SAS: Exam 2
1/38
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Respiratory Surgical Considerations
Pre op: Min restraint, ± cooling, rapid ET intubation
Rx: Oxygen, butorphanol, acepromazine
Extreme anesthetic risk
Risk: High risk, induction + recovery, examine upper airway at induction

Respiratory surgical procedures
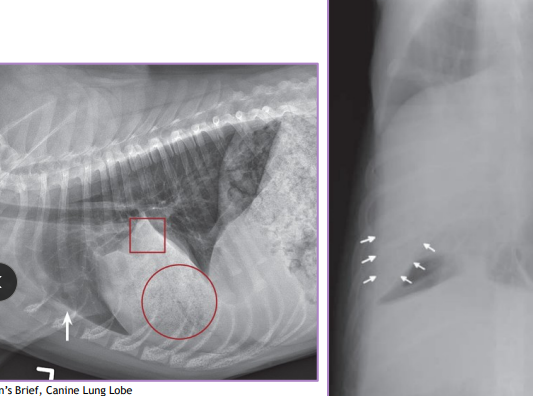
Normal lung volume: R → 58%, L → 42%
Partial Lung Lobectomy: SM Focal lesion at peripheral ½ to 2/3 of lung lobe : neoplasia, granuloma, bulla, biopsy
Dogs can tolerate removal up to 58% (compensate with hyperinflation, alveolar enlargement, capillary thinning)
Intercostal thoracotomy, remove with a normal margin
Complete Lung Lobectomy: (LG) abscess (large purulent), trauma, torsion, large/multifocal neoplasia/bulla, idiopathic
Right cranial and middle are most common
Intercostal thoracotomy or median sternotomy
Remove lung at pedicle and ligate artery/bronchus/vein
DO NOT untwist before removing
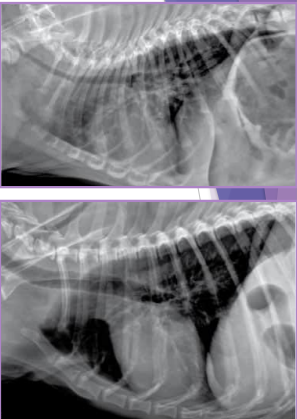
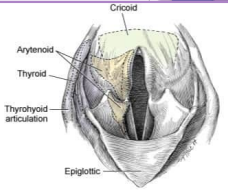
Brachycephalic Obstructive Airway Syndrome (BOAS)
Et: compressed face, stenotic nares, elongated soft palate, everted saccules ( → Laryngeal collapse), hypoplastic trachea
Sig: young, brachycephalic breeds
Cs: stertor(low), stridor(high), gagging, coughing, exercise intolerance, collapse, dyspnea
Dt: CBC/Chem, rads, airway exam under single anesthetic episode
Tx:
Stenotic Nares: Cartilage resection/anastomosis or amputation
Elongated Soft Palate: staphylectomy/palatoplasty
1-3mm beyond epiglottis - needs to be cut @ tonsil level, watch for laryngeal edema
Everted Laryngeal Saccules: temporary extubation, resection, bleeding stops w/ ET tube
Prolapse of mucosa lining, inhibit airflow
1st stage of laryngeal collapse
Hypoplastic Trachea: none
Tracheal diameter : thoracic inlet <0.2
Laryngeal Collapse: laryngectomy or permanent tracheostomy

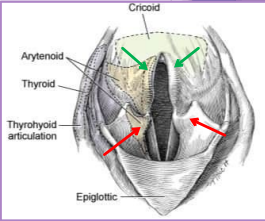
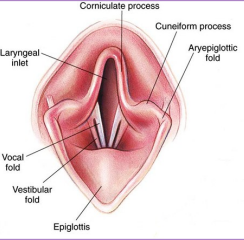
Laryngeal collapse
Due to chronic upper airway obstruction/airway resistance
3 stages
I – everted laryngeal saccules
II – I + collapsed cunieform cartilages (red)
III – I + II + collapsed corniculate cartilages (green)
TX: Laryngectomy, Permanent tracheostomy
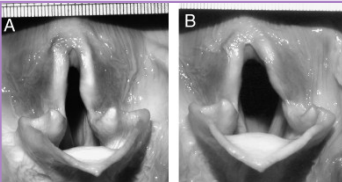
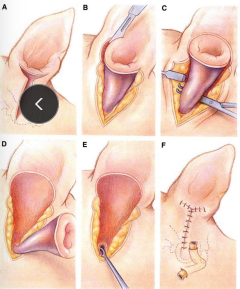
Laryngeal Paralysis
Et: arytenoid cartilages fail to abduct (recurrent laryngeal n. & Cricoarytenoideus dorsalis muscle)
Congenital, idiopathic, trauma, systemic dz, iatrogenic
Sig: Lg breeds - unilateral then progresses to bilateral
Cs: progressive signs, inspiratory stridor, voice change, exercise intolerance, cough/gag, anxiety, collapse
Dt: BW, Rads, neuro exam, laryngeal exam under light anesthesia(ready to do sx)
Abduction of arytenoids and vocal folds on inspiration
Tx: unilateral arytenoid lateralization (reduce obx and resistance) tie back
Prognosis is good, life-long aspiration risk, heat intolerance, Progression of polyneuropathy – if GOLPP is present
Lung Lobe Torsion
Et: chronic resp dx, chylothorax, trauma, thoracic Sx, neoplasia, idiopathic
Sig: deep, narrow chest dogs - pugs
Cs: right cranial & middle congestion & consolidation - most common
Tx: complete lobectomy
DO NOT untwist lobe
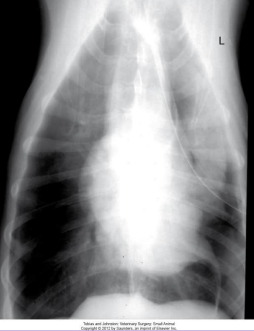

