Anxiety disorders PTSD
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
90 Terms
EUSTRESS
BENEFICIAL STRESS; MOTIVATES PEOPLE
DISTRESS
CAUSES EMOTIONAL AND PHYSICAL PROBLEMS; COULD RESULT IN DEPRESSION, CONFUSION, HOPELESSNESS/HELPLESSNESS, FATIGUE, ETC
Stress response
fight or flight
survival mechanism
Neurobiology
LIMBIC SYSTEM: “EMOTIONAL BRAIN”; MADE UP OF
AMYGDALA, HIPPOCAMPUS, THALAMUS, HYPOTHALAMUS,
BASAL GANGLIA, AND CINGULATE GYRUS
• THREE FUNCTIONS:
• 1. SCAN ENVIRONMENT FOR THREAT
• 2. INITIATE BODY’S READINESS BY ELICITING FIGHT-OR-
FLIGHT RESPONSE
• 3. TERMINATE REACTIVITY AFTER STRESSOR SUBSIDES TO
RESTORE HOMEOSTASIS
Neurotransmitters involved in Anxiety
SEROTONIN: THOUGHT TO BE DECREASED IN ANXIETY
DISORDERS; SSRIS OFTEN CONSIDERED A FIRST-LINE
PHARMACOLOGIC INTERVENTION
• NOREPINEPHRINE: INCREASES WHEN PERSON FEELS
THREATENED AND CAN CAUSE HYPERAROUSAL; MEDS
LIKE PROPRANOLOL CAN BLOCK THIS ACTIVITY
• GABA: INHIBITORY NEUROTRANSMITTER; SLOWS
NEUROTRANSMISSION, WHICH HAS A CALMING EFFECT
Prolonged Stress
BODY REMAINS IN “HIGH ALERT,” AND CORTISOL AND
ADRENALINE STAY IN BODY, WHICH CAN HAVE NEGATIVE
EFFECTS ON THE BODY
Anxiety
APPREHENSION OR UNEASINESS FROM A REAL
OR PERCEIVED THREAT WHERE THE SOURCE IS
UNKNOWN/UNRECOGNIZED
Fear
fight or flight response to a specefic danger
Normal anxiety
healthy, productive
acute anxiety
loss or threat to sense of security; an expected response
Pathological
maladaptive-greater in duration, intensity and impact on persons functioning
DEFENSE MECHANISMS
(FREUD)
MEANS OF MANAGING CONFLICT AND AFFECT
• USUALLY UNCONSCIOUS
• DISCRETE FROM ONE ANOTHER
• MAY SIGNIFY PSYCHIATRIC ILLNESSES, BUT ARE
REVERSIBLE
• ADAPTIVE AS WELL AS PATHOLOGICAL
• TYPICALLY, FREQUENCY, DURATION, AND INTENSITY
DICTATE WHETHER USE IS ADAPTIVE OR MALADAPTIVE
examples of defense mechanism
ALTRUISM
• SUBLIMATION
• HUMOR
• SUPPRESSION
• REPRESSION
• DISPLACEMENT
• REACTION FORMATION
• SOMATIZATION
• UNDOING
• RATIONALIZATION
• PASSIVE AGGRESSION
• ACTING-OUT
• DISSOCIATION
• DEVALUATION
• IDEALIZATION
• SPLITTING
• PROJECTION
• DENIAL
SUBLIMATION
is a defense mechanism involving the channeling of unacceptable impulses into socially acceptable behaviors or activities, allowing for personal growth and expression.
REACTION FORMATION
is a defense mechanism that involves converting unacceptable feelings or impulses into their opposites, often leading to exaggerated behaviors that reflect those opposite feelings.
UNDOING
is a defense mechanism that involves attempting to reverse or negate a thought, feeling, or action that one finds distressing, often through acts of kindness or reparative behavior.
devaluation
is a defense mechanism where a person attributes exaggeratedly negative qualities to self or others, reducing their perceived value, often to cope with feelings of insecurity or inadequacy.
suppression
is a defense mechanism involving consciously pushing distressing thoughts, feelings, or memories out of awareness, aiming to reduce anxiety and promote emotional stability.
repression
is a defense mechanism that involves unconsciously blocking distressing thoughts, feelings, or memories from awareness, often to protect oneself from emotional pain.
Rationalization
is a defense mechanism that involves offering reasonable explanations for behaviors or actions that are otherwise anxiety-provoking, often to avoid facing uncomfortable feelings or realities.
