L4: Anaemia1- reduced red cell production
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
what are the two causes of reduced marrow production
primary:
bone marrow failure or dusfunction
secondary
insufficient nutrients iron, folate, vitamin B12, EPO
how much iron is stored in the body?
4 gm
where is iron located in the body?
RBCs, 70% of body Fe in Hb
one g Hb contains 3.5 mg iron→ 2.5 g iron in RBC
ferritin 30% body Fe
myoglobin Fe in muscle 4%
enzymes- cytochrome system in mitochondria
what are the sources of body iron?
daily intake: 10-20mg/day
10% intake is absorbed (1mg/day)
iron absorption requires acidic environment
what substances can increase or inhibit iron absorption
iron absorption requires acidic environment
vitamin C increase iron absorption
coffee and tea are alkaline and inhibit iron absorption
iron in human milk is more easily absorbed than cows milk
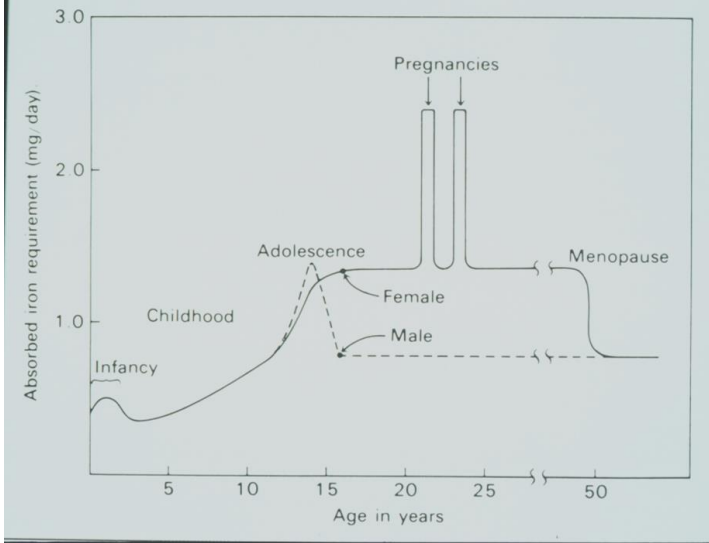
how much iron is required daily?
males and non mesturating females: 1mg/day to compensate for normal iron loss: skin shed, faeces
menstruating females 2mg/day→ iron intake increased to compensate for blood lost
how is body iron distributed?
normal iron content is around 4000 mg
RBCs: 2500mg
myoglobin 300mg
enzymes 200mg
storage iron 1000mg → liver, spleen reticulo-endothelial system + bone marrow
how is iron lost
skin, gut, sweat 1mg/day
menses, 1mg/day
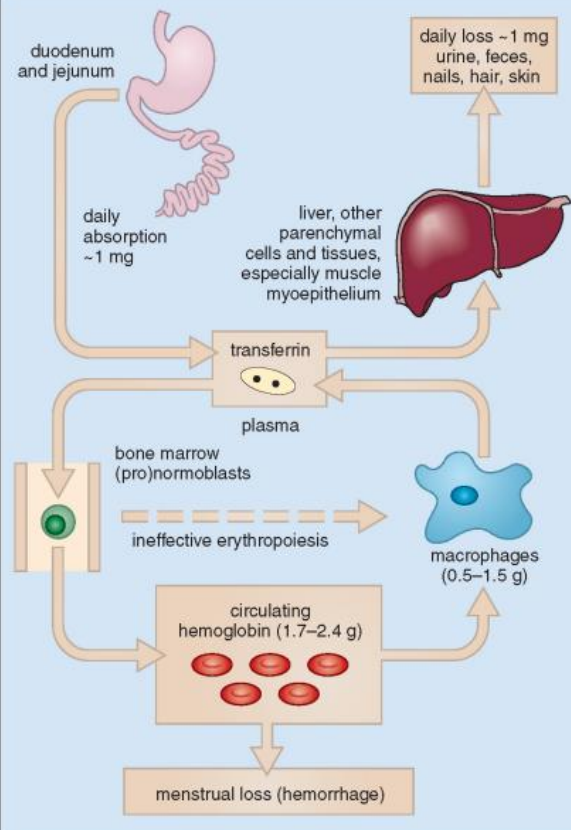
describe the iron cycle
Absorbed iron transported to marrow bound to transferrin
Iron utilised in erythropoiesis
Released iron taken up by macrophages
Excess iron is stored in macrophages and liver as ferritin
prevelence of iron deficiency anaemia
WHO estimates >30% of world population is anaemic
\males: 10%
non pregnant females: 30%
pregnant women: 40%
mainly due to iron deficiency
causes of iron deficiency
reduced intake
