Ventilation/Perfusion and Regulation of Respiration
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
What does normal respiration depend on?
balance between air and blood flow in the lungs
hypoxia
general term the refers to low PO2 levels
hypoxemia
low blood O2 = low PaO2 (low partial pressure of O2 in arterial blood)
*usually defined as PaO2 < 85 mmHg
Under what partial pressure of oxygen is blood considered hypoxemic?
PaO2 below 85mmHg
What is hypercapnea defined as?
high CO2 in blood ==> increase in PaCO2 to greater than 45mmHg
What are the principal effects of hypercapnea?
affects the CNS ==> headache, confusion, memory loss, & coma
What is the normal alveolar ventilation (V) at rest?
4.2 L/min
What is the normal pulmonary blood flow (Q) at rest?
approx 5L/min
True or False: In an ideal lung, the ventilation/ perfusion (V/Q) would be the same
True ==> V/Q = 1 for all alveoli in ideal lung
What is the optimal ratio of gas flow & blood flow (V/Q) for oxygenation at rest?
0.84
*resting ventilation (V)/ resting pulmonary blood flow (Q)
V/Q = 4.2/5.0 = 0.84
What is the effect of using the minute ventilation to calculate V/Q instead of the alveolar ventilation?
V/Q for the lung as a whole = a little greater than 1
What does the ventilation/ pulmonary blood flow ratio allow for?
optimal gas exchange between lung & pulmonary capillaries
True or False: Lungs are ideal except for in cases of pulmonary pathology, like COPD.
False ==> lungs are normally non-ideal due to regional distributions of both ventilation & perfusion
*both ventilation & perfusion increases from the apex to the base of the lung but at equal rates in an upright human
Why is the intrapleural vacuum greater at the apex of the lung?
b/c of the tendency of the lungs to settle on the diaphragm & pull away from the apical chest wall --> distends the apical alveoli --> decreases their compliance --> difficult to distend further during inspiration
Why do basal alveoli receive more gas than apical alveoli during each inspiration?
basal alveoli are less distended & more compliant
What factors cause less ventilation and perfusion at the apex of the lung?
-intrapleural pressure more negative
-greater transmural pressure
-large alveoli
-lower intravascular pressure
-less blood flow
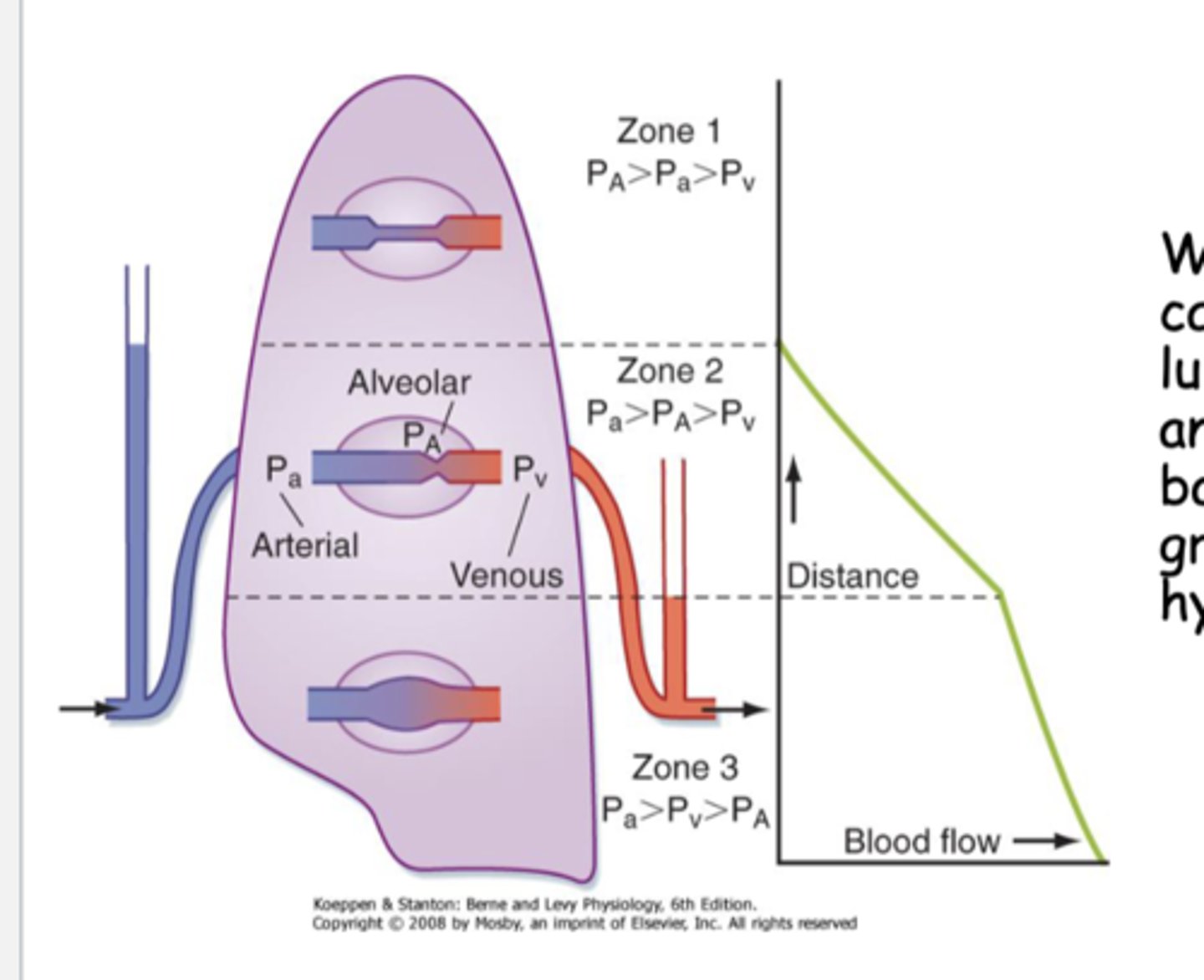
