Mechanical Agents
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
Mechanical Agent Modalities
theraputic mech devices to apply froces such as compression, distraction, vibration, or controlled mobilization
Instrument assisted modalities
refers to the therapeutic use of an instrument or tool that is manually applied to target specific tissues such as Skin, Fascia, and other connective tissues, or muscle
Mechanical agent physiological
Mechanical deformation (stretch movement of collagen fibers), localized inflammatory response (increased blood flow) and activation of the immune system
Examples of Mechanical Agents
Compression (Wraps, compression garments, short or long stretch)
Superficial effleurage or manual lymphatic drainage (MLD)
Taping (elastic, athletic, Leaukotape with Hypafix)
Cupping
steel Blading
Massages devices
Changes with fascia and superficial vessels/nerves
increase stiffening of the carotid and other vessels with pregnancy and post menopausal women
arterial stiffening with age, especially carotid and femoral
Hypertension affects the extensibility of arteries
Post radiation arterial changes, stenosis, weakening of the wall
Desired Depth
.1mm skin
.6mm epidermis
1.5mm Nerves and lymphatics
2.5 mm Fascia
3.5mm muscle start
4 components involved with Edema
capillaries
tissue channels
macrophages
initial lymphatics
Circulatory system
Arterial functions: nutrients/immune
Venous functions: carry de oxygenated blood, a reservoir
Capillary functions: fluid and nutrient exchanges
Lymphatic Functions: Remove excessive fluid and waste product. return fluid and plasma proteins to the blood, alert the immune system
Types of lymphatic system failures
dynamic insufficiency: increase lymphatic load- healthy lymphatic system
Mechanical insufficiency: Normal lymphatic load- on a damaged lymphatic system
Combined insufficiency: Increased lymphatic load - on a damaged lymphatic system
Causes of Edema
imbalance between hydrostatic and osmotic pressure
venous or lymphatic obstruction or insufficiency
increase capillary permeability
immobility
pregnancy
neurological injury
surgery/ trauma
Volume Measurements
Used to quantify the edema in a patient and compare the affected limb to the non affected.
What is the gold standard for Volume Measurements
Perometer: volume is determined from the 3D silhouette cast of the limb. Only con is that it doesn’t provide a composition breakdown
Water displacement
Clinic would use a volumetric edema gauge system, however this is not realistic in a clinic due to
money for equipment
time to perform
water source
patient may not be able to submerge limb due to wounds or limb being to large
bioimpedance
Electrical current through the body via 2 points of contact
measures the body’s resistance in response to this electrical current to provide an assessment of extracellular fluid, intercellular fluid, and total body water
tissues with high levels of fluid and electrolytes have high conductivity while fat and bone slow the single down
Bioimpedance Cons
Most rely on population-specific data to create an estimate, which does not consider that body geometry
impedance is greater with extremes in levels of fat. hydration is higher in significant obesity, so it underestimates body fat
Measuring progress with treatment with edema
initial measurements
during treatment to judge progress
before and after treatment
progress notes for MDs, patients and/or insurance
at discharge
Contraindications to compression in general
arterial insufficiency
neuropathy
inability to communicate pain and discomfort
Ankle Brachial Index: <0.8-40 mmHg at most, >0.5 to <0.8:23-30 mmHg at most, <0.5: compression should be avoided
Compression: principles
Compression: Forces exerted to an area on the body surface
Pascal’s Law: when pressure is applied (functional activities) on a fluid (a muscle or muscle group) in a closed container (fascia and compression bandage) there is an equal increase at every other point in the container
