OPP 3 - Knee + Ankle Pain (Lect & Lab)
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
MCL
from medial epicondyle (femur) to medial margin (tibia), also attaches to medial meniscus and joint capsule
less flexible, more prone to injury
LCL
From lateral epicondyle (femur) to fibular head
no contact w/ meniscus or joint capsule
Arcuate Popliteal Ligament
“Y” shaped, from lat. epicondyle (femur) and intercondylar area of femur to fibular head
fibers blend w/ posterolat. joint capsule
ACL
from posteromed. lat. femoral condyle to anteromed. intercondylar area of tibal plateau (posterior on femur to ant on tibia aka: starts at back, attaches at front)
restricts tibia from sliding forward on femur
PCL
Attaches from the anterolateral aspect of the medial femoral condyle to the posterior aspect of the tibial plateau (starts front, ends back)
Restricts the tibia from sliding backward on the femur
Fibular Head Motion
reciprocal motion
distal fib follows tib rotation
Internal rotation of the tibia brings the distal fibula anteriorly and the fibular head posteriorly.
External rotation of the tibia brings the distal fibula posteriorly and the fibular head anteriorly.
Musc that flex the knee
Posterior muscles:
Biceps Femoris, Semimembranosis, Semitendonosis, Popliteus, Gastrocnemius, Sartorius, Gracilis, plantaris
Musc that extend the knee
Ant. thigh muscles: Rectus Femoris, Vastus lateralis, Vastus Medialis, Vastus Intermedius
Femur and Tibial motion
During tibiofemoral flexion, the femoral condyles roll posteriorly and glide anteriorly on the tibia.
Note: Tibiofemoral joint has very little active abduction and adduction, and passive abduction and adduction tends to increase with ligamentous laxity, whether from age or trauma.
Musc that int. rotate the knee joint
Medial thigh muscles: Popliteus, Semimembranosus, Semitendinosus, Sartorius, Gracilis
Musc that ext. rotate the knee joint
biceps femoris
Femoral neck angle
angle b/t anatomic & longitudinal axis of femoral neck, normal “angle of inclination” = 120-135 degrees
Coxa valgus (>135 degrees) —> Will lead to Genu Varus
Coxa varus (<120 degrees) —> Will lead to Genu Valgus
Q-angle (quad)
angle b/t quad musc (primarily rect fem) and patellar tendon = where lines from ASIS to patella mid point & tibial tubercle to patellar mid point cross