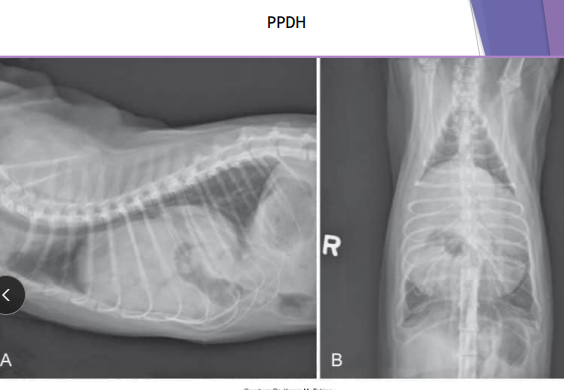
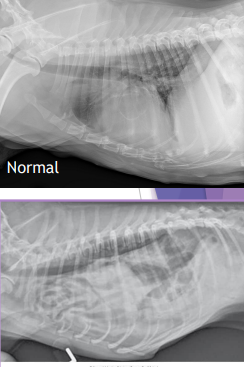
Diaphragmatic Hernia
Et: trauma, pressure gradient disruption, genetic
abdominal organs migrate into thorax, liver is #1
Peritoneopericardial d. hernia (PPDH) → congenital
Sig: Cocker spaniel, Weimaraner, Himalayan, DLH
Cs: shock(acute), dyspnea(chronic), exercise intolerance, ADR
Congenital is asymptomatic
Tears → weakest areas: muscle
Dt: thoracic rads (#1), US, CT
Tx: Sx (8-16w if congenital) (trauma: be ready for anything)
abdominal explore, identify hernia, reduce contents, close defect (absorbable 3-0 PDS, simple continuous, dorsal → ventral), remove air
Caution of adhesions
Do not close the pericardial sac (genetic)
Risk: re-expansion pulmonary edema, abdominal compartment syndrome, ARDS
Do NOT manually re-expand lungs, do not close pericardial sac
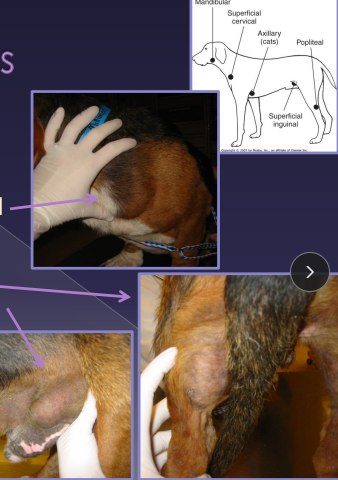
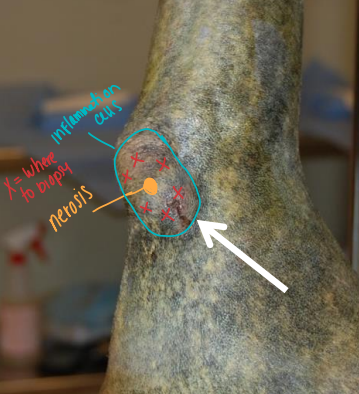
Lymphadenomegaly
Palpable - when enlarged
Maxillary, Accessory axillary, Cervical, Femoral, Retropharyngeal, Sublumbar (L7), Mesenteric
Et: infection, inflam, neoplasia, systemic dx
Size does not correlate with disease
Cs:
Painful: suppurative lymphadenitis → infection
Non-painful: lymphoid neoplasia
Fixed: metastatic neoplasia, fungal
Normal Palpable: Mandibular, superficial cervical, axillary (C), popliteal, superficial inguinal, tonsils (visible)
Abnormal if Palpable: Maxillary, accessory axillary, cervical, femoral, retropharyngeal, sublumbar, mesenteric
Lymph Node Surgical Procedures
#1 FNA!!: bacti, fungal, neoplasia, culture, staging, tx planning
screening tool, cellular only, specific but not sensitive
Needle (Tru-Cut) biopsy: Lg accessible LN
Lg bore (14-16g), aseptic, core sample (small)
Only be done in areas that allow it - no important organs/BV near
Incisional (wedge/removal) Biopsy: small LN, tricky location
Stabilize node, wedge excision, close capsule(H. mattress)
Lymphadenectomy Excisional (LN removal): smaller node, evaluate for metastasis - does not prevent mets
Full dissection, ligate vessels
Sample Preservation: Neoplasia (formalin fixed), Bacti (fresh), Fungal (fresh/frozen), impression smears - cytology

