2nd midterm
1/121
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
122 Terms
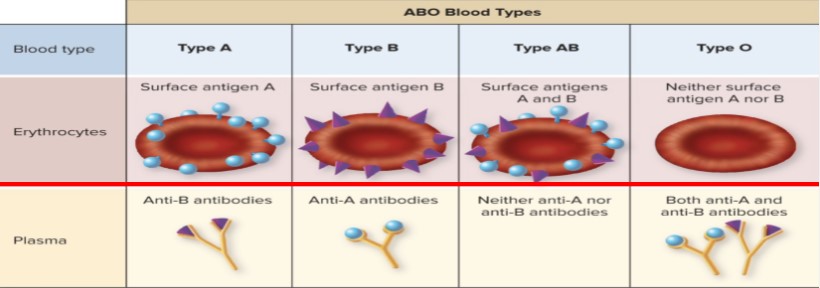
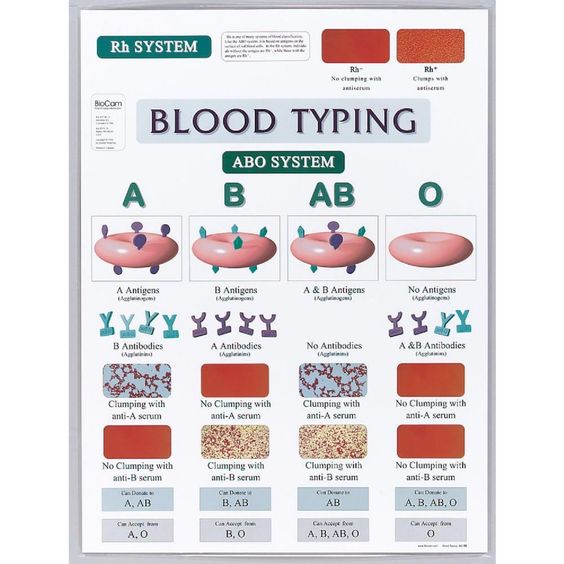
What are the different blood types according to the ABO blood typing system? What antigens/antibodies?
Type A
Antigen A
Anti-B antibodies
(+/-) if presence of antigen D
Type B
Antigen B
Anti-A antibodies
Type AB
Antigen A
Antigen B
no Antibodies
Type O
no Antigen
Anti-A antibodies
Anti-B antibodies
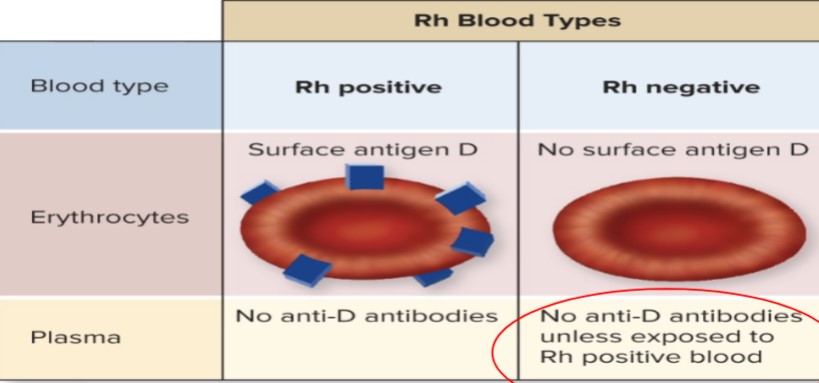
What is the Rh factor? What makes blood Rh positive?
Rh factor aka D antigen
Rh +
Antigen D
No anti-D antibodies
Rh -
no antigen D
no anti-D antibodies (unless exposed to Rh+ blood)
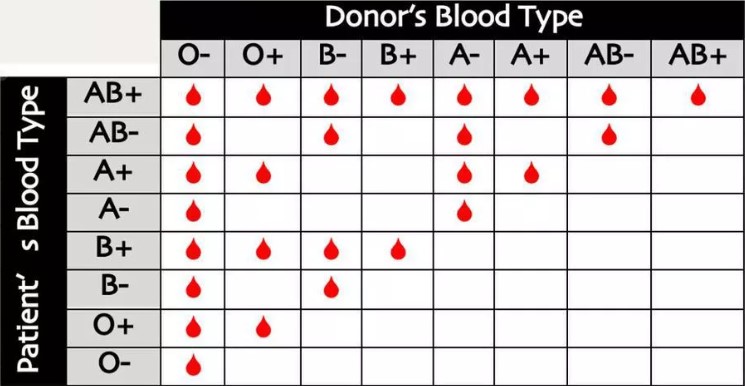
Complete a table of ABO blood types including its Rh factor. Add which can donate to whom and receive from whom safely.