poor iron absorption/malabsorption
chronic blood loss
increasedd iron utilisation
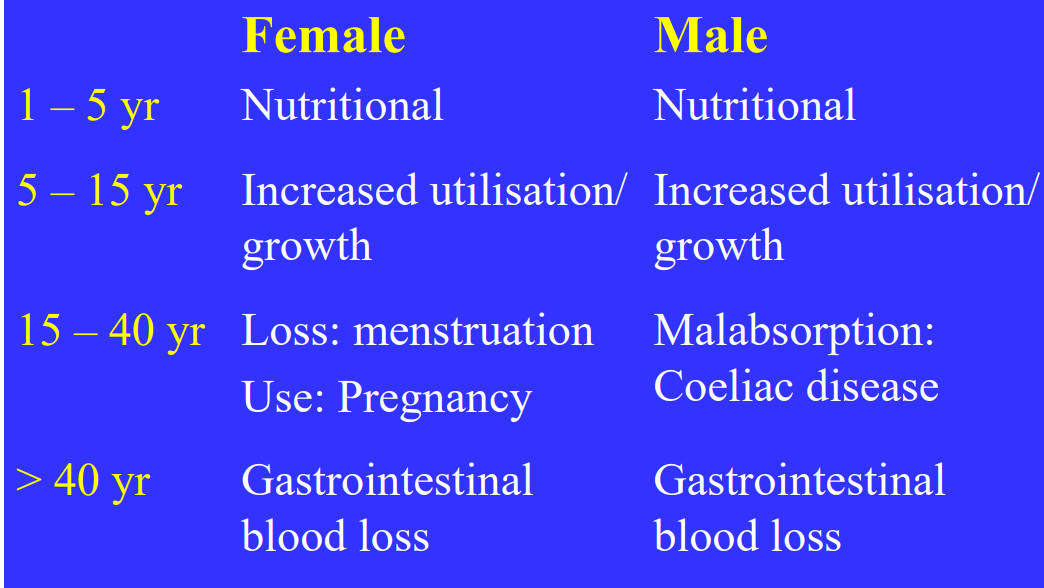
reduced intake of iron
rare in developed world
commonest form of anaemia in paediatrics beacuase theyre not getting weaned and not getting enough from breastmilk
what causes malabsorption of iron
stomach or bowel; gastrectomy removal of some of the bowel
coeliac disease→ possible causeif its a young man
chronic blood loss
loss of iron
GI: ulcers, carcinoma,varices(expanded oesophagus) haemorrhoids
uterine bleeding menorrhagia
increased iron utilisation
neonates puberty, pregnancy(which uses 3mg per day)
tissue and organ growth
what are the stages of iron deficiency
negative iron balance- reduced iron stores, normal RBC iron, no anaemia
iron deficient erythropoiesis - reduced iron stores, mildly reduced RBC iron, no anaemia
iron deficiency anameia- reduced iron stores, reduced RBC iron and anaemia
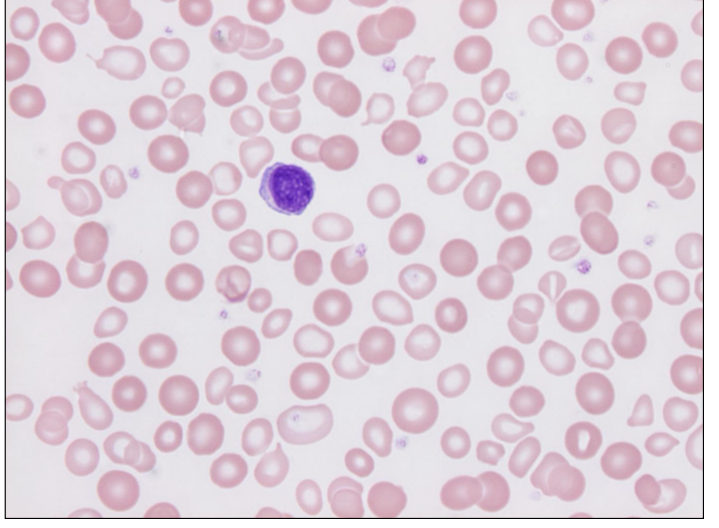
what is the haematology of iron deficiency anaemia
anaemia, low Hb, reduced MCV (<80fl)
blood film: hypochromic(pale) microcytic (small) RBCs, some pencil shaped cells and elliptocytes
what are the lab features of iron deficiency anaemia
mild thrombocytosis: increased pllatelet count
reduced reticulocyte count (insufficient new RBCs being made in BM)
bone marrow:
reduced erythropoiesis
reduced iron stores: when looking at a blood marrow the iron is stained blue
what are the lab measures of iron stores
Serum iron:
Highly variable. Not useful to assess iron stores
measures how much is being absorbed
Serum transferrin (Tf):
Measure of iron transporter: increased
Transferrin saturation:
% of iron transporter occupied by iron: reduced
Serum Ferritin:
Reflects body iron stores: reduced
summary: low ferritin, low iron, high transferrin
how to find the cause for iron deficiency?