Why is the capillary perfusion pressure in the lungs the lowest in the apical region?
gravitational effects on hydrostatic pressure
True or False: The ventilation/perfusion ratio (V/Q) ratio matching is more uniform in the prone position (laying down).
True
True or False: Although both V and Q decrease from the base to the apex of the lung, their gradients are not equivalent
True
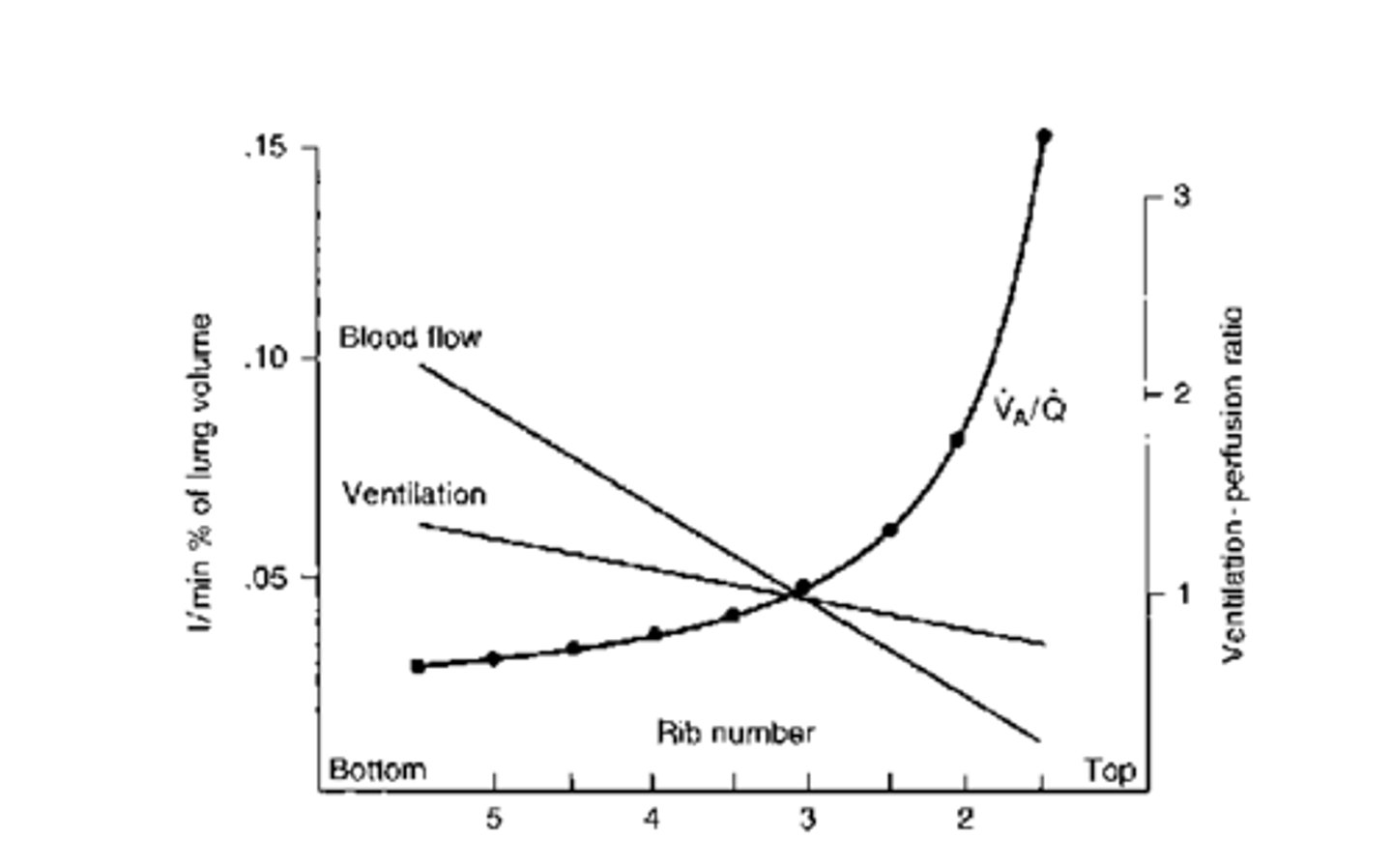
What is the ventilation/perfusion ratio (V/Q) at the top of the lung?
> 3
What is the ventilation/perfusion ratio (V/Q) at the base of the lung?
0.6
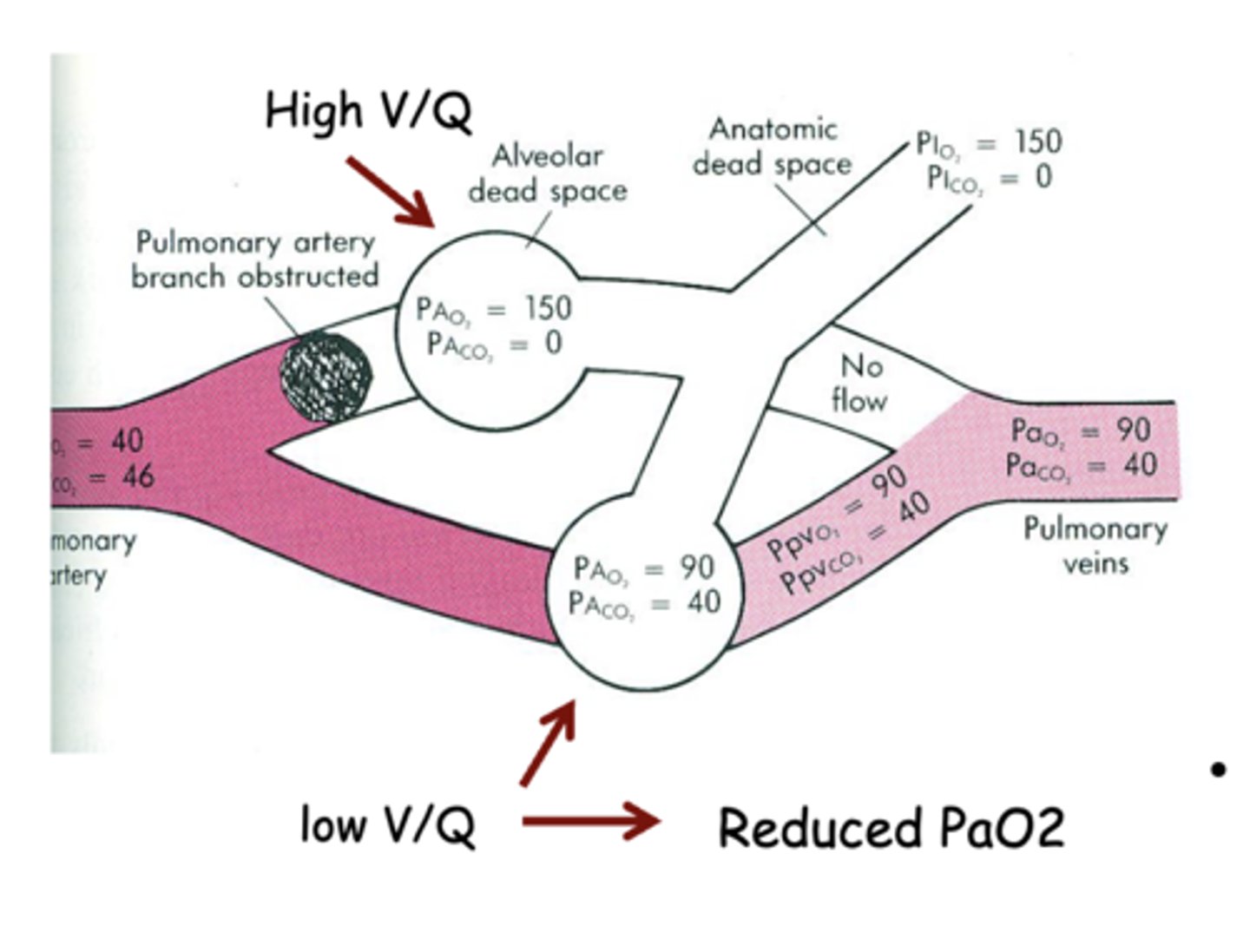
What effect will a partial blockage in pulmonary capillaries have on the ratio of ventilation/perfusion (V/Q)?
increases V/Q ==> inversely proportional to blood flow (b/c Q is in the denominator)
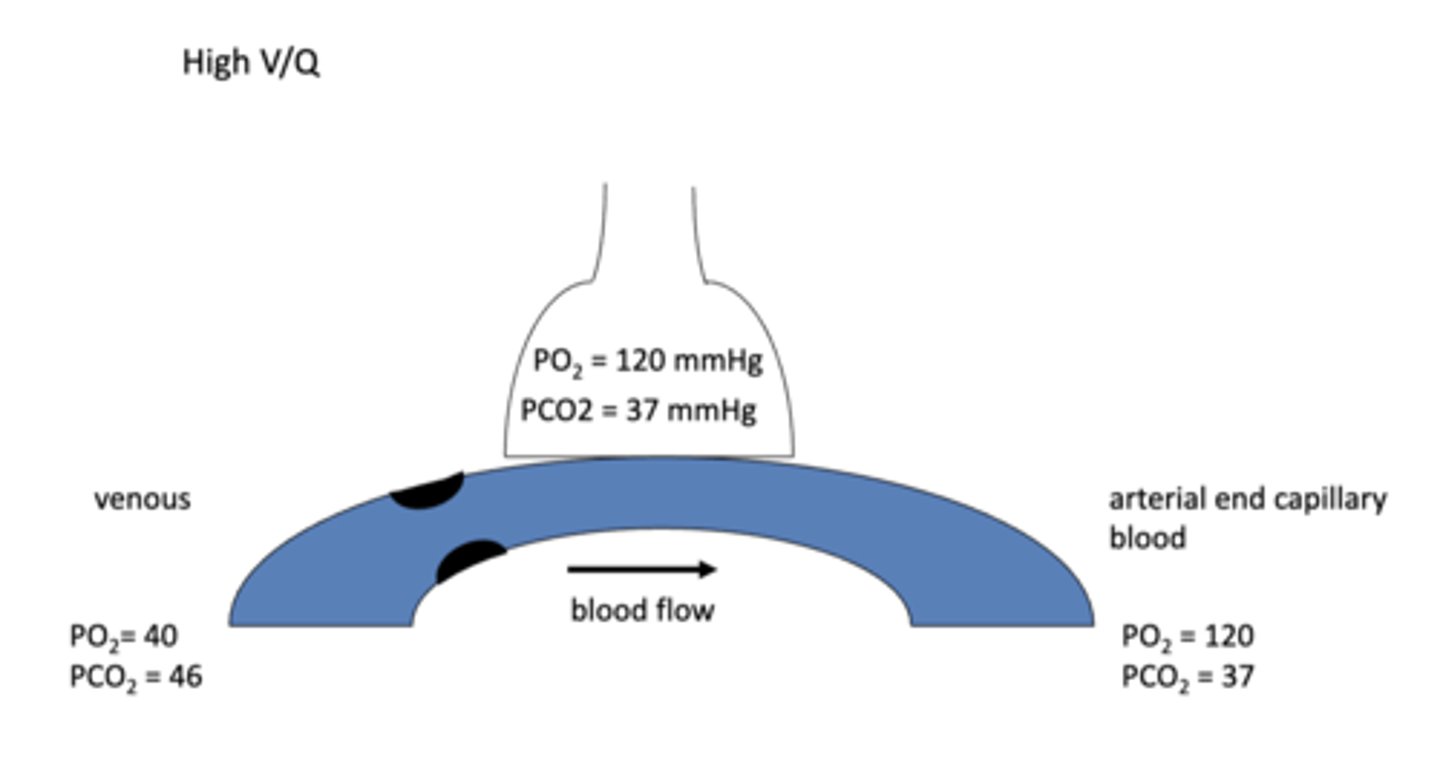
When the ventilation/perfusion ratio (V/Q) is high like in the case of partial blockage of blood flow in the pulmonary capillaries, what effect does this have on the partial pressures of O2 and CO2 in the alveoli and the pulmonary capillary blood at the arterial end?