BLOOD TYPE | CAN GIVE TO | CAN RECEIVE FROM |
A+ | A+, AB+ | A+, A-, O+, O- |
A- | A+, A-, AB+, AB- | A-, O- |
B+ | B+, AB+ | B+, B-, O+, O- |
B- | B+, B-, AB+, AB- | B-, O- |
AB+ | AB+ | EVERYONE |
AB- | AB+, AB- | AB-, A-, B-, O- |
O+ | O+, A+, B+ AB+ | O+, O- |
O- | EVERYONE | O- |
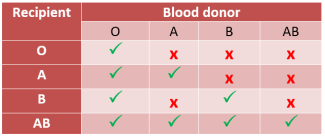
ABO blood type compatibility
O
receive blood from O
A
receive blood from O and A
B
receive blood from O and B
AB
receive blood from all
Rh blood type compatibility
+
can give to +
-
can give to + and -
Most common blood type
O+
Rarest blood type
AB-
Universal donor blood type
O-
Universal receiver blood type
AB+
What is erythroblastosis fetalis/hemolytic disease of the newborn? What is the typical scenario that can lead to this condition (Rh of mother, father and baby)?
When mother (Rh-) develops anti-D antibodies when exposed to baby’s blood (Rh+) which will attack the next baby (Rh+)
Father Rh+
Mother Rh-
Babies Rh+
Can we prevent erythroblastosis fetalis? If yes, how?
administration of exogenous Rh immune globulin to mother
@26-28 wks of pregnancy
within 72 hr of delivery
to prevent mother from developing anti-D antibodies
What is agglutination reaction?
RBC sticking together because of antigen-antibody binding
In a blood typing test, what anti-sera and blood type combination will result to clumping/agglutination? Give examples.
Type A
Anti-A serum clumping
no anti-b serum clumping
Type B
no anti-a serum clumping
Anti-B serum clumping
Type AB
Anti-A serum clumping
Anti-B serum clumping
Type O
no clumping
Rh+
clumping
Rh-
no clumping
What are the two main categories of WBCs? Categorize the WBCs, describe each in detail and draw them.
granulocytes (BEN)
basophils
eosinophils
neutrophils
agranulocytes (LM)
lymphocytes
smaller, round nuclei
monocytes
larger, kidney shaped nuclei
most and least common leukocytes
neutrophils = 40-70%
lymphocytes = 20-40%
basophils = 0-1%
Which WBC is phagocytic
monocytes
neutrophils
eosinophils
basophils
(aka all except lymphocytes)
Average WBC count
5,000-10,000/mm3
Neutrophils
55-75%
Lymphocytes
20-40%
Monocytes
3-8%
Eosinophils
2-4%
Basophils
0.5-1%
Meaning of CBC with diff
CBC = complete blood count of white cells in blood
CBC w/ diff = measure of each type of WBC
Define the following WBC response to inflammation terms: diapedesis, adhesion, phagocytosis, rolling, capture
Diapedesis
when WBC squeeze through tiny blood vessel walls to reach site of infection or injury
neutrophils + monocytes
Adhesion
WBC stick to the inner blood vessel walls near inflammation site, preparing to exit bloodstream
neutrophils + monocytes
Phagocytosis
WBC engulf and EAT harmful invaders like bacteria or debris to remove them from the body
neutrophils + monocytes
Rolling
WBC lightly stick to blood vessel walls and slowly move along to find best spot to exit
neutrophils + monocytes
Capture
WBC are temporarily caught by the blood vessel walls, helping them get ready to leave bloodstream and enter affected area
all WBC
explain diapedesis as a WBC response to inflammation
Diapedesis
when WBC squeeze through tiny blood vessel walls to reach site of infection or injury
neutrophils + monocytes
explain adhesion as a WBC response to inflammation
Adhesion
WBC stick to the inner blood vessel walls near inflammation site, preparing to exit bloodstream
neutrophils + monocytes
explain phagocytosis as a WBC response to inflammation
Phagocytosis
WBC engulf and EAT harmful invaders like bacteria or debris to remove them from the body
neutrophils + monocytes
explain rolling as a WBC response to inflammation
Rolling
WBC lightly stick to blood vessel walls and slowly move along to find best spot to exit
neutrophils + monocytes
explain capture as a WBC response to inflammation
Capture
WBC are temporarily caught by the blood vessel walls, helping them get ready to leave bloodstream and enter affected area
all WBC
What are the cardinal signs of inflammation?
