Immuno 38 | Immune-Mediated Respiratory Tract Disease
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
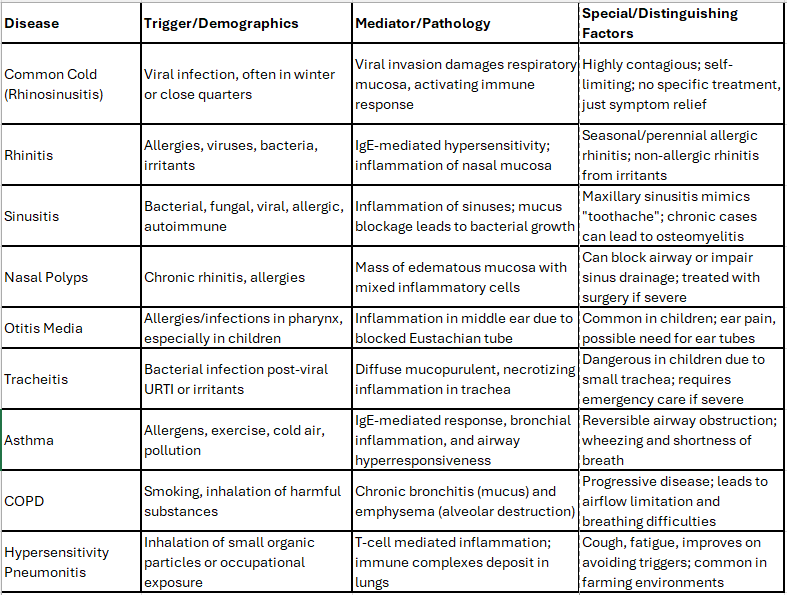
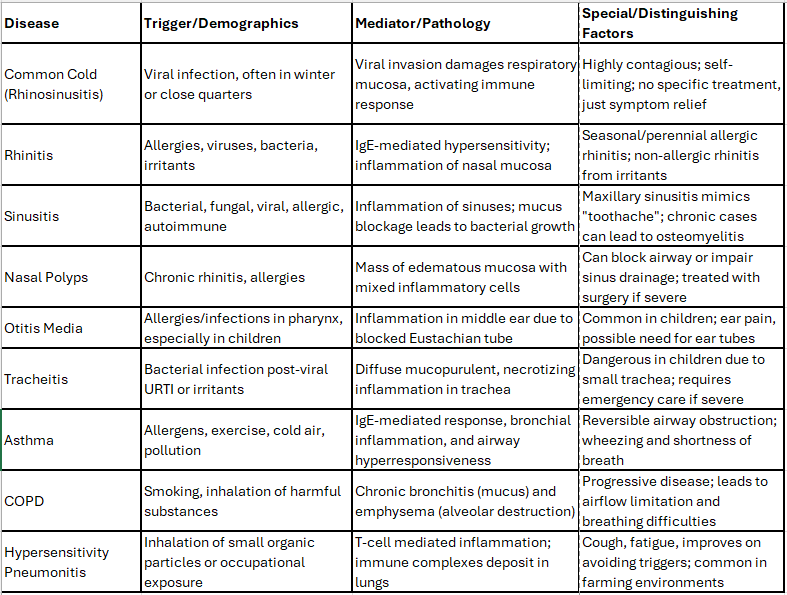
What are the four pairs of sinuses?
Maxillary Sinus - Largest, located under the eyes in the maxillary bone. Most often infected
Frontal Sinus - Above the eyes, in the frontal bone.
Ethmoid Sinus - Small air cells in the ethmoid bone between the nose and eyes.
Sphenoid Sinus - In the sphenoid bone, at the skull base center under the pituitary gland.
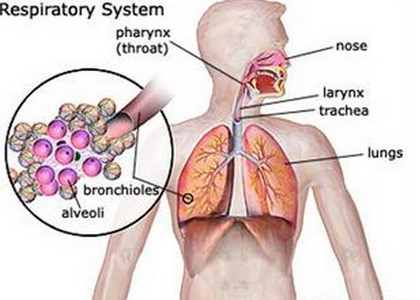
What is the first line of upper respiratory tract defense?
The mucociliary escalator helps clear microbes from the nasal cavity and lungs. It relies on pseudostratified ciliated columnar epithelium, which acts as the first line of defense in the URT by moving mucus and trapped particles out of the respiratory system.
What increases susceptibility to upper respiratory infection?
Seasonal allergies trigger IgE production and histamine release.