Sub-Bandage or Interface Pressure
Pressure exerted by compression on the skin expressed in mmHg
Resting Pressure (RP)
pressure exerted by the compression on the bandaged segment at rest
Working Pressure (WP)
pressure exerted by the compression on the bandaged segment during muscle contraction
Categories of compression
No stretch: 0% (cast)
Low Low stretch: 1-50% (Durelast, Una Boot)
Low stretch: 51-90% (lymphedema brown bandages)
Medium Stretch: 91-140% (lekelast)
High stretch >140% (ace, tubigrip)
Benefits of gradient compression
Increase:
venous and lymphatic circulation/transport
muscle pump temperature
tissue temperature
Decrease:
Risk of DVTs and severity of post-thrombotic syndromes
fibrosclerotic tissue
pain reduced via reduced stress on nerves, joints, ligaments, and fascia
Hypertrophic scarring from burns and trauma act as a mold for the growth of new tissue
Helps with shaping a residual limb and fluid reduction
General rules with Gradient Compression
Needs to be gradient: more pressure distal
Worn while exercising
Types of compression must meet the needs of the person
Compression MUST go at least 2 inches above where the edema stops
cannot prevent a person from performing ADL
Garments: help maintain the reduction a person has received with bandageing or preventatively post op to limit the amount of edema
compression pumps
Uses:
post-op edema or inactivity to prevent DVTs, and dependent edema. post-traumatic edema, chronic venous insufficiency
Only use in low-pressure settings: 40 mmHg on LE and 25 mmHg on UE
Precautions for compression pumps
Arterial insufficiency
open wounds
fragile skin
easy bruising / clotting issues
reduced sensations
inability to communicate pain, pain with the pump
genital involvement
active cancer
edema in the adjacent trunk
Taping (theories with pain reduction)
removes pressure on free nerve ending
allow more fluid movement to reduce pressure on painful tissue
increase sensory receptor reactions (decrease pain or abnormal sensations)
blocks stimulation to the brain like TENS
Adverse outcomes with taping
Too much stretch on tape: Reaction will not be uniform on skin, often seeing blisters, scabs, or skin irritations/burns in select areas
Allergic reaction to tape: Will usually be uniform, can be bumps, discolorations, itching or any skin irritation
Athletic Tape Roles
restricted motion of an injured joint
compress soft tissue to reduce swelling
support anatomical structures involved with the injury
serve as a splint
secure dressing
protect the site from being reinjured
Athletic Tape Mechanism
enhances proprioceptive feedback from a limb or joint
provide support
limiting motion will prevent injury and allow the injured tissue to heal
gate theory
limits edema by increasing the tissue pressure to limit ultrafiltration from arterial capillaries
feedback for postural or mechanical control
Athletic Tape Disadvantages
skin damage
damage to other joints/tissues from limiting area under application
tape can lose stiffness over time
can develop dependency
costly with prolonged use
Leukotape and hypafix
-reduce pain
-provides support and stability to joints
assist in realigning structures or joints alignment
sensory feedback via cutaneous mechanoreceptors
help protect the area
restores functional movement
postural tape
does not affect circulation or ROM
Leukotape and hypafix Disadvantages
risk of skin breakdown or allergy
expensive
can restrict blood flow if to tight
damage to other joints/tissues from limiting area under application
can develop dependency
Elastic Tape theories in increasing ROM
to find the direction for tape, gently pull skin around joint in different directions to see which reduces pain
then apply the stabilization strip in the SAME direction
the decompression strips would be PERPENDICULAR
Elastic Tape theories for scar reduction
passive prolongs static stretch can improve
lengthening of the tissues
