Ventilation-Perfusion Matching and Mismatching
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
38 Terms
distribution of blood flow is uneven due to
gravity
ratio of ventilation to blood flow for single alveolus
Va/capillary blood flow
ratio of ventilation to blood flow for entire lung
total Va/cardiac output
if ventilation > perfusion,
V/Q > 1
if perfusion > ventilation,
V/Q < 1
where is V/Q highest?
zone 1, at 3.0
where is V/Q lowest?
zone 3, at 0.6
V/Q mismatching is the most frequent cause of
arterial hypoxemia (reduced blood PO2) in cardiopulmonary disease
ventilation increases more slowly than blood flow from apex to base, so
V/Q ratio at apex > 1 and decreases as move down lung
regional differences in VQ produce
regional differences in PaO2 and PaCO2, with regional differences in PaO2 being much greater than those of PaCO2
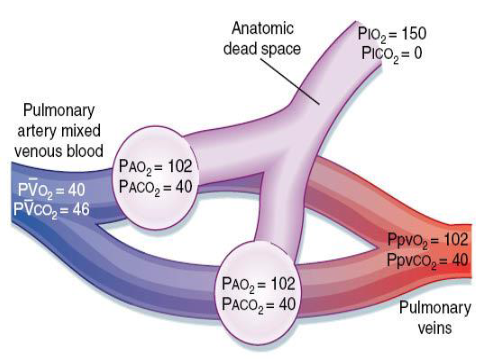
normal flow (without shunt)
2 normal, parallel lung units, both receiving equal quantities of fresh air and blood flow
blood and alveolar gas partial pressures are typical for a resting individual
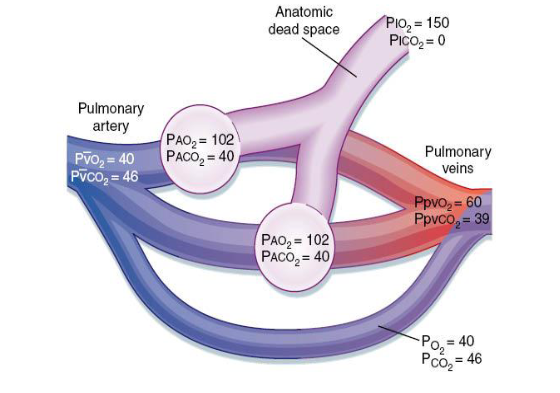
right-to-left shunt flow
mixed venous blood bypasses the gas exchange unit and goes directly into arterial blood
thebesian vessels
tiny veins in the wall of the heart chambers
of left ventricular myocardium, coronary venous blood drains directly into left ventricle rather than right atrium via these vessels
this is an example of how normally some blood always bypasses gas exchange units
arterial hypoxemia
result from additional defects that can occur
deoxygenated blood from right atrium or ventricle crosses septum and mixes with blood from left atrium or ventricle
cannot necessarily be corrected by administering 100% O2—shunted blood never exposed to enriched O2
final PaO2 will depend on size of shunt
a PaO2 less than 80mmHg in an adult breathing room air at sea level
bronchial circulation
1-2% total cardiac output, contains oxygenated blood, arises from aorta
supplies support tissue of lungs, including connective tissue, lower trachea, and bronchi
empties into pulmonary veins e.g. pleurohilar bronchial veins into the axygous vein which passes into vena cava
shunt
blood that enters the arterial system without going through ventilated areas of the lung
example of anatomic shunt
some of the bronchial circulation also passes directly (via deep bronchial veins) to the pulmonary veins
other abnormalities related to bronchial circulation
connection between pulmonary artery and vein (pulmonary arteriovenous fistula)
congenital defects can lead to right-to-left shunting after birth e.g. teratology of fallot (hole between ventricles)
result is to slightly depress arterial PO2 (since no gas exchange)
atelectasis
obstruction to ventilation of a gas exchanging unit with subsequent collapse- an example where the V/Q ratio = 0
causes include mucous plugs, foreign bodies, tumours
physiological shunt
ventilation to lung units is impaired in the presence of normal perfusion
lung unit with no ventilation has a V/Q ratio of 0
blood perfusing this unit is mixed venous blood and in the absence of gas exchange, the blood leaving is still mixed venous blood
deoxygenated blood bypasses the opportunity to exchange gas via contact with a gas exchange unit
dead space
V/Q = infinity
ventilation without perfusion (e.g. pulmonary embolism)
no gas exchange because there is no blood flow to receive O2 from alveolar gas
alveolar gas will have same composition as humidified, inspired air (PAO2= 150 mmHg; PACO2= 0 mmHg)
what happens to alveolar-arterial gradient during ventilation-perfusion mismatch on gas exchange?
