HRM - Lecture 11: Diuretics and Chronic Renal Diseases
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
A substance which decreases reabsorption of sodium and water, along with bicarbonate and/or chloride
Briefly define "diuretic"
Increased loss of sodium chloride with passive water loss
What is the main aim of diuretics?
- Oedema
- Hypertension
- Hypercalcaemia
- SIADH
Give 4 indications for diuretics
Loop diuretics act in the TAL on the NaK2Cl transporter, where they bind to the Cl- site.
How do loop diuretics work?
More sodium is delivered to the late DCT and CD. Here sodium is absorbed by principal cells at the expense of K+ secretion. INcreased K+ secretion causes increased K+/H+ exchange at A intercalated cells, which lowers [H+]. Side effects: Hypokalaemia and alkalosis. Also hypocalcaemia due to decreased NaK2Cl and ROMK mediated paracellular calcium reabsorption
What are the potential side effects on solute concentration of loop diuretics? Why do these occur?
up to 25%
How much Na+ can be excreted through loop diuretics?
Inhibition of Na+/Cl- symporter in (early) DCT by binding to Cl- site
How do thiazide diuretics function?
Thiazide diuretics cause more K+ and Na+ to be in the lumen. More Na+ and K+ in the lumen at the DCT results in increased H+ secretion and alkalosis. Also hypercalcaemia/increased calcium reabsorption. Decreased intracellular Na+ increases basolateral Na+/Ca2+ exchange and increased transcellular reabsorption of Ca2+
