GI 2: Circulation/Motility
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
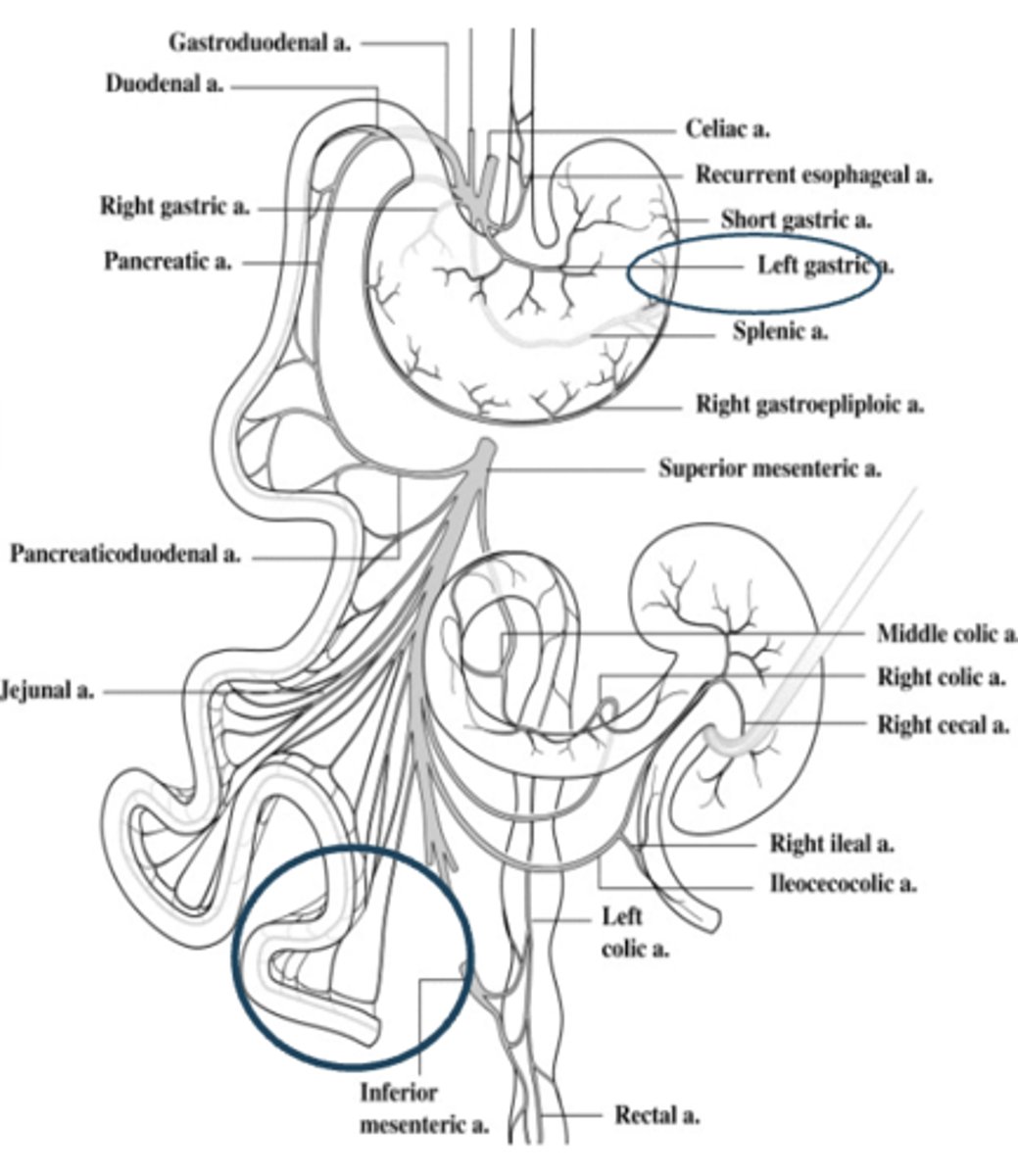
Arterial blood is carried to the GI tract through?