will increase because relative over-ventilation of one area will not compensate for under-ventilation of another area
pulmonary embolism
blood clots that lodge in pulmonary arteries, often arise from detached portions of venous thrombi formed in lower extremities
thrombi cause shortness of breath, cough, hemoptysis (coughing up blood), tachycardia (increased heart rate), fall in blood oxygenation
example of V/P mismatching
restrict blood supply to alveoli being ventilated
high V/P and hypoxemia (low PAO2)
factors leading to venous thrombi
stasis of blood (e.g. immobilization after surgery)
alterations on the blood coagulation system (e.g. increased coagulability seen in sickle cell disease)
abnormalities in the vessel wall (e.g. due to local trauma or inflammation)
very large thrombi impact in
large arteries, but more common to break up and block several smaller vessels
pulmonary hypertension
mean pulmonary arterial pressure is approx 15 mmHg, increases are this
pulmonary hypertension causes
increase in left atrial pressure
increase in pulmonary blood flow
increase in pulmonary vascular resistance (most common)
pulmonary hypertension causes- increase in left atrial pressure
e.g. mitral stenosis (narrowing of the mitral valve opening that slows blood flow from left atrium to left ventricle) or left ventricular failure
sustained increases in left atrial pressure lead to structural changes in the walls of small pulmonary arteries (thickening)
result: dyspnea, hemoptysis, pulmonary edema
pulmonary hypertension causes- increase in pulmonary blood flow
e.g. congenital heart disease, patent ductus arteriosis- DA shunts most of blood from pulmonary artery to descending aorta in fetus. failure of the DA to close following birth results in left-to-right shunt
sustained high flow through pulmonary circulation results in recruitment/distention mechanisms being overwhelmed and structural changes in wall occur
pulmonary hypertension causes- increase in pulmonary vascular resistance
e.g. vasoconstrictive, like high altitude
obstructive, like thromboembolism
obliterative, like emphysema in which capillary bed is partly destroyed
effectiveness of gas exchange determined by
alveolar-arterial PO2 difference; A-a gradient
usually between 5-10mmHg in healthy person
value rises approx 3mmHg per decade of life
very upper limit of normal is 25mmHg
abnormalities in PaO2 may or may not
be associated with VQ inequality
hypercapnia
defined as an increase in arterial PCO2 above the normal range (40 ± 2mmHg)
hypocapnia
defined as an abnormally low arterial PCO2 (less than 35mmHg)
A-a gradient or alveolar-arterial PO2 difference (AaDO2)
subtract arterial PO2 (easily measured from blood gas analysis) from the ideal alveolar PO2, in absence of any inequality (derived from alveolar gas equation)
PAO2= PIO2 - (PACO2/R) + F (can ignore F)
mechanisms of hypoxemia
ventilation perfusion mismatch (most common)
shunt
diffusion abnormalities
alveolar hypoventilation (seen in overdoses of sedative/narcotic drugs, neuromuscular disease, etc)
low atmospheric oxygen (seen at high altitude)
VQ and hypercapnia
mismatching should cause both hypoxemia and this (CO2 retention)
but pts with mismatching often show normal arterial PCO2 since there is a reflex increase in ventilation rate triggered by chemoreceptors
increased dead space can also increase PaCO2 in absence of compensation, but local bronchoconstriction usually occurs immediately to redistribute perfusion
occurs in cases of hypoventilation
what kind of relationship between alveolar ventilation and alveolar CO2?
inverse, hypoventilation always causes decreased PaO2 and increased PaCO2