intake: dietary history
absorption: test for coeliac disease
blood loss(gastrointestinal and uterine)
endoscopy,colonoscpy
pelvic examination
increased utilisation
management of iron deficiency
Determine and treat the underlying cause
• Iron replacement therapy:
Oral (tablets or syrup)
Intravenous
Intramuscular (rare)
Duration: to normalise Hb and ferritin (stores)
Response: increase in Hb; reticulocytosis
• Blood transfusion: rarely required
describe a dimorphic blood film
Partially treated iron deficiency
Both small pale and cells (residual iron deficient cells) and normal RBC
vitamin b12 and folate
Required for DNA production
• Required for nuclear maturation
• Deficiencies cause reduced red cell production
• Abnormal “ineffective: erythropoiesis, called “megaloblastic”
• Deficiencies result in anaemia (macrocytic)
Vitamin B12
Complex molecule (Cyanocobalamin)
\• Dietary source (animal products) • Meat, fish, eggs, milk, butter
• Absent from vegetables, cereals, fruit
• Daily requirements = 0.5 - 1 µg / day
• Western diet contains 10‐15 µg/day (50% absorbed)
• Body stores 2 ‐ 5 mg (mainly liver)
• Sufficient for 10 years without further supply
• Deficient intake may take years to manifest
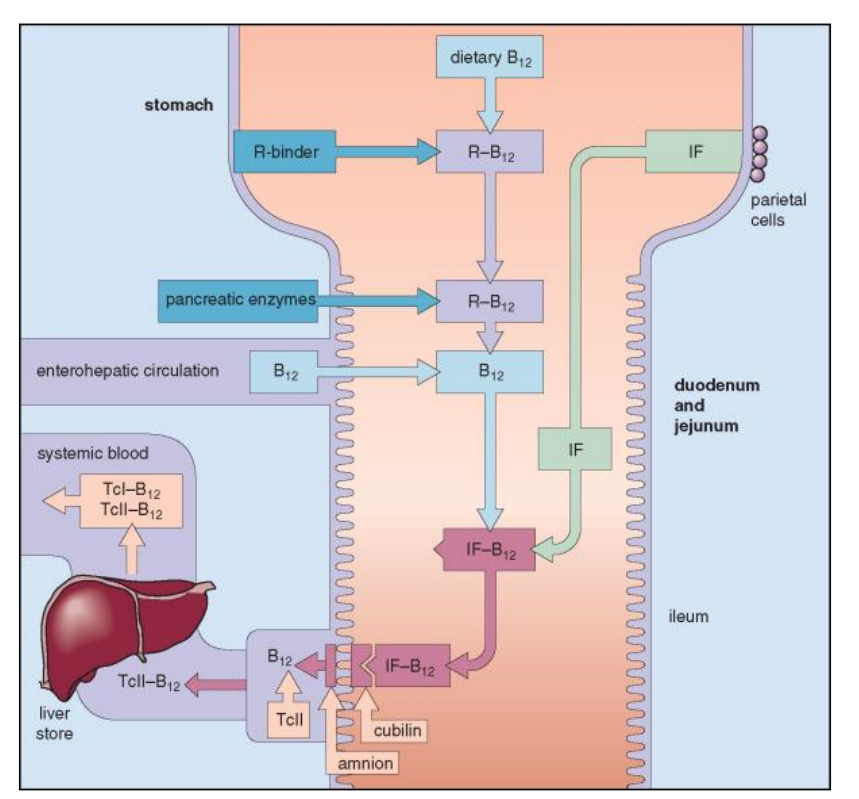
How is Vitamin B12 Absorbed?