increased PAO2 & decreased PACO2 ==> b/c not as much blood available for exchange so less exchange happens at the alveoli
*(PaO2 & PaCO2 at the arterial end of capillary will be the same as the PAO2 & PACO2 b./c the exchange bwtn alveoli & blood will always be 1:1)
When the ventilation/perfusion ratio (V/Q) is high like in the case of complete blockage of blood flow in the pulmonary capillaries, what effect does this have on the partial pressures of O2 and CO2 in the alveoli and the pulmonary capillary blood at the arterial end?
alveolar dead space = no gas exchange ==> O2 and CO2 in the alveoli will come in and go staright back out
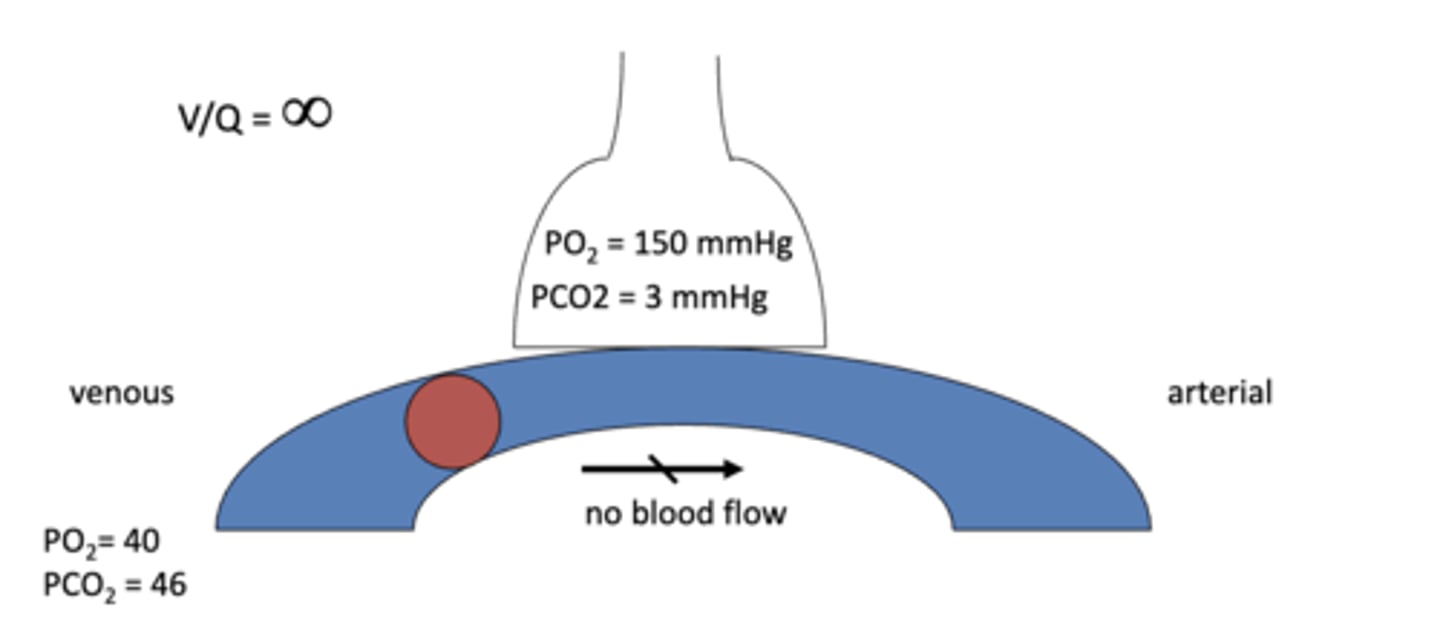
hypocapnic bronchoconstriction
alveoli w/ blocked perfusion (completely blocked = infinitely high V/Q) partially compensates by constricting bronchiole to decrease airflow to bring V/Q closer to 1
*aimed at bringing V/Q closer to normal by decreasing ventilation to zero too = V/Q = 0/0 =1
How is a region of high V/Q like in the case of a pulmonary blood flow blockage compensated for?
-hypocapnic bronchoconstriction --> constrict the bronchiole of the alveoli that isn't receiving blood flow to decrease ventilation to make it closer to zero (the value of blood flow due to the blockage)