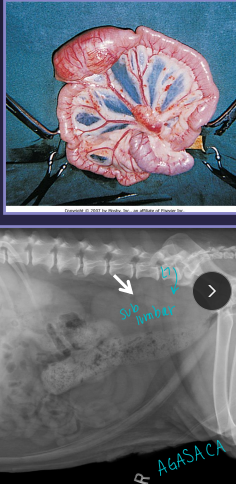
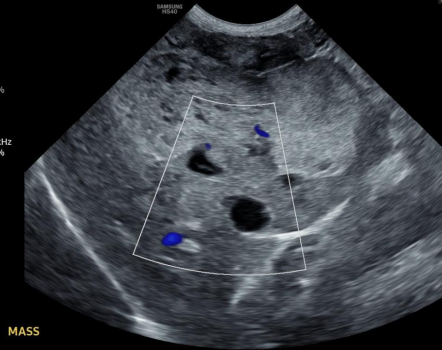
Splenomegaly
Anatomy:
Gastrosplenic ligament - left side
Celiac artery → Splenic artery → pancreas → Left gastroepiploic a. → Short gastric aa
Diffuse: Congestion
Splenic torsion, RHF, GDV, drugs, infection, Immune mediated, lymphoma
Focal: Nodular regen, hematoma, trauma, neoplasia
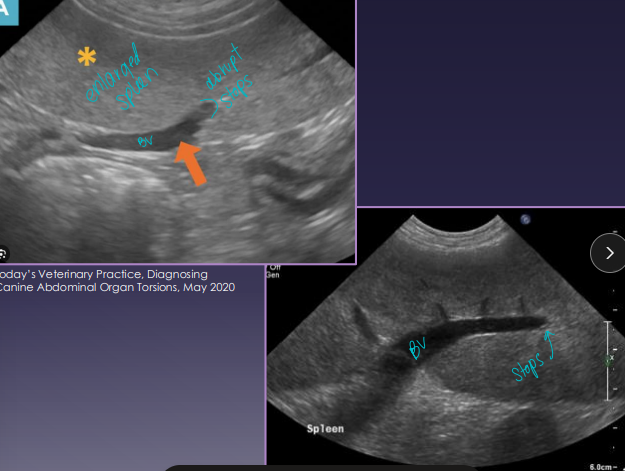
Splenic Torsion “acute abdomen”
Et: spleen twists on pedicle, congestion, necrosis
splenic artery and vein
Sig: Lg-breed dogs
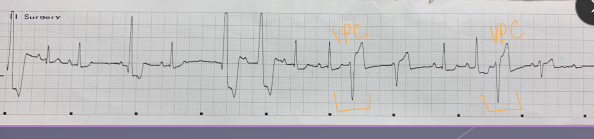
Cs: shock(acute), anorexia, V/D, pain, enlarged spleen, hemoglobinuria(chronic), VPCs
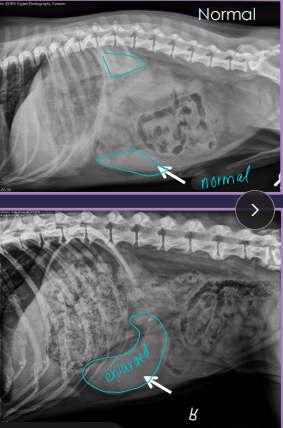
Dt:
Rads: abnormal location, mass effect, gas bubbles, comma-shaped spleen
US: variable echotexture, dilated vessels, thrombi
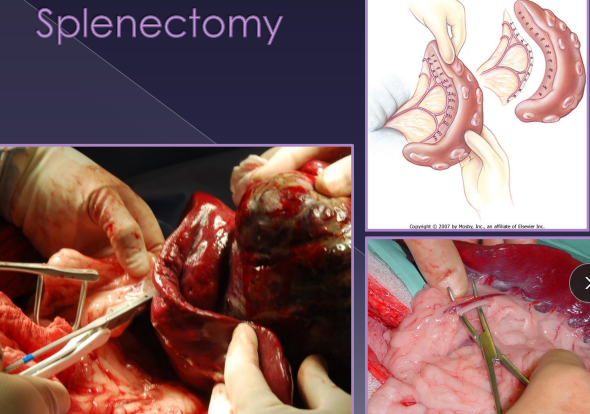
Tx: splenectomy DO NOT untwist, Unasyn
necrotic debris → emboli risk