• From mouth – stomach – small bowel (ileum)
• Dietary Vit B12 combines with intrinsic factor (IF)
• IF is secreted by parietal cells in the stomach
• IF – Vitamin B12 complex travels through small bowel
• Attaches to receptors in terminal ileum
• Vitamin B12 is absorbed •
Absorbed Vit B12 attaches to Transcobalamin II
• Carries Vit B12 in plasma to the liver, BM, tissues
• Most B12 in plasma is attached to another B12 binding protein (Transcobalamin I) and is functionally inactive
Causes of Vitamin B12 Deficiency
Diet: inadequate intake
• Vegans: no animal products in diet
• Infants born to B12-deficient mothers and breastfed • Malnutrition, famine, poverty •
Malabsorption:
• Gastric causes: Pernicious anaemia (IF); gastrectomy
• Intestinal causes: defects of the ileum (resected; Crohn’s disease); Bacterial overgrowth
Long-term nitrous oxide exposure
clinical features of vitamin B12 deficiency
Asymptomatic; incidental finding
• Gradual onset anaemia
• Mild jaundice (ineffective erythropoiesis due to lack of B12)
• Neuropathy:
• Tingling of the feet; difficult walking
• Subacute combined degeneration of the spinal cord • Neurodegenerative condition
• Demyelination of the dorsal (posterior) and lateral spinal columns
what is Pernicious Anaemia?
• Commonest cause of Vitamin B12 deficiency
• Auto-immune disease (family history; blood group A)
• Auto-antibodies to parietal cells or intrinsic factor interfere with formation IF-B12 complex and B12 absorption
• Females > Males; greying hair
• Anaemia with “lemon yellow” tint
• Macrocytic anaemia (MCV >100 >110 fL) •
Low vitamin B12
• Rx: Intra-muscular vitamin B12
Nitrous Oxide and Vitamin B12
Anaesthetic (>150 yrs) and laughing gas
• NO binds irreversibly to and inactivates Vit B12
• Repetitive or heavy “use” over extended time causes anaemia and neurotoxicity 2o to Vit B12 deficiency
• Demyelination of dorsal columns leads to subacute combined degeneration of the spinal cord
• “Recreational” use increasing; admissions to ED
• Rx: stop nitrous oxide; Vit B12 (hydroxocobalamin)
Alcohol and Vitamin B12
• Consumption of alcohol reduces B12 absorption by 5%
• In alcoholic liver disease there is deficiency of vitamin B1, vitamin B2 and vitamin B6.
• The causes include:
Inadequate dietary intake
Increased use of vitamin B
Decreased storage in the liver
Reduced intestinal absorption by ethanol
Abnormal metabolism of the vitamins
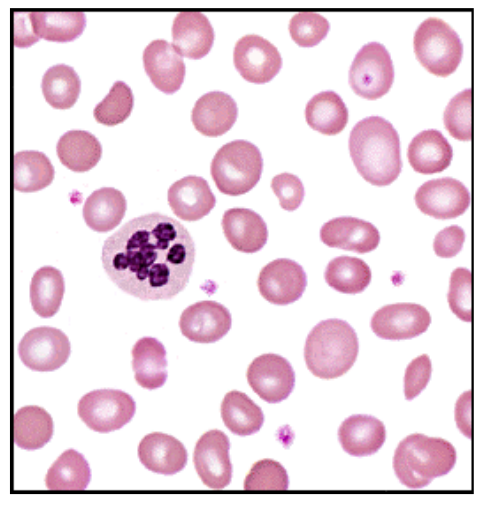
vitamin B12 deficiency blood film features