Edema (tumor)
Redness (rubor)
Pain (dolor)
Heat (calor)
Loss of function
Where can you find lymphocytes? What are T cells? What are B cells? Differentiate between the two.
lymphocytes are found in thymus, lymph nodes and spleen
Thymus derived lymphocytes = T cells
Bone marrow derived lymphocytes = B cells
Function of neutrophils
help body fight off bacterial + fungal infections by phagocytosis
phagocytosis + release of enzymes and antimicrobial peptides
releases NETS (neutrophil extracellular traps)
apoptosis (programmed cell death)
What is antigen, antibody, epitope and immunity?
antigen
molecules that activate the immune system
antibody
recognize and combat harmful substances in body
epitope
spot on pathogen that antibodies bind to to make pathogen a target
immunity
body’s ability to defend itself against harmful invaders
What is the “lock and key” model of antibody structure?
lock = unique shape of antigen
key = identical shape of antibody’s antigen-binding site
Difference between B and T cells
B cells
humoral immunity
secretes antibody
develop into plasma cells
bacterial infections
types of destruction
phagocytic - antibodies coat bacterial cell
complement system - attachment of antibody to antigen
T cells
cell mediated immunity
doesn’t secrete antibody
must be close to victim cells to destroy
viruses, cancer cells, and cells of tissue transplants
3 types
Killer (Cytotoxic) T cells – kill victim cells
Helper T cells – promote the activity of killer T cells and B cells
Regulatory (suppressor) T cells – dampen immune responses
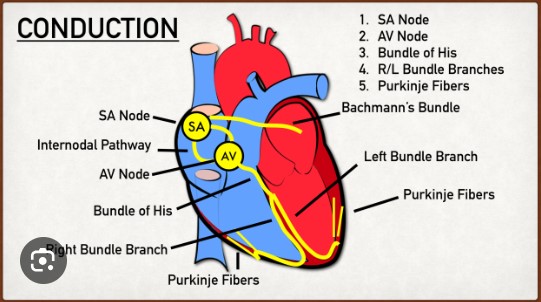
ECG stands for
electrocardiogram
What is an ECG? What does it show?
A recording of electrical events of the heart
Mainly records heart rate and rhythm to check for irregularity
What is the rationale behind ECG?
body fluids has high concentration of electrolytes. The electrical activity generated by heart travels throughout the body. This activity is then monitored by placing a pair of electrodes on different areas of the skin.
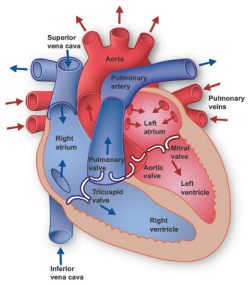
What are the basic concepts that are important to know about the heart?
The chambers
The valves
The great vessels
Oxygenated and deoxygenated blood
Systole and diastole
Pacemaker
Pulmonary and systemic circulation
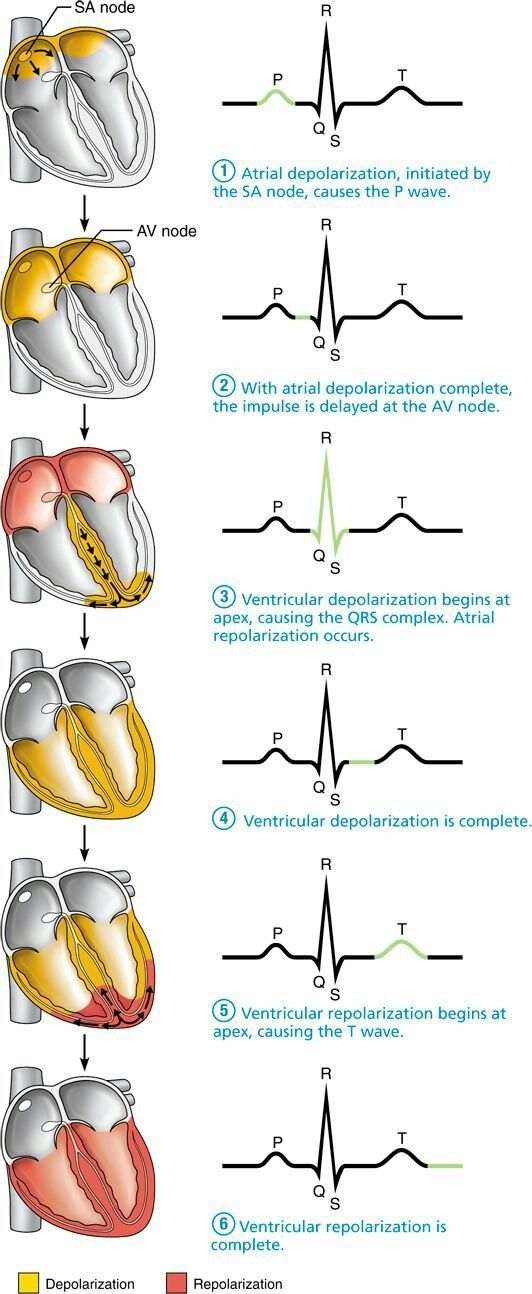
Define the cardiac cycle terms: systole, diastole, automaticity, rhythmicity
Systole- contraction phase
Depolarization → contraction → systole
Diastole- relaxation phase
Repolarization → relaxation → diastole
Automaticity - able to stimulate itself electrically in the absence of neural input (involuntary) (unlike skeletal muscle)
Rhythmicity- having a regular, repeated pattern
Intrinsic regulation of systole and diastole
Enumerate the different heart valves, their other names, shape, location in the heart.