A Q-angle less than normal may be associated with genu varum or patellofemoral dysfunction.
A Q-angle greater than normal is often associated with genu valgum, subluxing patella, increased femoral anteversion, or increased lateral tibial torsion.
IT band
Attaches the tensor fasciae latae and gluteus maximus muscles to the ilotibial tubercle of the tibia (Gerdy’s tubercle).
Helps stabilize the knee joint
Often related to pelvic dysfunction
Pes Anserinus tendon
sartorius, gracilis, semitendinosus (SAy GRACe before TEa) [from ant to post]
Knee neurovasc
femoral A&V pass post thru adductor canal, become popliteal A&V
sciatic branches into tibial N and common fibular N
fibular N entrapment/injury
can cause foot drop (L5 nerve root)
also can be facilitated by fib head dysfunction
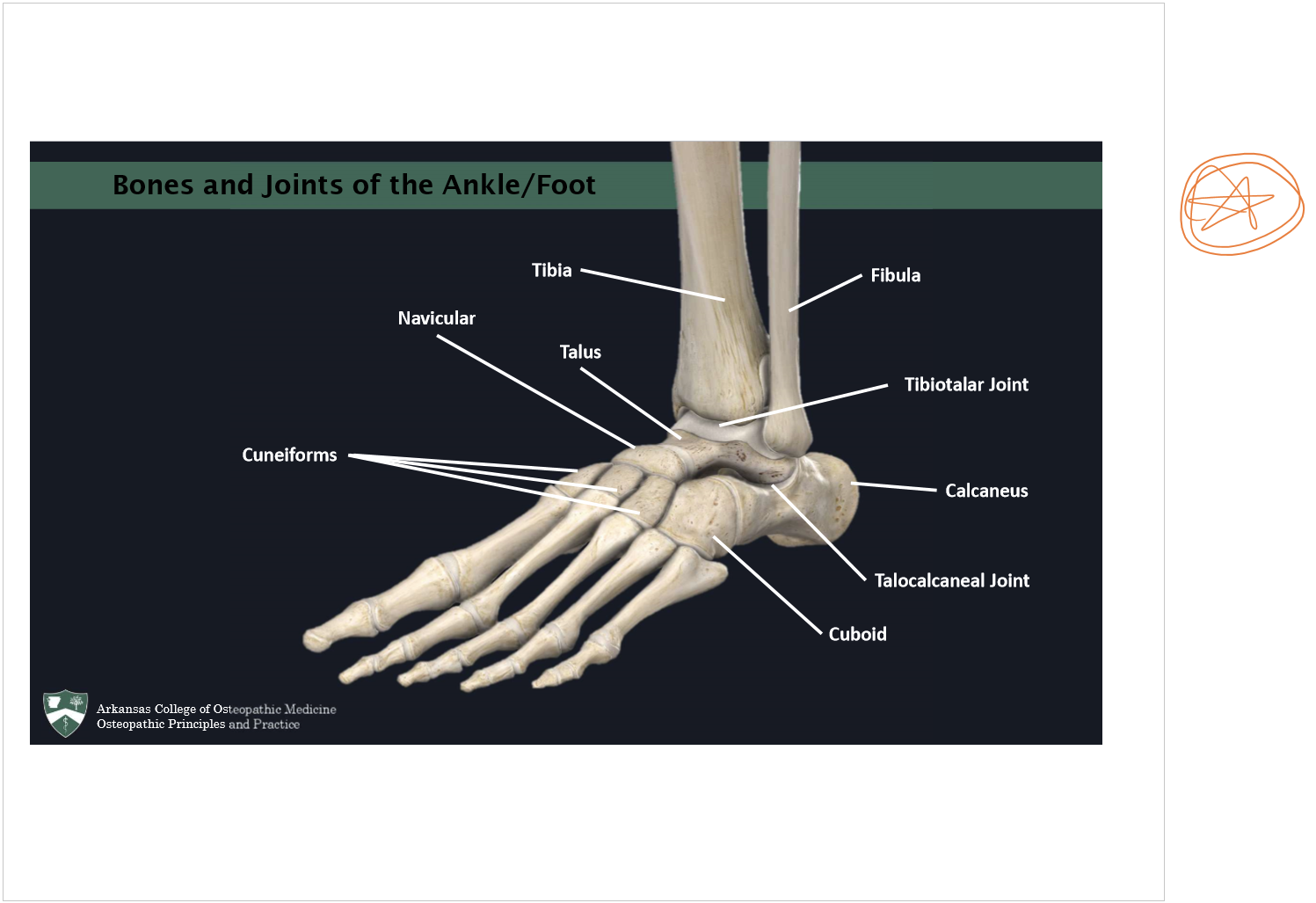
Foot/ankle bones
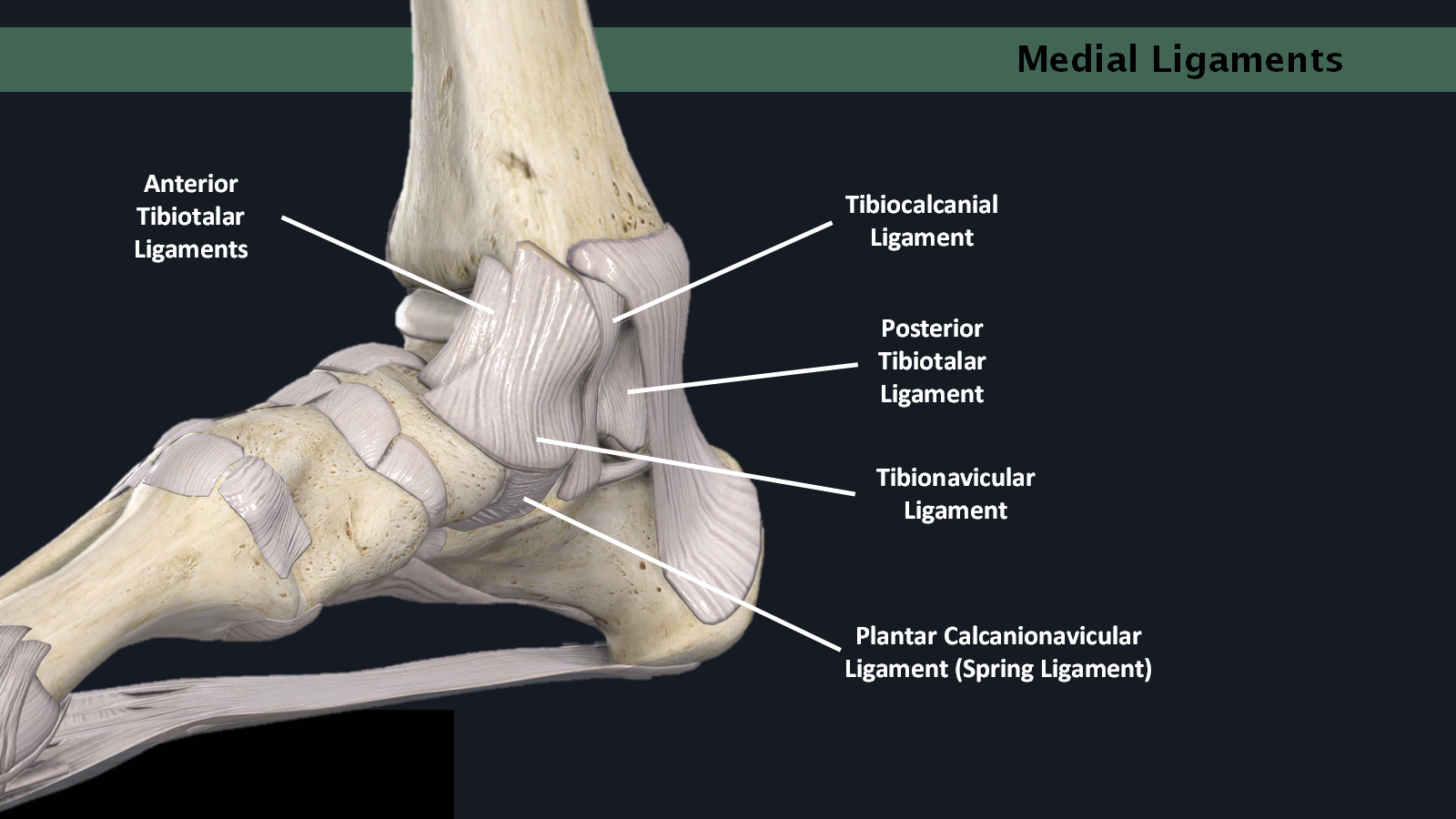
Medial ankle ligaments (deltoid ligs)
Ankle ligs vulnerable during INVERSION
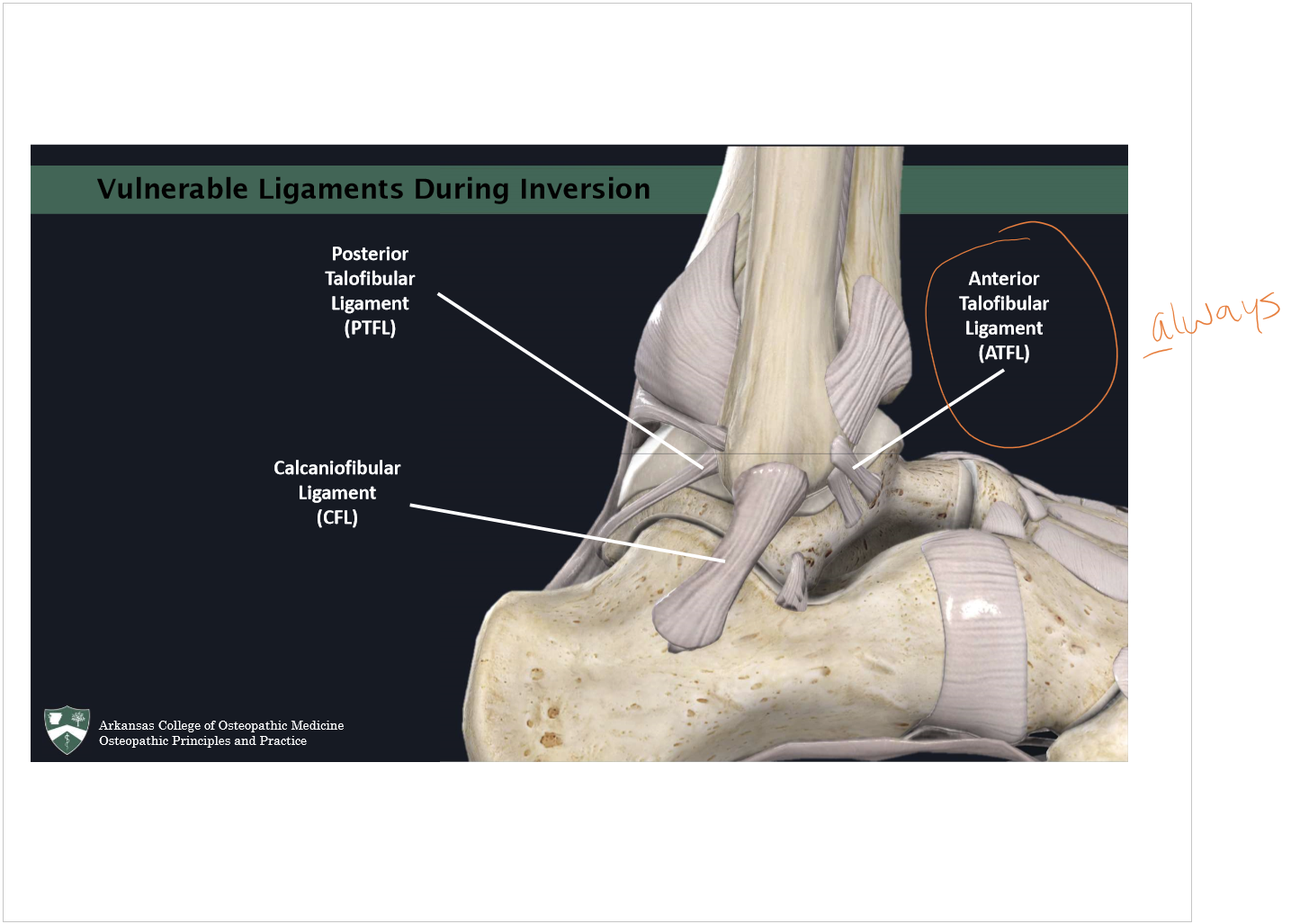
Always tears first
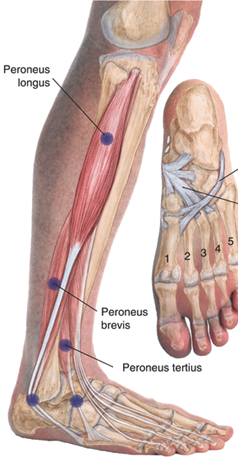
Peroneus Longus, Brevis, and Tertius
The peroneus muscles originate from the fibula.
Brevis and Tertius insert on the base of the fifth metatarsal.
Longus inserts on the cuboid and base of the first metatarsal.
Function: Everts and plantarflexes the foot.
Quadratus plantae
Origin: Medial and Lateral aspects of the plantar surface of the calcaneus.
Insertion: Tendon of flexor digitorum longus muscle.
Function: pulls on the flexor digitorum longus muscle to assist in flexion of the 2nd-5th phalanges.
Tarsal Tunnel contents
Contents (anterior to posterior):
Tibialis Posterior
Flexor Digitorum Longus
Tibial Artery
Tibial Nerve
Flexor Hallucis Longus
“Tom Dick ANd Harry”
Clinical exam steps
inspect, palpate, active & passive ROM, neuro, special tests
combined motions of the ankle
SUPINATION = plantarflexion + adduction + inversion
PRONATION = dorsiflexion + abduction + eversion
Anterior Drawer test
Testing: ACL
Procedure: pt supine, hip flexed 45*, knee flexed 90*, pull ant
+ test: visible and palpable anterior displacement of the tibia with a soft end point.
Lachman’s test
Testing: ACL
Procedure: hold pt’s knee b/t 15-30* of flexion, (b/c in this position, stabilizing function of ACL is essential to brake and pivot direction)