What are the side effects of thiazide diuretics in terms of solute concentration? How do these occur?
Method 1: K+ sparing diuretics are aldosterone antagonists. These decrease Na+ reabsorption in the collecting duct and also decrease K+ secretion
Method 2: ENaC blocker. Decreased intracellular Na+ decreases basolateral Na/K ATPase activity. This decreases movement of K+ into the cell from the interstitium and thereby spares K+
How do K+ sparing diuretics function?
K+ sparing diuretics
Which diuretics are the only type not to act at the luminal/apical side?
thiazide diuretics
Which is the most common diuretic for hypertension
Osmotic diuretics are freely filtered and simply work through increasing osmosis into the tubule. These act at all sites of the nephron which are permeable to water: PCT, descending loop of Henle, and CD (in presence of ADH). Biggest impact at PCT.
How do osmotic diuretics work?
CA inhibitors stop the creating of H2CO3 from H+ and HCO3- in the PCT. This means HCO3- isn't reabsorbed and excreted in urine along with H2O, Na+ and K+
How do carbonic anhydrase inhibitor diuretics work?
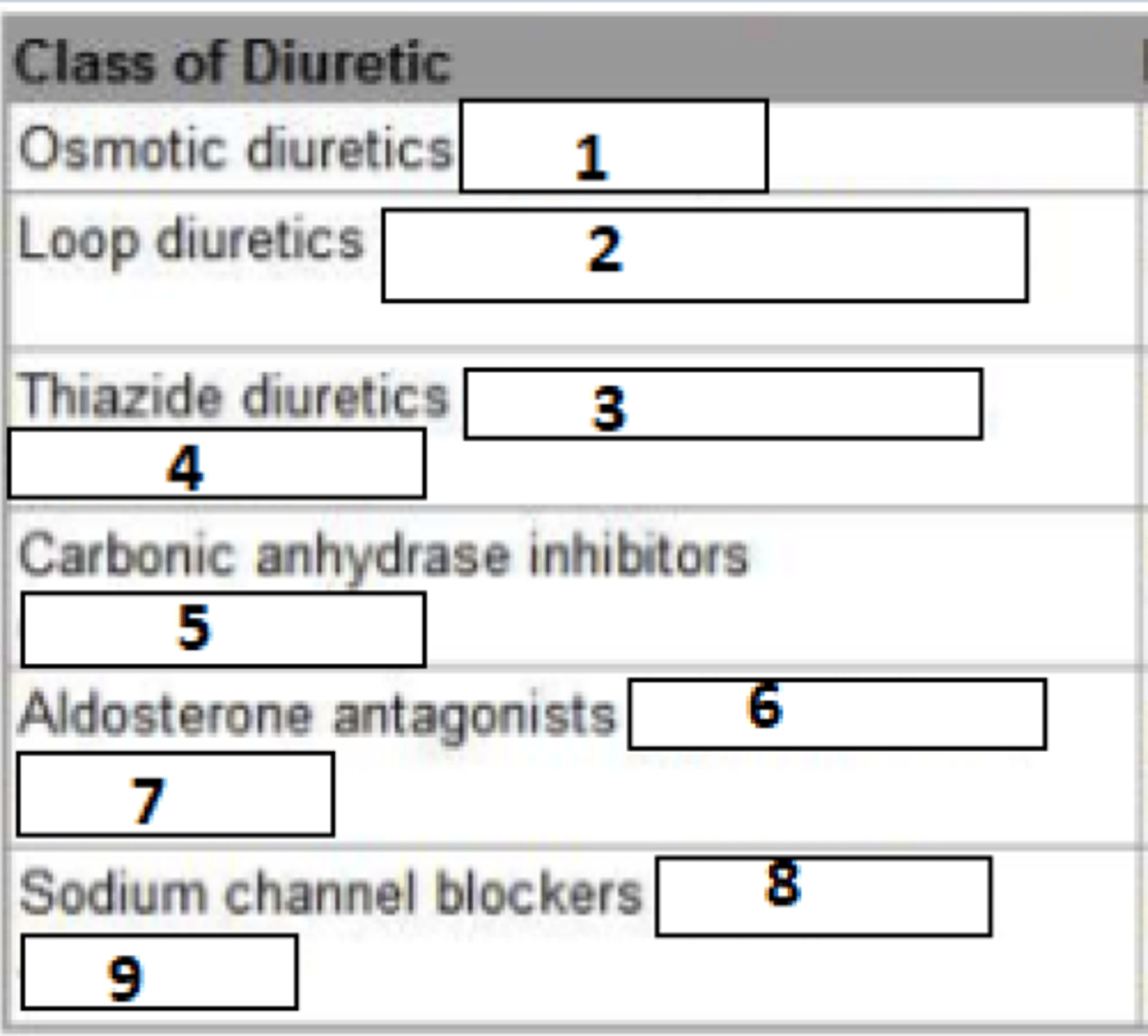
1. Mannitol
2. Furosemide
3. Bumetanide
4. Hydrochlorothiazide
5. chlorthalidone
6. spironolactone
7. eplerenone
8. triamterene
9. amiloride
Name the common medications
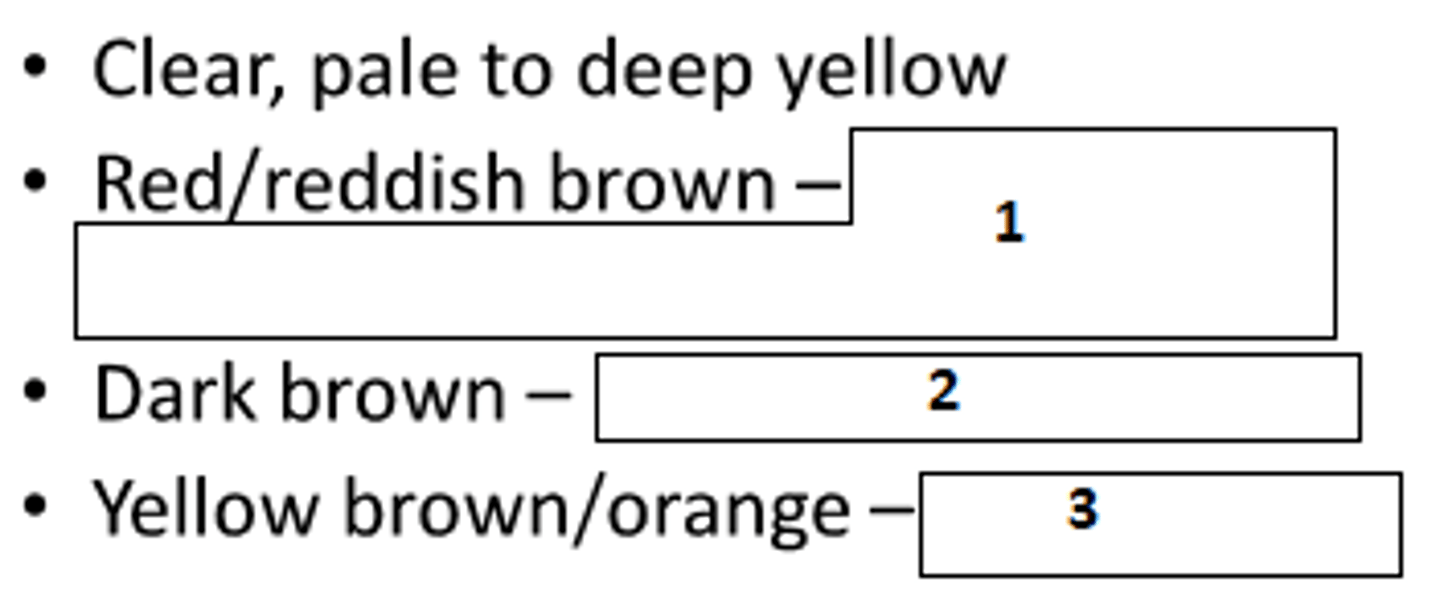
1. haematuria, haemoglobinuria, myoglobinuria
2. methaemoglobinuria
3. bilirubinuria
What do these urine colours indicate?
