TEST 3: Circulatory System (Ch 13)
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
plasma
- liquid portion of the blood including the dissolved substances
- 92% water, 8% salt and organic molecules
- top layer after centrifuging
serum
serum = plasma - fibrinogen
- plasma with clotting factors removed
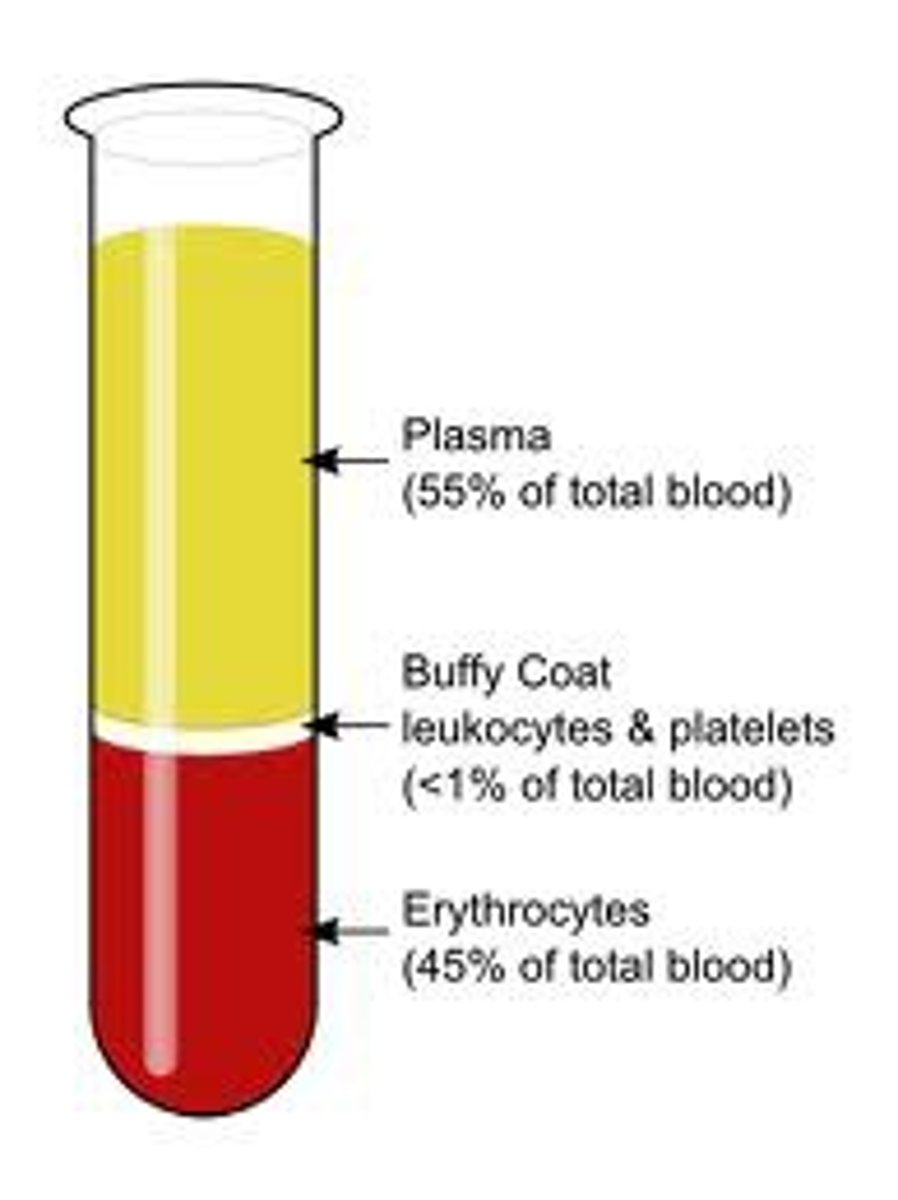
layers after centrifuging
top: plasma (matrix)
bottom: formed elements (55%)
- upper bottom: buffy coat (WBCs and platelets)(<1%)
- lower bottom: RBCs (45%)
hematocrit
percent of blood volume that RBCs make up (usually about 45%)
plasma proteins
- aid in clotting, immune defense, and transport
albumins
- most abundant plasma protein
- good for TRANSPORT
- good at acting as a pH buffer
- produced in the liver
- affect blood osmolarity
blood osmolarity
- concentration of particles that CANNOT pass through the blood vessel walls
- high osmolarity= high H2O; high at VENULE end; response: water removed from the tissues causing volume and pressure to increase at the VENULE end
- low osmolarity= low H2O; low at ARTERIAL end; response: water remains in the tissues causing the volume and pressure to decrease at the ARTERIAL end
globulins
- play a role in transport, immunity, and clotting
fibrinogen
IMPORTANT
- plays a key role in blood clotting
- soluble
- converted into fibrin to produce a clot
viscosity
thickness/stickiness; resistance to flow
formed elements
- WBCs, platelets, and RBCs
= blood - plasma
red blood cells
- erythrocytes
- small, bioconcave disks, no nucleus
-shape: large surface area for fast diffusion
- two functions:
1) transport O2 from the lungs
2) pick up CO2 from the tissues
hemoglobin
- respiratory pigment (red)(bc of iron)
- 4 globin chains (2 alpha, 2 beta)
- each chain contains a heme group (containing 1 molecule of iron each)
heme group
- 1 per globin chain (4 per hemoglobin)
- each contains an iron molecule
- each iron molecule binds to 1 O2 molecule
globin chain
- globin binds CO2
- 4 chains (2 a, 2 b) per hemoglobin molecule
oxyhemoglobin
- oxygenated
- bright red
deoxyhemoglobin
- deoxygenated (hemoglobin not bound to O2)
- maroon
erythropoiesis
- production of RBCs
-originate in hemopoietic stem cells
- erythropoietin: a hormone produced by the kidneys in response to low blood oxygen
Iron (modification during erythropoiesis)
- modified in small intestine/stomach
- transported from the stomach via gastroferritin
- uptake in small intestine
- circulates in the blood; transported by transferrin
- stored in the liver/spleen by ferritin
- when RBCs are destroyed, iron released to plasma and bound to transferrin
gastroferritin