+ test: excessive motion of the tibia in respect of the femur without a hard stop.
Posterior drawer test
Testing: PCL
Procedure: pt supine, hip flexed 45*, knee flexed 90*, translate post
+ test: visible and palpable posterior displacement of the tibia with a soft end point.
Valgus and Varus stress tests
Testing: MCL and LCL
Procedure: pic
+ test:
Laxity during valgus stress is suggestive of MCL injury.
Laxity during varus stress is suggestive of LCL injury.
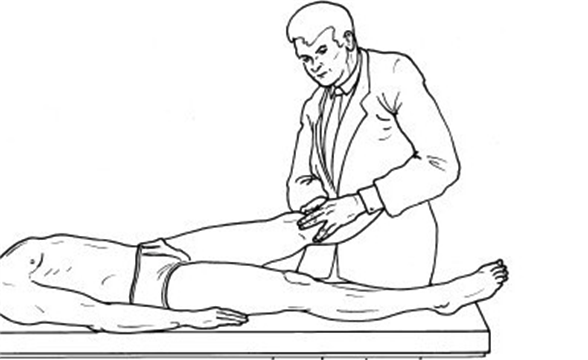
Apley Compression test
Testing: meniscus injury
Procedure:
+ test: Pain or reproduction of symptoms is suggestive of meniscus injury.

McMurray’s test
Testing: meniscus injury
Procedure: supine with the knee and hip of the affected leg in maximum flexion. The examiner grasps the patient’s knee with one hand and the patient’s foot with the other. Holding the patient’s lower leg in maximum external and abduction or internal rotation and adduction, the examiner then passively extends the knee into 90° of flexion. (ROTATION IS OF THE LOWER LEG)
+ test:
Pain during external rotation and abduction is suggestive of medial meniscus injury.
Pain during internal rotation and abduction is suggestive of lateral meniscus injury.
Thessaly Test
Testing: meniscus injury
Procedure: Have patient stand on only the affected leg, they may hold onto provider for support. Ask patient to rotate their body overtop the tibia 3x with the knee flexed at 20 degrees.
+ test: Pain or reproduction of symptoms is suggestive of meniscus injury.
Patellar grind test
Testing: patellofemoral pain
Procedure: pt supine, dr applies post. directed pressure on sup. patella and has pt flex quads
+ test: reproduction of pain
Ankle Anterior drawer test
Testing: ATFL
Procedure: The patient lies supine with the knee slightly flexed to neutralize the pull of the gastroc muscle. With the ankle joint held at 10 to 15° of plantar flexion, the examiner grasps around the heel with one hand and stabilizes the tibia from the anterior side with the other. After asking the patient to relax the muscles, the examiner pulls the heel forward while continuing to stabilize the tibia with the other hand.
+ test: visible and palpable anterior displacement of the talus and calcaneus with a soft end feel on injured side (compared to other side).