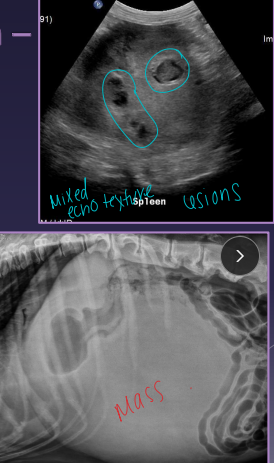
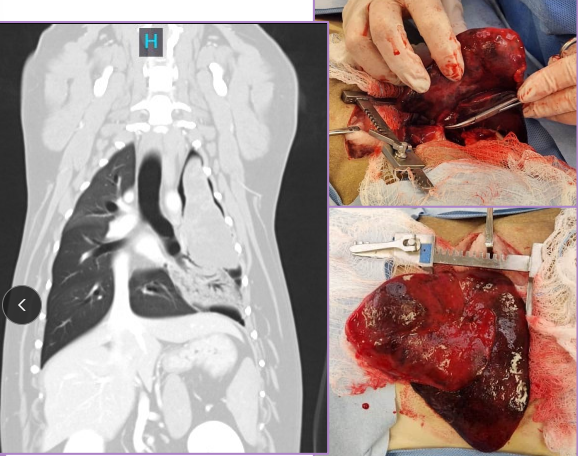
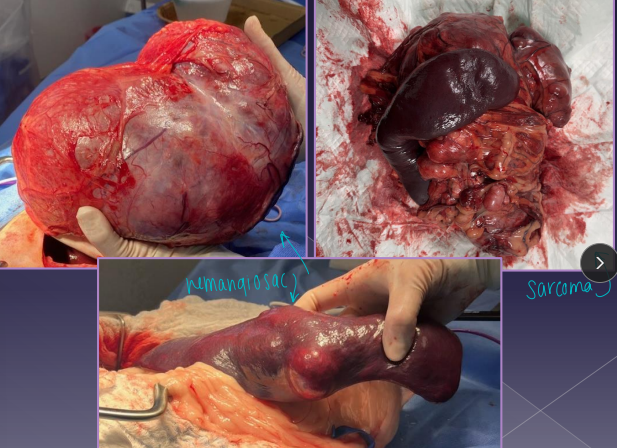
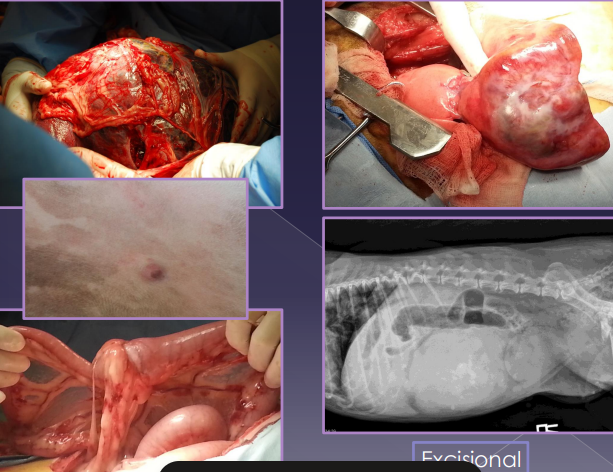
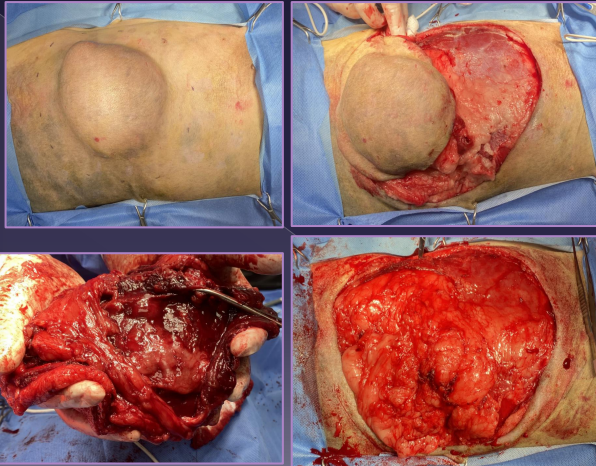
Splenic Neoplasia
Et: VERY common!
Non-neoplastic: hematoma, lipoma, myelolipoma
Benign: hemangioma, fibroma
Malignant: hemangiosarcoma HSA (#1), fibrosarcoma, liposarcoma, MCT
Sig: Lg-breed dogs
Cs: shock, mass, enlarged abdomen, fluid wave, lethargy, pain, vomiting, PCV on free fluid - determine blood, VPCs
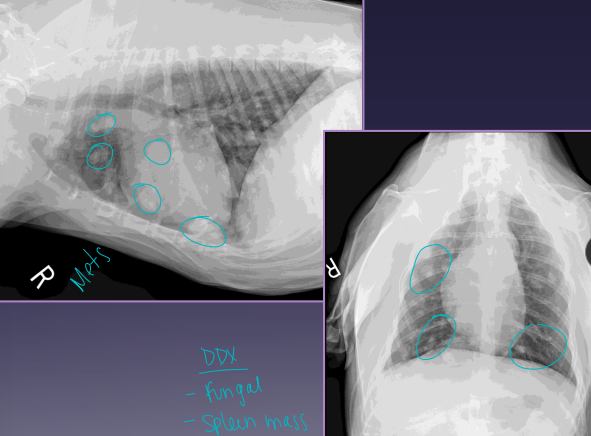
Dt: Abd rads (mass effect, effusion, metastasis), US (mixed echotexture, cavitated lesions, enlarged spleen), biopsy
Xray chest for mets!
Tx: splenectomy
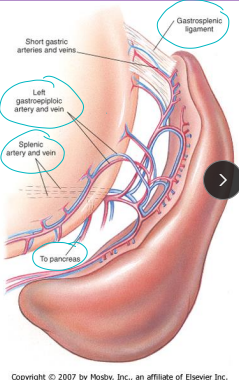
Splenic Surgical Procedures
FNA: percutaneous, cheap, easy
concern for diffuse dz, avoid cavitary lesions
Ddx: infection, mast cell, lymphoma
non-diagnostic for neoplastic masses (blood back)
Excisional Biopsy: diffuse dx, small/focal mass, culture, histopath
Sx incision → sample → capsule sutured closed, direct pressure hemostasis
NOT really done, just remove the entire thing at once
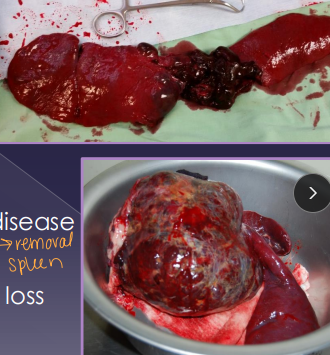
Splenectomy: Neoplasia, trauma, IM dz
Classic: dissect & ligate/divide all hilar vessels; protect short gastric a.
Alternate: Abdominal exploration, isolate, ligate splenic a. & v. distal to pancreatic branch/short gastric aa. / L gastroepiploic
quicker, best for no adhesions
Complications:
Hemorrhage
Resist this temptation to break down adhesions
Operative Considerations for the Spleen
Rx: Blood transfusion(depends), Oxygen(natural anti-arrhythmic), fluids → Crystalloid/colloid fluid support
Monitor: ECG: ventricular arrhythmias (ECG), coagulation (PT/PTT)
Patient Assessment - oncology
History
Visual inspection
Mass palpation
Evaluate:
Gross appearance
Consistency
Size
Mobility
Palpation of regional lymph nodes
Secondary effects of a tumor present
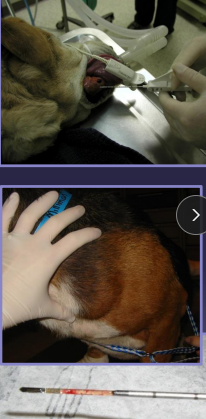
Fine Needle Aspiration - Oncology
Cytological evaluation - Cells
Definitive diagnosis:
AGASCA
Lymphoma
Melanoma
Mast cell tumor
Supportive information
Biopsy - Oncology
Obtain a diagnosis → skip FNA (Oral, airway)
Need to know tumor behavior
› Degree of local invasion
› Metastatic potential - tumor grade (high/low)(1-4)
› Biologic activity - histamine release
Pre- or postoperative
Pre: helps plan surgery
Post: obtain clean margins
Never for TCC, intestinal cancer → remove mass fully then biopsy
Biopsy procedure - oncology
Incisional/TruCut: Removal of part of the tumor
Requires a second surgery, seeding
Fixed masses

