Tendons, ligaments and bursae
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
What are tendons and ligaments?
Tendons (sinews) and ligaments (and fascia) are tough bands of dense fibrous connective tissue that withstand tension
What do a) tendons b)ligaments and c)fascia connect?
a) tendons connect muscle to bone
b) ligaments connect bone to bone
c) connect muscles to muscles
Briefly outline the role of tendons and ligaments
Tendons: transmit muscle force to boon in a controlled manner to effect movement at joints and to control the direction of the muscle force (some act as springs, storing and releasing energy).
Ligaments limit and control direction of motion at a joint.
Outline function of tendons
transmit muscle force to bone to allow joint movement
passive springs, store energy and reduce work of muscles
tendons reduce weight over lower limbs by keeping muscle mass near the body.
What are benefits of tendons in limbs
reducing weight
keep neuro-vascular bundles as short as possible
permits rapid and efficient limb movement
Outline tendon morphology
most are narrow and oval/round in cross section
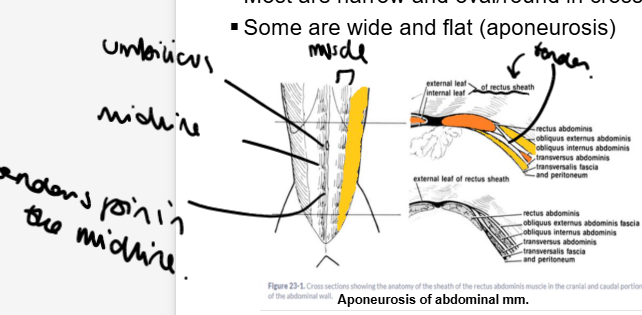
some are wide and flat - called aponeurosis
Give an example of aponeurosis
abdomen
no bones in the abdominal wall therefore the tendon is flattened out allowing a wide attachment to other structures.
Acts as a sheath (called the rectus sheath)
How does tendon insertion work?
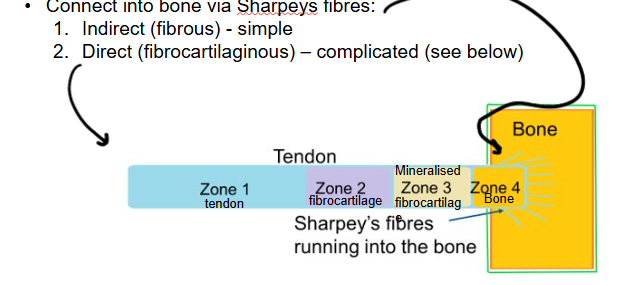
Muscles have origin and enthuses (insertion poitns) where they attach to bone.
Tendons of origin vs tendons of insertion
connect into bone via Sharpeys fibres
1. Indirect (fibrous) - simple
2. Direct (fibrocartilaginous) - complicated (see image)
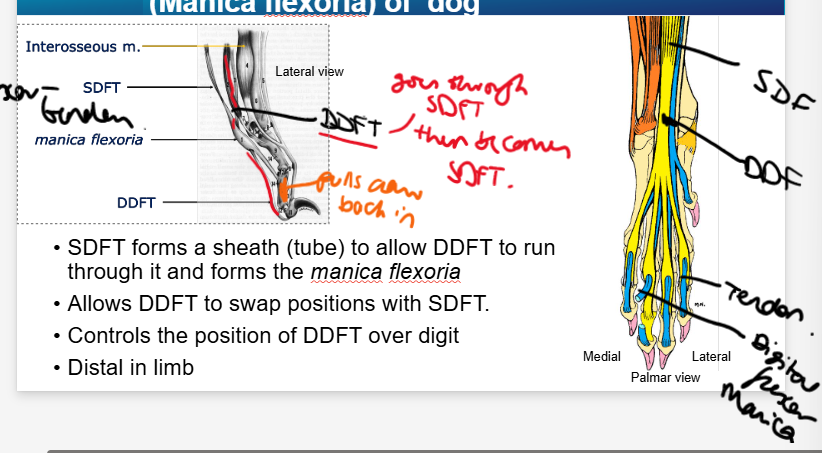
What is an example of a specialised tendon?