• Macrocytic anaemia (high MCV); oval macrocytes
• Hypersegmented neutrophils
• Mild reduction in leucocytes and platelets
B12 deficiency biochemistry features
Low serum vitamin B12 • HoloTransCobalamin assay: measures active B12 • Normal serum folate; raised bilirubin and LDH
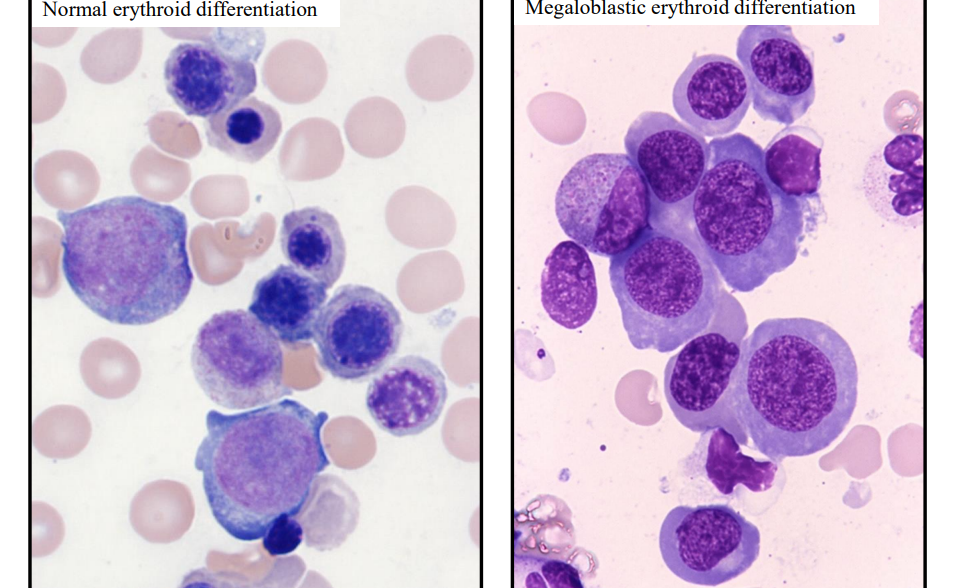
b12 deficiency bone marrow
• Megaloblastic (ineffective) erythropoiesis
treatment for B12 deficiency
• 1,000 µg hydroxocobalamin IM
• 3x per week for 2 weeks (6 doses) •
Then, 1,000 µg hydroxocobalamin every 3 months for life (unless the deficiency is corrected)
• Large doses of oral vitamin B12 can be given:
• 1 – 2 mg daily
• Less reliable than IM (esp. for pernicious anaemia)
what is folic acid
• Folate: water‐soluble naturally occurring B group vitamin (B9)
• Folates present in most foods, especially'
: • Green leafy vegetables; fruits; liver
• Folic acid is added to bread, flour, cereals, pasta
Normal diet contains 250 - 500 µg (50% absorbed)
• Daily adult requirements approx. 100 µg
• Body stores 5 - 10 mg; sufficient for 3 - 4 months
• Absorbed in upper gastrointestinal tract
Causes of Folate Deficiency
• Diet: reduced folate intake
• Poor absorption
• Increased folate requirements: cell turnover
• Physiological: pregnancy; lactation; prematurity
• Pathological: haemolytic anaemia; inflammatory conditions; exfoliative dermatitis
• Excess folate loss: dialysis (protein bound)
• Drugs: anti-convulsants
• Other: alcoholism
Treatment of Folate Deficiency
• Folic acid: 5mg per day for a few months
• Correct the anaemia
• Decide whether ongoing folic acid is required: depends on the underlying cause
• Dietary advice
Megaloblastic Anaemia
Due to Vitamin B12 or folate deficiency
• Impaired DNA synthesis of all cells
• Large RBC precursors (“megaloblasts”) in BM
• Macrocytic anaemia (oval): MCV > 100 > 115 fL
• Hypersegmented neutrophils
• Hypercellular bone marrow (failed “ineffective” erythropoiesis)
• Reduced serum Vitamin B12 or RBC folate
• Causes as described above
Folate and Neural Tube Defects
• Fetal growth characterised by widespread cell division
• Adequate folate is critical for DNA and RNA
• Neural tube defects arise from failure of embryonic neural tube closure 21 - 27 days post-conception when most women unaware of pregnancy
• Folate deficiency at conception can cause birth defects of brain, spine, spinal cord
• Anencephaly (stillborn); Encephalocoele; Spina bifida
• No cure; birth defects are permanent
• Prevention: folic acid