Excisional: Remove entire tumor with normal tissue
a single procedure
Small, movable skin masses
Internal organs: intestines, spleen, liver
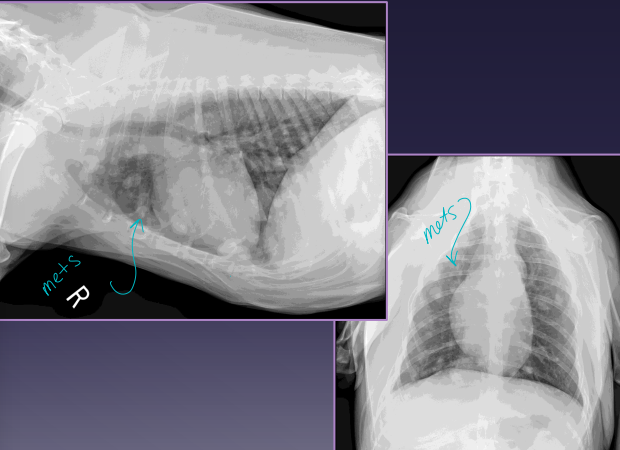
Tumor Staging
Diagnostic process
evaluate for progression/extent of disease
BW, UA, Bio chem
Xray → 3 views
US - abdomen
LN aspiration
Enlarged nodes
Draining/sentinel LN (popliteal drains the foot)
MRI, CT
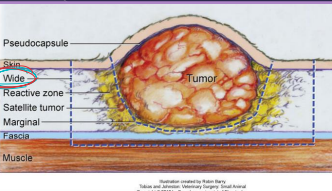
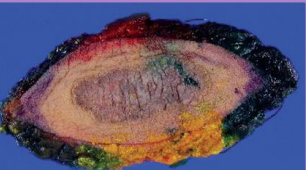
Surgical Principles - oncology
1 and done
Excise all neoplastic tissue
Aggressiveness (surgical ‘dose’) - common to leave some
› Intralesional (debulking) - leave some behind (airway)
› Marginal - edge, peripheral to pseudocapsule, Lipoma, common w/o biopsy
› Wide - clean margins
Solid masses, 1-2 facial planes deep, margin of normal tissue excised
› Radical - amputation, entire tissue
splenectomy, mammary chain
better to leave a wound open … than tumor cells remaining
Resection: “dirty” margins
Have to go Deep and lateral

Surgical technique - oncology
Sharp dissection → scalpel blade is best
Gentle tissue handling
Hemostasis
Prevent release of tumor emboli → ligate vein 1st
Minimal handling of tumor itself
Use appropriate suture → monofilament (PDS)
Lavage, Avoid drain
Change instruments, gloves, drapes for closure
limit contamination / seeding
Post removal biopsy!!!
Allows for margin assessment
Dictates adjunctive treatment plan
radiation, chemo, 2nd sx
Lymph Nodes
Palpate regional lymph nodes
› Enlargement
› Symmetry
› Degree of fixation
Size does not indicate metastasis!!!
Biopsy: if Tx dictates or concerned about mets!
Lymph nodes are a poor barrier to disease
Palliative Therapy / Surgery
cancer is not curable
Improve quality of life
Examples:
Upper airway obstruction
Non-resectable mass
Bone tumor, amputation not possible
Hemoabdomen
Debulking → Rarely acceptable
Follow up w/ radiation
Vascular access points → chemo
Feeding tubes
Pain management
Prophylactic Surgery
Ovariectomy/ovariohysterectomy “spay”
› Mammary neoplasia
› Ovarian/uterine neoplasia
Orchidectomy “neuter”
› Testicular neoplasia
› Perianal neoplasia
› Prostatic neoplasia
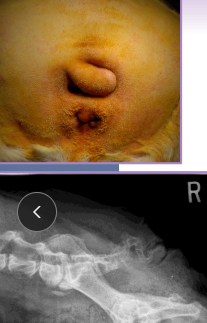
Rectal polyp
Often transform into malignancy
CNS Surgical Considerations
relies on oxygen and glucose!!
BP: blood flow constant if MAP = 50–160 mmHg in CNS
Trauma ↑ ICP → ↓ local blood flow
Metabolic: blood flow adjusts to metabolic demand - local blood flow will decrease w/ trauma
Sensitive to PaCO₂: ↑ CO₂ → vasodilation → ↑ ICP
hypoventilation, Increases blood flow
Remember: anesthesia, trauma
Cs: hemorrhage (1), edema (1), demyelination (2), necrosis (2), inflam (2)
Spine: paraspinal pain/defect, limb neuro deficits
Head: anisocoria, abnormal pupils, nystagmus, mentation change, bleeding (nose/ear/eye), Cushing response, herniation
Tx: only do diagnostics once stable → Xray/CT/MRI
Rx: Head elevated, fluids, oxygen, opioids, Mannitol (x3), Dexamethasone (once), neck brace
Sx: subdural hematoma, depressed skull fx, spinal stabilization
Craniectomy: ↓ ICP 15%
Durotomy: ↓ ICP 65%
Prog: deep pain nociception caudal to lesion is good
guarded when DPS absent
Schiff-Sherrington: T13-L1 stiff front, floppy back
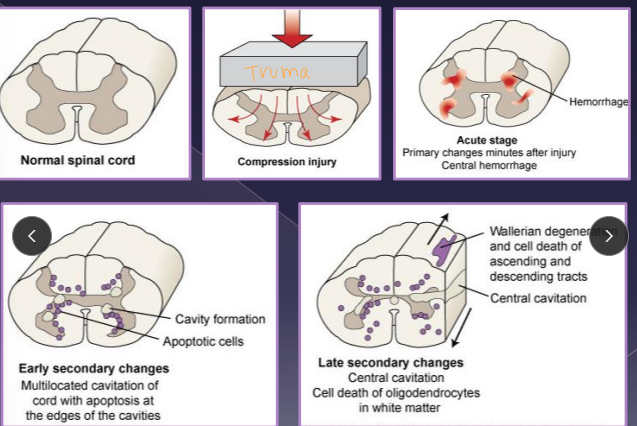
Mechanisms of Trauma
1º damage
› Mechanical trauma
› Axonal injury
› Hemorrhage
› Edema
2º biochemical effects
› Demyelination
› Neuronal and glial cell necrosis
› Inflammatory response
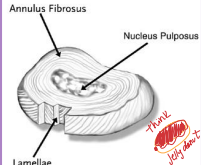
Anatomy of the disk (IVDD)
Shock absorption and distribution
Annulus fibrosus
Parallel arrangement of lamellae
Thicker ventrally
Nucleus pulposus: Center
Cartilagenous vertebral end plates
Source of nutrients via diffusion
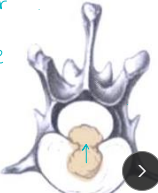
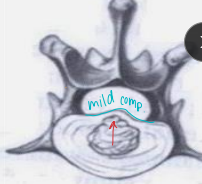
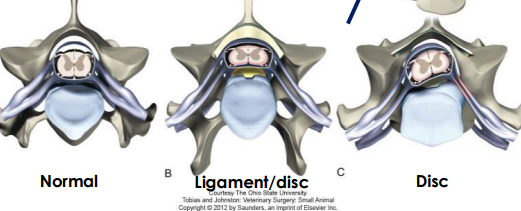
Intervertebral Disk Disease
Herniation (Hansen Type I) Acute → fast progressive
Et: chondroid metaplasia, increased intradisc pressure
Sig: chondrodystrophics, 3-5y (TL) T10/11-L6/7 ¾ dogs
8-12y C2/3-C5/6 (Cervical) ¼ dogs
Cs: Compressive myelopathy, Contusion injury
paraspinal hyperesthesia, hunched back, vocalization(cervical), forelimb lameness, ataxia/paresis, plegia