Smoking and pollution cause mucus overproduction, tissue damage, and weaken the mucociliary escalator impairing BALT defense.
IgA deficiency: The most common immune disorder, increasing risk of infections like bronchitis and pneumonia.
Stress: Alters immune response, raising infection risk.
What is viral rhinosinusitis?
An acute viral infection of the upper respiratory tract, typically lasting about a week and more common in winter; Common cold
What causes rhinosinusitis?
Viruses like RSV, adenovirus, parainfluenza, picornavirus, coronavirus, and enterovirus; spread by aerosols, contact, or fomites.
What is the pathophysiology for rhinosinusitis?
Virus damages respiratory mucosa, triggering immune response.
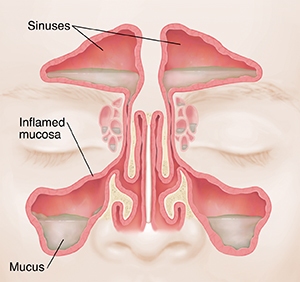
What is rhinitis?
Rhinitis is the inflammation of the nasal mucosa, often triggered by allergies from pollution & irritants
What type of allergic reaction is rhinitis?
Type I hypersensitivity reaction, where exposure to allergens causes the immune system to produce IgE antibodies, leading to symptoms like sneezing, congestion, and itching.
How is rhinitis treated?
Treatment focuses on symptomatic relief and may include immunotherapy to encourage an antibody switch from IgE (which causes allergy symptoms) to a different antibody called IgG4, making you less sensitive to the allergens over time.
What is seasonal allergic rhinitis?
Triggered by tree and flower pollen in spring (March-April) and mold spores from fallen leaves in fall (October-November).
what is perennial allergic rhinitis?
Happens year-round, caused by sensitivity to things like pet hair, mold, dust from wallpaper, houseplants, carpeting, and upholstery.
What is non-allergic rhinitis?
Not related to allergies or IgE. Often caused by irritants like cigarette smoke or pollutants, and can be worsened by factors like a deviated septum, infections, or overuse of nasal decongestants.
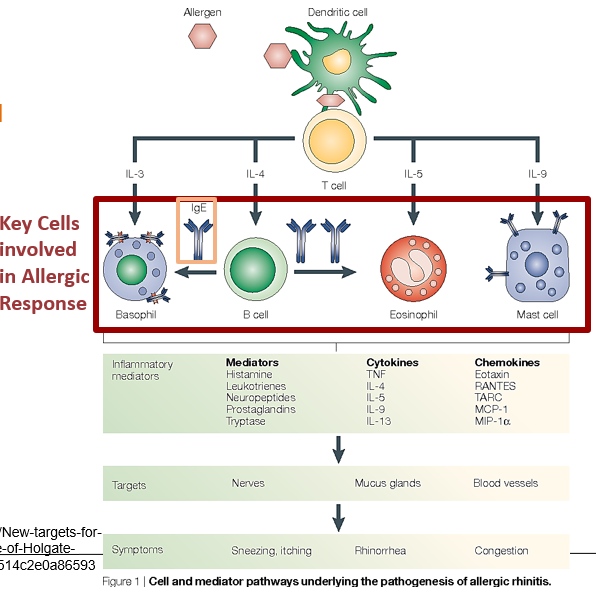
Which immune cells cause inflammation in allergic rhinitis?
Key cells involved: CD4 Th2 cells, IgE-producing B cells, mast cells, eosinophils, and basophils.
Cytokines: IL-4, IL-5, IL-13 help signal immune responses.
IgE: Binds to allergens and activates cells like mast cells and basophils.
Mediators: Histamine, prostaglandins, and leukotrienes are released by these cells, leading to inflammation and allergic symptoms like sneezing, itching, and congestion.