Ankle posterior drawer test
Testing: posterior talofibular lig or calcaneofibular lig
Procedure: supports the tibia from posteriorly with one hand while grasping the midfoot with the other. The examiner then moves the foot posteriorly at the ankle joint while continuing to hold the tibia with the other hand. If there is an injury to the posterior talofibular or calcaneofibular ligaments, the talus moves posteriorly and rotates medially.
+ test: talus moving posteriorly and rotating medially on the injured side (more-so than the other ankle).
Talar tilt test
Testing: calcaneofibular and ATFL tears
Procedure: patient lies supine or sits with legs over the edge of the examination table. The examiner holds the calcaneus with one hand in order to bring the foot and ankle into the neutral position. The other hand grasps above the ankle to stabilize the lower leg. The thumb or the fingers palpate the calcaneofibular ligament. From this position and maximal dorsiflexion, the examiner inverts the foot at the ankle joint (hindfoot varus stress).
+ test: a visible and palpable angulation > 10 degrees.

Morton squeeze test
Testing: morton’s neuroma
Procedure: grasps the patient’s forefoot in a pincer grip and compresses it. This pushes the adjacent metatarsal heads against each other.
+ test: pain and occasional paresthesia between the metatarsal heads and toes.
Tinel’s sign (Ankle)
Testing: tarsal tunnel syndrome
Procedure: prone with the knee flexed 90°. The examiner taps the tibial nerve posterior to the medial malleolus with a reflex hammer.
+ test: reproduction of pain and paresthesia on the plantar aspect of the foot.
“too many toes” sign
Testing: pes planus
Procedure: pt standing, observe. Collapse of the medial arch causes the calcaneous to deviate toward the lateral side of the foot and a posterior view reveals more toes that normal on the affected side, indicating pes planus
+ test: too many toes visible
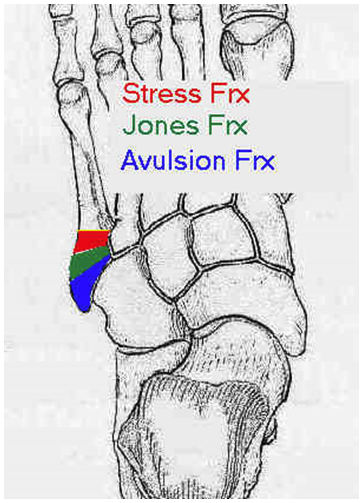
Ottawa Rules (Foot & Ankle) *****
X-ray is indicated when there is a history of trauma AND any one of the following:
Inability to bear weight both initially and in the ED
Tenderness over posterior 6 cm of medial or lateral malleolus
Tenderness at base of 5th metatarsal (avulsion fx, higher up = Jone’s fx concern)
Tenderness at navicular
This applies to those aged 3 - 55
Cuboid dysfunction
dx: everted cuboid (dropped cuboid)
May feel a firm protrusion on the plantar aspect of the foot.
May be very tender
Common in inversion ankle sprain.
Navicular dysfunction
dx: inverted navicular (dropped)
May feel a firm protrusion on the plantar aspect of the foot.
May be very tender
Common in inversion ankle sprain.
Anterior talus
aka: posterior tibia on talus
The talus glides anteriorly with plantar flexion of the foot.
If the talus is anterior, it will be difficult to dorsiflex the foot (restricted dorsiflexion)
Common in inversion ankle sprain.
Knee OA/DJD
wear & tear of articular cartilage, loss of joint space
meniscus tears
sx: pain @ joint line (med or lat)
causes: Weight bearing twisting injury in young. More fragile in older populations and less significant trauma can precipitate a tear.
meniscus tears research findings
No significant difference in functional outcomes between surgery or PT for partial meniscal tears.
In 2-year follow-up of patients with symptoms of a degenerative medial meniscus tear, the outcomes after partial meniscectomy were no better than those after placebo surgery.
Patellofemoral pain syndrome
F>M (b/c F have wider Q-angle), usually bilat., pain usually ant (on/under/around patella) and usually worse with stairs (esp descending), squatting, and prolonged sitting (theater sign)
“the low back pain of the knee” b/c so common and tx’s don’t work well, frustrating
Medial tibial stress syndrome (shin splints)
Inflammation of the muscles, tendons, and bone tissue around the tibia.
Usually occurs in runners or dancers after a sudden increase in exercise.
Pain typically occurs along the inner border of the tibia, where muscles attach to the bone.
ddx from stress fx? —> vibrations of bone would HURT and wouldn’t get better w/ rest
Chronic Exertional Compartment Syndrome
Majority of patient’s present with anterior and/or lateral compartment symptoms, mostly bilat
Transient pain which is brought on by exercise and relieved by rest.
Conservative tx: ice, NSAIDs, massage, shoe modifications, and gait mods.
Surgical release may be necessary in more severe cases.
would see increased opening pressure and diminished pulses
Pes anserine bursitis or tendonitis
Impossible to distinguish b/t the two.
Patients will complain of anteromedial knee pain below the joint line and, on physical examination, will be tender to palpation of the anteromedial tibia below the joint line.
Tx: ice, rest, NSAIDs, and PT
Unhappy triad = O’Donaghue triad
lateral blow to the knee dmg’s ACL, MCL, and medial meniscus
but recent studies say lat meniscus is more likely (know med menisc for boards tho)
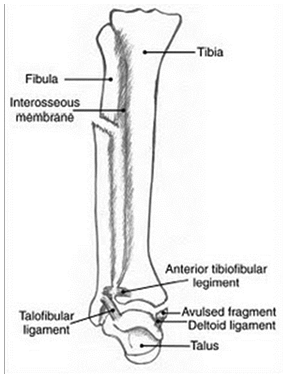
Maisonneuve Fx
MOI: External Rotation of ankle
Important: Palpate the proximal lower leg (fibular head), pt will NOT be able to wt bear
Maisonneuve Fracture – includes both of the following:
Fx at the fibular head
Syndesmotic injury - Tibiofibular clear space widened (>5mm)
Requires surgical fixation, 2 screws and a long leg cast, unlike simple syndesmotic fracture (just 1 screw)
Inversion ankle sprain
Foot is unstable during plantarflexion as talus glides anteriorly and the ankle becomes prone to inversion.