-shunting of blood from blocked vessels to non-blocked vessels
What is the result of shunting blood from blocked pulmonary capillaries to non-blocked pulmonary capillaries in regions of high V/Q?
non-blocked vessels have increased blood flow --> have the capacity to take more O2 from alveoli during exchange & give away more CO2--> lower PAO2 & higher PACO2 --> blood leaving the alveoli is hypoxic & hypercapnic --> stimulates chemoreceptors to increase ventilation --> increases airflow to the alveoli to compensate for the increased blood flow
(remember that the partial pressures of blood leaving the alveoli are always going to be equal to the partial pressures within the alveoli regardless of the partial pressures in the blood leading up to the alv)
What does the extent of shunting blood from blocked pulmonary capillaries to non-blocked pulmonary capillaries in regions of high V/Q depend on?
number of alveoli affected by the loss of perfusion
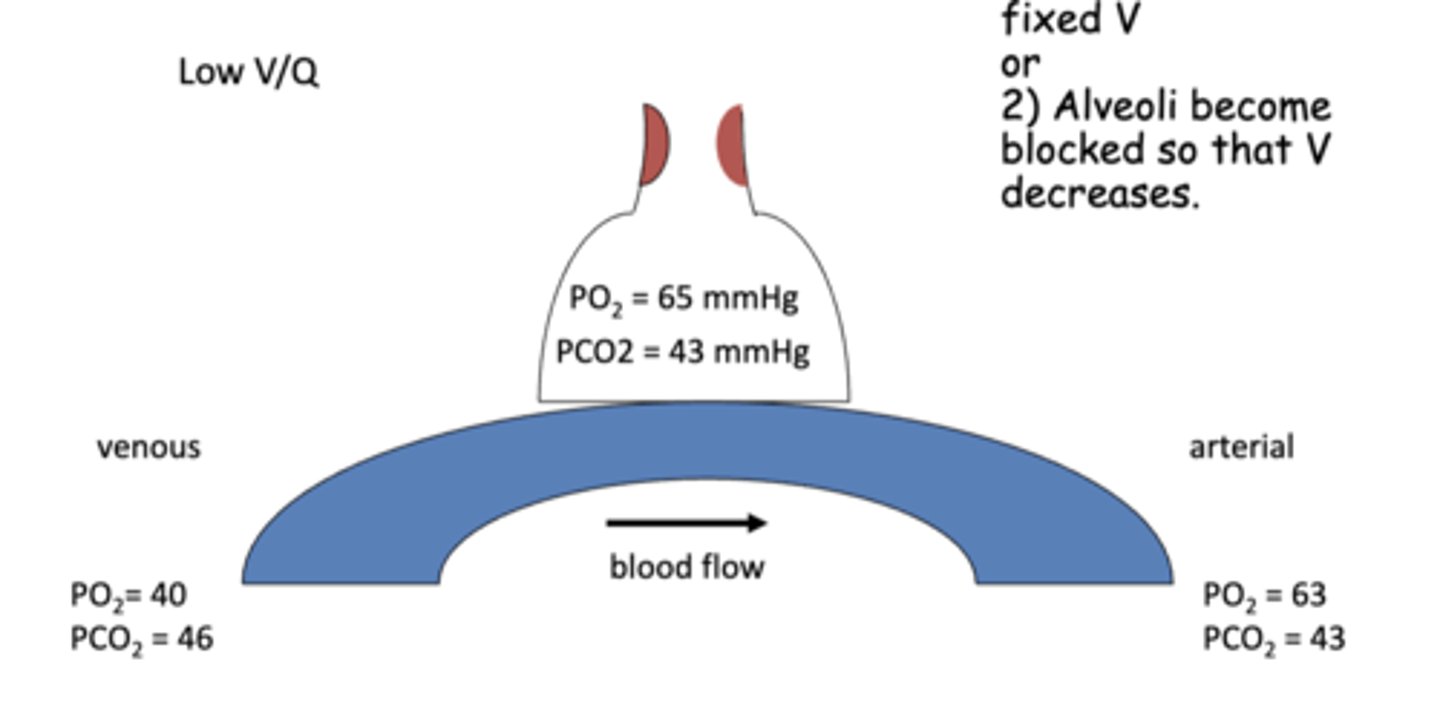
When does the ventilation/perfusion ratio (V/Q) decrease?