Atrioventricular valves (AV valves)
Mitral (bicuspid) valve
Located between L atrium and L ventricle
Shape resembles mitre hat
Tricuspid valve
Located between R atrium and R ventricle
Semilunar valves (SL valves)
Aortic valve
Located between L ventricle and aorta
Pulmonary valve
Located between R ventricle and pulmonary artery
What is the normal pacemaker of the heart? Write down the steps in heart conduction.
Sinoatrial Node (SA node)
Wave of depolarization easily spread across the R and L atria
Steps of heart conduction
SA node fires →
Excitation spreads through atrial myocardium →
AV node fires →
Excitation spreads down AV bundle →
Purkinje fibers distribute excitation through ventricular myocardium
Compare and contrast systemic circulation and pulmonary circulation
Systemic circulation
Circulated oxygenated blood across the rest of the body
Pulmonary circulation
Moves blood between heart and lungs
Deoxygenated blood → lungs, oxygenated blood → heart
Pulmonary artery → lungs → pulmonary veins
How many limb leads are there in an ECG? How about how many unipolar leads? How many chest leads? How many leads all in all?
6 limb/bipolar leads
6 chest/unipolar leads V1-6
The ECG has different waves. What do these waves represent: P wave, QRS complex, T wave and U wave?
P wave → QRS complex → T wave → U wave
P wave
Atrial depolarization
QRS complex
Ventricular depolarization
T wave
Repolarization of the ventricles at the beginning of diastole
U wave
Incompletely understood
What information can be provided by an ECG?
HR
cardiac hypertrophy
necrosis
ischemia
other conditions that may produce abnormalities of electrical conduction
heart rhythm
How are heart sounds produced?
Contraction and relaxation of ventricles →
Pressure changes →
One-way heart valves will close →
Heart sound
Produced by closing valves
What is S1? How about S2? Which valves closes in S1 and in S2? Which one is the “lub”? Which one is the “dub”? Are they normal heartbeats or not?
S1 is the first heart sound, S2 is the second
S1 = Lub
Closure of AV valves (atrioventricular valves)
MV + TV
ventricle contracts/systole
S2 = Dub
Closure of SL valves (semilunar valves)
AV + PV
ventricles relax/diastole
These are the sounds of normal heartbeats
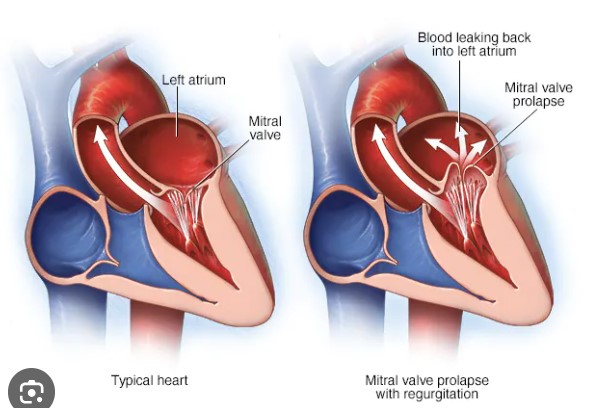
Give examples of abnormal heart beats?