- binds to and transports iron (Fe2+)from the stomach to the small intestine and releases it for absorption
transferrin
- in the blood plasma, Fe2+ binds to ferritin
- in the liver, some transferrin releases iron for storage
- remaining transferrin is distributed to other organs where Fe2+ is used to make hemoglobin, myoglobin, etc
ferritin
- iron binds to apoferritin in the liver to be stored at ferritin
- stores iron
RBC death
- RBCs cannot synthesize new proteins or repair membrane proteins
- membrane eventually becomes fragile and ruptures
- often happens in the liver or spleen (narrow passageways)(iron conserved)
hemolysis
- RBC rupture
- usually in the spleen or liver
- iron conserved
- hemoglobin converted to bilirubin (bile)
Bilirubin
- orange-yellow pigment in bile; formed by the breakdown of hemoglobin when red blood cells are destroyed
- broken down from heme, converted into bile
White Blood Cells (Leukocytes)
- larger than RBCs
- nucleated
- no color (no heme)
- functions (fight infection, destroy toxins etc, recognizing and remembering (infections etc)
- very dispersed; low amount in blood (<1%)
- two categories (granulocytes and agranulocytes)
granulocytes
- 1/2 categories of WBCs
- specific granules
-specific stain
- contain enzymes and chemicals used in defense
- neutrophils, eosinophils, and basophils
agranulocytes
- monocytes and lymphocytes
- lack specific granules --> don't stain (cytoplasm is clear)
platelets (thrombocytes)
- not "cells", but other organelles; fragments of large bone marrow cells
- considered formed elements
- many functions: secrete vasoconstrictors, platelet plugs, clotting factors, clot-dissolving enzymes, and growth factors
blood types
- A, B, AB, O
- based on antigens (and antibodies)
antigens
- complex molecules on the surface of the cell membrane to activate an immune response
- on RBCs
- foreign antigens generate an immune response
-basis for blood typing
- also called agglutinogens
- Ab has both A and B antigens, O has no antigens
antibody
- proteins secreted by WBCs
- bind to antigens for destruction
- immune response to foreign matter
- agglutinins: antibodies in the plasma, bring about transfusion mismatch
agglutination
-antibody molecule binds to antigen, causing the RBCs to clump together
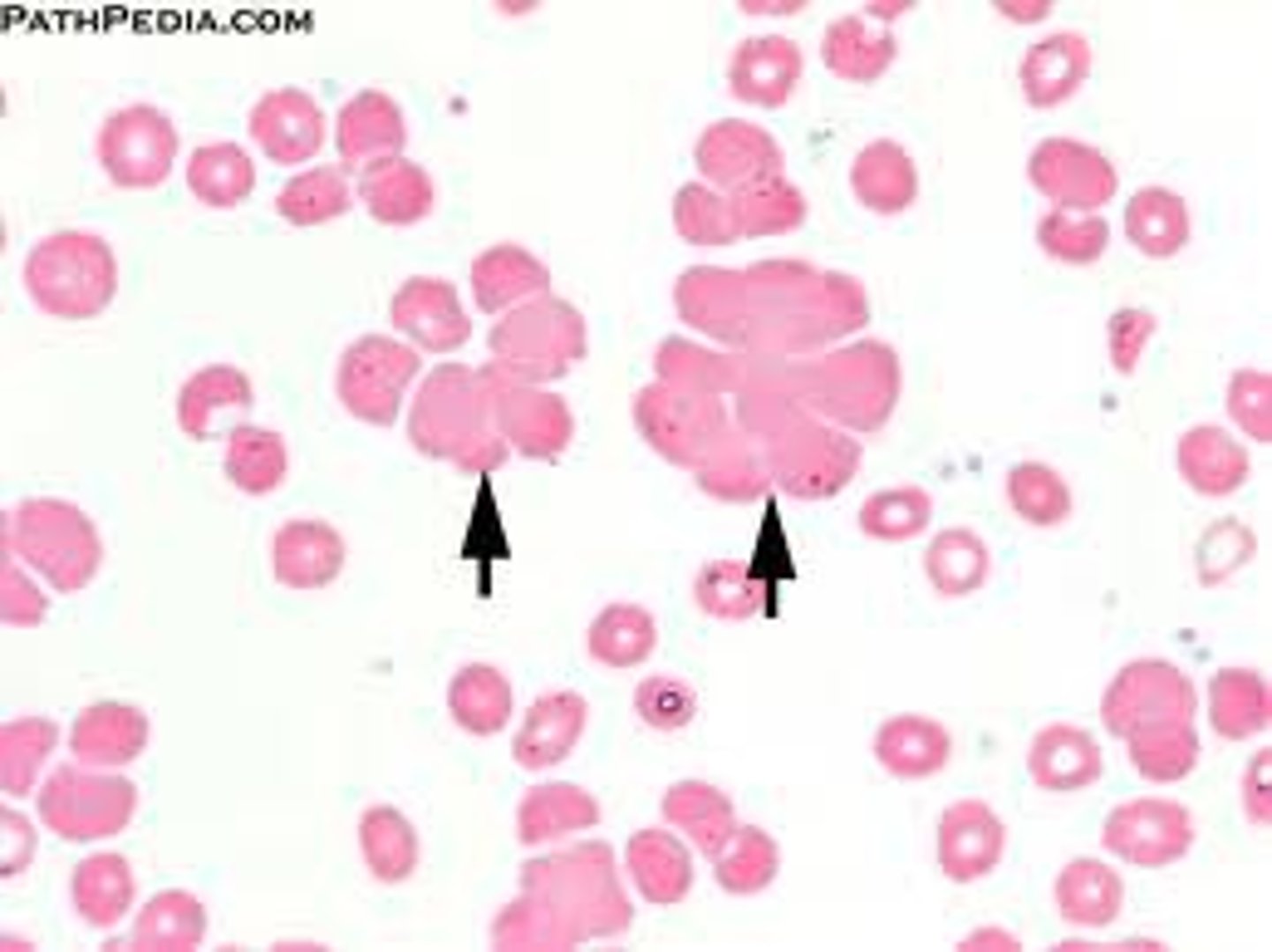
ABO Blood Type
- determined by presence or absence of antigens (agglutinogens) on RBCs
- each antibody can attach to several foreign antigens on several different RBCs at the same time
- blood vessels become blocked, hemolyze, and burst
- "transfusion rxn"
Rh group
- agglutinogens (on surface of RBCs)
- Rh+: have agglutinogen
- Rh-: do not
Anti-D agglutinins (antibodies)
- not normally present in any blood (+ or -)