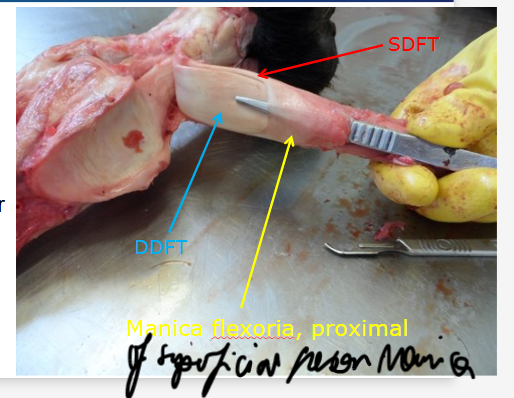
Manica Flexoria - a specialisation of the superficial tendons of digits
Outline manica of superficial ditigal flexor tendon (manica flexoria) of dog
Superficial ditigal flexor tendon forms a sheath (tube) to allow the deep digital flexor tendon to run through it forming the manica flexoria
allows DDFT to swap positions with SDFT
Controls the position of DDFT over digit
distal in limbs
How does the proximal manica flexora differ in the horse?
only 1
a small ring of SDFT which wraps around DDFT in proximal part of digital flexor sheath
what’s a risk of proximal manica flexoria in the horse?
often missing
can be torn
What cells do we find in tendons, ligaments and fascia
specialised fibroblasts that make the ECM
called tenocytes in tendons
What is in the ECM of tendons, ligaments and fascia
Varies however generally compromises:
Collagen type 1 fibres
Elastic fibres, amounts vary (allow stretch and elastic properties)
Proteoglycans (absorb and retain water)
Ground substance (material found b/w the above materials, some components inter, others potentially active.
Outline the cells found in tendons
Mechanocytes
Tenocytes are located b/w and associated with collagen fibrils
orientated to the long axis of fibrils
have a 3D network of processes that enable cell signalling via gap junctions - enables detection and response to mechanical loading
sense tensile loads transmitted by tendon or ligament through their contact with fibres and cells response by altering quantity and composition of ECM.
Tenocytes: detect changes in load by changing length - strain receptors
Why are tendons slow healing?
low cellularity
poor vascularity
difficult to rest and injured/repairing tendon
What is the composition of tendons?
55-70% water
Dry mass includes:
few cells
60-85% collagen, mostly type 1, some minor types too (2,3,4,5,6 and 10)
15-40% non collagen ECM
3% cartilage oligomeric matrix protein (glycoprotein) COMP
1-5% proteoglycans retains water to resist compression
1-2% elastin protein fibres
0.2% inorganic components (Cu2+, Mn2+, Ca2+)
When may tendons appear more yellow?
When they have more elastin
What role do elastin protein fibres have in tendons?
enable return to a normal size after stretching
Why are there so many kinds of collagen?
Amino acid variations
How is collagens steady turnover controlled
metallo-proteases (MPs) are enzymes that break down collagen cross-links
MPs are controlled by Tissue Inhibitors of Matrix Metallo-Proteases (TIMPs)
How is collagen synthesised
Procollagen is a triple helical protein made INSIDE fibroblasts
Outside the cell, procollagen is trimmed to a soluble triple helix collagen molecule helps elasticity.
Molecules cross link to become insoluble
Collagen molecules self-assemble into fibrils outside cells
bunches of fibrils arrange into a collagen fibre
these are wrapped up in a fine connective tissue sheath
what bonds hold collagen together
Initially by hydrogen bonds
Covalent inter- and intra-molecular links provide strength
Proteoglycans placed longitudinally and transversely strengthen them.
How do the molecules lay themselves out in collagen?
A staggered pattern with regular gaps, cuases bands
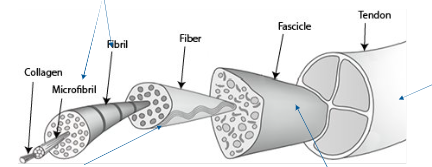
Outline gross anatomy of collagen
tenoctyes produce and secrete tropocollagen (precursor molecules) - self assemble into microfibrils then outside the cell into fibrils.
Bundles of fibrils are organised to form fibres
Bundles of fibres are organised parallel to each other with tenocytes and organised into fascicles (bundles) bound and separated by endotenons
bundles of fascicles form tendons - covered by an epitenon
tendon is enclosed by fascia loosely held on by a fatty areolar tissue (paratenon)
what feature do collagen fibres have and why
wavy pattern/crimp
Important in shock absorption, crimp straightens out taking the shock of the load, preventing bone damage)
What is the epitenon
an outer sheath of dense irregular connective tissue on the tendon
from which endotenons extend between fascicles
what is the paratenon
fatty areolar tissue that holds the fascia.