1. Superior mesenteric artery
2. Inferior mesenteric artery
3. Celiac trunk
- Thick artery that will divide into big arteries
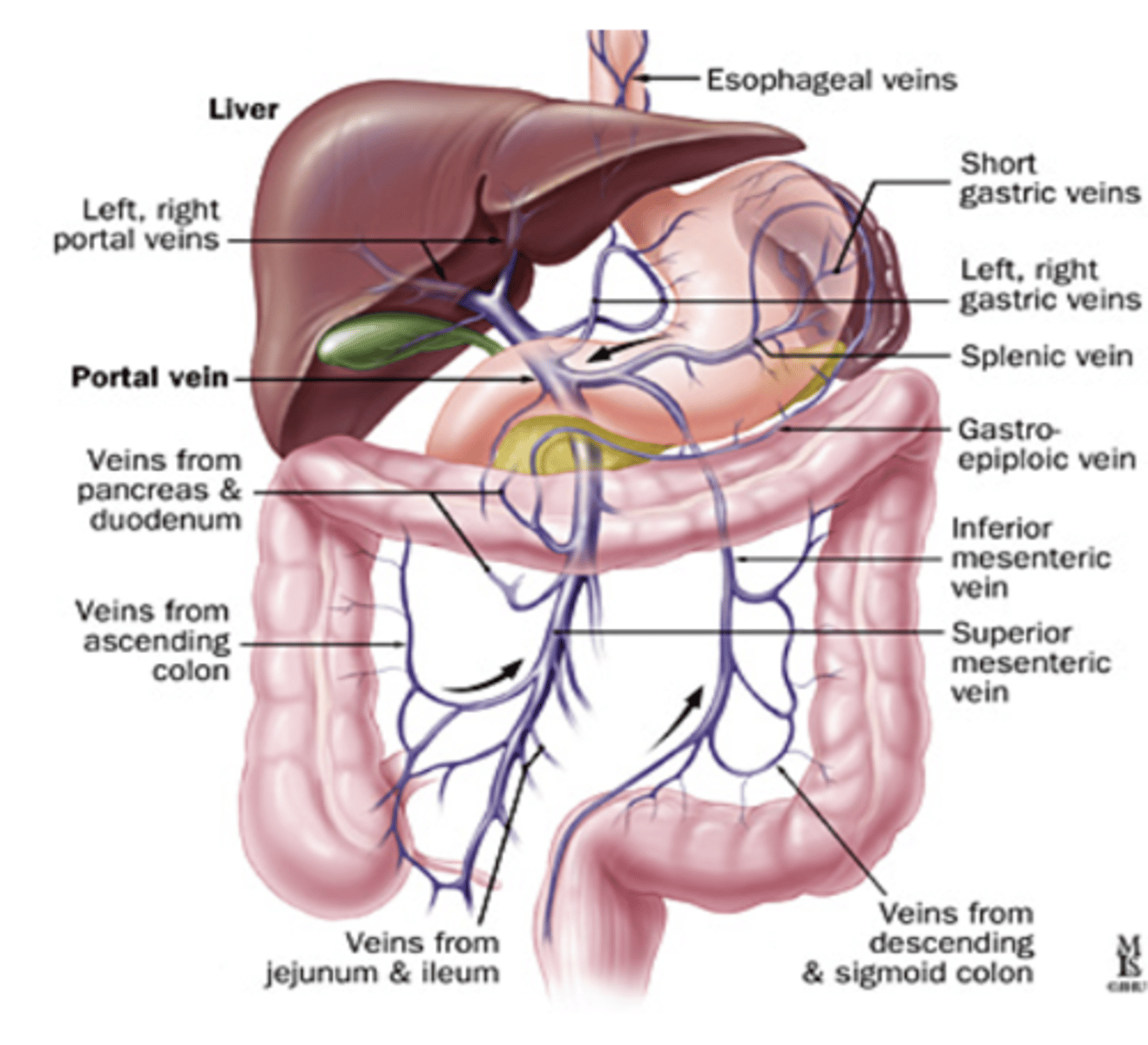
Portal Vein
carries blood to the liver from GI tract, spleen and pancreas
blood flow in the liver
flows through large sinusoids along which specialized cells remove bacteria and particulate mater
- Sinusoids are wide and lined with epithelium and contain macrophages
liver cells function in blood
detoxify the blood from the GI tract
- Chemical/enzymes bind to toxin in blood and removes it
From the liver, blood returns to the circulation through?
the hepatic vein
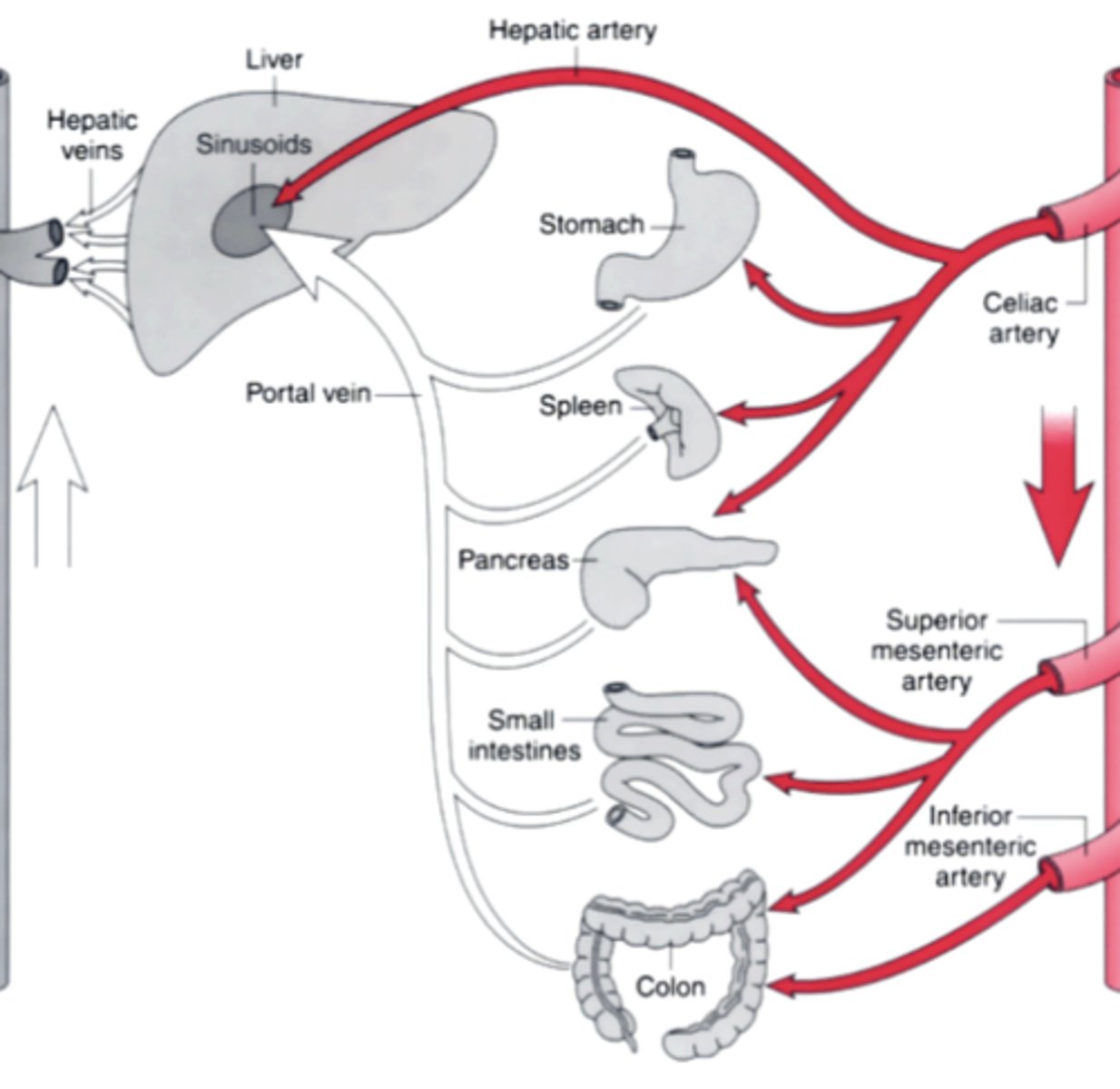
Hepatic Portal System
1. Small intestine absorbs products of digestion
2. Nutrient molecules travel in hepatic portal vein to liver
3. Liver monitors blood content
4. Blood enters general circulation by way of hepatic vein
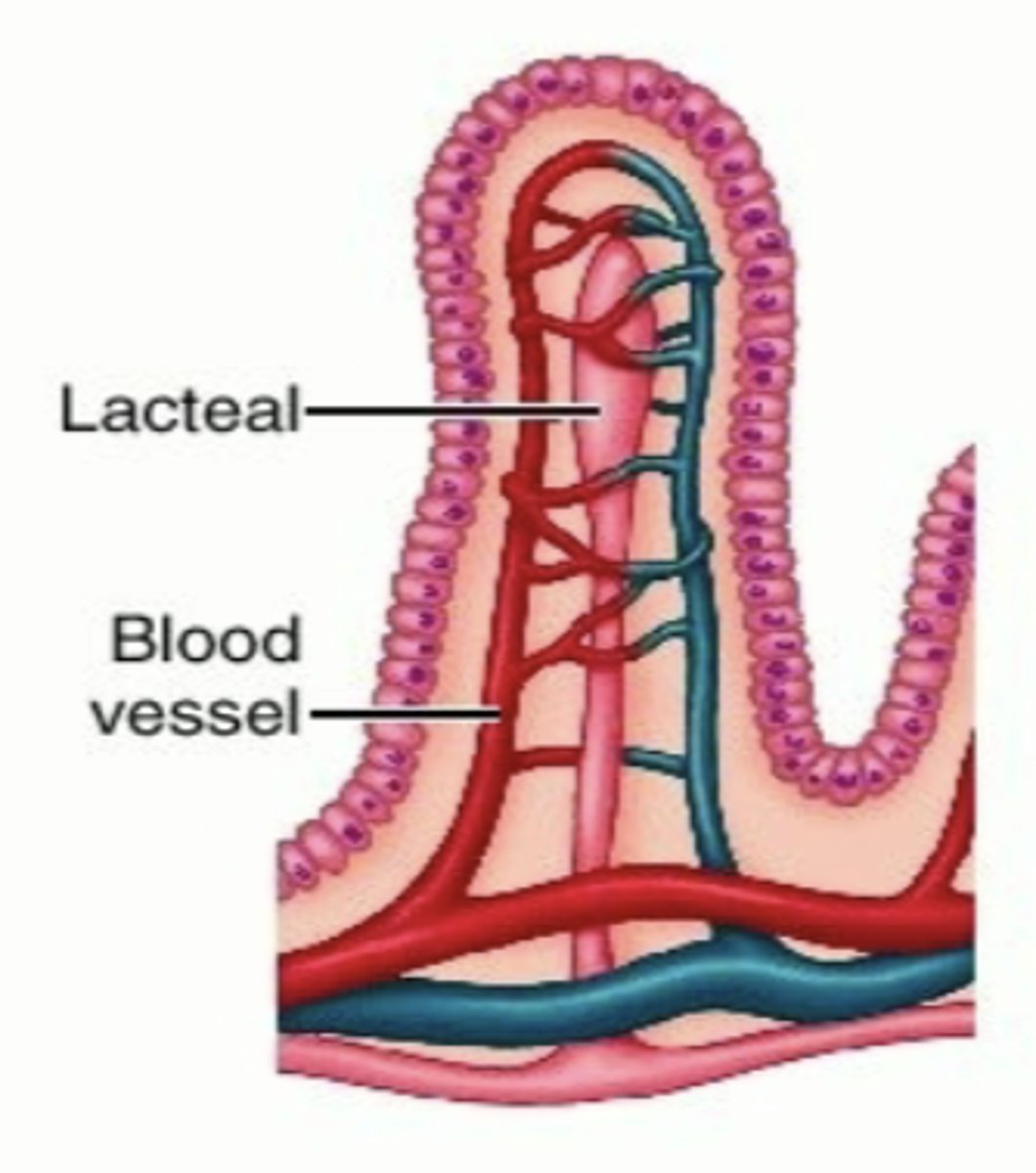
blood circulation in the small intestine
within the villi in the small intestine, smaller arteries have special arrangement
- arterial and venous blood flow are in opposite direction
- blood oxygen diffuses directly from the capillaries into the venules without the need to reach the tip of the villi
splanchnic circulation
Blood flow through the GI tract to organs, such as the spleen, pancreas, and liver
- circulating arteries penetrate the wall and branch into smaller arteries within the muscle, mucosa, and submucosa
− brings blood from aorta to the wall of the
gut
splanchnic circulation arteries
1. Superior mesenteric artery:
- To pancreas, small intestine, and proximal colon
2. Inferior mesenteric artery:
- To distal colon
3. Celiac trunk:
- hepatic artery to liver, spleen, pancreas, and stomach
Within intestinal villi, oxygen diffuses from arterioles to venules before reaching the tip. What is the consequence of this countercurrent flow?
