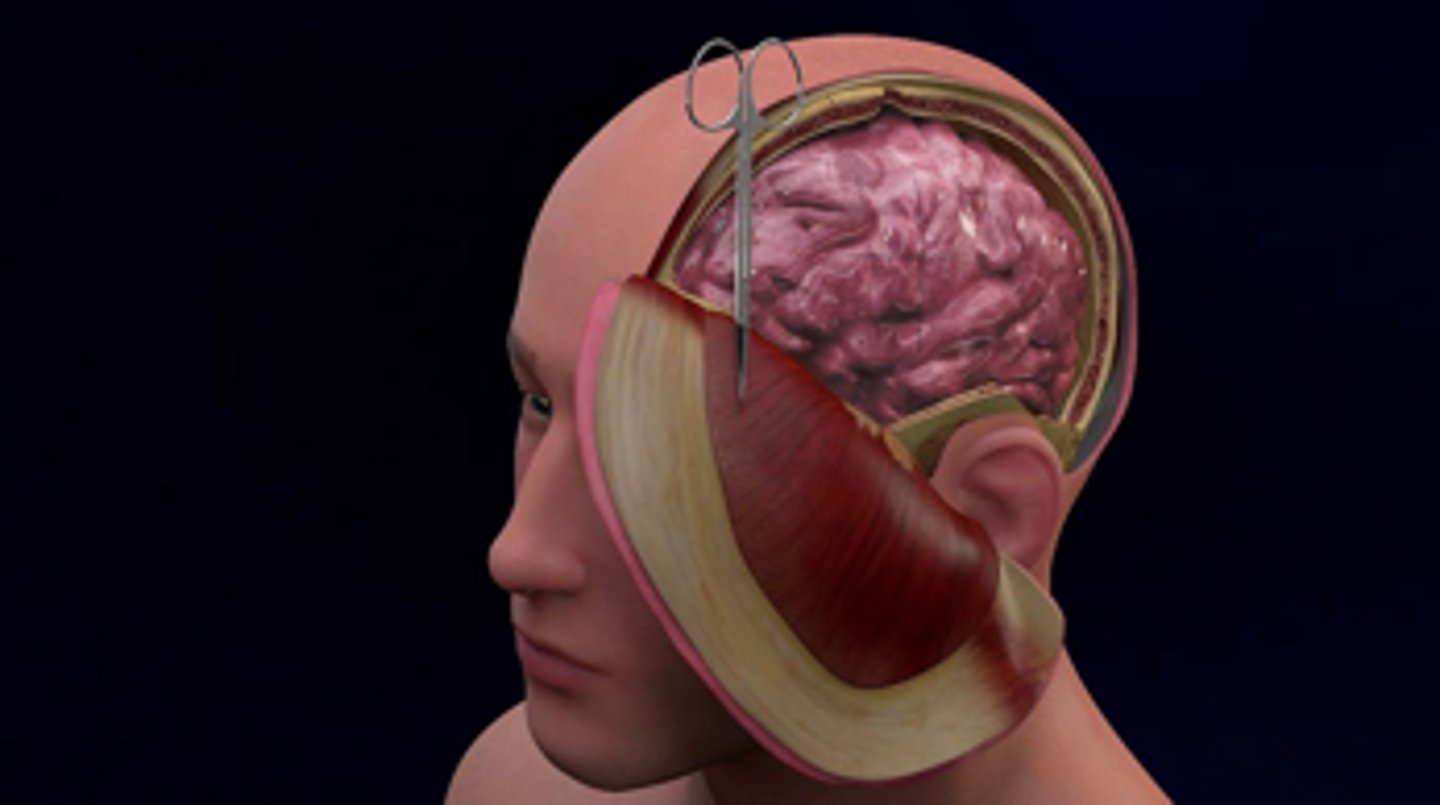
• Some hematomas are surgical (evacuation)
• Monitor and Keep ICP
HEMICRANIECTOMY
a surgical procedure where a large flap of the skull is removed and the dura is opened; this gives space for the swollen brain to bulge and reduces the intracranial pressure.