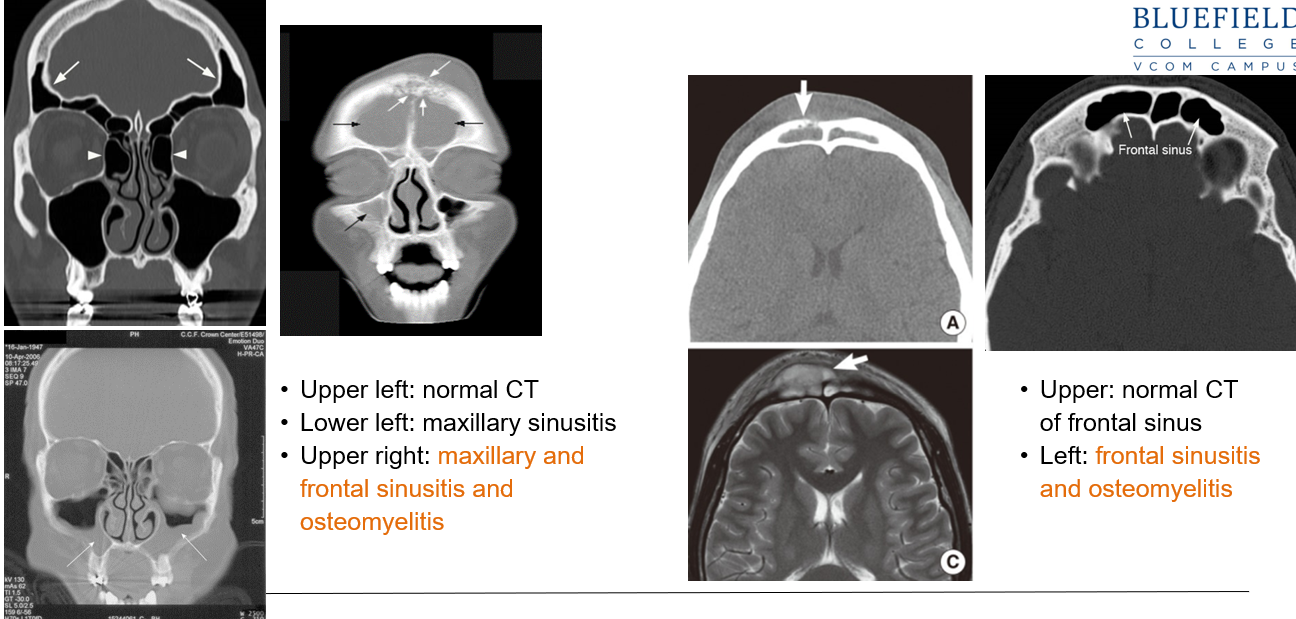
WWhich sinus is the most affected sinus?
Maxillary. Trapped fluid in the sinuses, especially the maxillary sinus, can lead to secondary sinus infections.
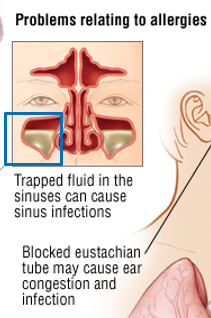
What are some complications of allergic rhinitis?
Trapped fluid in the sinuses, especially the maxillary sinus, can lead to secondary sinus infections.
Inflammation from allergic rhinitis can affect the lower airways, potentially leading to asthma.
Blocked Eustachian tubes may cause ear congestion and infections.
What are treatment options for allergic rhinitis?
Traditional: Weekly injections for 3-5 years to shift antibodies from IgE to IgG to desensitize the patient.
Sublingual: Self-administered drops under the tongue, effective for pollen, grass, and dust mites, promoting IgG4 and IgA production for tolerance.
What are Charcot-Leyden crystals?
Eosinophil-derived crystals found in severe eosinophilic inflammation, such as in chronic allergic rhinitis, asthma, and nasal polyps. They drive inflammation and may be reduced with antibody therapy.