Predisposes the villus tip to ischemia
Portal Circulation
1. Venous blood from the GI enters the liver through the portal vein
2. In the liver, the portal vein branches into sinusoids
- sinusoids receives blood from artery and portal vein
3. As the blood traverses the liver sinusoids:
- reticuloendothelial cells along the wall filters the blood
- macrophages in sinusoids clean
4. Liver cells detoxify the blood and use nutrients absorbed from the GI
5. Blood then enters the central vein which then empties into the hepatic vein
- portal vein leaves the liver via the hepatic
vein
GI Blood Flow: Splanchnic & Portal Circulations Overview
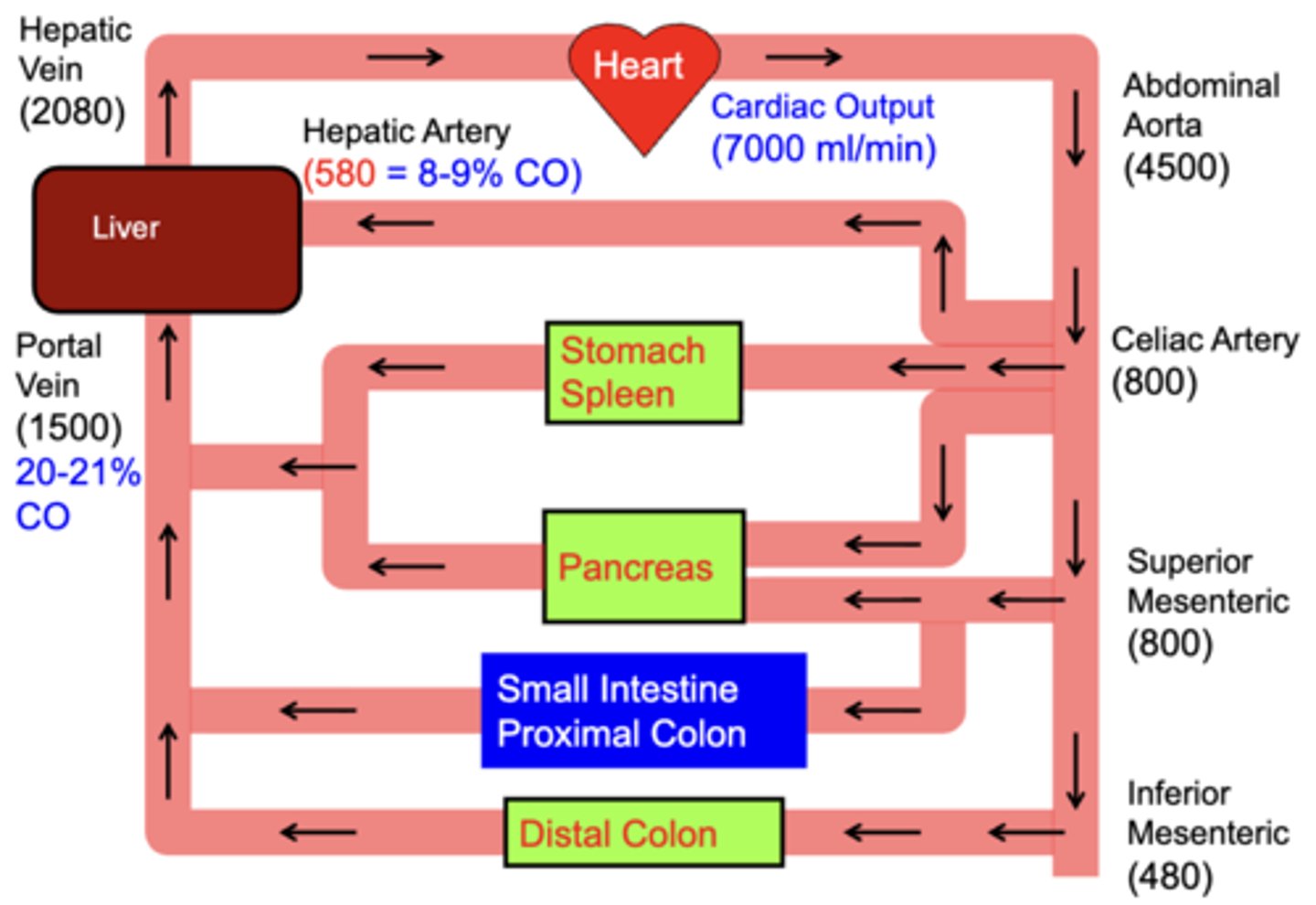
Which vessel carries nutrient-rich, deoxygenated blood from the GI tract to the liver?