- forms in Rh- exposed to Rh+ blood
- happens in pregnancy (2nd pregnancy)
- hemolytic disease of the newborn (HDN) mother forms antibodies after first pregnancy
- anti-D antibodies cross the placenta and attack the fetus
RhoGAM
- given to Rh- women during second pregnancy to prevent hemolytic disease of the newborn
- binds to fetal RBCs to prevent the attack
hemostasis
- clotting pathway
- cessation of bleeding
-stops fatal leaks
- 3 mechanisms
hemmorhage
excessive bleeding
step 1 of homeostastis (clotting pathway)
1) vascular spasm
vascular spasm
-reduces blood loss by triggering vasoconstriction
- spasm caused by pain receptors
- platelets then release serotonin (a vasoconstrictor)
- effects: prompt constriction of broken vessel
**-provides time for other 2 clotting pathways
step 2 of homeostasis (clotting pathway)
2) platelet plug
platelet plug
- intact vessels are coated with PROSTACYCLIN (platelet repellent that keeps platelets from binding to walls of blood vessels)
- broken vessel exposes collagen, platelets stick to the collagen
- platelets degranulate (activate) and release ADP (attracts more platelets) and Thromboxane (A2) (promotes platelet aggregation, degranulation, and vasoconstriction)
-POSITIVE FEEDBACK cycle
step 3 of homeostasis (clotting pathway)
3) coagulation (clotting)
coagulation
- most effective defense
-procoagulants produced by liver (present in plasma)
- goal: convert fibrinogen to sticky fibrin
- fibrin adheres to wall of vessel and platelets stick to it
- resultant clot formed, made up of fibrin, platelets, and RBCs
procoagulants
- proteins secreted by the liver
- inactive form always present in plasma
- activation of one causes an activation cascade
- promote fibrin formation by interacting with clotting factors
intrinsic (clotting) pathway
- clotting factors intrinsic to blood begin the cascade
- platelets release factor 12 and activates the cascade of reactions
- ends with factor 8
extrinsic pathway of coagulation
- clotting factors extrinsic to the blood (from damaged tissue)
- factor 3 (thromboplastin)
common pathway
- completes clotting process
- both intrinsic and extrinsic pathways end, factor 10 is activated
- factor 10 activates factor 2, which produces prothrombin, later concerted to thrombin
- thrombin converts fibrinogen to fibrin to form the clot
Common Pathway Summary
Factor X → prothrombin activator;
Prothrombin activator + prothrombin (factor 2)= thrombin;
Thrombin + fibrinogen= fibrin;
Fibrin: sticky mesh, traps platelets, forms clots
factor 10
- activates prothrombin activator (factor 2)
- converted into thrombin by factor 9
thrombin
- produced in common pathway