EVD (EXTERNAL VENTRICULAR DRAINS)
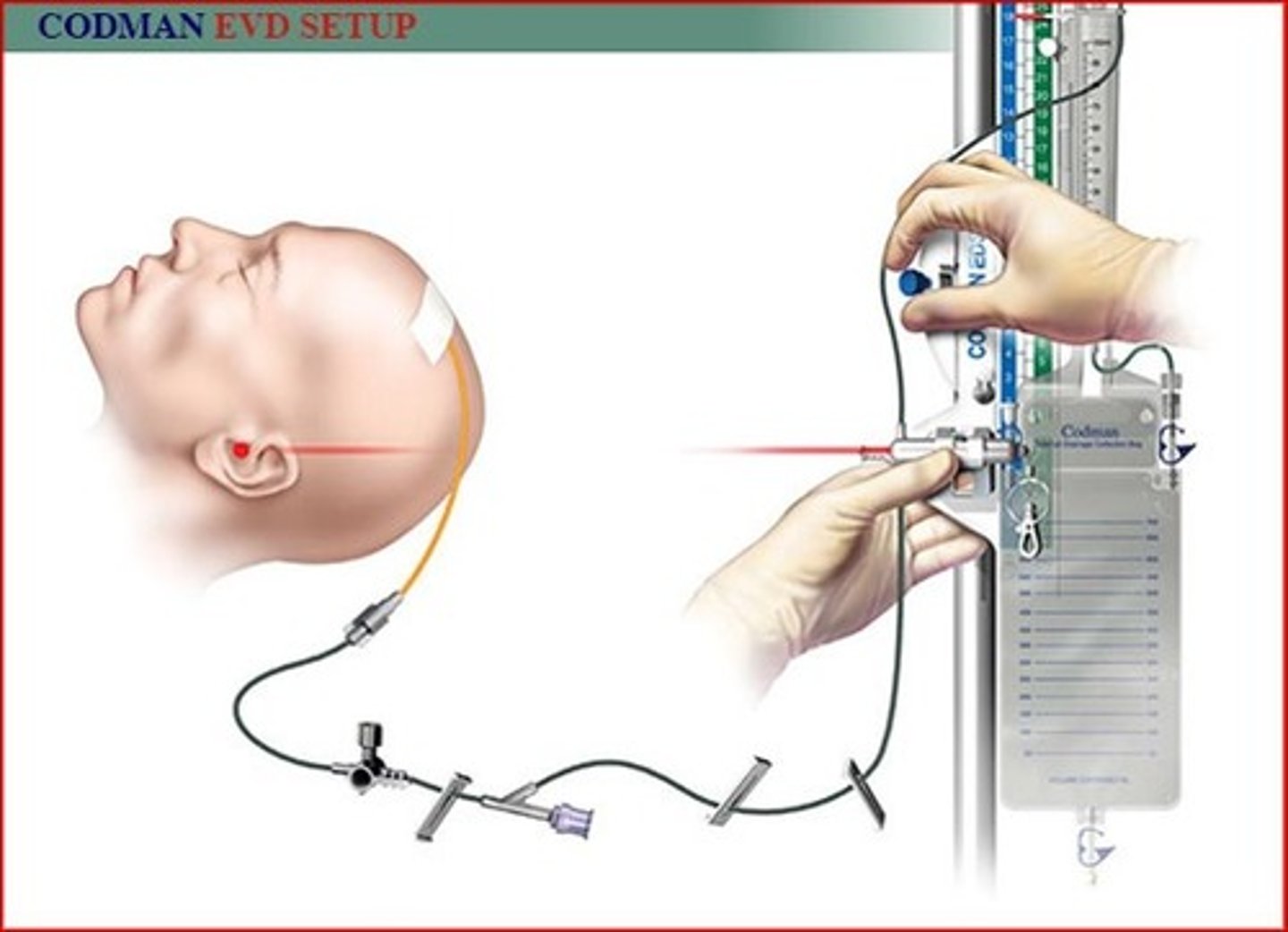
ICP monitors
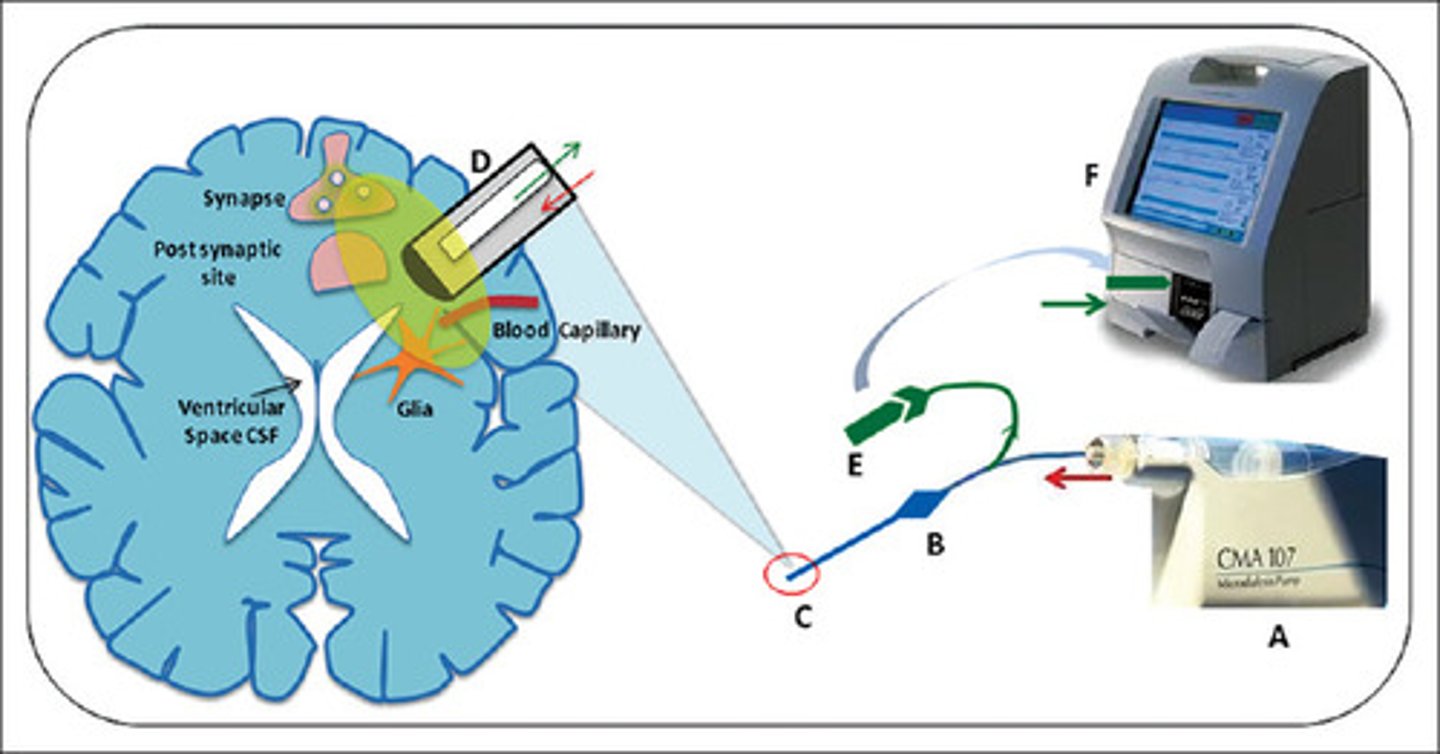
CEREBRAL MICRODIALYSIS
implant a tube, analyze chemicals found outside of cells
NURSING MANAGEMENT "post-op" Neuro
• Neuro:
• Serial Neurologic Exams (Q15min-Q4 hours)
• ICP
• Avoid agitation
• EVD management/Intracranial monitoring
• Repeat Imaging - urgency?
• Seizures (clinical vs sub-clinical)
• HOB
NURSING MANAGEMENT "post-op" CV
• CV:
• BP goals (Avoid hypertension in bleeds; Avoid hypotension to optimize CPP)
• Monitor HR
• Perfusion
• Shock (Fluid/Vasopressors)
NURSING MANAGEMENT "post-op" Resp/GI/GU/ID
-Respiratory
• Monitor status, GCS
NURSING MANAGEMENT "post-op" skin/heme/act
-Skin/MSK:
• Wound care
• Frequent turns/Repositioning-Heme:
• DVT prophylaxis
-Activity:
• OOB & PT/OT
• Patient/Family education & support!
Describe the anatomy of the spinal cord.