Structures of concern:
Anterior Talofibular Ligament (ATF)***
Calcaneofibular Ligament (CF)
Posterior Talofibular Ligament (PTF)
**Positive Ankle Drawer Tests or Talar Tilt Test
Basic ankle sprain grading
1st Degree Ligament Integrity is Intact
2nd Degree Partial Tear
3rd Degree Complete Ligamentous Rupture
Dysfunctions that are sometimes assoc. w/ inversion ankle sprains
Eversion of the calcaneus
Eversion of Cuboid
Inversion of Navicular
Posterolateral glide at talocalcaneal joint (posterior tibia, anterior talus)
Stretching and potential trigger point development in peroneus muscles
Distal fibula is drawn anteriorly with reciprocal posterior glide of fibular head
Tibia can externally rotate with anteromedial glide of tibial plateau
Plantar Fasciitis
usually >40yo, M>F
heel pain that is worse on first putting weight on the heel in the morning
bone spur/enthesiophyte at plantar calcaneus due to bone stress remodeling (Wolff’s law)
inflammed tendon —> increased Ca2+ deposits —> bone spur
Morton’s neruoma
“feel’s like a pebble”, worse in high heels or shoes w/ narrow toe box, usually 3-4th webspace or 2-3rd
high heels cause plantar flex, ext of phalanges @ metatarsophalangeal joints
Tarsal tunnel syndrome
compressed tibial N
pts w/ flat feet are prone
complain of pain and numbness on plantar aspects of feet
Jone’s fx
fx @ prox 5th metatarsal
Lisfranc Fx-dislocation
fx and dislocation of tarsometatarsal joints of foot
Car and motorcycle accidents are a common cause.
Pressure on a brake pedal with a plantarflexed foot can lead to the injury.
Three types
A: Total incongruity of TMT
B: Partial incongruity of TMT
C: Divergent (1st metatarsal move medial, 2nd-5th move lateral)
Talipes Equinovarus (clubfoot)
2 categories: idiopathic and those associated with congenital deformities.
Characterized by plantarflexion of the heel, varus and internal rotation of hindfoot and adduction of the forefoot.
Treatment usually consist of stretching and casting.
OMT may help isolated idiopathic type
Diagnosing Fibular Head
Grasp the fibular head between the 1st and 2nd digits of one hand
stabilize the leg with the other hand
Move the fibular head from anterolateral to posterior lateral.
If it is easier to move posteromedial it is called a posterior fibular head.
If it is easier to move anterolateral, it is called an anterior fibular head.
The tibiofibular joint is located on the posterolateral aspect of the the tibia. The fibular head glides from anterolateral to posterior medial.
Fibular head muscle energy
Anterior Fibular Head
Contact the anterolateral aspect of the fibular head with the thumb of the hand closest to the patient's knee.
The other hand internally rotates the patient's lower leg until the fibular head meets its posterior restrictive barrier.
The physician instructs the patient to externally rotate the lower leg as the physician applies an unyielding counterforce.
Posterior Fibular Head
Contact the posteromedial aspect of the fibular head with the MCP of the hand closest to the patient's knee.
The other hand externally rotates the patient's lower leg until the fibular head meets its anterior restrictive barrier.
The physician instructs the patient to internally rotate the lower leg as the physician applies an unyielding counterforce.
Diagnosing tibia
Monitor the tibial plateau and tibiofemoral joint space with the 1st and 2nd digits of one hand.
With the other hand, internally and externally rotate the leg.
If it is easier to move into internal rotation it is called an internally rotated tibia. The patient will usually have tenderness to the posterolateral aspect of the tibia.
If it is easier to move external rotation, it is called an externally rotated tibia. The patient will usually have tenderness to the anteromedial aspect of the tibia.
Distal Tibia Muscle Energy
Internally Rotated Tibia
Monitor the tibiofemoral joint with the hand closest to the patient's knee.
The other hand externally rotates the patient's lower leg until the tibia meets its externally rotated restrictive barrier.
The physician instructs the patient to internally rotate the lower leg as the physician applies an unyielding counterforce.
Externally Rotated Tibia
Monitor the tibiofemoral joint with the hand closest to the patient's knee.
The other internally rotates the patient's lower leg until the tibia meets its internally rotated restrictive barrier.
The physician instructs the patient to externally rotate the lower leg as the physician applies an unyielding counterforce.
Popliteus counterstrain (F IR)
Tender Point Location:
In the belly of the popliteus muscle just inferior to the popliteal space
Treatment position:
Patient prone with knee slightly flexed and leg internally rotated.

Tibiofemoral BLT
Cephalad hand palm down over the anterior distal femur and caudad hand palm down over the tibial tuberosity.
The physician leans down onto the patient's leg, directing a force toward the table.
The physician adds a compressive force in an attempt to approximate the femur and tibia.
The physician adds internal or external rotation to the tibia with the caudad hand to determine which is freer. The physician attempts to maintain this position.
Examples:
Internal rotation of tibia
External rotation of tibia
Articular and myofascial restrictions of tibiofemoral joint
Peroneus muscles (lat ankle) counterstrain
Tender Point Location:
Anterior and inferior to the lateral malleolus in the sinus tarsi (talocalcaneal sulcus). May also be found on the lateral surface of the leg below the fibular head in the peroneus longus, brevis, or tertius muscles
Treatment position:
Patient prone. foot eversion and external rotation. May need to add some plantar flexion.
Quadratus plantae counterstrain
Tender Point Location:
In the belly of the Quadratus Plantae muscle just anterior to the calcaneous
Treatment position:
Patient prone with knee slightly flexed and forefoot on thigh and marked flexion of the forefoot through a compressive on the calcaneous.
Anterior talus HVLA
The patient lies supine, and the physician stands at the foot of the table.
The physician's hands are wrapped around the foot with the fingers interlaced on the dorsum.
The foot is dorsiflexed to the motion barrier using pressure from the physician's thumbs on the ball of the foot.
Traction is placed on the leg at the same time dorsiflexion of the foot is increased.
The physician delivers a tractional thrust foot while increasing the degree of dorsiflexion.
Effectiveness of the technique is determined by reassessing the ankle range of motion.
Tarsal/metatarsal dysfunction BLT
Patient lies supine, and the physician stands or is seated at the foot of the table.
Physician grasps the foot with both hands, the fingers on the plantar aspect of the distal metatarsals and the thumbs on the dorsal aspect of the foot.
Physician flexes the distal forefoot slightly by contracting the fingers on the plantar aspect of the foot.
The physician then presses the thumbs downward into the metatarsals toward the table.
Physician attempts to position the foot at a point of balanced tension.