portal vein
functions of motility
mixing + propulsion
types of motility contractions
segmentation and peristalsis
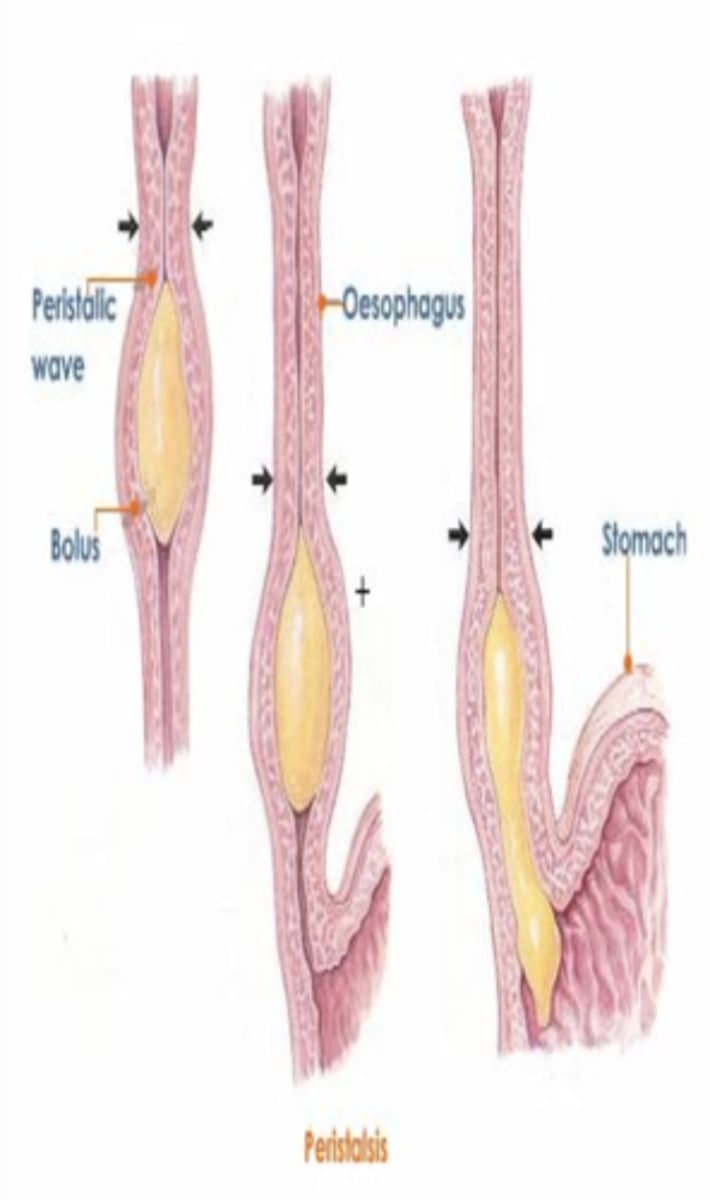
peristalsis
Propulsive movement: series of alternating contractions and relaxations of smooth muscle that lines the walls of the digestive organs and that forces food to move forward
- inherent property of smooth muscle
• Stimulation: Distension, Chemical, physical
Effectual peristalsis requires
1. active myenteric plexus
2. Contractile ring in circular muscle behind the point of distension
Absence of myenteric plexus
• Congenital megacolon
• Atropine
Peristalsis results from?
the initiation of a unidirectional Spreading Contraction of the Circular Muscle
- typically forms behind a food bolus and serves to move the bolus in the aborad direction
- the contractile wave is usually coordinated with Longitudinal Muscle layer contraction and Circular Muscle layer relaxation ahead (aborad) of the bolus
peristalsis mainly results in?
Propulsive Action on GI contents which causes net movement of material
- Some Mixing of contents also occurs
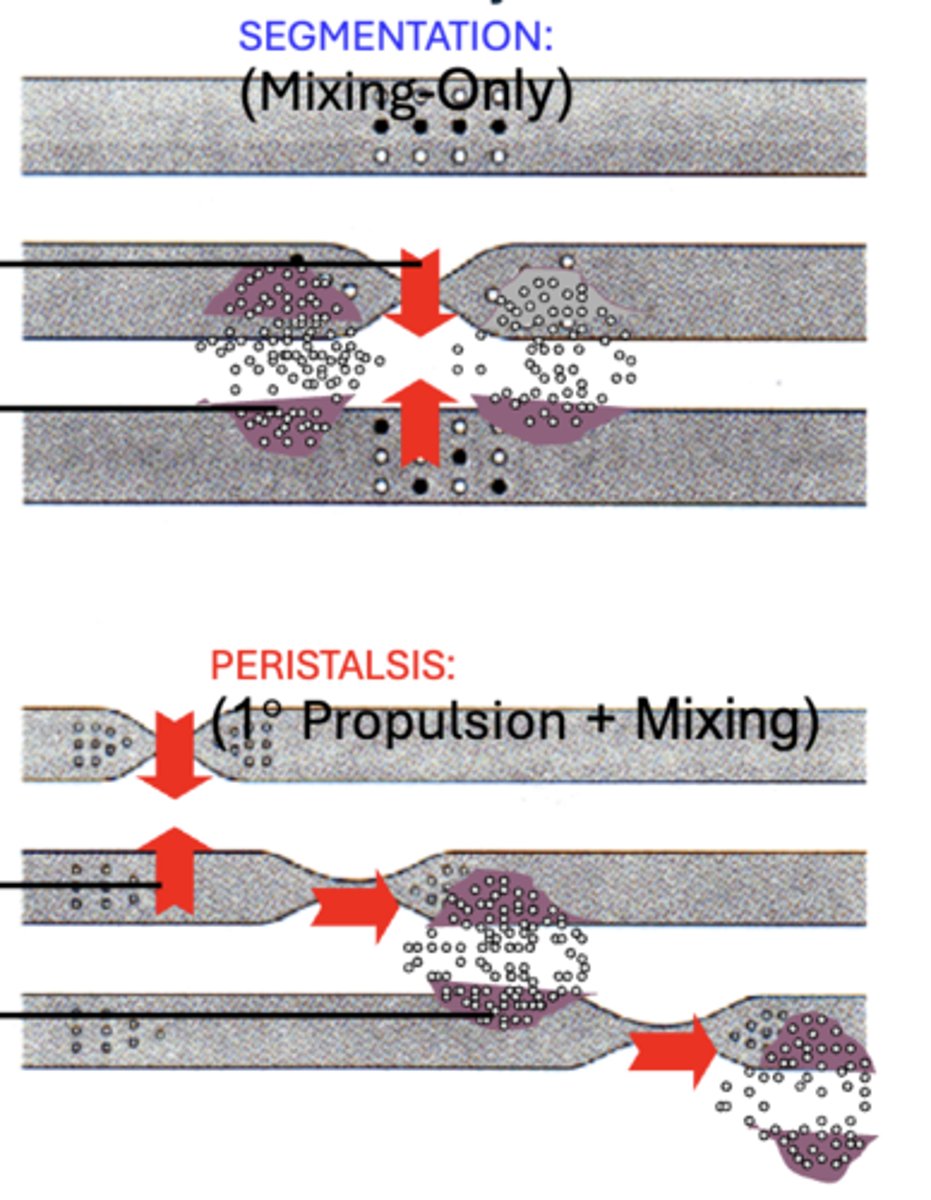
Segmentation
Mixing movement:
- Results from a Focal Contraction of the primarily Circular Muscle layer that constricts the lumen and compresses GI contents at the site
- often coordinated with Longitudinal Muscle layer contraction and Circular Muscle layer relaxation on either side of the constricted site