-Cervical:
• Small vertebral bodies
• Extensive joint surfaces (greater ROM)
-Thoracic
• Rib bearing vertebrae
• Designed to remain stiff and straight
-Lumbar
• Weight bearing vertebrae
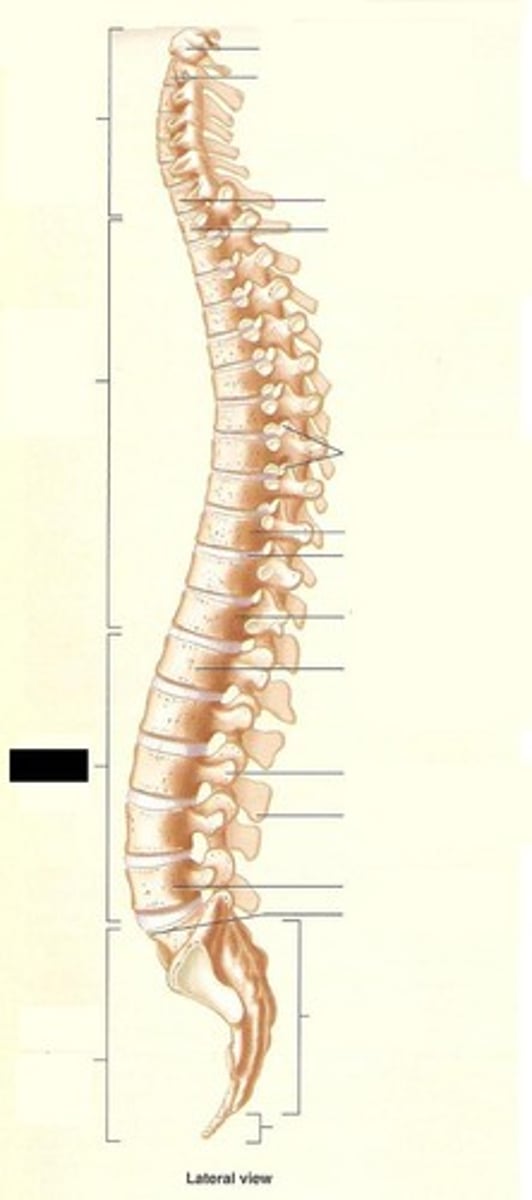
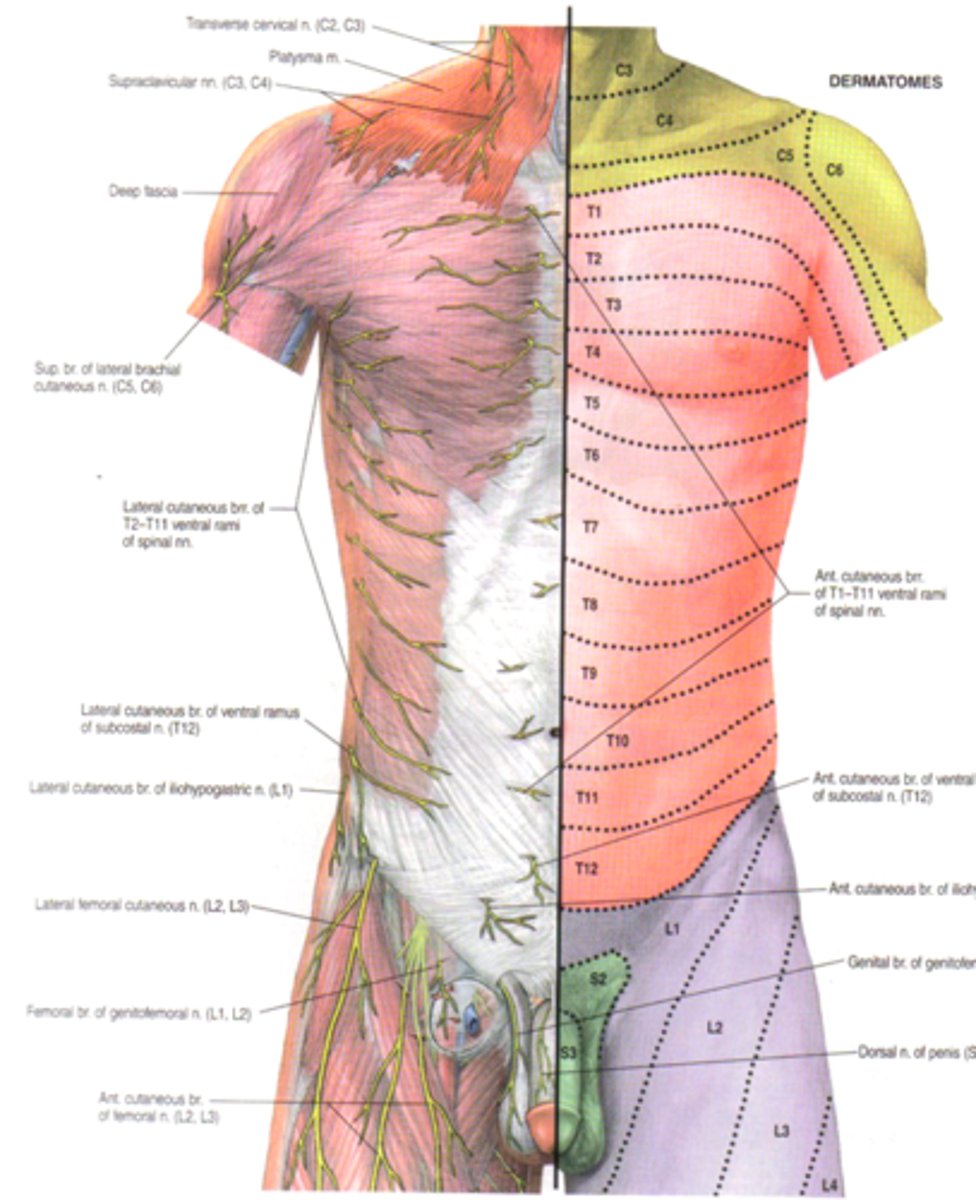
Review the dermatomes innervated by each spinal cord segment.