How are collagen arranged in tendons vs ligaments
tendons - parallel rows
ligaments - criss-crosses (so that forces can be applied in different directions)
what kind of stress to collagen fibrils resist
tensile stress
Outline elastin properties and function
fibroblasts make fibrillin that makes a scaffold for elastin to be deposited on.
Elastin:
hydrophobic = tight coils and loops
very elastic (150% stretch)
variations in amount alter mechanical properties
elastic vs positional tendons (nuchal ligament vs collateral ligaments)
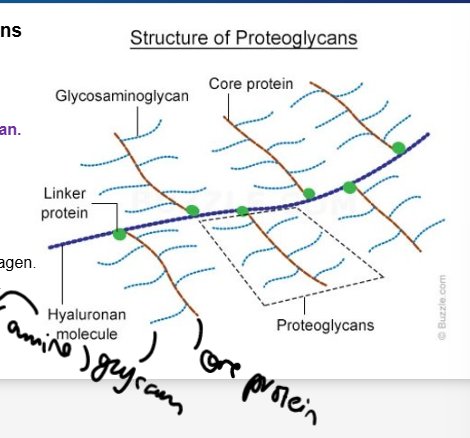
Outline proteoglycans (PGs):
function
what do they form
what do they consist of
2 examples
resist compressive stress
interconnect collagen fibres and bind water - forms a water bag
consist of a protein core bonded to GAG
examples
decorin
aggrecan
What are decorin and aggrecan
Decorin promotes fibril slippage, found in bones
Aggrecan binds water, resists compression and is a major PG of cartilage tendon
what GAG components in tendons are involved in collagen fibril assembly? What are each of their functions
Dermatan sulphate GAG - organises collagen fibrils (forms associations b/w them, causing parallel alignment and separates them whilst forming interfibril bridges)
Chondroitin sulphate GAG - involved with occupying volume b/w collagen fibrils - keeps separated and helps withstand deformation.
Outline proteoglycan structure
GAG side chains attached to a core protein (hyaluronan molecule)
Large PG:
form aggregates with hyaluronan, large swelling potential, bind cations and water, resist compression
Small PG:
bind to ECM molecules, fibril diameter and cross-linking, tensile strength, binds growth factors.
Look like toilet brushes
Outline GAG (glycosaminoglycan as special ECM molecules
repeats of CHO and amino acid as a chain
bind with collagen to create a meshwork: ECM
able to bind water - creates the gel-like qualities of tissues (important for tendon function)
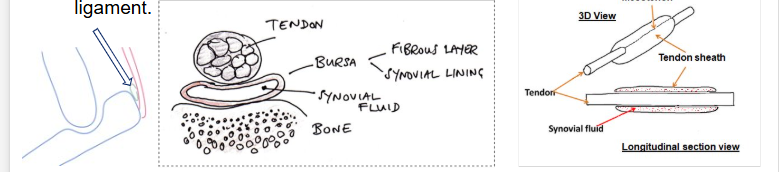
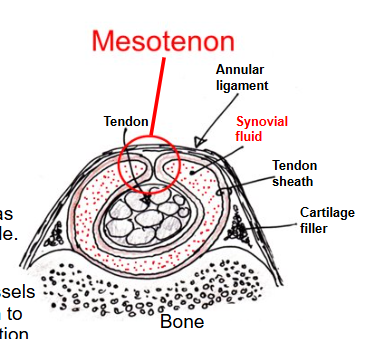
Outline sheaths and bursae:
what are they
what do sheaths secrete and what does this influence about their structure
what are they analogous with
where are they located
Synovial bursae and tendon bags
tough connective tissue bags
sheaths secrete and contain synovial fluid and a lubricant therefore are closed bags
analogous to synovial wall of joints
located mainly under tendons/ligaments near the insertion at joints to reduce friction on the tendon as it passes across a bone/under a ligament
Outline tendon neurovascularity
blood vessels run in endotenons, parallel to collagen fibres with occasional branching transverse anastomoses - poorly vascularised though
aneural in tendons - epitenon and paratenon do contain nerve endings. Golgi tendon organs are present at myotendinous junction b/w tendon and muscle
What is the clinical relevance to a tendon sheath injury
can be inflamed by repeated movements/strains e.g. tendonitis/tenosynovitis
note: blood supply in sheathed tendons is conveyed by the mesotenon n.v.b.