segmentation primarily results in
a Mixing Action
- reduces food particle size
- homogenizes particles with digestive enzymes and other secretions
- exposes contents to the mucosal surface
Segmentation does NOT typically result in?
significant net movement (Propulsion) of material along the tract
Basic Actions of GI Smooth Muscle Layers
SEGMENTATION: (Mixing-Only)
- Focal Contraction of Circular Layer
- Bilaterally:
• Long. Layer Contraction
• Circ. Layer Relaxation
PERISTALSIS: (1° Propulsion + Mixing)
- Spreading Contractile Wave of Circular Layer
- Aborad to Bolus:
• Long. Layer Contraction
• Circ. Layer Relaxation
Congenital Megacolon
Congenital disorder of peristalsis of distal bowel
- caused by absence of parasympathetic ganglion cells in the myenteric plexuses
Atropine
Paralyze cholinergic nerves of smooth muscle by blocking acetylcholine
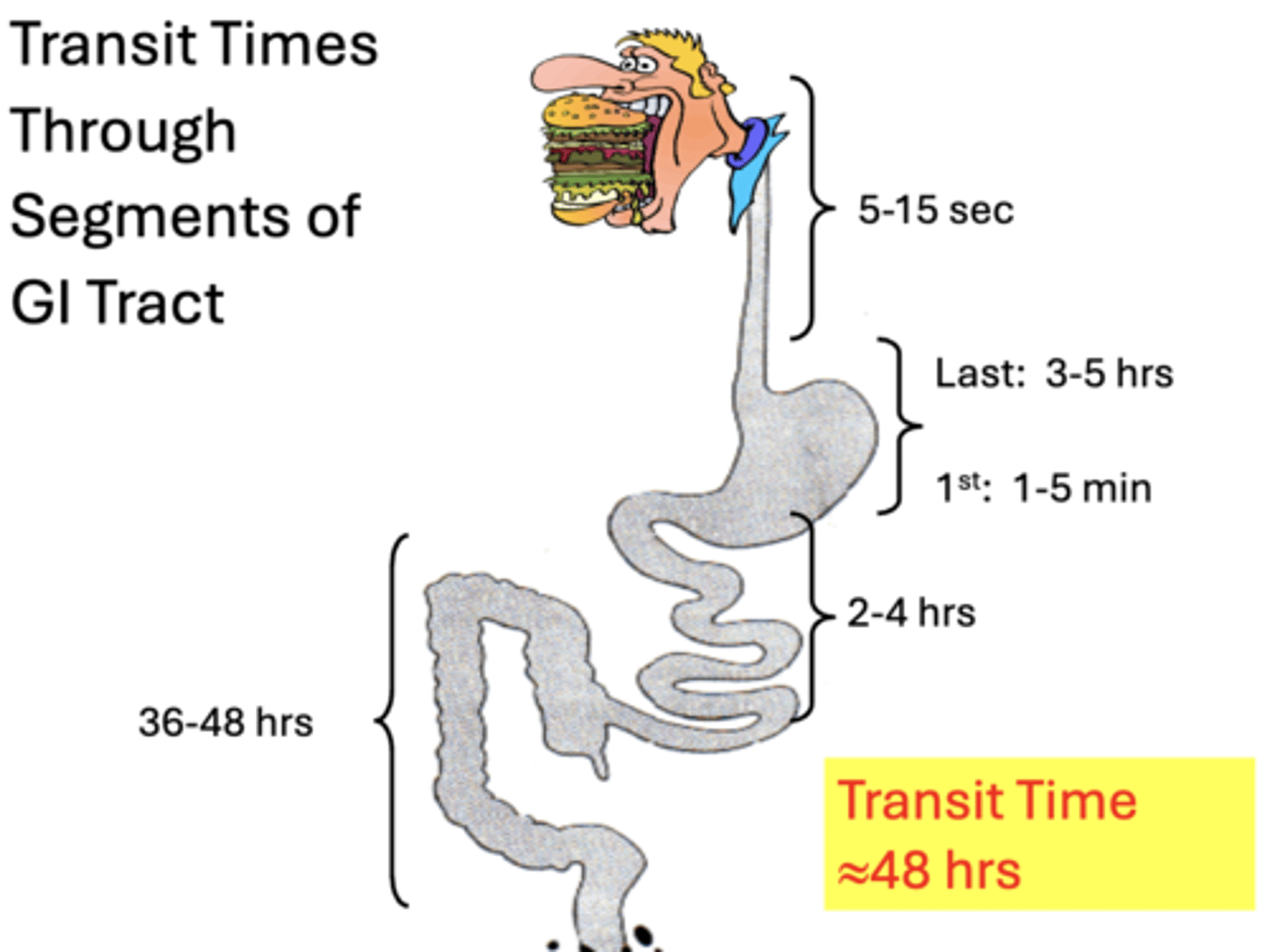
Transit Times Through Segments of GI Tract
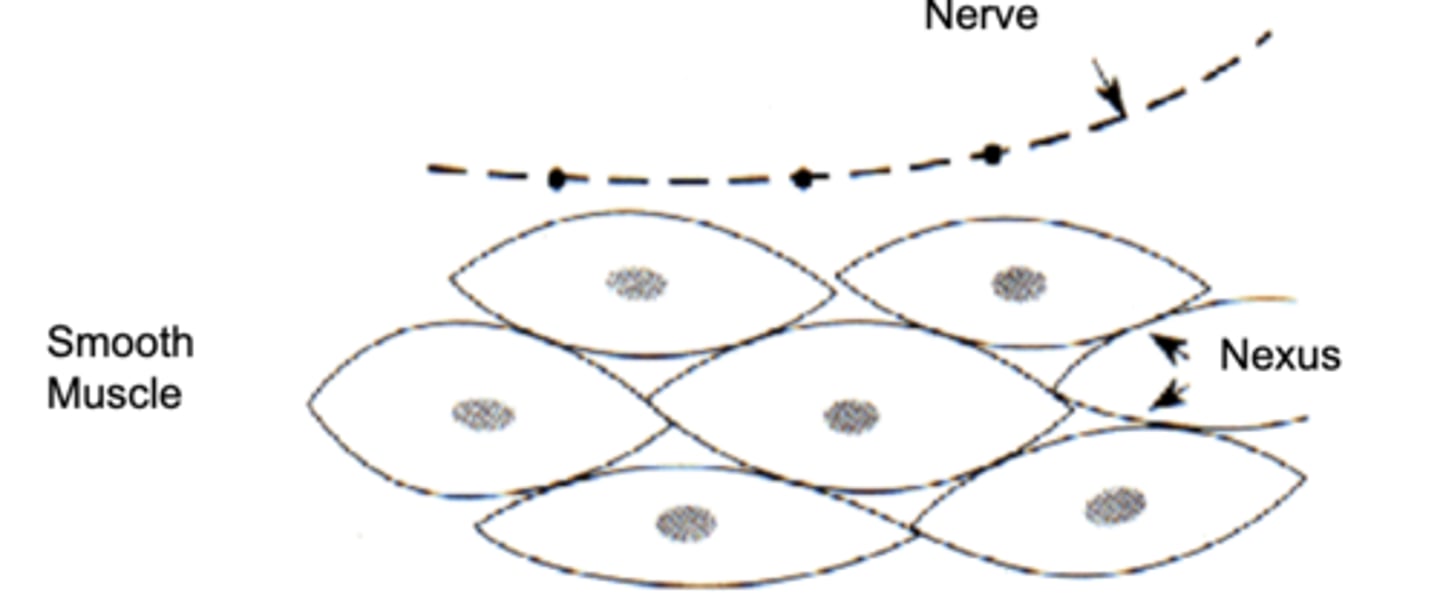
Smooth muscle + GI motility
− Contraction of smooth muscle layers increases GI motility
− Relaxation of smooth muscle decreases GI motility
Anatomy of Smooth Muscle
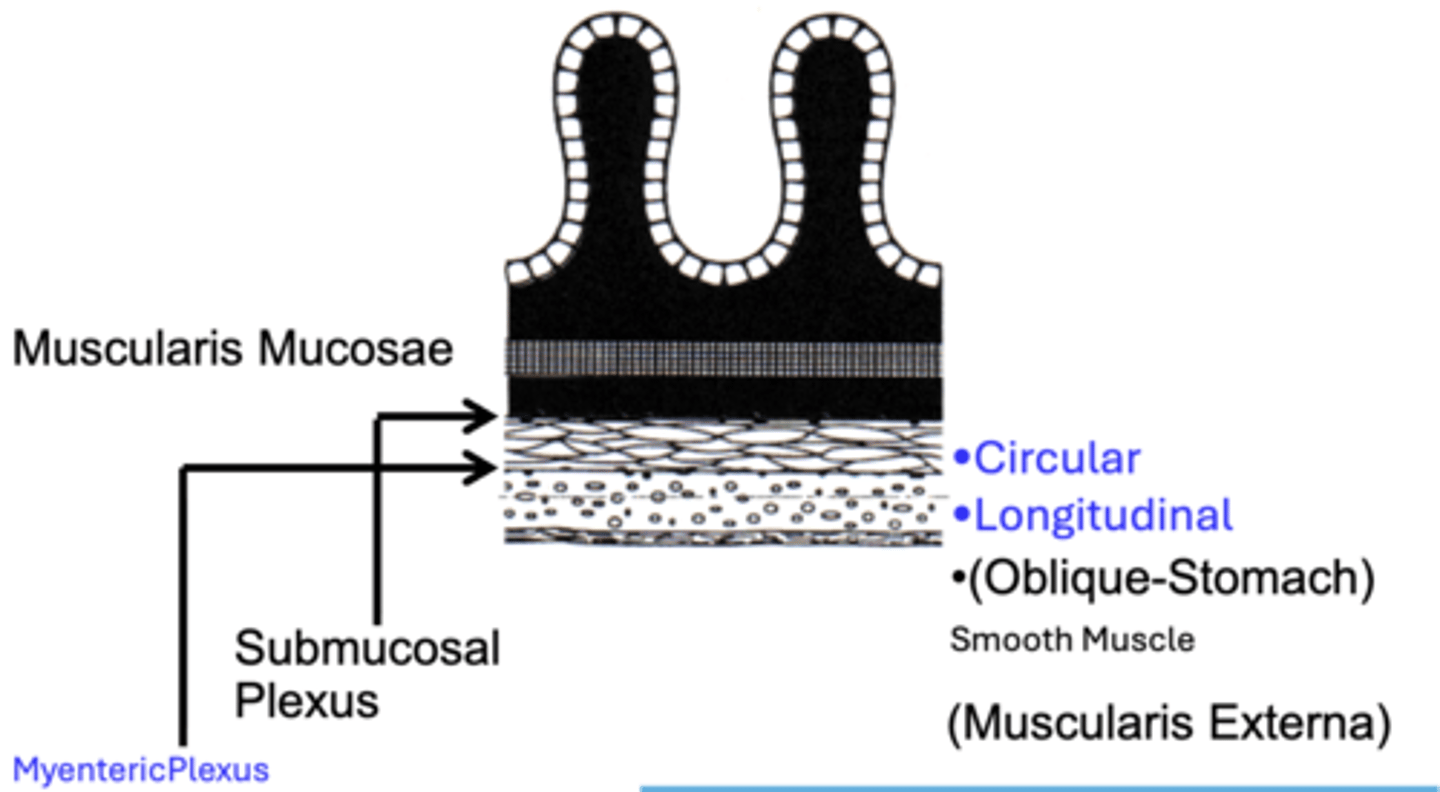
Gastrointestinal motility functions are carried out primarily through?
contractile activities of outer smooth muscle layers (muscularis externa) lining the tract
- voluntary skeletal muscle activities are not involved