Describe different mechanisms of spinal cord injury.
• Compression
• Flexion
• Extension
• Rotation
• Lateral bending/stress
• Distraction
• Penetration
Describe different types of spine injury.
• Complete= No residual function more than three levels below the injury affecting both sides equally
• 3% of patients will regain some function within 24 hours, after which the expectation is distal function is lost
• Incomplete= Any residual sensory or motor function below the injured level
How does the American Spinal Injury Association Scale classify spinal cord injury?
• A= Complete: No motor or sensory function is preserved in the sacral segments S4-S5
• B= Incomplete: Sensory but not motor function is preserved below the neurological level and includes sacral segments S4-5
• C= Incomplete: Motor function is preserved below the neurological level, and more than half of key muscles below the neurological level have a muscle grade less than 3
• D= Incomplete: Motor function is preserved below the neurological level, and at least half of key muscles below the neurological level have a muscle grade of 3 or more • E= Normal: motor and sensory function are normal
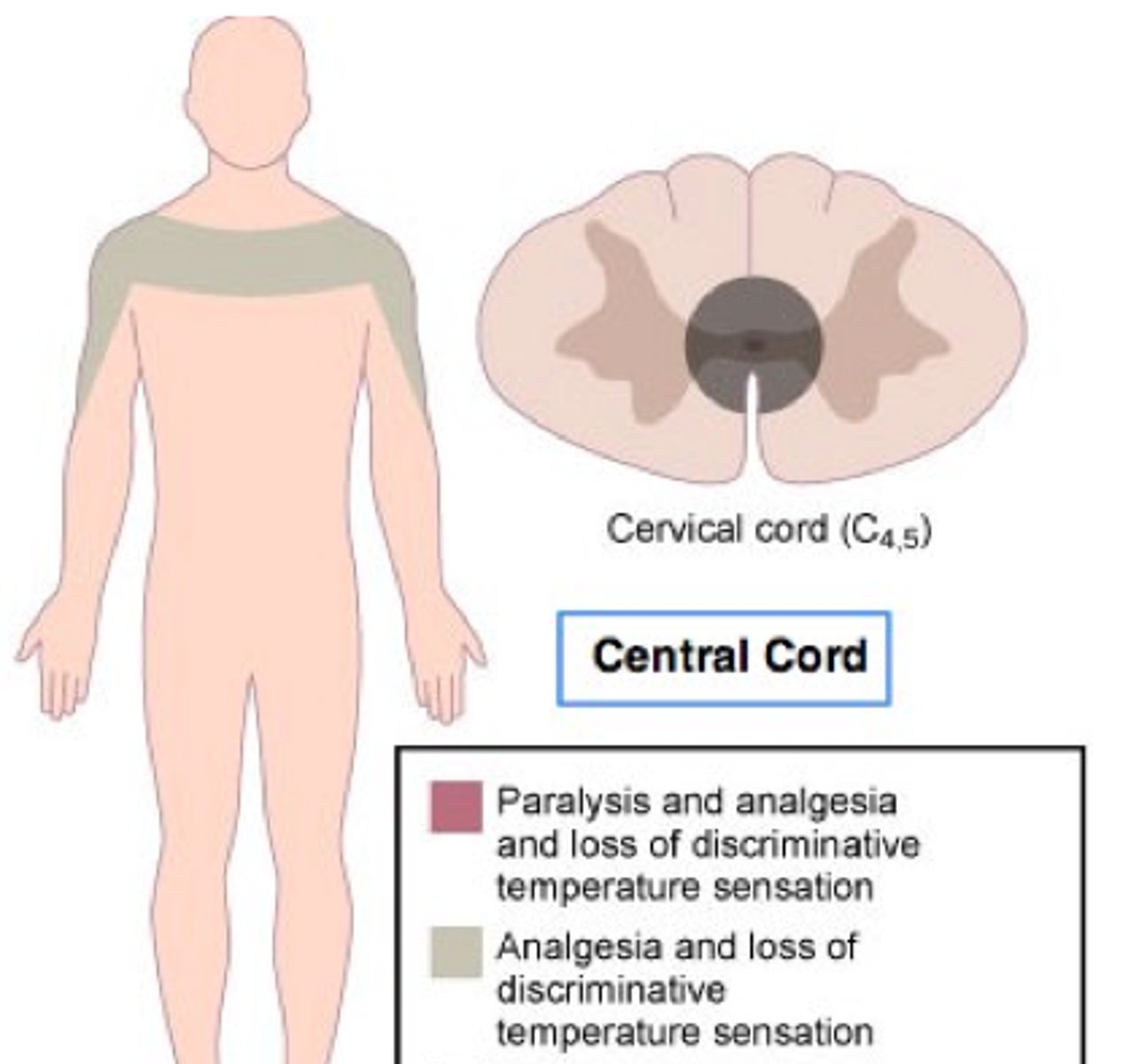
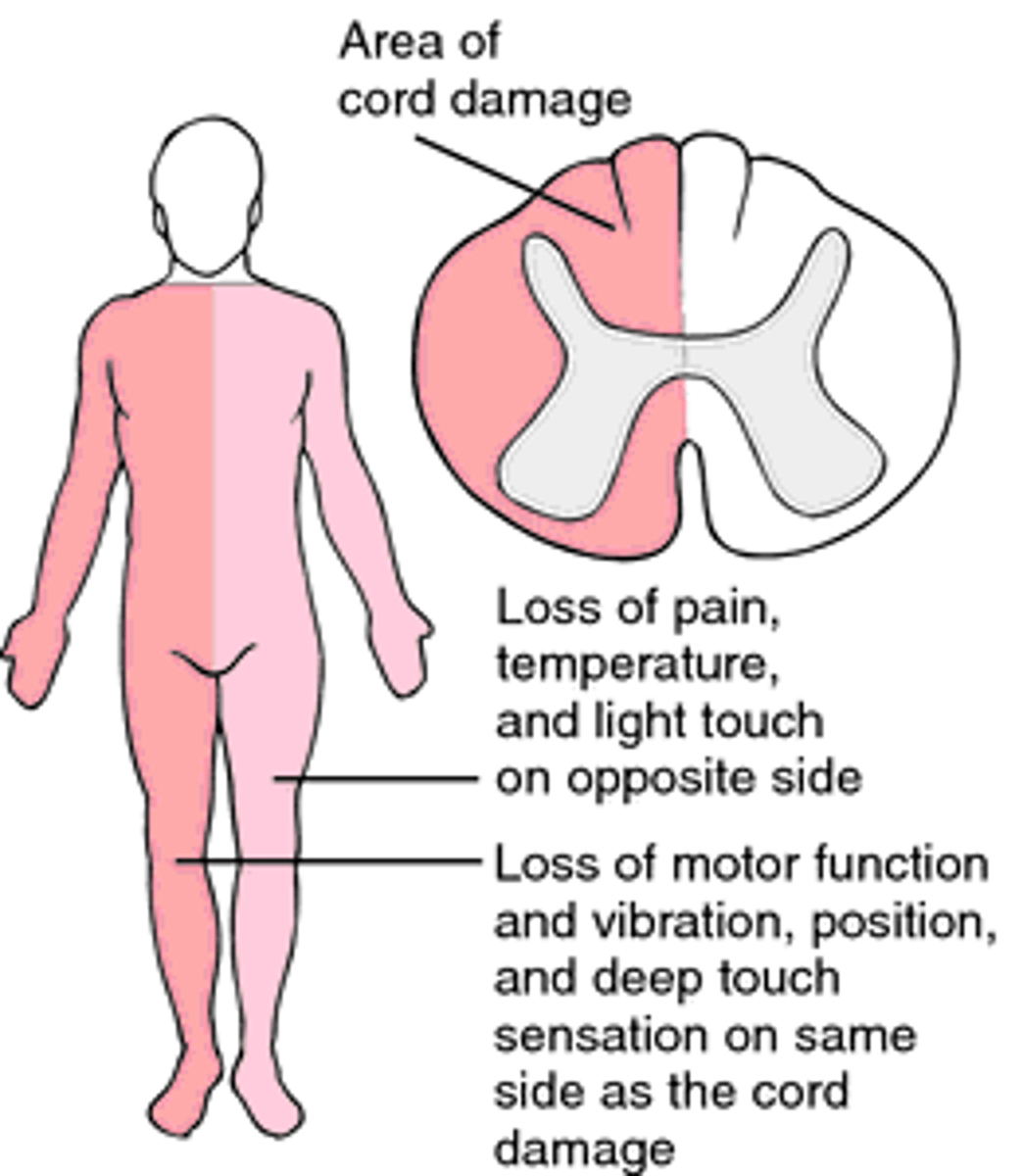
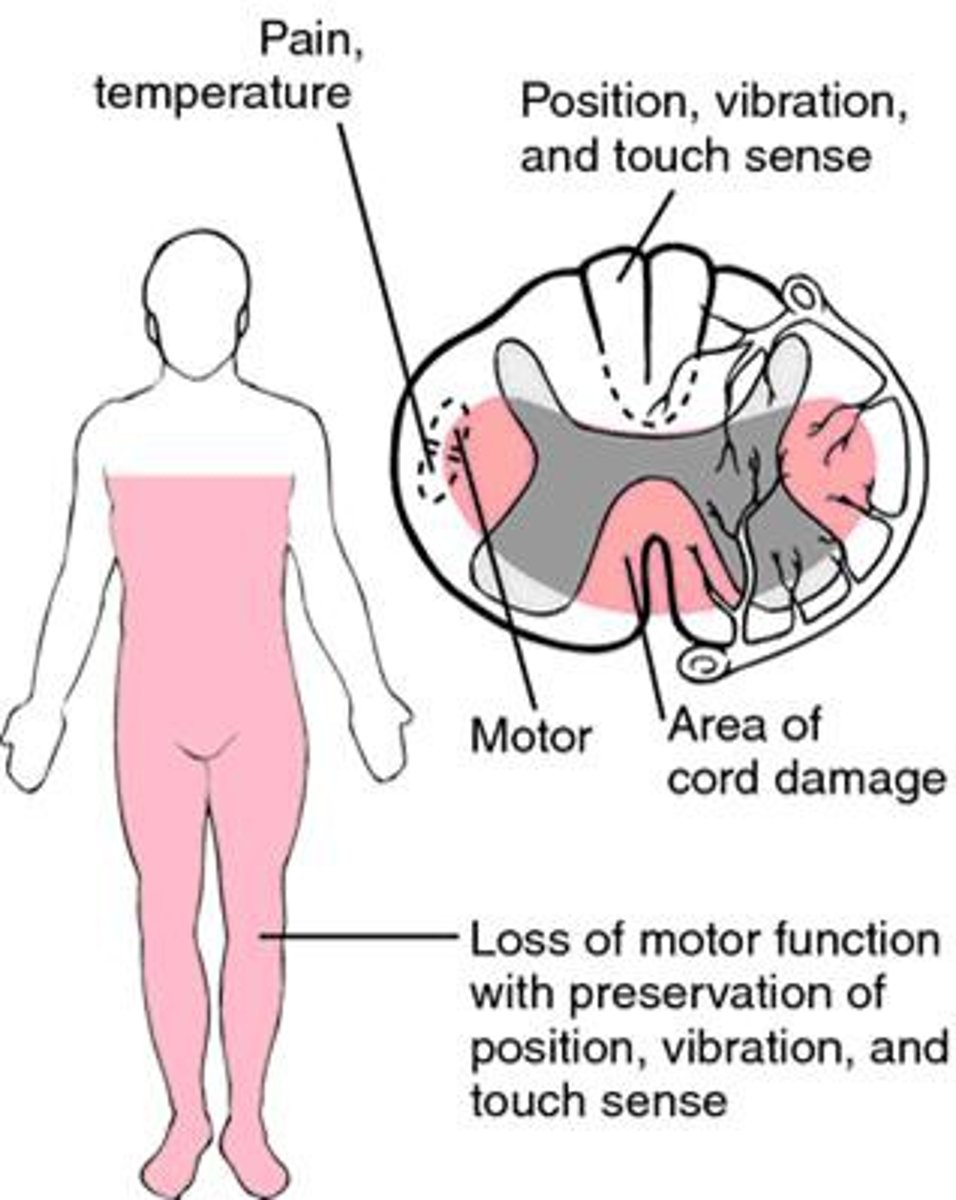
Differentiate the types of spine syndromes.