Heart murmurs
Valve irregularity, septal defect, persistent fetal opening (foramen ovale) between the right and left atria after birth
Mitral valve prolapse
Most common cause of chronic mitral regurgitation, where blood flows backward into left atrium
Can be congenital or acquired, people may live without symptoms, and others may need mitral valve to be repaired or replaced
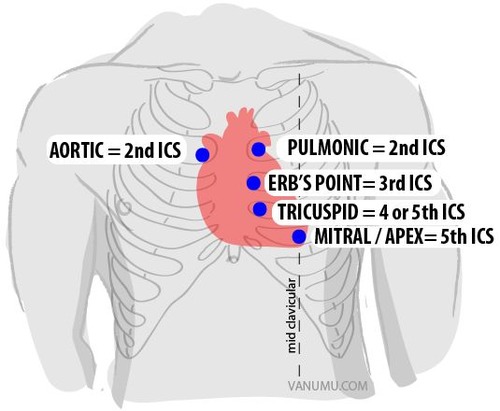
Where to place stethoscope for both heart sounds?
S1 Lub
Left 5th intercostal space, MCL
MCL = midclavicular line
S2 Dub
Right and left 2nd intercostal space (both sides)
Where to place stethoscope to best hear valves?
AV aortic valve
R 2nd ICS (near sternum)
PV pulmonary valve
L 2nd ICS (near sternum)
BV bicuspid valve
L 5th ICS
TV tricuspid valve
L 5th ICS MCL (midclavicular line)
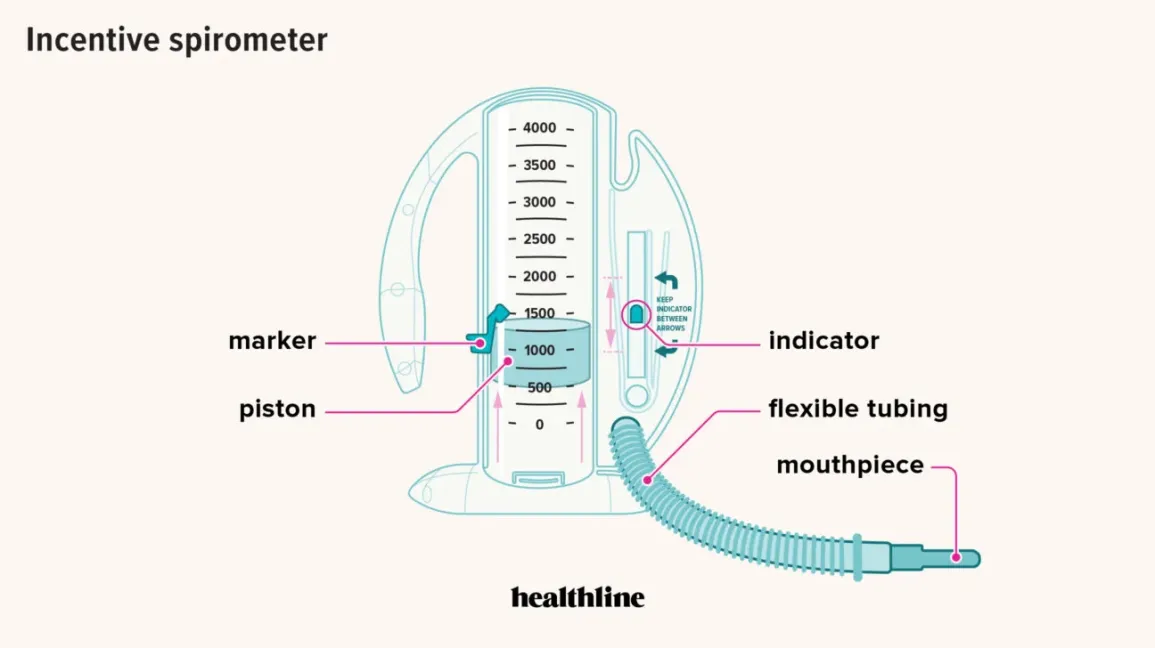
What is spirometry and what does it measure?
Spirometry or lung function test.
Measure:
– lung volumes and capacities
– ventilation as a function of time
– lung function or lung health
(lung, chest wall and respiratory muscles)
What are the parts of a spirometer?
Spirometer– is the apparatus
–volume indicator scale
–drum retainer
–floating bell
–water tank
– hose/tube
– single use mouthpiece
Enumerate the different volumes and capacities. Define each, state normal values (if discussed) and formulas.