-when blood flow increases at a fixed ventilation
-when alveoli become blocked & ventilation decreases
When the ventilation/perfusion ratio (V/Q) is low like in the case of decreased ventilation due to partial blockage of alveoli, what effect does this have on the partial pressures of O2 and CO2 in the alveoli and the pulmonary capillary blood at the arterial end?
decreased exchange of air w/ the atmosphere (decreased airflow) --> drops PAO2 & increases PACO2 because less O2 able to enter & less CO2 able to be exhaled after gas exchange
*same changes reflected in the arterial end capillary
When the ventilation/perfusion ratio (V/Q) is low like in the case of decreased ventilation due to complete blockage of alveoli, what effect does this have on the partial pressures of O2 and CO2 in the alveoli and the pulmonary capillary blood at the arterial end?
blocked alveolus has the same PO2 & PCO2 as mixed venous blood ==> no exhange occurs b/c there's no ventilation (blood on the arterial capillary end does not pick up O2 nor eliminate CO2)
How is a low ventilation/perfusion ratio (V/Q), like in the case of blocked alveoli, compensated for?
hypoxic vasoconstriction of the pulmonary capillary occurs to re-route blood flow to unblocked alveoli --> V/Q in unblocked region that the blood is shunted to has a initial decrease of V/Q (b/c Q increased) --> rise in PaCO2 + drop in PaO2 (more blood than air in the region) --> chemoreceptors stimulate increased ventilation --> V/Q returns to normal (& so does partial pressures)

What diseases/conditions cause of low V/Q?
decreased ventilation due to decreased lung compliance or increase airway resistance
-mucus airway obstruction
-extreme broncho-constriction
-pulmonary edema
-pulmonary fibrosis
-prolonged anesthesia w/ atelectasis
What diseases/conditions cause high V/Q?
decreased blood flow due to impaired pulmonary circulation
-emphysema
-pulmonary embolism
-hemorrhage
-positive pressure ventilation
Why can positive pressure ventilation cause high V/Q?
too much air in alveoli crushed capillary surrounding the alveoli = decreased blood flow = decreased Q = increased V/Q
True or False: Emphysema patients have a low ventilation/ perfusion ration (V/Q)
False ==> emphysema impairs pulmonary blood flow so it causes an increase in V/Q (decreased Q = high V/Q)