Key feature of SEVERE asthma & chronic rhinitis w/nasal polyps
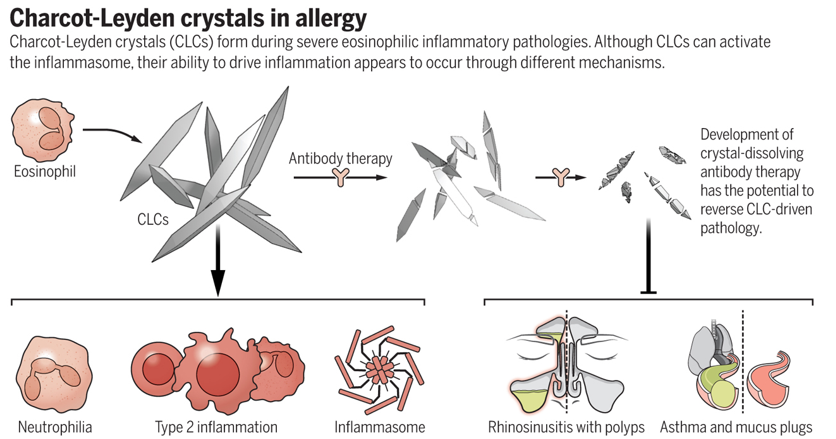
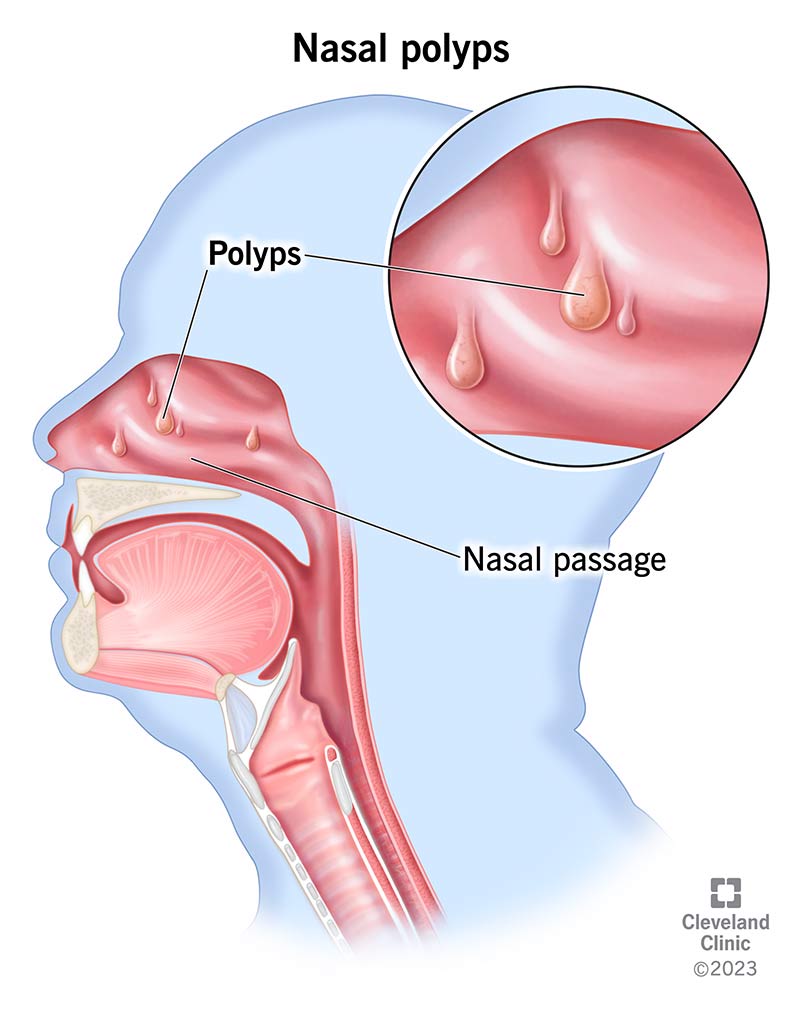
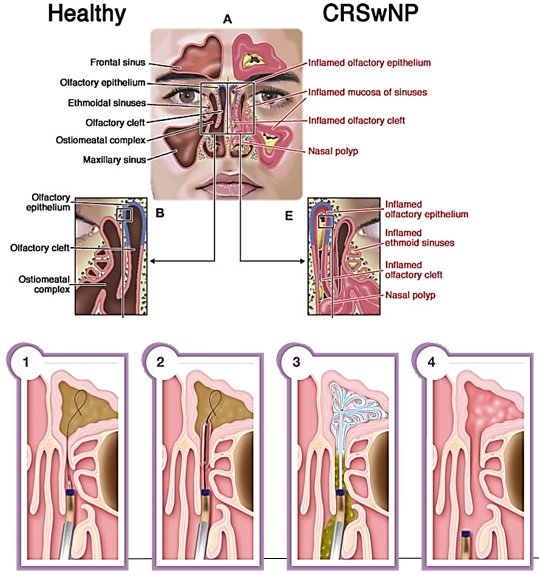
What are nasal polyps?
Chronic rhinitis may cause sufficient irritation to cause polyp formation. They are swollen mucosal tissue that form due to chronic rhinitis irritation.