(TV) Tidal Volume
–- represents the normal volume of air inspired and expired during each normal (unforced) ventilation cycle
Normal TV = 500 mL
(RV) Residual Volume
– volume of air REMAINING in the lungs after a maximum (forced) exhalation
Cannot be measured using expiration-only spirometers
RV = VC X age factor
(IRV) Inspiratory Reserve Volume
– MAXIMUM volume of air that can be FORCEFULLY inhaled after normally (unforced) inhalation
Cannot be measured using expiration-only spirometers
IRV = VC - ERV - TV
(ERV) Expiratory Reserve Volume
– is the MAXIMUM volume of gas that can be FORCEFULLY EXHALED after a normal exhalation
Normal ERV = 1,200 mL
(VC) Vital Capacity
–MAXIMUM volume of air that can be exhaled after maximum (forced) inhalation
Normal VC is based on GENDER , AGE and HEIGHT in cm
VC= IRV + TV= ERV
(IC) Inspiratory Capacity
– MAXIMUM volume of air that can be inhaled after normal (unforced) exhalation
(FRC) Functional Residual Capacity
– volume of air REMAINING in the lungs after a normal (unforced) exhalation
(TLC) Total Lung Capacity
– TOTAL VOLUME of air in the lungs after maximum inhalation
– Maximum volume of air the lungs can accommodate
– Sum of all volume compartments
Cannot be measured using expiration-only spirometers
TLC = VC X age factor
TLC = TV + IRV + ERV + RV
What is TV tidal volume and possible formulas
(TV) Tidal Volume
–- represents the normal volume of air inspired and expired during each normal (unforced) ventilation cycle
Normal TV = 500 mL
What is RV residual volume and possible formulas
(RV) Residual Volume
– volume of air REMAINING in the lungs after a maximum (forced) exhalation
Cannot be measured using expiration-only spirometers
RV = VC X age factor
What is IRV Inspiratory Reserve volume and possible formulas
(IRV) Inspiratory Reserve Volume
– MAXIMUM volume of air that can be FORCEFULLY inhaled after normally (unforced) inhalation
Cannot be measured using expiration-only spirometers
IRV = VC - ERV - TV
What is ERV Expiratory Reserve volume and possible formulas
(ERV) Expiratory Reserve Volume
– is the MAXIMUM volume of gas that can be FORCEFULLY EXHALED after a normal exhalation
Normal ERV = 1,200 mL
What is VC Vital Capacity and possible formulas
(VC) Vital Capacity
–MAXIMUM volume of air that can be exhaled after maximum (forced) inhalation
Normal VC is based on GENDER , AGE and HEIGHT in cm
VC= IRV + TV= ERV
What is IC Inspiratory Capacity and possible formulas
(IC) Inspiratory Capacity
– MAXIMUM volume of air that can be inhaled after normal (unforced) exhalation
What is FRC Functional Residual Capacity and possible formulas
(FRC) Functional Residual Capacity
– volume of air REMAINING in the lungs after a normal (unforced) exhalation
What is TLC Total Lung Capacity and possible formulas
(TLC) Total Lung Capacity
– TOTAL VOLUME of air in the lungs after maximum inhalation
– Maximum volume of air the lungs can accommodate
– Sum of all volume compartments
Cannot be measured using expiration-only spirometers
TLC = VC X age factor
TLC = TV + IRV + ERV + RV
Your lung volumes and capacities are considered normal If your score is
_______ of the predicted value?
Your lung volumes and capacities are considered normal If your score is
> 80 % of the predicted value?
What is Boyle’s Law? Apply Boyle’s Law during inhalation? How about during exhalation?
The PRESSURE of gas is INVERSELY PROPORTIONAL to its VOLUME
Inhalation:
thoracic cavity volume ↑
intrapulmonary pressure ↓ and air flows into the lungs
Exhalation:
thoracic cavity volume ↓
intrapulmonary pressure ↑ and air exits the lungs
What is the anatomic division of the respiratory system? What are the structures in each division?
ANATOMICALLY: divided into upper and lower respiratory tracts
upper respiratory tract
nasal cavity, pharynx, larynx
lower respiratory tract
trachea, bronchi, lungs
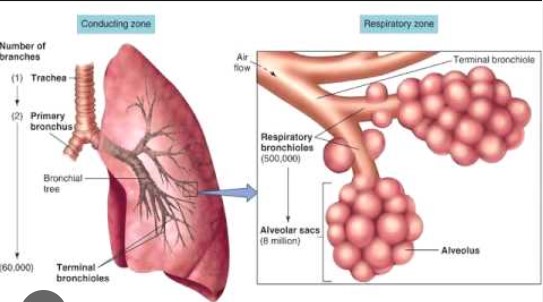
What is the functional division of the respiratory system? What are the structures in each division?