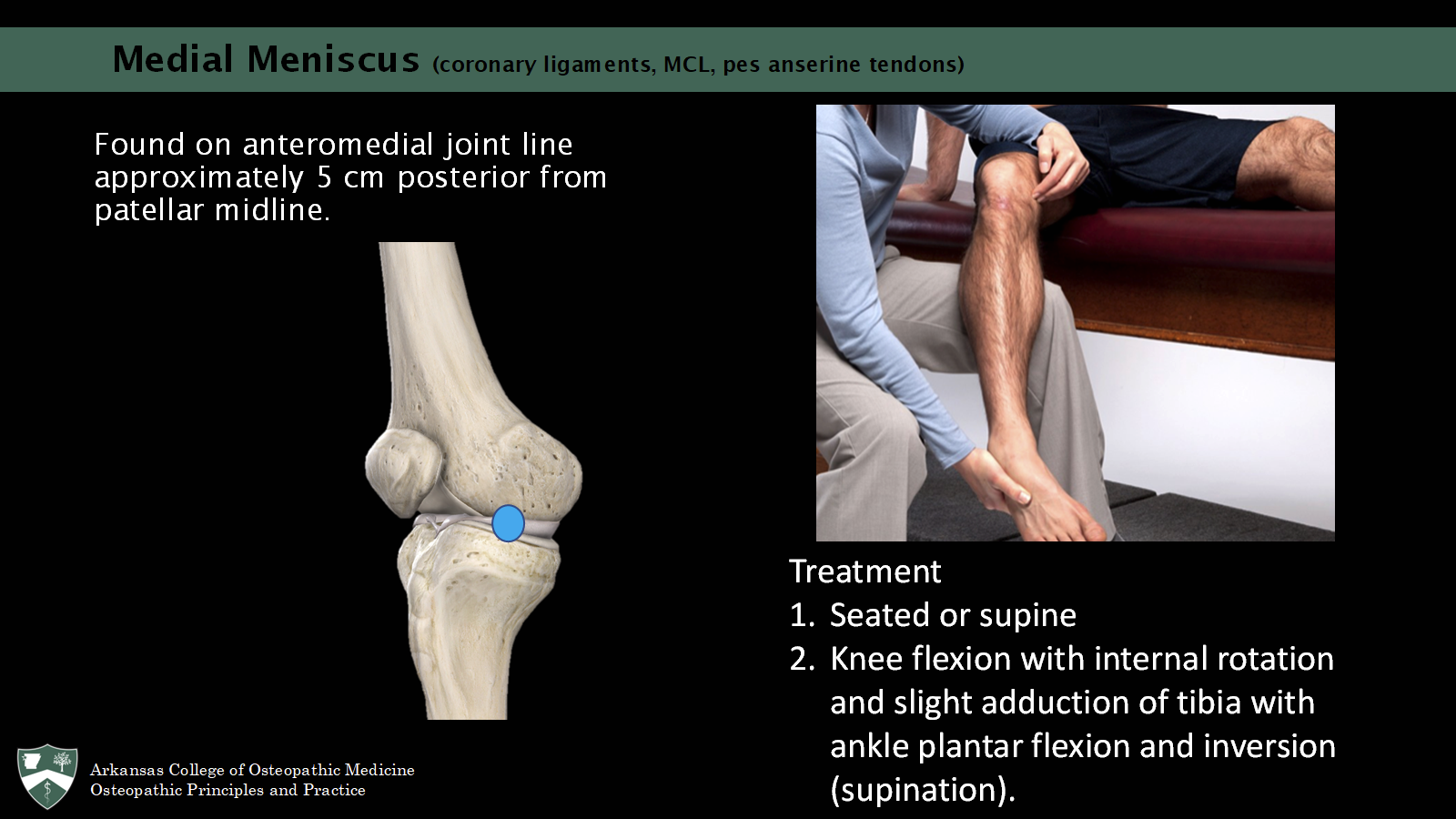
Medial meniscus counterstrain (coronary ligaments, MCL, pes ansersine tendons)
Found on anteromedial joint line approximately 5 cm posterior from patellar midline.
Seated or supine
Knee flexion with internal rotation and slight adduction of tibia with ankle plantar flexion and inversion (supination).
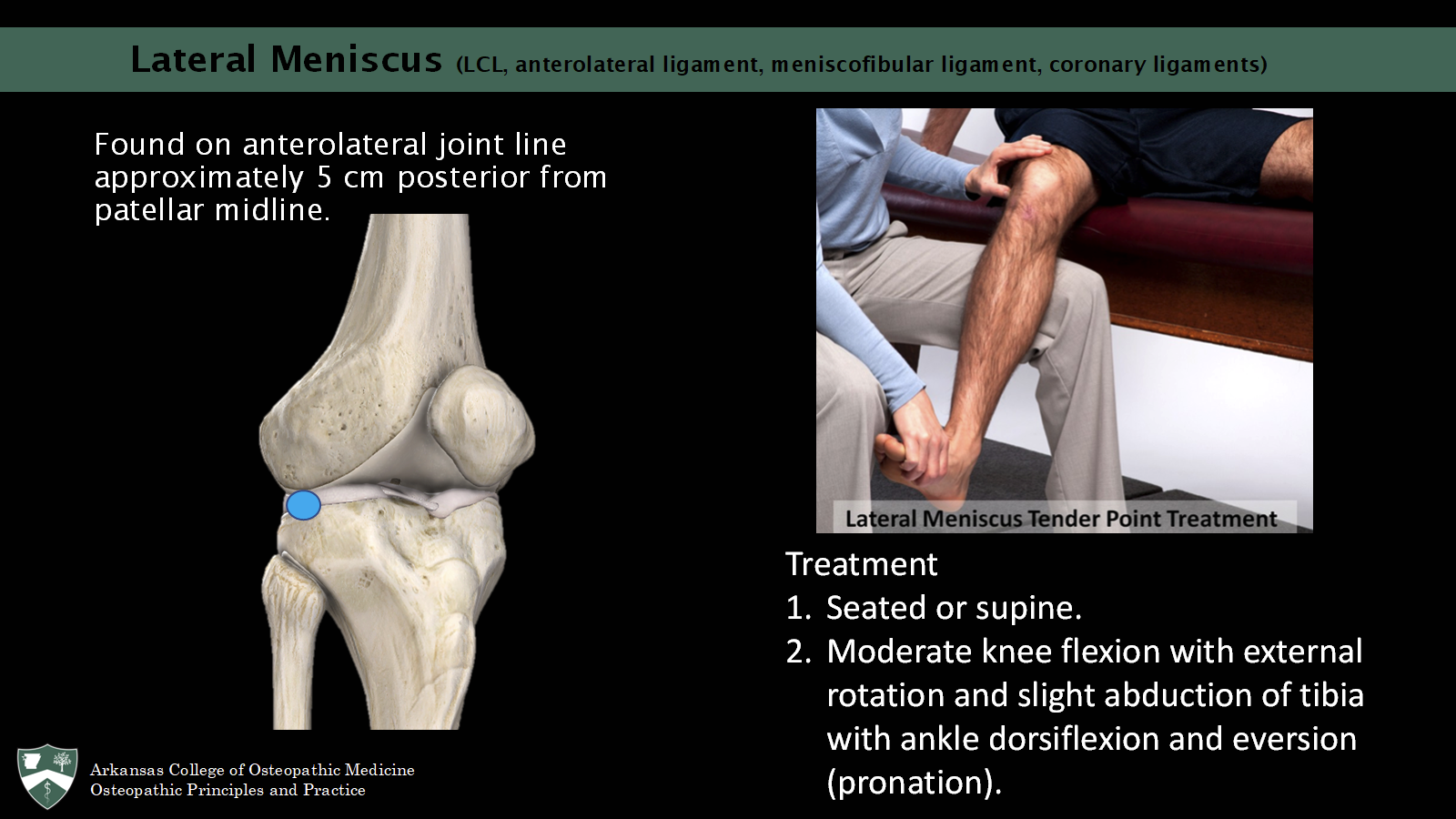
Lateral meniscus counterstrain (LCL, meniscofibular lig, coronary ligs)
Found on anterolateral joint line approximately 5 cm posterior from patellar midline.