Dt: CT/MRI (#1), Rads(r/o) (narrowing, wedging, mineralized disc in SITU)
Tx: percutaneous laser disc ablation(prevent T10/11-L5/6), >4w rest, NSAID, gabapentin, amantadine, ventral slot Sx (C), Hemilaminectomy (TL)
Reoccurrence: 15-20%, increased w/ >5 mineral disks
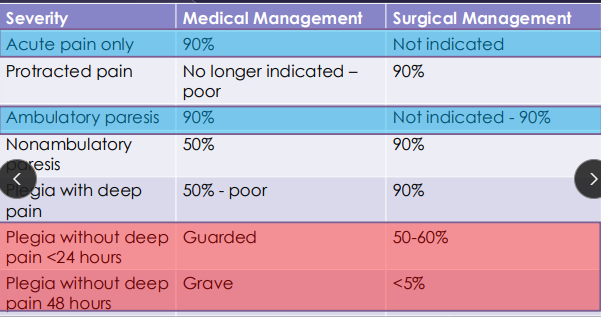
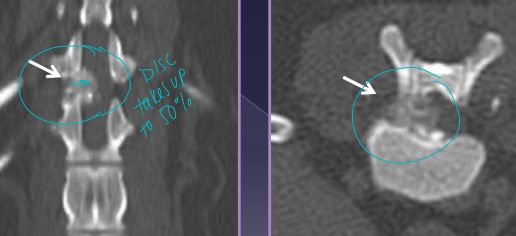
Protrusion (Hansen Type II) Chronic → slow progressive
Et: fibroid metaplasia, dorsal annulus weakens, nucleus bulges, TL > cervical
Sig: Lg, non-chondrodystrophic, 5-12y older dogs
Cs: slow progressive ataxia, pain at lesion, paresis
Dt: MRI
Tx: Medical(best): NSAID, gabapentin, SX: dorsal laminectomy → decompression #1 goal

Percutaneous laser disk ablation (PLDA)
Why: IVD herniation, reduce risk of recurrence
How:
Approach to remove (ablate) the nucleus pulposus
Performed from T10-11 thru L5-6

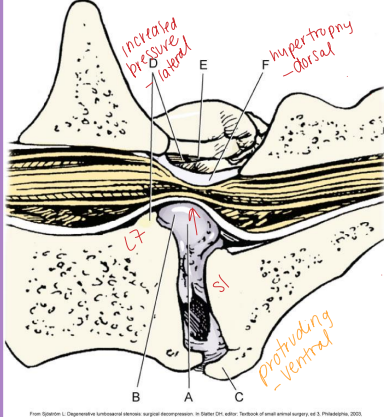
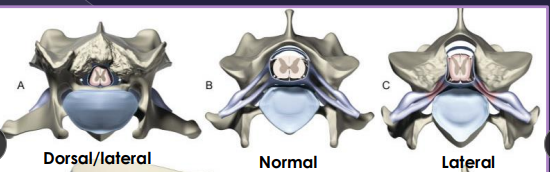
Lumbosacral Disease (Cauda Equina Syndrome)
Et: L7-S1/3 → spinal cord stops @ L5-6
Degenerative: disc protrusion, lig hypertrophy, facet hypertrophy, spondylosis, instability
Congenital: stenosis, malformation, transitional vertebrae, end plate OC
Sig: Lg, middle-aged, working dogs, GSD
Cs: reluctance to jump, stiff gait, low tail, incontinence, back pain, weakness(non-weight bearing), LMN signs(L4-3)
Patellar “pseudohyperreflexia” – exaggerated reflex
Sciatic affected, patellar reflex spared
Dt: rads (spondylosis, narrowed disc), CT, MRI(best)
Tx: NSAID, gabapentin, 4-6w rest, epidural steroids (MPA protocol: wk 0, 2, 6)
SX: laminectomy + discectomy = reoccurrence 1-2y esp. w/ lateral compression

Cervical Spondylomyelopathy (Wobbler Syndrome)
Et: cervical vertebral instability/malformation, cord/nerve root compression, disk protrusion → C5/6-C6/7
Sig:
Disc-associated: middle-aged Lg breeds Dobermans; C6-C7 IVD protrusion(ventral); 50:50 single/multi
Ligamentum flavum hypertrophy (dorsal)
Osseous-associated: young giant breeds, Danes; C6-7 Vertebral stenosis; multi sites 80%
Cs: chronic progressive ataxia, neck pain, proprioceptive deficits, Proliferation of the vertebral arch
Dt: Rads(r/o), CT(bone), MRI(both) site/severity/parenchymal assessment (#1)
Tx: Mild cases: restriction, harness, NSAID, gabapentin, good footing
Surgical(static): direct decompression (ventral slot, dorsal laminectomy), distraction/stabilization w/ spacers/implants(dynamic)
domino effect deterioration → adjacent VB effected
Both Sx and Rx equally successful
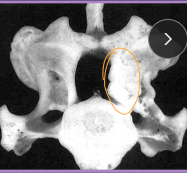