FUNCTIONALLY: divided into a conducting portion (where only air transport occurs) and a respiratory portion (where gas exchange occurs)
conducting zone
nasal cavity, pharynx, trachea, bronchi, bronchioles
respiratory zone
bronchioles, alveolar ducts and sacs, alveoli
Define pulmonary ventilation
Is the movement of air into and out of the respiratory system, inhalation/exhalation
Define gas exchange
External respiration exchanges gases between atmosphere —> blood (in the lungs)
Internal respiration exchanges gases between blood —> body’s cells
What are the two muscles of quiet breathing?
Skeletal muscles of QUIET BREATHING include diaphragm and external intercostals
– contraction → inhalation
– relaxation → exhalation
What are the volume changes in the thoracic cavity that occur during inhalation and exhalation?
During inhalation and exhalation, the thoracic cavity changes in ALL three dimensions
Vertical changes result from diaphragm movement
Lateral changes result from the rib cage elevation or depression
Anterior-posterior changes occur as the sternum moves anteriorly or posteriorly
What is blood pressure
The measurement of force applied to artery walls
What is the equation for blood pressure in relation to cardiac output, total peripheral resistance, heart rate and stroke volume?
BP = CO x TPR
CO = HR x SV
BP = blood pressure
CO = cardiac output
vol of blood pumped per min
TPR = total peripheral resistance
HR = heart rate, SV = stroke volume
Which artery do you auscultate when taking the blood pressure?
brachial artery
What is Korotkoff sound?
It is heard when there is turbulent blood flow through a constriction in the brachial artery
Compare and contrast laminar flow with turbulent flow when taking the blood pressure
Laminar (“layered”) flow–occurs when all parts of a fluid move in the same direction, parallel to the axis of the vessel.
Turbulent flow occurs when some parts of the fluid move in radial and circumferential directions, churning and mixing the blood.
Enumerate the instructions or questions you should ask/give your patient before taking his/her blood pressure?
Patient should relax for at least 5 minutes.
Smoking, exercise, drinking caffeinated and alcoholic drinks, full stomach,full bladder, extreme temperature–relax for at least 30 minutes.
Patient should sit with back straight and supported.
Feet flat on floor and uncrossed.
Remove excess clothing that might interfere BP cuff or constrict the arm.
*Pain can increase BP
*Use appropriate size BP cuff (pediatric BP cuff, adult and XL)
What is the importance of taking the palpatory BP first
The importance of taking the palpatory first is because it helps establish a baseline before using a blood pressure clift.
What is pulse pressure and its formula?
Pulse pressure is the “gap” between the highest and lowest blood pressure numbers.
Formula: Pulse Pressure = SBP-DBP
systolic bp - diastolic bp
What is mean arterial pressure and its formula?
The average pressure in a person’s arteries during one heartbeat.
Formula: MAP= ⅓ PULSE PRESSURE+DBP
What is hypertension?
May be indicated by chronically elevated blood pressure measurements
What are the two main categories of hypertension? Compare and contrast each category.
The two main categories of hypertension are Primary and Secondary Hypertension.
Primary hypertension is common and has no specific cause.
Secondary hypertension is less common and caused by a specific medical condition.
They both are conditions characterized by high blood pressure.
Blood pressure classification table in adults
Optimal
SBP = <120
DBP = <80
Normal
SBP = 120-129
DBP = 80-84
High normal
SBP = 130-139
DBP = 85-89
Grade 1 hypertension
SBP = 140-159
DBP = 90-99
Grade 2 hypertension
SBP = 160-179
DBP = 100-109
Grade 3 hypertension
SBP = >= 180
DBP = >= 110
Isolated systolic hypertension
SBP = >= 140
DBP = <90
What are the 3 body controls of acid-base balance?
lung
kidney
bicarbonate system
What is pH? What is the pH of pure water?
Concentration of hydrogen ions (H^+) in a solution
Pure water is 7 ( neutral solution)
What is a buffer? What is the major buffer of blood?
A solution that resists changes in pH when an acid or alkali is added to it.
To keep pH at a nearly constant value
bicarbonate
What is the normal blood pH?
7.35-7.45
What is an acid?
A molecule that can donate free H+ to a solution and LOWER its pH
What happens to our acid-base balance during hypoventilation + hyperventilation
Hypoventilation
→ CO2 is not all blown off
→ CO2 accumulates in the blood
→decrease in blood pH
→Respiratory acidosis
Hyperventilation
→ low CO2 levels in blood
→ Respiratory alkalosis
What happens to acid-base balance when we exercise?