encourages proper laydown of tissue
don’t apply the tape over incision is 6 weeks out
usually applied alternating medial and lateral in incision/cut with pressure towards midline
Elastic Tape disadvantages
does not stick as well as normal tape
may be to elastic to provide support
risk of skin break down
expensive with prolong use
Precautions with Elastic Taping
there should be 15-20% stretch inherent in the tape, up to 40% with pull
When possible stretch the skin (flex/bend) instead of the actual tape
if pt has never been taped before use a test patch
remove if itching
Precautions or contraindications with cupping
areas of current or previous DVTs
Directly over superficial veins/arteries
over an infection
over an open wound
avoid boney area
Precaution:
pediatrics
fragile skin
geriatrics
pregnancy
mensurating women
Theories: impact of skin and tissue
Compressive stress to skin at the rim
tensile stress to skin/tissue under the cup (distraction forces)
Cupping uses a (-) low pressure, like a vacuum, to move fluid and displace the the layers in cutaneous tissues
Cupping Outcomes/Results
Increases:
temperature
circulation
healing
Decrease:
Blood pressure
muscle tension
scars from trauma or burns
cellulite appearance
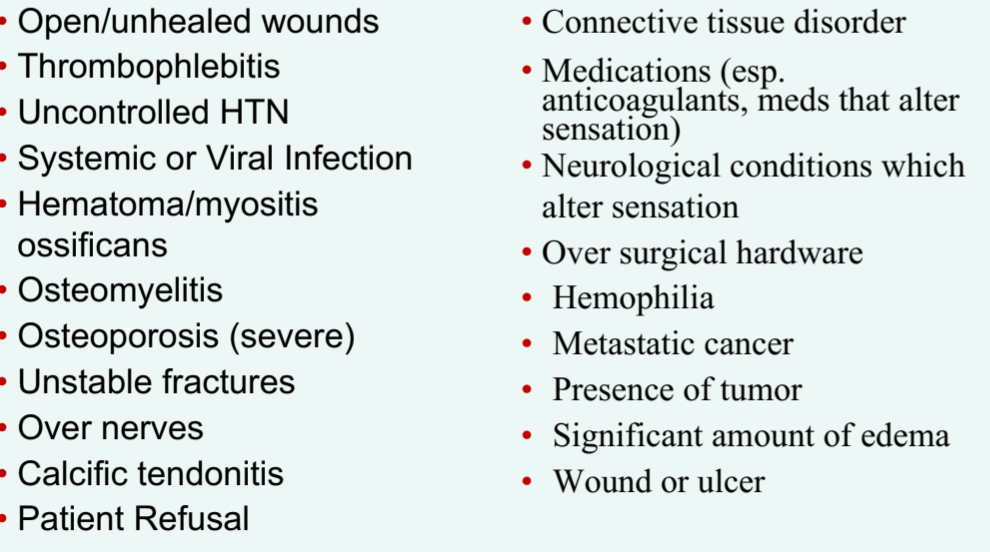
ABSOLUTE contraindications of IASTM (steel Blades)
Relative Contraindications/ precautions of IASTM
Cancer
Mature Scars
Kidney dysfunction
Pregnancy
RA
Varicose Veins
Lymphedema
Polyneuropathy
Tattoos
Osteoporosis
Diabetes
CHF
Benefits for IASTM
increase precision with regards to location and shape
can feel the tissue through the tool
increased tactile feedback
decreased stress/ fatigue on clinician
noninvasive
easy to clean up
IASTM Mechanical
Pressure and shear on collagen fibers initiated inflammatory cascade
increase blood flow
stimulates release of cellular mediators and growth factors to draw fibroblasts to the area
fibroblast proliferation - collagen production - connective tissue healing
Traumatic Hyperemia: which leads to pain relief and decreased scar tissue
Pain Relief from IASTM
stimulates type 1 and type 2 mechanoreceptors
types I: superficial capsule, limbs and vertebrae
Type II: deep capsule
Pain relief via gate control control theory
decreased central sensitization/ altered neural input
Indications for IASTM
Cumulative trauma
tendinopathies
trigger points
fascial restrictions
ligament sprains
edema
soft tissue entrapment
post operative
Clinical Use of IASTM
Goals are to increase rom, decrease pain, improved connective tissue mobility/texture
warm up/recover from performance, reduce edema
However no evidence for optimal parameters
Instrument Selection
Size
conforms to different body surfaces
single bevel: penetrates deeper that double bevel edges
double bevel edges can be applied in both directions
Concave instrument on convex body part: disperses forces over a large area and improved patients tolerance
convex instrument on convex body part: focuses force at a small surface area, more specific treatment
Method Strokes
Brush
Sweep
Fan
Strum
J stroke
Negative outcome
-soreness
-bruising
-petechiae
-should be mild and of a short duration
-manage with use of ice
Foam rolling Application
Located the Tender spot in the muscle
Place the ball/cane on the tender area
apply pressure with: hands, body weight
hold and roll for at least 30 sec
Release pressure for 10 secs and then repeat 4-5 times
BE CAREFUL OF PRESSURE ON NERVES
Theragun Percussive Therapy
Uses rapid, repetitive strokes to stimulate blood flow and heat
only use for 30 seconds of each area
deliver 16 mm of amplitude at a speed of 40/29 percussions per second on the body
different attachments and an adjustable arm
no complling reasearch
Mechanical Agents Documentation
history Of condition and/or subjective comments
current conditions/objective measures
skin
edema/girth
pain scale
adl ability
treatment parameters
outcomes or response to treatment