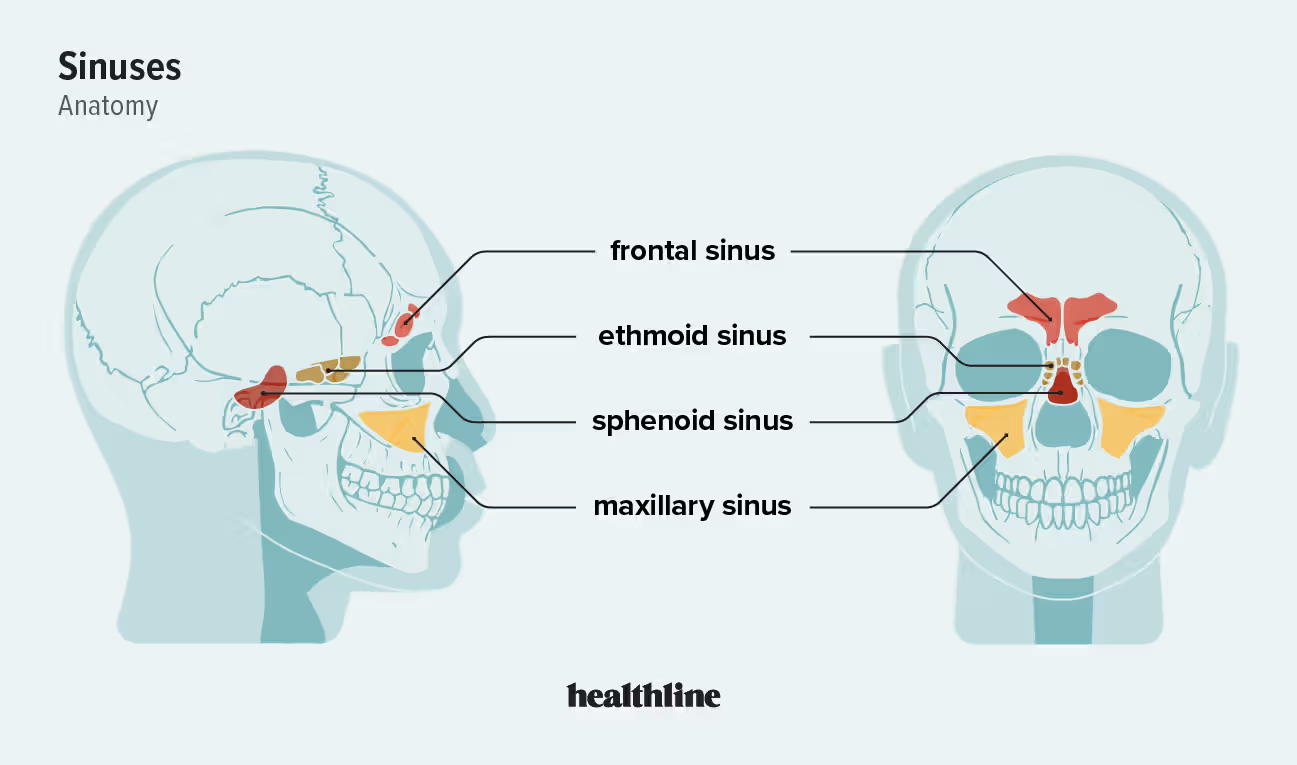
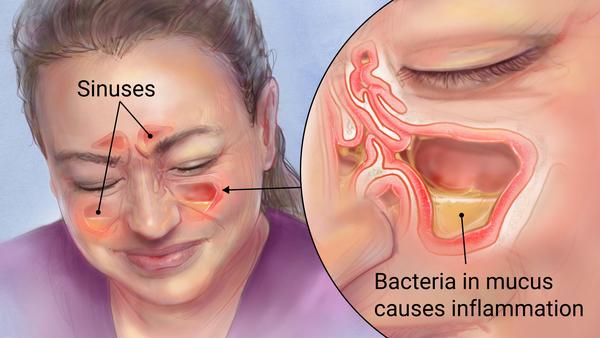
What is sinusitis?
Inflammation of paranasal sinuses
What are the two classes of sinusitis?
Acute (<4 weeks): Often follows a viral upper respiratory infection or allergies, leading to bacterial colonization (e.g., Streptococcus).
Chronic (>12 weeks): Due to allergies, environmental factors, or bacterial/fungal infections (e.g., Staphylococcus).
If someone has cheek pain, that mimics a “toothache”, where is that pain located?
Maxillary sinus
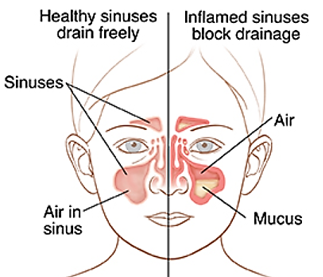
What is the pathogenesis of sinusitis?
The respiratory mucosa reacts to stimuli (e.g., virus) by producing mucus and attracting inflammatory mediators, leading to congestion, swelling, and blockage, which can encourage secondary bacterial growth.