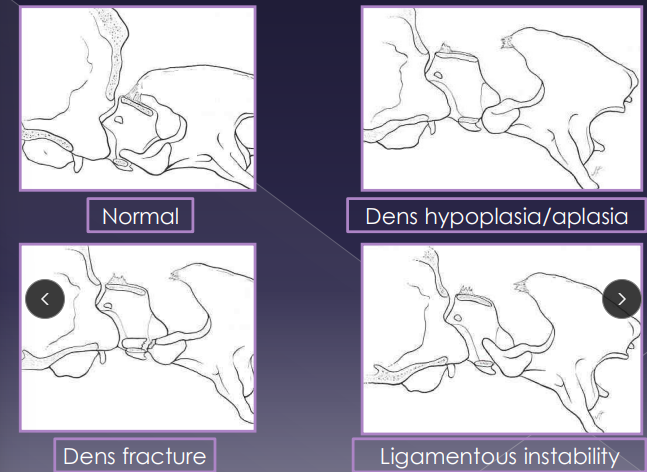
Atlantoaxial Instability (AA)
C1-C2
Et: congenital, dens aplasia, dens hypoplasia, dorsal angulation, ligament laxity, trauma
cranial axis(C2) dorsal displacement in relation to C1, cord compression
Sig: young, sm breeds
Cs: neck pain(30-60%), progressive tetraparesis, ataxia, neuro defects(94%)
Dt: rads (C1-2 misalignment), CT/MRI
do NOT flex neck!!
Tx: 6-8w rest, neck brace, NSAID, gabapentin, Sx A-A fusion (#1)
Moderate peri-op mortality
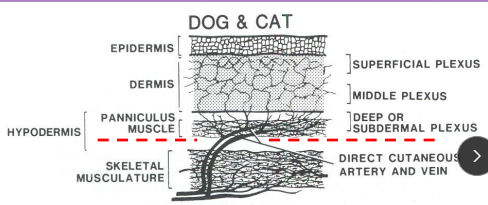
Surgical Considerations for the skin
Sharp dissection
Trauma: Dissect deep to subdermal plexus to prevent devascularization
Scalpel < scissors < CO₂ laser < electroscalpel
Skin hooks/suture stays < tissue forceps/repeated manipulation
Healing:
Primary: immediate closure
Delayed primary: <3-5d, before granulation
Secondary: >3-5 days, after granulation
Second intention: granulation + epithelialization
Tension:
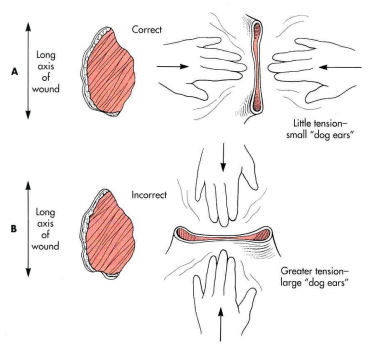
Close parallel to lines: faster healing, less dehiscence
Perpendicular = wider scars, delayed healing, “dog ears”
Excision: First attempt = best attempt
Lipoma: 0 cm margins
Mast cell tumor: 1–2 cm
High-grade sarcoma: 3 cm
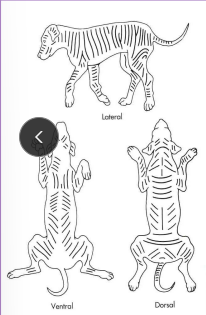
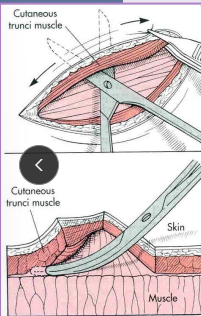
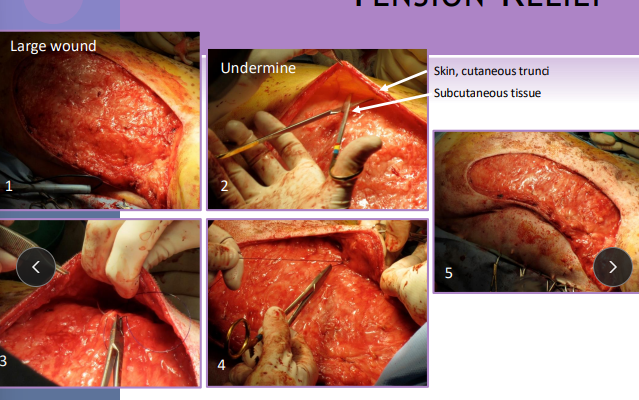
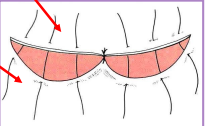
Skin Tension relief Surgery Techniques
Undermining: Tension relief, simple, max elastic potential
separate skin + panniculus from SC tissue
Delayed wound healing
Walking sutures: Tension relief, move skin / tack down, obliterate dead space, distribute tension
Stretch skin over defect
Use multi rows of suture anchored in fascia and dermis
Do not penetrate the skin surface
Tension Relief Sut: cruciate(skin), horizontal/vertical mattress (fascia/deep tissue), far-near-near-far (support)
Limited effect