Tendon healing w/in a sheath will be delayed as only the internal tendon blood supply is available
If the tendon sheath is torn, healing will be accelerated (vessels have easier access) but may lead to adhesions which impair gliding functionD
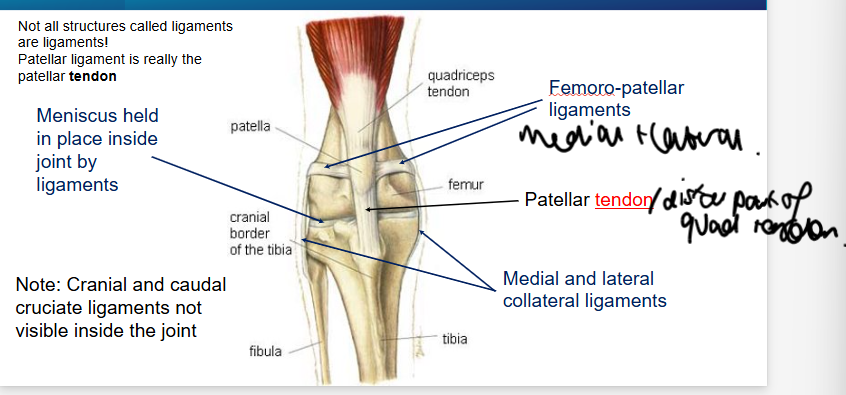
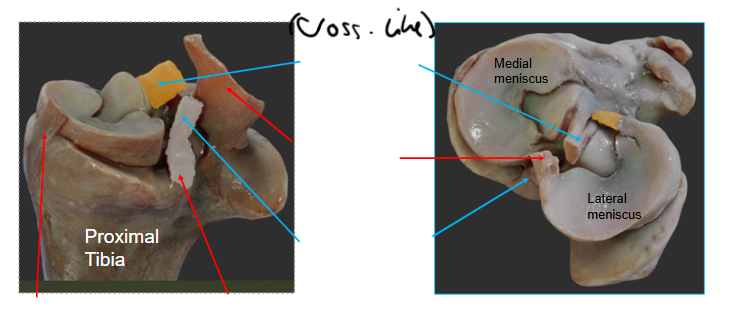
Outline the gross anatomy and role of ligaments
dense collagen fibre bundles - tough thickened parts of joint capsule, dense bundles of elastin fibres (multiple directions but not irregular), lined by synovial membrane
similar composition to tendons, 10% elastin content, more type 3 collagen and more cells.
Role: support and control movement
Skeletal ligaments join bone to bone/cartilage
Briefly outline splanchnic ligaments (organ related)
peritoneal - a fold of the peritoneal membrane supporting and separating abdominal organs
remnants of a foetal tubular structure - should close up and shrivel after birth, becoming a cord-like structure.
peridonteal ligament - attaches tooth cement to alveolar (socket) bone.
Outline some features of skeletal system ligaments
reinforce joint to limits its direction of motion
viscoelastic
provide stability at the price of mobility
collagen fibres are criss-crossed
what are the 3 locations formations of ligament attachment
form the joint capsule (capsular)
form outside the capsule reinforcing it (extracapsular)
form inside the capsule (intracapsular)
what does the viscoelastic property of ligaments enable
deformation when strained and tension when under stress but return to normal shape as long as it’s not deformed past strain threshold.