Presence of bacteria, as these metabolise urea to ammonia
What may ammonia odour of urine indicate
Acetone in urine -> DM
What may fruity smell of urine indicate?
- 95% water 5% solutes
- urea biggest contributor by weight
- nitrogenous wastes: uric acid, creatinine
- electrolytes: Na+, Cl-, PO4-, SO4-
What is the composition of urine normally?
- clear
- slightly hazy
- hazy
- cloudy
- very cloudy
- turbid
How is opacity or urine classified?
- bacteria
- cells
- mucin
- pus
- amorphous crystalline material
What may hazy, cloudy or turbid urine indicate?
1.001-1.035
What is the specific gravity of urine?
600ml-1600ml/24hours
What is the normal daily urine excretion?
diuresis is any increase in excretion, whereas polyuria is a constant abnormally large increase in excretion of urine
What is the difference in diuresis and polyuria?
Stick is dipped into urine and small squares react with certain contents. The dipstick can be compared to a template to assess the contents.
How do urine dipstick tests work?
Presence of intact RBCs in urine
What is haematuria?
Presence of WBCs in urine
What is leukocyturia?
Disease of:
- glomerulus
- tubules
- interstitium
- vessels
Which 4 anatomical categories of kidney disease exist?
- acute or chronic
- usually due to immunological causes
Are glomerular diseases usually acute or chronic? What usually causes these, broadly speaking?
- acute
- toxic or infectious agents
Are tubular disease usually acute or chronic? What usually causes these, broadly speaking?
- kidney stones
- infections
- tumours
What may cause haematuria?
UTI
What may cause painful urination accompanied by fever and chills?
glomerular damage
What may cause proteinuria?
Renal failure
What may cause azotaemia?
Abnormally high levels of nitrogen-containing compounds (such as urea, creatinine, various body waste compounds, and other nitrogen-rich compounds) in the blood
What is azotaemia?
Acute renal failure/acute kidney injury:
- sudden onset
- interruption of kidney function with rapid azotaemia
- decrease in urine output
What is ARF?
Slow onset renal failure due to decline of renal function over months or years. Irreversible loss of functioning nephrons
Briefly define chronic kidney disease
- aging
- comorbidities
- insult (injury) of kidney
What may cause ARF?
- pre-renal: perfusion issue, not enough blood flow
- renal/intrinsic: cellular dysfunction within the kidney itself, filtration dysfunction
- post-renal: obstruction, backlog of urine
What are the 3 main types of acute renal failure?
Heart failure, hypovolaemia, vascular disease including atherosclerosis
What might cause pre-renal ARF?
The kidney is healthy but responds to a perceived low stimulus, increasing reabsorption, causing a big increase in BUN
What problems arise from pre-renal ARF?
- decreased GFR
- oliguria
- elevated sodium retention
How does renal/intrisic ARF manifest?
acute tubular necrosis (toxic or ischaemic), glomerulr disease, acute interstitial nephritis
What may cause intrinsic AFR?
Often due to kidney stone obstruction
What may cause postrenal ARF?
- Depends on duration of obstruction
- Irreversible kidney damage if severe and prolonged
- diagnosed via kidney ultrasound
How might postrenal obstruction manifest?
- Oedema
- hypertension
- decreased GFR
- water and electrolyte retention
- metabolic acidosis
- erythropoetin suppression
- oliguria/anuria
- progressive uraemia
What are the common symptoms of AFR?
- Similar symptoms, but persistant.
- structural damage of the kidney or GFR<60ml/min for 3 months or longer is diagnostic
How does chronic kidney disease compare with ARF?