How do you diagnose sinusitis?
Allergy tests
Exudate culture
CT scans
How do you treat sinusitis?
Acute
antihistamines, decongestants, analgesics
nasal irrigation (e.g., neti pot),
antibiotics if symptoms persist over 48 hours.
Chronic:
nasal irrigation
if necessary, surgical procedures like FESS (functional endoscopic sinus surgery) or balloon sinuplasty.
What is otitis media?
An ear infection or inflammation of the middle ear, the space behind the eardrum. It often occurs when the Eustachian tube, which connects the middle ear to the back of the throat, becomes blocked.

What causes otitis media?
This can happen due to allergies, colds, or respiratory infections, leading to fluid buildup in the Eustachian tube and creating an environment for bacteria or viruses to grow.
Which population is otitis media most common?
Children

How is otitis media treated?
Antibiotics; severe cases may need ear tubes for drainage.
What is tracheitis?
An infection or inflammation of the trachea, often caused by bacteria following a viral upper respiratory infection (e.g., S. aureus) or irritants like chlorine gas, sulfur dioxide, and smoke, which damage the tracheal lining.
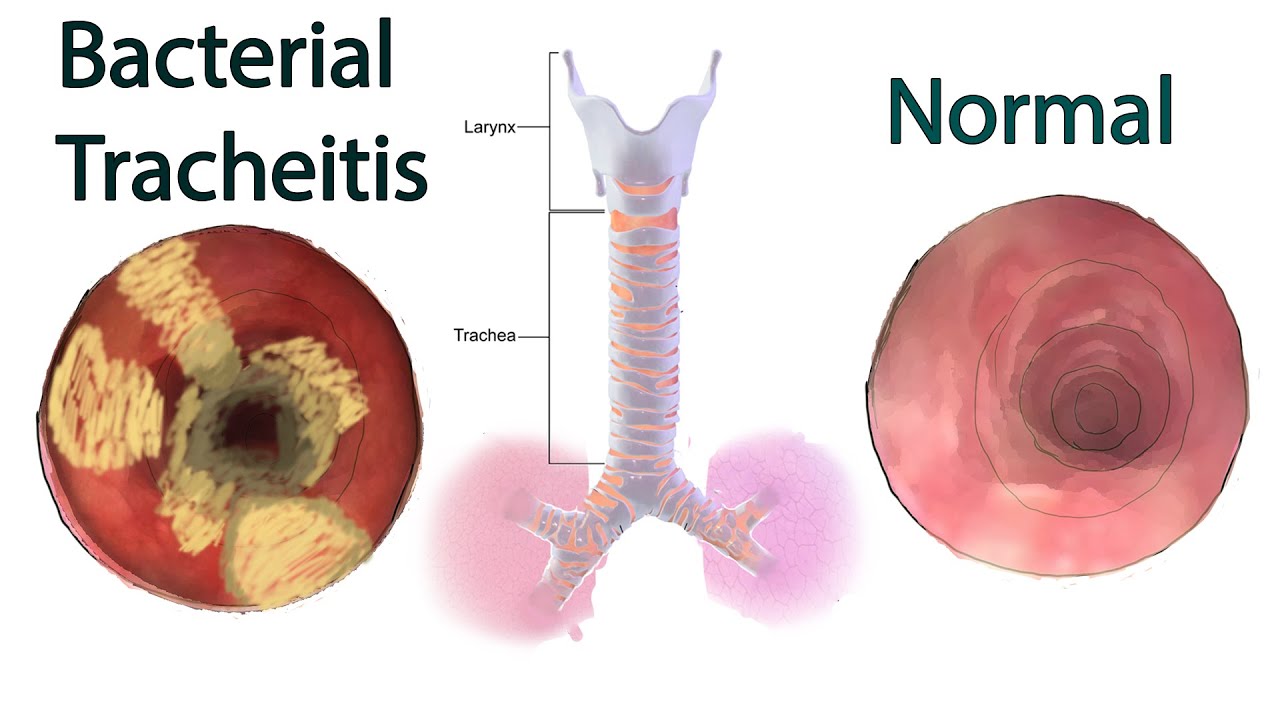
Who is tracheitis more dangerous for?
Dangerous for young children due to their smaller trachea, which can swell and block the airway.
What are the symptoms of tracheitis?
Deep cough, scratchy throat, fever
Inspiratory stridor (crowing sign during inhalation)
Chest pain, intercostal retractions
How is tracheitis diagnosed?