what is a potential consequence of a weakened ligament
joint becomes unstable and may dislocate
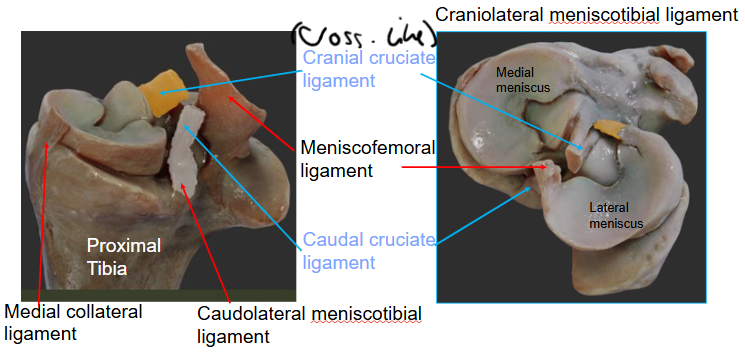
Label this diagram
Label this diagram
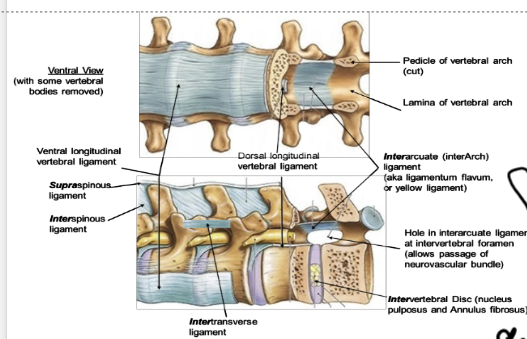
What are the names of the 6 ligaments found in the spinal column
supraspinous (above spinous processes)
interspinous (b/w spinous processes)
intertransverse (b/w transverse processes)
interarcuate (b/w vertebral arches, online one that lies inside dorsally)
Intervertebral (b/w vertebral bodies)
longitudinal (run longitudinally along vertebrae)
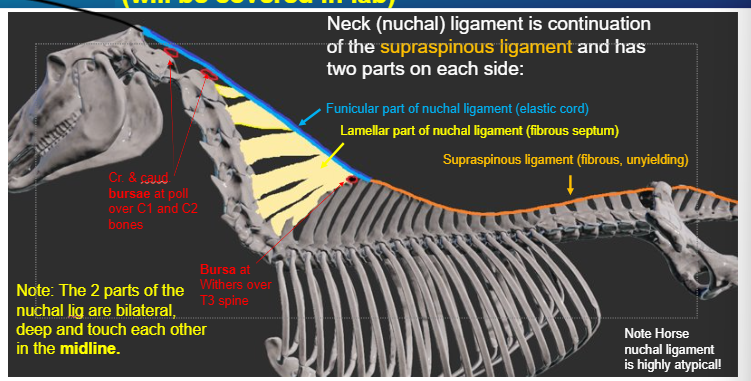
what is the function of the nuchal ligament
support head and neck
prevents head/neck descending on every stride, storing energy that helps neck muscle mass to pull head back up at each stride, preventing muscle fatigue
Outline some features of the nuchal ligament in different animals
better developed in animals with large heads and/or long necks
can have 2 parts (lamellar and funicular e.g. horse) - most only have funicular (e.g. dog)
pigs have no nuchal ligament
what enables the nuchal ligament to stretch and store energy?
dense elastin
Outline the nuchal ligament in the horse - structure.
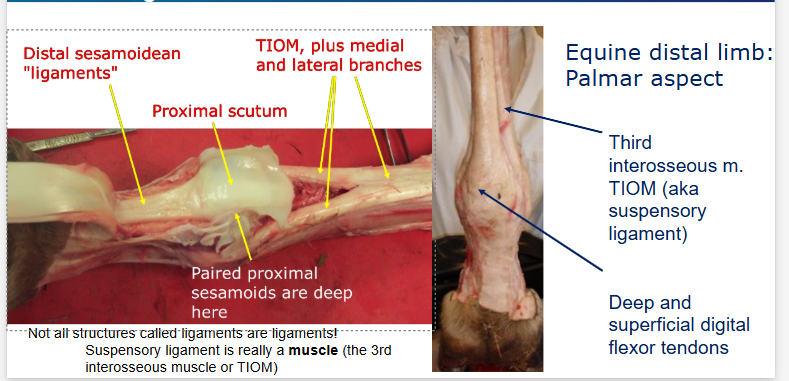
outline the structure of the 3rd interosseous muscle (TIOM) aka suspensory ligament
Key point - a ligament in horses, the TIOM in dogs and other small animals
outline the gross anatomy of retinaculae and what are they
straps of tissue similar to ligaments that cross over the long axis of joints (don’t directly serve the joint e.g. cross the entire wrist rather than b/w individual bones)
binds down the tendons close to the bone - preventing bow-stringing away from the bone
what will happen if the retinaculum is ruptured?
tendons will displace (bow-string) and ‘tent’ the skin
what are fascia
membranous sheets, similar to ligaments
what kinds of fascia are there
superficial: connect/anchor skin to deep fascia - loose adipose, vascular
deep - wrap up muscles, less adipose, more elastic, many thin blood vessels
visceral - connect/anchor serous membranes to organs and inside of body wall

what do fascia form?
fascial compartments separated by inter-fascial compartments
enable fluid to be drained

what is the clinical use of (inter-) fascial compartments
can predict the spread of infections
administering IM injections - keep the muscles in place.