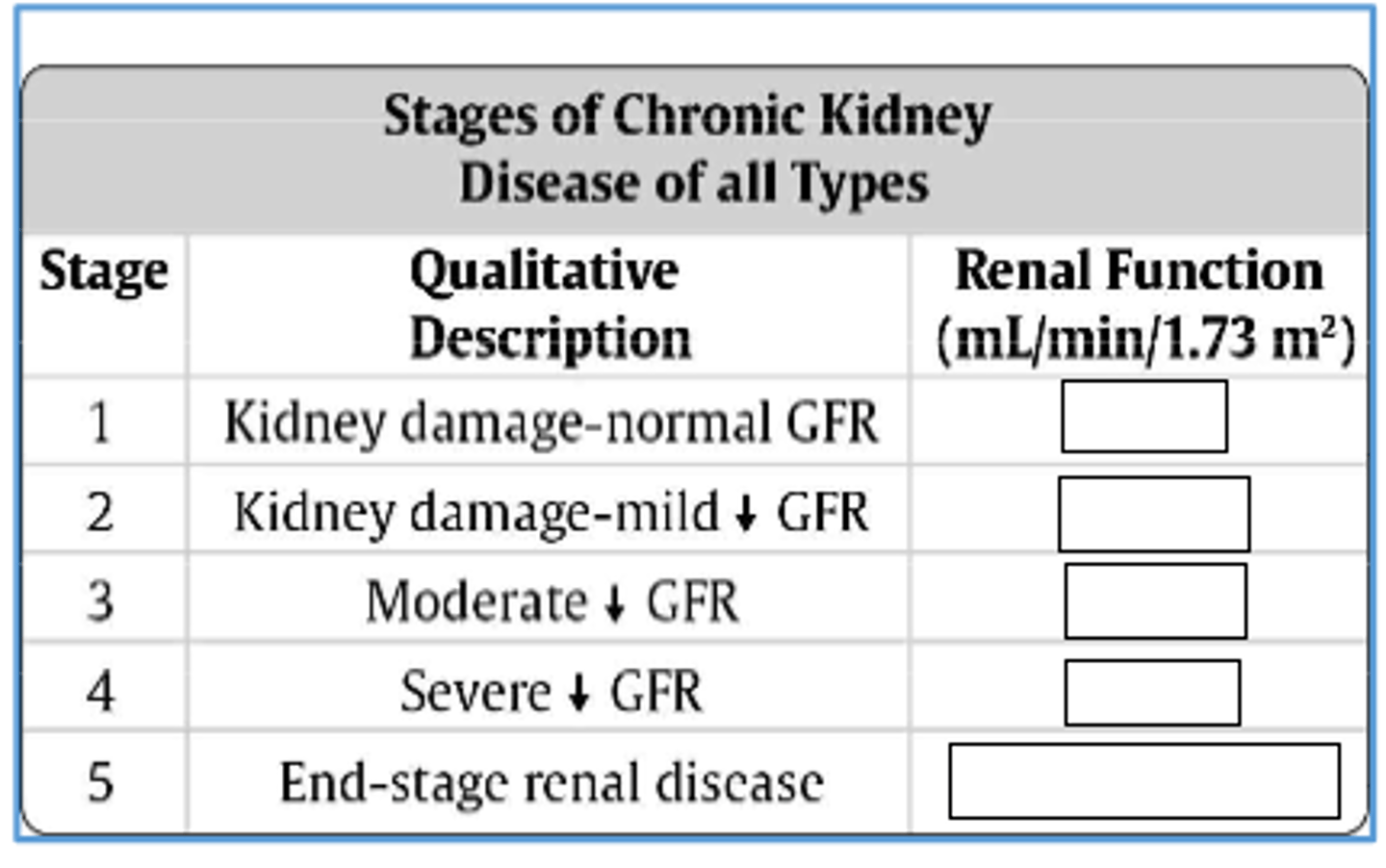
GFR<15ml/min (<5%)
How is end-stage renal disease defined?
- hypertension
- diabetic kidney disease
- vascular disease/ahterosclerosis
- urinary tract obstruction
- recurrent renal stones
- glomerular disease
What may cause chronic kidney disease (ckd)?
- diabetic nephropathy
- membranous glomerulonephritis
- membranoproliferative glomerulonephritis
- minimal change disease
Give 4 diseases/causes which cause glomerular pathology and lead to CKD
- long standing hypertension
- chronic pyelonephritis
- intake of high doses of analgesics
- renal stones, blood clots, tumours -> obstruction
Give 4 diseases/causes which cause tubulointerstitial pathology and lead to CKD
1. >90ml/min
2. 60-89ml/min
3. 30-59ml/min
4. 15-29ml/min
5. <15ml/min or dialysis
Fill the blanks
Decreased renal reserve: no symptoms, normal BUN and creatinine
What happens at 50% of renal function?
Renal insufficiency:
- polyuria, nocturia
- elevated BUN and creatinine
What happens at 20-50% of renal function?
Renal failure:
- Oedema
- Metabolic acidosis (acids not cleared)
- hypocalcaemia
- symptoms of uremia
What happens at <20% of renal function?
End-stage renal/kidney disease:
- uraemic syndrome
What happens at <15% of renal function?
Vitamin D3 is no longer produced
Why does hypocalcaemia occur in renal disease?