− circular and longitudinal muscle layer are responsible for performing most GI motility
o Regulated through the myenteric plexus
muscularis mucosae layer
thinner smooth muscle
- involved in altering the mucosal surface area in coordination with circular and longitudinal muscle actions
Smooth muscle sphincters
o Upper esophagus: oral cavity – esophagus
o Lower esophagus: esophagus – stomach
o Pyloric sphincter: stomach – duodenum
o Illeocecal sphincter: ileum – colon
o Colorectal sphincter: colon – rectum
o Internal anal sphincter: rectum – anal canal
o External anal sphincter: anal canal – external
GI sphincters function
restrict or facilitate orad and/or aborad movement of GI contents between different GI segments by increasing or decreasing lumen diameter
Constriction/Relaxation of Smooth Muscle Sphincters
Relaxation: increases GI propulsions (PNS)
Constriction: decreases GI propulsions (SNS)
The absence of myenteric plexus neurons in a bowel segment results in
congenital megacolon (hirschprung disease)
control of motility
primarily neural control
1. Extrinsic Autonomic Control
2. Enteric Autonomic Control
3. Voluntary & GI Peptide Control
Extrinsic Autonomic Control of Motility
•↑ Parasympathetic: = ↑ Propulsion & Mixing
•↑ Sympathetic: = ↓ Propulsion & Mixing
Enteric Autonomic Control of Motility
• Primarily Myenteric Plexus (Muscularis Externa)
• Integrates w/ Extrinsic Controls
• Allows Fine Local Control