Stents & quills: Tension relief
red rubbers

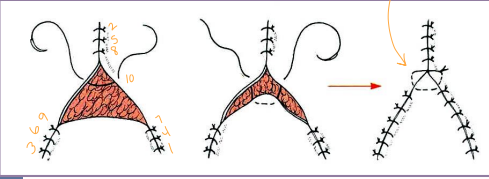
Abnormal Wound type closures
Dog ears: excess skin puckers
Excise ellipse or trim excess → scissors
Circular defects:
Linear: Start at center and close parallel with line of tension
Ellipse: 4:1 length:width ratio, eliminates dog ears
Combo V: 45° from axis of tension, extra skin is not removed → eye lid masses
Triangular defects:
Y-closure: Start at points and work inward, horizontal suture at center
Rotational flaps: 4:1 length:width ratio, semi circular flap formatted onto defect
Square/rectangular: start at corners work inward, may use advancement flap
Fusiform/elliptical: place central suture, bisect segments
Crescentic: one side is longer than other
close from midpoint, sutures closer on concave side

Skin Grafts
Transfer of a segment of free dermis and epidermis to a distant recipient site
Full-thickness (recommended)
Epidermis and dermis
Mesh:
* Increased surface area
* Better conformity
* Fluid drainage
Critical to graft survival
Healthy vascular bed
Lack of motion
Contact between the bed and graft
Lack of infection
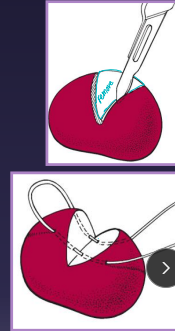
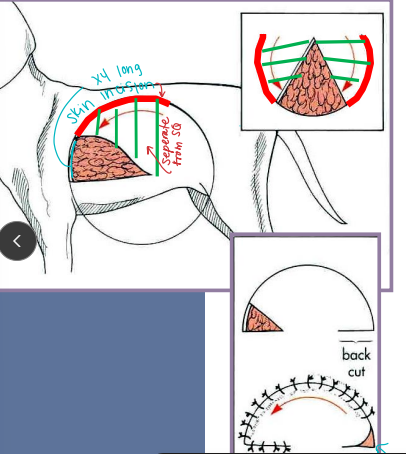
Ear Surgical procedures
Pinna Lacerations: partial thickness vs amputation
Aural hematoma: longitudinal planar fracture of articular cartilageobliterate dead space (incision+suture, CO₂ laser, steroid infusion)
Lateral ear canal resection: for otitis externa only / vertical, small lateral neoplasia
remove lateral wall of the vertical ear canal
New opening is at junction of vertical and horizontal canal
must still Medicate ear
Vertical ear canal resection: confined vertical otitis (normal horizontal) better cosmetic sx
Total ear canal ablation TECA + lateral bulla osteotomy BO: chronic otitis, neoplasia
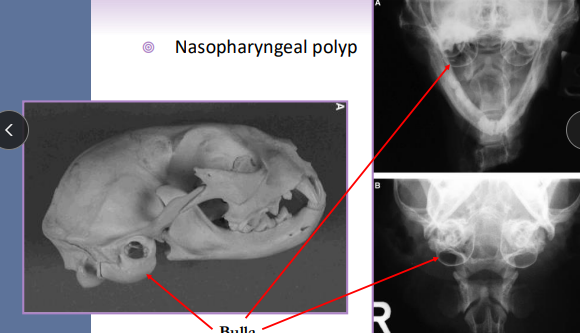
Ventral bulla osteotomy: cats neoplasia, polyps
increased exposure to tympanic cavity and bulla drainage
Cats have two bulla compartments
Tail & Rear Surgery
Caudectomy (Tail docking): Cosmetic, trauma, neoplasia
Puppies 3-5d: local anesthesia
Adults: general anesthesia, ligation, V-incision closure
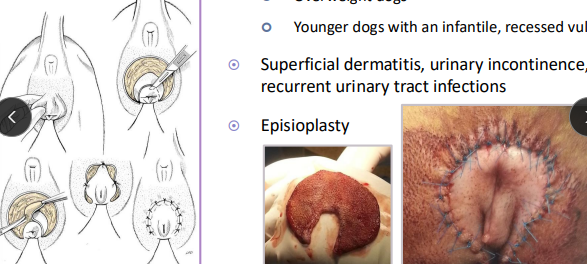
Episioplasty: Vulvar folds
overweight dogs, younger recessed vulva
En-bloc resection: Tail folds
Bulldogs
Redundant skin overlaps a deformed terminal
caudal vertebrae & prone to 2ndary infections
Foot surgical procedures
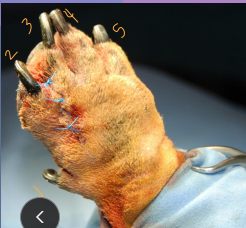
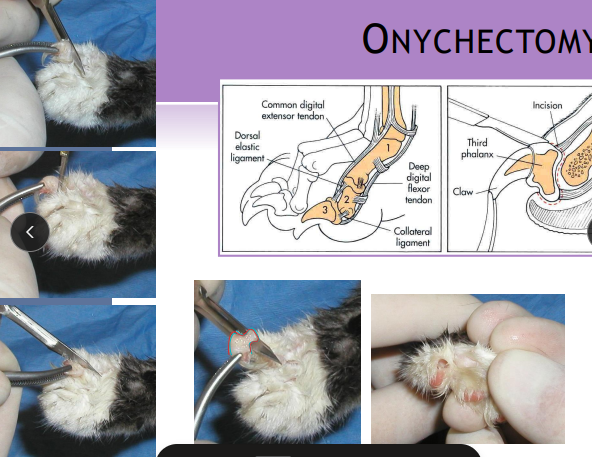
Onychectomy (Declawing): P3 removal at 3-12m
Scalpel, Resco clippers (risk bone left), CO₂ laser
Local /ring block to provide additional analgesia
Place a tourniquet (Radial neuropathy - limit time)
absorbable monofilament sutures
Post-op bandage, paper litter
Dewclaw removal
Puppies (3-5d): no anesthesia, silver nitrate
Adults: GA, excision (bony vs soft tissue)
Digit amputation: neoplasia, infection, osteomyelitis, severe trauma
3rd & 4th digits = weight-bearing
Footpad lacerations: irrigation, 2-layer closure, padded splint
Interdigital pyoderma: treat cause first → fusion podoplasty if refractory
fuses webbing/space between digits