what are 5 functions of fascia
reduce friction of muscular force - provide a movable wrapping, supporting and separating muscle groups and for structures that pass through/b/w muscles e.g. nerves and blood vessels
support muscle - provide attachment, for muscle fibres to exterior of muscle
stabilise and connect structures- distribute tensional forces across several joints in a network-like manner
store and release elastic potential energy
proprioceptive ability - due to the innervation of sensory nerve endings

what is the clinical significance of fascia
problems if it loses stiffness, too stiff, decreased shearing ability.
inflammatory fasciitis or trauma may cause fibrosis and adhesions (where fascia fail to separate adjacent structures effectively (post surgery for example)
increase in intra-fascial compartment pressure (compartment syndrome) may require fasciotomy
What are the mechanical properties of tendons
Vary, matched to functional requirements
energy storing tendons tend to be flexors, more elastic/less stiff, so store/absorb energy - fail at higher strains (12-15%)(horse SDF can stretch in excess of 20% when galloping)
stiffer ‘positional’ tendons tend to be extensors, less elastic, so can provide finer control of movement. Guide limb movement.
tendons respond to changes in mechanical loading with growth and remodelling processes, disuse tendon results in a decreased average thickness of its collagen fibre bundles
What’s responsible for the crimp of tendons, where do we see it and what happens as the animal ages
tenocytes are contractile and responsible for the crimp
seen in secondary bundles (wavy appearance when relaxed, disappears when first loaded)
degree of crimp reduces with age - leads to a more rigid structure so more prone to failure.
what are 4 properties of tendons and what enables these properties
cross linking - GAGs
ability to stretch - related to water content and proteoglycans
elasticity due to elastin and helical collagen molecules
shock absorption due to crimp
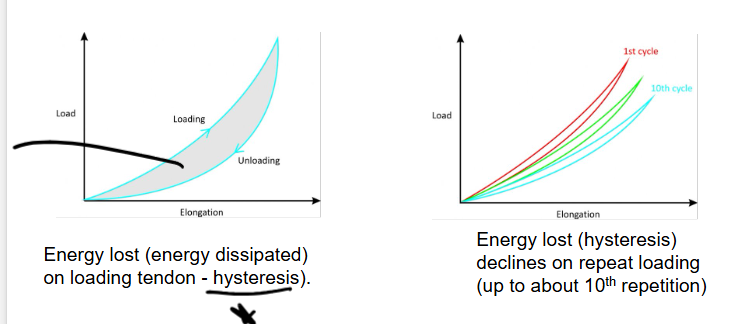
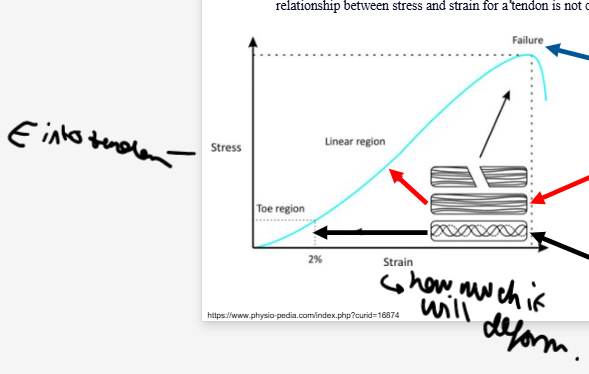
Outline the stress-strain curve
tendons have viscous and elastic behaviours (viscoelastic) so their mechanical behaviour is dependent on RATE of mechanical strain
SS curve starts with a very low stiffness ‘toe’ region (shock absorbing) as the crimp straightens and the collagen fibres align
after ‘toe’ region, linear part of SS curve where tendon becomes significantly stiffer and collagen molecules slide past one another (Inter-molecular sliding) - tendon can revert back to original length.
When intercollagen cross links fail get irreversible plastic deformation and failure.
Outline the mechanical properties of tendons with 2 diagrams