THEORIES REGARDING ANXIETY
LEARNING THEORIES: ANXIETY IS A LEARNED RESPONSE;
E.G., WE LEARN TO BE FEARFUL BASED ON HOW WE SEE OTHERS RESPOND TO A THREAT
THUS, WE CAN LEARN NOT TO BE FEARFUL IN SITUATIONS THROUGH GRADUAL EXPOSURE
COGNITIVE THEORIES: ANXIETY DISORDERS RESULT
FROM DISTORTIONS IN THINKING AND PERCEPTION
REFRAMING THINKING CAN LITERALLY CHANGE BRAIN
CHEMISTRY
Levels of Anxiety
Mild:
Moderate
Severe
Panic
Mild Anxiety Signs and symptoms
Can be seen in normal functioning. ABLE TO
SEE/HEAR/GRASP MORE INFORMATION, PROBLEM SOLVING MORE EFFECTIVE
Moderate levels of anxiety
LESS THAN OPTIMAL ABILITY TO LEARN AND
PROBLEM-SOLVE; MAY ONLY SEE/HEAR CERTAIN THINGS IN
THE ENVIRONMENT. POSSIBLY STILL ABLE TO BE
CONSTRUCTIVE
Severe Anxiety Signs and symptoms
PERCEPTUAL FIELD GREATLY REDUCED; LEARNING
AND PROBLEM-SOLVING NOT POSSIBLE
Panic Signs and Symptoms
Most severe; unable to process environment and may lose touch with reality
Mild to Moderate Anxiety Interventions
Employ open-ended questions, give braod openings and seek clairification
•Restricting topics and talking about irrelevant topics can increase the patient’s anxiety
•Stay calm! Be willing to listen
Severe to panic level anxiety interventions
•unable to problem solve, behaviors may be unproductive; regression is common
•Firm, short and simple statements most effective
Theories Regarding Anxiety
Learning theories: anxiety is a learned response; e.g., we learn to be fearful based on how we see others respond to a threat
Thus, we can learn not to be fearful in situations through gradual exposure
Cognitive theories: anxiety disorders result from distortions in thinking and perception
Reframing thinking can literally change brain chemistry
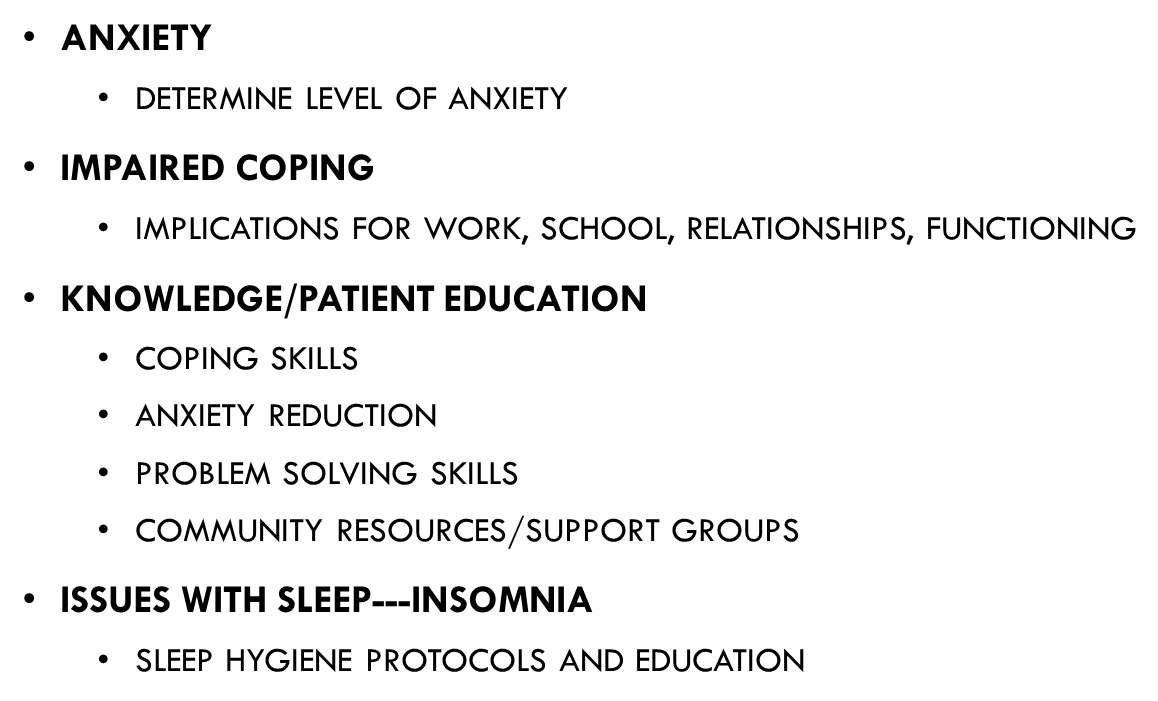
Common Patient Problem
•Anxiety
•Determine level of anxiety
•Impaired coping
•Implications for work, school, relationships, functioning
•Knowledge/patient education
•Coping skills
•Anxiety reduction
•Problem solving skills
•Community resources/support groups
•Issues with sleep---insomnia
•Sleep hygiene protocols and education
Four Cardinal Symptoms of PTSD
Intrusive reexperiencing of the initial trauma
avoidance
Persistent negative alterations in cognitions and mood
alteration and arousal activity
Intrusive reexperiencing of the initial trauma (ptsd sign 1)
•(flashbacks, nightmares, unwanted memories that are distressing, and feelings of unreality
Avoidance (PTSD Sign 2)
Avoidance (avoid memories and feelings as well as places or people that remind person of event)
Persistent negative alterations in cognitions and mood (PTSD Sign 3)
(feelings of detachment, cognitive distortions about themselves or others)
Alteration and arousal activity (PTSD 4)
(irritability, anger outbursts, self-destructive behavior, hypervigilance, exaggerated startle response, sleep disturbances)
PTSD Nursing Interventions