• Coordinates Interregional Propulsive/Mixing Movements
Voluntary & GI Peptide Control of Motility
Overall Minor Role
• Voluntary – Swallowing Reflex & Defecation Control
• GI Hormones – Motilin: Stomach Motility Action
Intrinsic myogenic control
Some smooth muscle regions of the GI tract are under tonic contraction, also known as intrinsic basal tone
- the “natural” state of the muscle without extrinsic influences is in the contracted state
- distinguished because it is initiated without apparent extrinsic input from nerves or hormone factors
− tone is generated intrinsically by smooth muscle cells
ex. lower esophageal sphincter
Tonic Contractions can be transiently modulated by?
certain extrinsic factors
o Autonomic neural input
o Hormones & peptides
this mechanism can be viewed as a separate control mechanism used in the regulation of GI motility
Which statement about intrinsic myogenic control is correct?
A. Refers to neural control from myenteric plexus
B. Requires circulating hormones
C. Originates from smooth muscle's inherent contractile tone
D. Mediated exclusively by sympathetic input
C. Originates from smooth muscle's inherent contractile tone
Parasympathetic vs. Sympathetic effects on motility include:
A. Both increase motility
B. Both inhibit motility
C. Parasympathetic increases, sympathetic decreases motility
D. Parasympathetic decreases, sympathetic increases motility
C. Parasympathetic increases, sympathetic decreases motility