- Central Cord Syndrome
• Brown-Sequard Syndrome
• Anterior Cord Syndrome
• Cauda Equina Syndrome
CENTRAL CORD SYNDROME
• Most common type of incomplete injury
• Injury to the cervical cord
• Results in weakness in arms (loss of fine motor) more than legs, cervical motor fibers are located towards the center of the cord
• Surgical treatment remains controversial
• Commonly found in hyperextension injury: older persons with cervical spondylosis & younger persons with traumatic injury
• Recovery is possible but variable
BROWN-SEQUARD SYNDROME
• Rare
• Weakness or paralysis on one side of the body and loss of sensation on the opposite side (ipsilateral loss of motor, contralateral loss of sensation)
• Damage to half of the spinal cord
- can be seen in patients with spinal cord tumor, trauma, infection and inflammatory disease, as well as disc herniation
ANTERIOR CORD SYNDROME
• Complete motor paralysis and loss of temperature and pain perception distal to the lesion, with preserved light touch, vibration and proprioception
• Caused by compression of the anterior spinal artery
• Associated with burst fractures
CERVICAL BURST FRACTURE

CAUDA EQUINA
• Cauda Equina= Latin for "Horse's Tail"
• Nerve roots of the cauda equina are compressed (herniated disc, tumor, abscess)
• Symptoms: weakness, difficulty urinating, loss of rectal tone, saddle anesthesia*
• Medical emergency
What are acute complications of spine injury?
-Shock:
• Spinal Shock- Transient depression or loss of reflex activity below the level of an acute spinal cord injury
• Neurogenic Shock- Form of distributive shock-hemodynamic changes resulting from sudden loss of autonomic tone due to spinal cord injury (hypotension, bradycardia); Generally in patients with injury T6 and above
• Management: Airway support if needed, Fluids as needed, Atropine for Bradycardia (pace maker??), Vasopressors as needed
*Different but both shocks may coexist in a patient!*
SPINAL INJURY: ACUTE COMPLICATIONS (Autonomic Dysreflexia)
• Uncontrolled sympathetic response secondary to a stressor in patients with a spinal cord injury T6 and above (unlikely to occur is below T10)
• Life threatening HTN and Bradycardia when there is a noxious stimulus below the level of injury, most often a urological source (UTI, distended bladder)
• Initial complaint is headache- any patient with headache and spinal cord injury above T6 should have their BP checked immediately
AUTONOMIC DYSREFLEXIA MANAGEMENT
• Non-pharmacological Management:
• Remove the cause of injury/stimulation • Position patient upright
• Loosen tight clothing
• Pharmacological Management for sustained elevated BP
• Antihypertensive drugs (nifedipine and prostaglandin E2)
What are the treatments for each?
• Stabilization of spine (surgery, brace, traction)
• Distributive Shock Management: Fluid resuscitation, Atropine for Bradycardia, Vasopressors as needed
• BP management: spine perfusion
• Respiratory: secure airway
• Steroids?: current evidence=no
• Intensive supportive care
Spinal chord injury ASSESSMENT
• ABC...DE
• Neuro Exam
• Motor strength assessment & Sensory Exam
• Respiratory: "C3-4-5 keeps the diaphragm alive!"
• Secretions, cough?
• GI/GU- Bowel/bladder function
• Skin- assessment
• PMH & Medications
What is the nursing management for spinal cord injury?
• Neuro:
• Serial neurologic exams (early in acute injury) especially motor strength, and sensation
• Maintain proper spinal precautions/alignment
• Pain management (neuropathic pain)• Patient/family education & support
• Encourage patient to be active participant in their care/recovery (give them back some control)
SPINAL PRECAUTIONS
• C-Spine: Immobilize the c-spine. 2 to 3 nurse turn
• T-Spine: No reaching, crossing arms, bending, TLSO brace?
• Full Spine: Log roll, HOB Flat (reverse T)
NURSING MANAGEMENT
Resp/cv
• Respiratory:
• Close monitoring
• Pulmonary toileting (cough assist, chest PT, quad cough)
• Management of secretions
• CV:
• BP monitoring
• HR/telemetry
• Optimize perfusion
NURSING MANAGEMENT
GI/GU/skin/heme/discharge
GI/GU
• Bowel regimen (may need standing suppository/rectal stimulation)
• Strict bladder training
• Skin:
• Frequent turns & skin assessments - offload pressure
• Mobilize!!
• Heme:
• DVT prophylaxis
• Discharge Planning:
• Early PT/OT/Speech
• SCI rehabiitation/PM&R