•Nursing problem: Posttrauma Syndrome
•assess for SI/HI, anxiety level, substance use
•assess that physical symptoms are not due to physical cause (dizziness, headaches, etc.)
•avoid minimizing trauma
•teach cognitive and behavioral techniques to manage symptoms of emotional or physical reactivity
•
PTSD GOALS/OUTCOMES of treatment
•Patient and others (family, friends) will feel safe
•Patient will receive treatment for co-occurring conditions (e.g. substance abuse, depression, anxiety)
•Patient will attend support groups
•Patient will expand social support
•Patient will experience increase in restful sleep with fewer nightmares and flashbacks
•Patient will express decreased irritability
•Patient will effectively demonstrate anxiety reduction techniques
Acute Stress Disorder
Can occur after same types of events as those that trigger PTSD
Difference is that symptom resolution occurs within a month
May require short-term medications to manage symptoms of anxiety and insomnia
Difference between Acute Stress Disorder and PTSD
Acute Stress resolve within a month
Secondary Stress/Compassion Fatigue
Differs from burnout, which is related to emotional distress and withdrawal as a result of increased workload and occupational stressors
Secondary traumatic stress and compassion fatigue are used interchangeably-emotional effect that nurses and other health care workers experience as a result of being indirectly traumatized through attempting to help those who have experienced trauma
Symptoms of compassion fatigue
Feeling overwhelmed, exhausted physically and mentally
Unable to function effectively
Intrusive thoughts
Difficulty separating self from work
Pessimism, short temper
Feelings of dread
Depression
Inability to effectively use coping mechanisms
Social withdrawal
Sleep issues
Decreased self-esteem
Hopelessness
Self-doubt; questioning one’s competence
Those of high risk of secondary trauma/compassion fatigue
Hospice care
Pediatrics
Emergency departments
Oncology
Forensic nursing
Psychiatric nurses
Social workers
anxiety disorders
• Can be a symptom of a medical condition, or can mimic a physical ailment
Anxiety is an expected reaction to threatening situations
•Everyone experiences occasional distress
•Problematic when interferes with adaptive behavior, causes physical symptoms, or exceeds what is tolerable to individual
•Causes dysfunction at work and in social settings, and impacts relationships
Separation Anxiety Disorder
Developmentally inappropriate level of concern about being away from a significant other
Typically diagnosed before age 18 after a month of symptoms, but adults can have/develop too
Creates relationship strain
The most common anxiety disorder in children
The fear, anxiety, or avoidance is persistent, lasting at least 4 weeks in children and adolescents and typically 6 months or more in adults.