Seated or supine.
Moderate knee flexion with external rotation and slight abduction of tibia with ankle dorsiflexion and eversion (pronation).
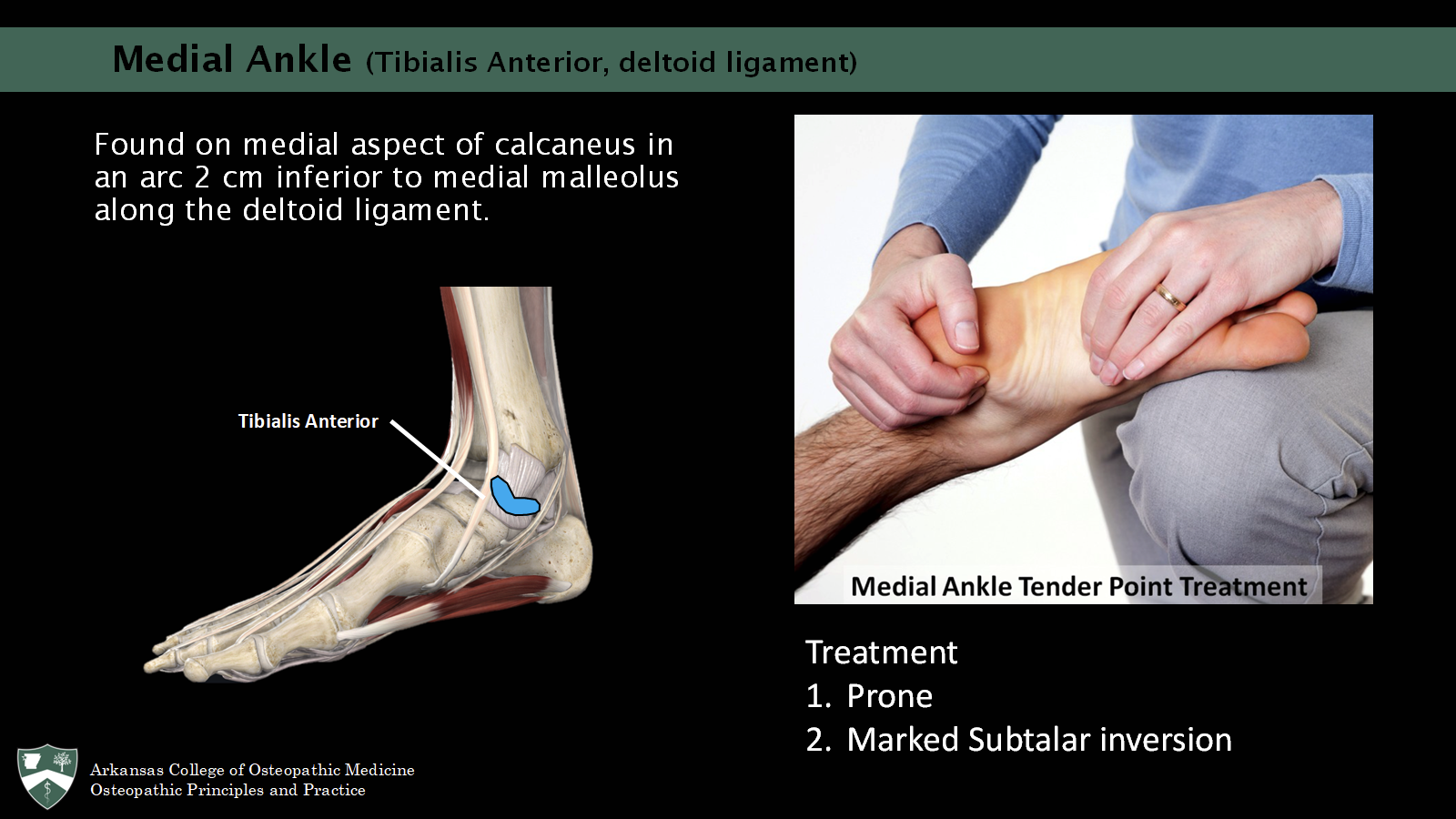
Medial ankle counterstrain (tibialis anterior, deltoid ligaments)
Found on medial aspect of calcaneus in an arc 2 cm inferior to medial malleolus along the deltoid ligament.