- converts fibrinogen into fibrin
- forms the clot (fibrin is sticky and traps the platelets)
- positive feedback
fibrin
- the sticky mesh that traps platelets to form a clot
- insoluble (unlike soluble fibrinogen, which it is produced from)
fibrinogen
- plasma protein that is converted to fibrin in the clotting process
- produced by the liver
coagulation vs agglutination
BOTH: blood cell or platelet aggregation
coagulation: platelets stuck together by fibrin
agglutination: RBCs stuck together by antibody molecules
significance of blood viscosity and osmolarity:
- viscosity: controls blood flow resistance
-osmolarity: controls blood concentrations of protein, Na+, RBCs, and water; important for cell nourishment and waste excretion; causes changes in blood volume, which affects blood pressure and flow
structure and function of erythrocytes:
- large surface area for quick diffusion
- carries O2 from lungs to tissues
-picks up CO2 at the tissues and takes to the lungs
structure and function of hemoglobin
- 4 globin chains (2 alpha, 2 beta); globin molecules binds CO2 in the tissues and carry back to the lungs
- 1 heme group per chain, contains 1 iron molecule each; iron molecule binds 1 molecule of O2 in the lungs and carries to the tissues, where it is released
explain what determines a person's ABO and Rh blood types, and how this relates to transfusion compatibility:
- ABO blood type based on antigens on the surface of RBCs
- Rh+/- based on presence or absence of Rh factor (antigen/agglutinogen) on RBC surface
- transfusion compatibility: based on antigens and Rh factor; Rh+ blood can receive either positive or negative blood (neg blood has no Rh factor), Rh- can only receive neg blood; type O blood can only receive O blood (no antigens present), and type AB blood can receive any blood type
describe the body's mechanisms for controlling bleeding
- homeostasis:
1) vascular spasm
2) platelet plug
3) clotting
- clotting pathway: extrinsic or intrinsic, followed by the common pathway which results in fibrin formation and forms a clot with platelets that stick to it in the vessels
what happens to blood clots when they are no longer needed:
clot dissolution:
- platelet-derived growth factor secreted from the platelets
- stimulates damaged tissue replacement
- platelets initiate a reaction chain
- ends with plasmin, which is an enzyme that digests the fibrin and dissolves the old clot
clotting factor deficiencies
- can shut down coagulation cascade if one is missing
- hemophilia: hereditary lack of single protein in cascade that results in the inability to clot (most lack factor 9)
Plasmin
an enzyme that digests fibrin and dissolves blood clots