Separation anxiety: Nursing interventions
•Identify and acknowledge specific fears
•Desensitization
•Medications (SSRIs, Benzodiazepines) in early stages
Panic Disorders
Panic attack is key feature of panic disorders
Sudden onset of extreme apprehension or fear; feelings of impending doom
Occur suddenly, often without warning, and last generally 1-30 minutes
Can happen day or night
Perceptual field limited, normal function not possible, misinterpretation of reality
Physical symptoms: palpitations, chest pain, diaphoresis, muscle tension, urinary frequency, hyperventilation, breathing difficulties, nauseas, feelings of choking, chills, hot flashes, and GI symptoms
•At least one of the attacks has been followed by 1 month (or more) of one or both of the following:
•Persistent concern or worry about additional panic attacks or their consequences (e.g., losing control, having a heart attack, “going crazy”).
•A significant maladaptive change in behavior related to the attacks (e.g., behaviors designed to avoid having panic attacks, such as avoidance of exercise or unfamiliar situations).
Nursing Interventions for Panic Attack
Provide a Safe, calm environment
reassure the patient and listen actively
encourage patient to talk about feelings and concerns
use reframing techniques
Identify negative self-talk
refer to the appropriate services
administer meds
Having a panic attack?
5 things you can see
4 things you can touch
3 things you can hear
2 things you can smell
1 thing you can taste
Phobias
Persistent, intense, irrational fear of a specific object, activity, or situation
Leads to desired or actual avoidance
Specific phobias: e.g., spiders, heights, storms, blood, closed spaces-very common
Behavioral therapy, rather than meds, is most effective for specific phobias
typically last for 6 months or more
Which therapy is most effective for phobias?
behavioral therapy is most effective for phobias.
common phobias
Clinical Name | Feared Object or Situation |
Acrophobia | Heights |
Agoraphobia | Open spaces |
Astraphobia | Electrical storms |
Claustrophobia | Closed spaces |
Glossophobia | Talking |
Hematophobia | Blood |
Hydrophobia | Water |
Monophobia | Being alone |
Mysophobia | Germs or dirt |
Nyctophobia | Darkness |
Pyrophobia | Fire |
Xenophobia | Strangers |
Zoophobia | Animals |
Social Anxiety Disorders(Social Phobias)
Anxiety or fear provoked by exposure to social situation or performance situation
Fear of humiliation or embarrassment
Deals with fear of being evaluated or rejected by others
Fear of public speaking: most common
Treatment of Social Anxiety Disorders (social phobias)
Treatment: Propranolol (reduces physiological symptoms, but not cognitive)
For more pervasive cases, SSRIs and MAOIs, CBT
Agoraphobia
Excessive anxiety about or fear of being in places or situations where help is not available, or where escape is difficult or embarrassing
DSM 5 diagnosis made when person experiences fear or anxiety in two situations
•Avoidance can be debilitating and impact quality of life-work, family, etc.
Nursing Interventions for Social Anxiety and Agoraphobia
Again, identify faulty thought patterns/distortions
Systematic desensitization
Flooding (implosion therapy)-not always appropriate
Behavior therapy
General Anxiety Disorder (GAD)
Chronic, associated with severe distress
Pervasive difficulties in cognition and functioning
Often see poor health-related outcomes
Characterized by excessive, persistent, and uncontrollable anxiety, as well as excessive worrying
At least three of the following are present: restlessness, fatigue, poor concentration, irritability, muscle tension, and sleep disturbance.
Most occur for the better part for 6 months
GAD treatment
Treatment: SSRIs, SNRIs, Buspirone, CBT
Nursing Interventions For GAD
Encourage discussion about feelings/concerns
Ask clarification questions
Help patient identify thoughts/feelings that occur before onset of worry
Encourage problem solving
Role play/model
Explore behaviors that have been effective in the past
Identify cognitive distortions
Diagnostic Criteria GAD
At least three of the following are present:
restlessness,
fatigue,
poor concentration,
irritability,
muscle tension, and
sleep disturbance.