tx: prone, marked subtalar inversion
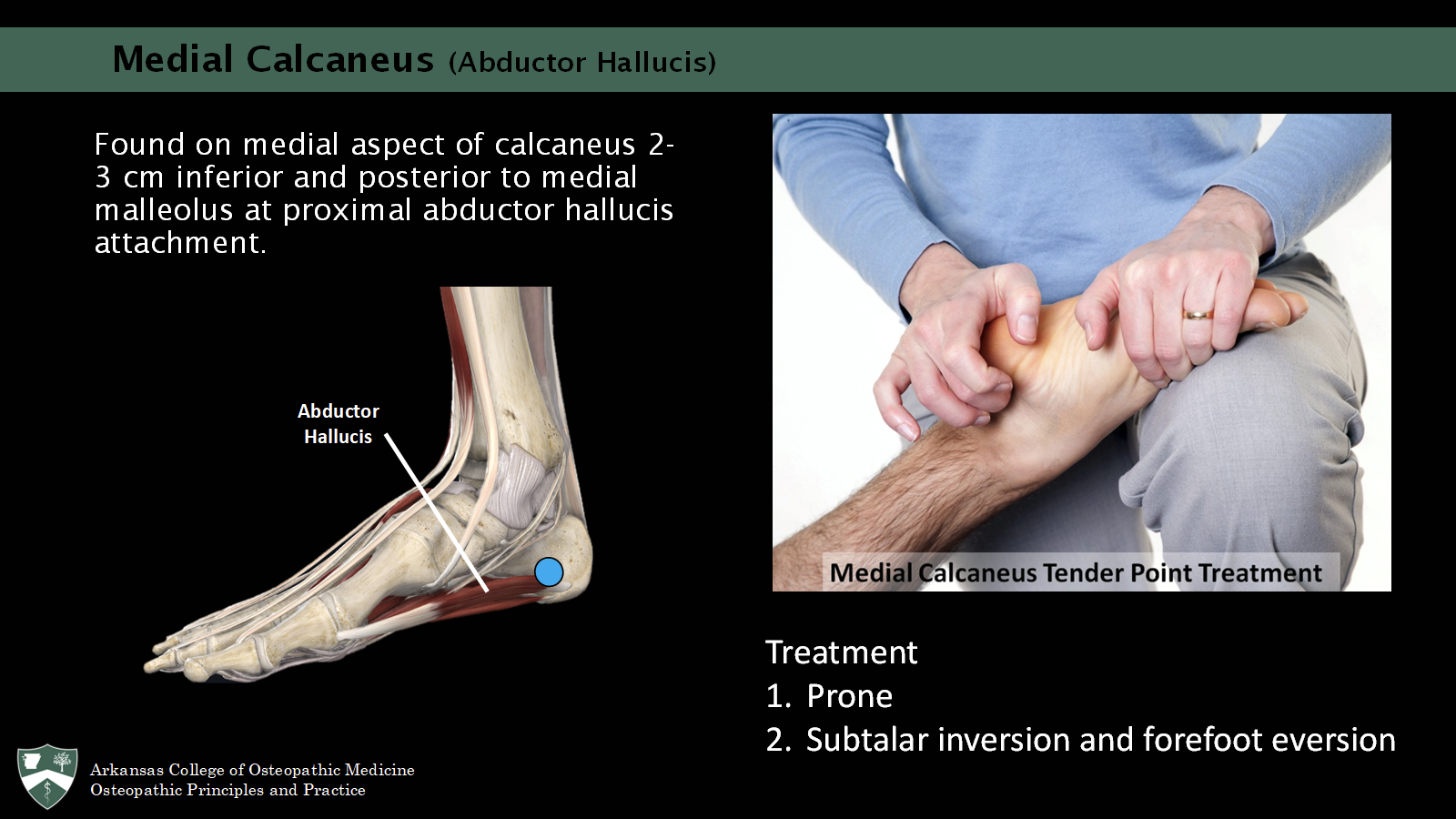
Medial calcaneus counterstrain (abductor hallucis)
Found on medial aspect of calcaneus 2-3 cm inferior and posterior to medial malleolus at proximal abductor hallucis attachment.
tx: prone, subtalar inversion and forefoot eversion
BLT principles (indirect)
Disengagement of the dysfunctional area - compression/decompression
Exaggeration of the dysfunctional pattern - returning to the position of injury or ease
Balanced tension of ligaments - maintained until release
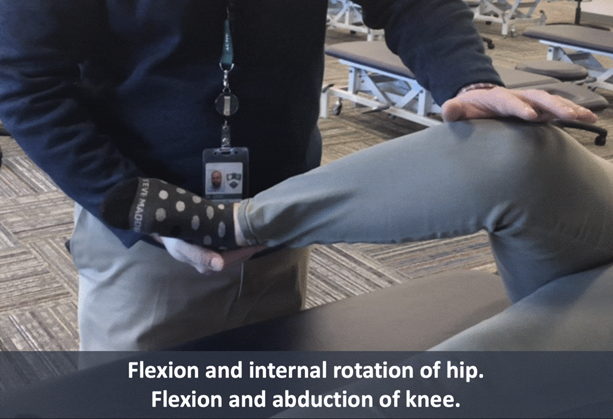
BLT for knee collateral ligs and tibiofemoral joint
With hip and knee flexed, internally rotate hip and apply a gentle valgus force to knee (LCL) with one hand and use the other to apply a counterforce.
While maintaining the gentle force, slowly return the leg to neutral.
When the motion becomes sluggish or interrupted, pause for 3-5 seconds.
Repeat steps 2 and 3 until the leg is fully in its neutral position on the table.
Repeat with externally rotated hip and a varus force on the knee (MCL).
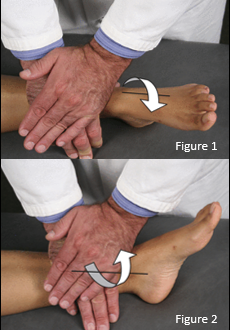
BLT for anterior talus tibiotalar dysfunction
The patient supine with the heel of the foot on the table.
The physician places the proximal hand palm down across the distal tibia with the metacarpal-phalangeal joint of the index finger proximal to the distal tibia.
The physician presses directly down toward the table and balances the tension coming up through the heel and the tibiotalar joint.
The physician's other hand can be placed on top of the treating hand to create more pressure. The physician internally rotates (Fig. 1) or externally rotates (Fig. 2) the tibia slightly to bring the compression to a point of balanced tension.
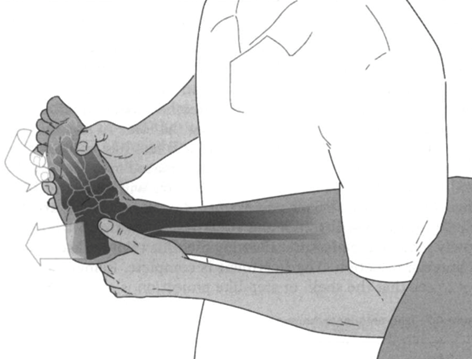
BLT for foot/ankle dysfunction (Boot-Jack)
Patient supine, the physician stands facing the foot of the table.
Patient’s leg is placed under the physician's axilla.
Physician grasps the calcaneus with the thumb and index finger.
Physician flexes the patient's hip and knee approximately 90 degrees and gently externally rotates and abducts the patient's femur.
Physician's elbow touches the patient's femur just above the popliteal fossa as a fulcrum to generate proximal pressure.
Physician leans back, carrying the patient's hip and knee into further flexion while maintaining tight control of the patient's calcaneus. This exerts a distraction effect on the calcaneus from the talus.
Physician induces slight plantar flexion to a point of balanced tension in the metatarsals and tarsals of the patient's foot.