Measuring blood oxygen levels to assess breathing efficiency.
Taking chest radiographs to examine the trachea.
Performing a nasopharyngeal or tracheal culture to identify any bacterial infection.
What is asthma?
An immune-related disease that causes inflammation and mucus production in the small airways (bronchioles) and makes the airway muscles overly responsive, leading to airway obstruction.
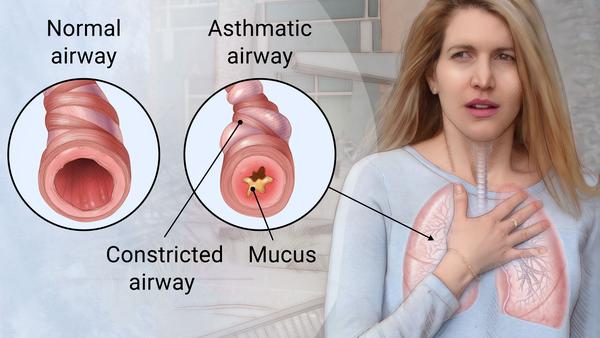
What causes asthma?
About 70% are triggered by allergens (IgE-mediated).—Type 1 HS response
About 30% are due to non-immune triggers like drugs, cold, or exercise.
What is the pathophysiology of asthma?
Sensitization: Initial allergen exposure activates T cells (Th2) and IgE production.
Early Stage: Re-exposure triggers mast cells, causing airway narrowing and mucus production.
Chronic Stage: Repeated inflammation leads to tissue damage, remodeling, fibrosis, and reduced airway elasticity.
What is hypersensitivity pneumonitis?
A type of allergic reaction that causes inflammation in the lungs.
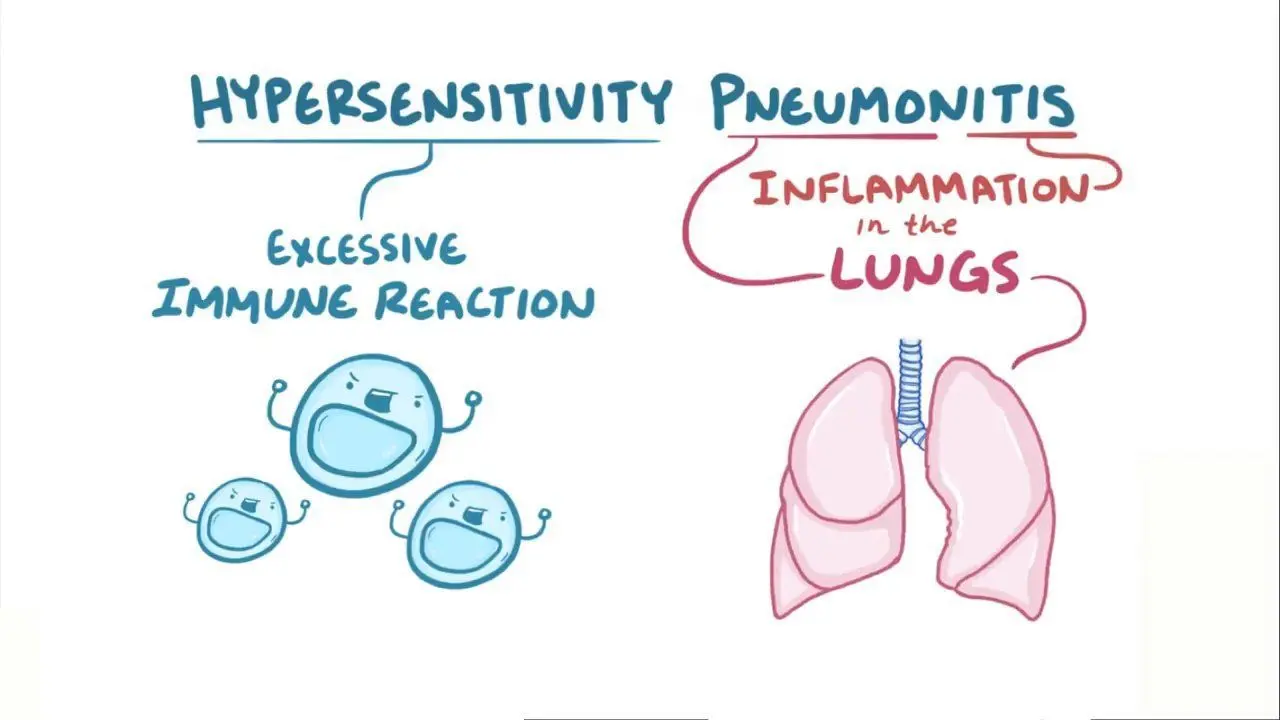
What are the key characteristics of hypersensitivity penumonitis?