Exercise Hyperpnea– deep breathing (+/- increase RR)
Does it produce respiratory alkalosis?
Does not produce respiratory alkalosis
Is matched with increased product CO2 during exercise
Think of situations where respiratory acidosis can happen? How about situations where respiratory alkalosis can happen?
Respiratory acidosis is a medical condition that occurs when the lungs are unable to remove enough carbon dioxide from the body, leading to an increase in blood acidity
hypoventilation
Respiratory alkalosis is a condition in which the blood pH becomes too high due to low levels of carbon dioxide
hyperventilation
What makes a blood type O?
absence of O antibody
absence of a and b antigen
none
absence of a and b antibody
presence of o antibody
absense of B antibody
absence of O antibody
absence of a and b antigen
none
absence of a and b antibody
presence of o antibody
absense of B antibody
The statement, "there are more people with Rh (-) blood than people with Rh (+) blood", is ____________________________________.
true
false
false
Which is responsible for programmed cell death or apoptosis?
neutrophils
all are correct
lymphocytes
monocytes
basophils
eosinophils
none
neutrophils
all are correct
lymphocytes
monocytes
basophils
eosinophils
none
In simple terms, what is the "lock and key" model of antibody structure?
the antibody is the key that will unlock the antigen in the bacteria
none
antibody must match antigen epitope in order to result in binding
antibody must open the lock of the antigen in order to result in untangling
the antibody is the key that will unlock the antigen in the bacteria
none
antibody must match antigen epitope in order to result in binding
antibody must open the lock of the antigen in order to result in untangling
There are two ways of bacterial destruction by B lymphocytes. Which way is described as destroying bacteria by coating it with antibodies to make it easier for neutrophils and tissue macrophages to phagocytize?
none
coating
antibody coating
phagocytic
complement system
none
coating
antibody coating
phagocytic
complement system
Which term refers to molecules that activate the immune system?
antigen
exposure
none
antibody
immunity
receptor protein
antigen
exposure
none
antibody
immunity
receptor protein
Which is mismatched with it's Latin term?
pain: dolor
edema: tumor
redness: dolor
none
heat: calor
pain: dolor
edema: tumor
redness: dolor
none
heat: calor
Which is a cardinal sign of inflammation?
heat
loss of function
pain
edema
redness
all
heat
loss of function
pain
edema
redness
all
Which is true about the B lymphocytes?
develop into plasma cells
secrete antibody
usually activated in bacterial infection
none
all are correct
responsible for humoral immunity
develop into plasma cells
secrete antibody
usually activated in bacterial infection
none
all are correct
responsible for humoral immunity
Which type of WBC is an agent of the immune system?
neutrophils
lymphocytes
none
all are correct
monocytes
eosinophils
basophils
neutrophils
lymphocytes
none
all are correct
monocytes
eosinophils
basophils
Where can you find lymphocytes?
lymph nodes
none
spleen
thymus
all are correct
lymph nodes
none
spleen
thymus
all are correct
How many leads did you use in our in-class lab activity on ECG?
12
9
3
6
none
3
Which is true about ECG?
none
the rationale behind ECG is —- body fluids has high concentration of electrolytes. The electrical activity generated by heart travels throughout the body. This activity is then monitored by placing a pair of electrodes on different areas of the skin.
all are true
it can show a + or - abnormal pattern in the heart rhythm
it stands for electrocardiogram
it is the recording of electrical events of the heart
none
the rationale behind ECG is —- body fluids has high concentration of electrolytes. The electrical activity generated by heart travels throughout the body. This activity is then monitored by placing a pair of electrodes on different areas of the skin.
all are true
it can show a + or - abnormal pattern in the heart rhythm
it stands for electrocardiogram
it is the recording of electrical events of the heart
Which of the following is mismatched?
U wave: incompletely misunderstood
QRS complex: ventricular depolarization
all are mismatched
P wave: atrial depolarization
none
T wave: depolarization of the ventricles at the beginning of diastole
U wave: incompletely misunderstood
QRS complex: ventricular depolarization
all are mismatched
P wave: atrial depolarization
none
T wave: depolarization of the ventricles at the beginning of diastole
Which information can be provided by ECG?
HR
cardiac hypertrophy
necrosis
ischemia
other conditions that may produce abnormalities of electrical conduction
heart rhythm
none
all are correct
HR
cardiac hypertrophy
necrosis
ischemia
other conditions that may produce abnormalities of electrical conduction
heart rhythm
none
all are correct