Involves widespread inflammation in the bronchioles, driven by T cells, triggered by inhaling tiny particles (<3 µm).
What are the triggers of hypersensitivity
Often environmental or occupational
Smoking is not a risk factor and may actually reduce incidence and severity.
Explain the pathophysiology of hypersensitivity pneumonitis
Antigen inhalation activates immune cells (B cells and Th1 cells).
IgG and IgA antibodies bind antigens, forming immune complexes in the lung tissue.
Activates memory Th1 cells, CD8 T cells, and macrophages, leading to inflammation, granulomas, fibrosis, and eventually potential respiratory failure.
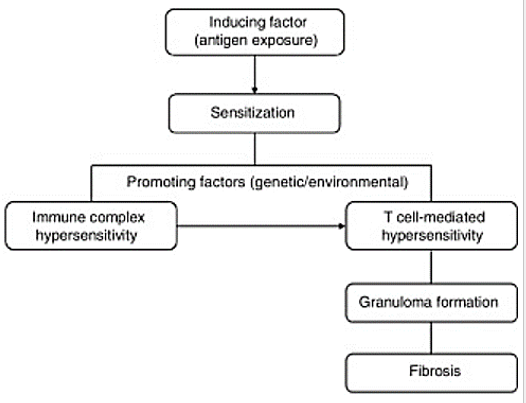
What type of hypersensitivity reaction is Hypersensitivity Pneumonitis?
Type 4 HS
Early hypersensitivity pneumonitis starts with immune complexes in the lungs (Type 3 hypersensitivity) and CD4 cytokines (Type 4 hypersensitivity). With repeated exposure, it becomes primarily T cell-driven (Type 4 hypersensitivity).
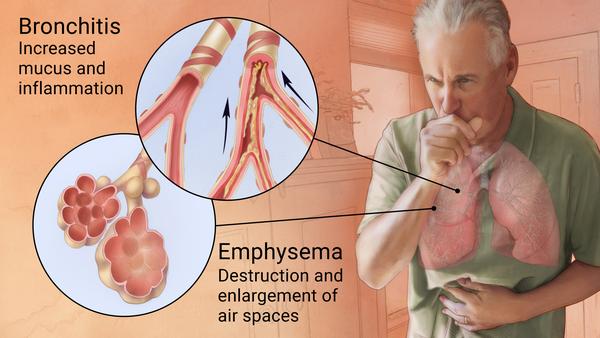
What is COPD?
a condition caused by damage to the airways or other parts of the lung. COPD includes conditions like chronic bronchitis and emphysema, which damage the lungs and restrict airflow.
What is the #1 risk factor of COPD?
Smoking
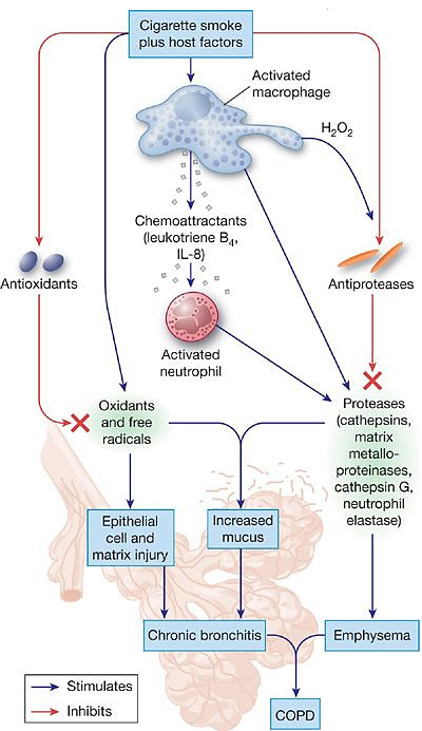
Explain the pathophysiology of COPD
Inhaling toxins (e.g., from smoking) triggers oxidative stress.
White blood cells (PMNs and macrophages) are activated, releasing enzymes that break down proteins.
Inflammation thickens the airway walls and increases mucus production.
Elastin (a protein in the lung tissue) is destroyed, causing the air sacs (alveoli) to lose structure.
Airways narrow, air sacs are damaged, and air exchange is impaired, making it difficult to breathe.