Most occur for the better part for 6 months
Anxiety due to Medical Conditions
•Direct physiological result of a medical condition
•Respiratory: asthma, hypoxia, pulmonary edema, COPD, pulmonary embolism
•Cardiovascular: cardiac dysrhythmias such as torsades de pointes, angina, CHF, mitral valve prolapse, HTN
•Endocrine: hyperthyroidism, hypoglycemia, hypercortisolism, pheochromocytoma
•Neurological: Parkinson’s disease, akathisia, postconcussion syndrome, complex partial seizures
•Metabolic: hypercalcemia, hyperkalemia, hyponatremia, porphyria
Obsessive-compulsive and Related Disorders
Obsessive-compulsive disorder (OCD): thought to be related to hyperactivity in the prefrontal cortex and dysfunction in basal ganglia and cingulum
Dysregulation of Serotonin
Obsessions: thoughts, impulses, or images that persist to an extent that they cannot be ignored by person experiencing them
Compulsions: ritualistic behaviors that a person feels compelled to perform in order to reduce anxiety
Almost always occur together, as in OCD diagnosis
Obsessions
thoughts, impulses, or images that persist to an extent that they cannot be ignored by person experiencing them
Compulsions
Ritualistic behaviors that a person feels compelled to perform in order to reduce anxiety
Nursing Interventions (OCD)
Teach techniques that can distract and distance PT self from thoughts
Gradually assist patient in reducing time spent in ritualistic behaviors
•Cognitive restructuring
•Relaxation techniques
•Modeling techniques
•Behavior therapy
Body Dysmorphic Disorder
Sometimes have minor physical defects, but usually have a normal appearance
Preoccupation with imagined “defective” body part
Obsessive thinking about this; resulting compulsions (excessive grooming, picking, etc.)
Impairs social, academic, or occupational functioning
Body Dysmorphic Disorder treatment
Treatment: SSRIs, clomipramine (tricyclic), and CBT
Second generation antipsychotic added to SSRI may help in severe cases (if more delusional)
Hoarding
•Excessive collecting of items that are essentially worthless (but wealthy people may hoard more expensive items)
•Often feel shame related to behavior
•Impacts relationships with family and friends, as people may hoard so much that they isolate
•Compulsive hoarding does not meet criteria for OCD
Nursing Interventions for Hoarding Disorder
Assist in decision-making and categorizing
Cognitive restructuring
Behavioral exposure
Habituation to discarding
Medications may be helpful for anxiety and depression
Difficult to treat due to resistance to treatment, lack of insight, etc.
Trichotillomania Disorder and Excoriation Disorder
Trichotillomania (hair pulling)
Excoriation (skin picking)
Result in varying levels of disability, stigma, and altered appearance
People often try to hide activity
SSRIs most common form of treatment; with excoriation, may involve dermatologist as well (with psychiatric professionals)
Most common form of treatment for trichotillomania, or excoriation
•SSRIs most common form of treatment; with excoriation, may involve dermatologist as well (with psychiatric professionals)
Pharmacological Interventions for Anxiety
Benzos: short term
Buspirone
SNRIs(venlafaxine)
Tricyclin Antidepressants
MAOIs(recently used in ppl with sad)
Blood pressure Meds (Beta Blockers, alpha agonist)
Antihistamines (Hydroxyzine/Vistaril)
Combo meds:travil
Venlafaxine is the only FDA approved
SNRI for Panic disorder, GAD and SAD
Tricyclic Antidepressants are
2nd or 3rd line for anxiete
Treatment for PTSD
Meds-SSRIs, Clonidine, Prazosin
CBT
EMDR
Acupuncture, animals, yoga, etc.
CPT
Methylphenidate?
Treatment for Panic Disorders
CBT
SSRIs(Fluoxetine, sertraline, escitalopram)
Tricyclics(amitriptyline, noritriptyline)
MAOS( Phenelzine, tranylcypramine)
Benzodiazepines(Alprazolam, clonazepam, lorezepam) SHORT TERM
Special consideration for Benzos
Only short term treatment of anxiety
Benzos to know
Valium/Diazepam
Ativan/Lorazepam
Klonopin/Clonazepam
Nursing Implications of Benzo
Promote activity of GABA
Sedative/hypnotic effects
Risk for tolerance/withdrawal
Risk for respiratory depression, coma, and death (especially in combination with other sedating medications)
Affects motor ability and judgment (risk for falls, impaired driving, etc.)
Medication/substance interactions (muscle relaxants, alcohol, allergy medications)
BENZODIAZEPINE WITHDRAWL SYMPTOMS
Possible symptoms:
Headache
Sweating
Dizziness
Shakiness/tremor
Nausea
Sleep disturbances
Anxiety
Poor concentration
Palpitations
Perceptual disturbances
Seizures (greatest risk)
SSRIs for anxiety (Panic, SAD, GAD)
fluozetine
sertraline
paroxetine
Nursing Implications: SSRIs
uSSRIs inhibit reuptake of serotonin, increasing availability at the synapse
uCan actually result in anxiety
uOther side effects: sexual dysfunction, insomnia, GI disturbance, dizziness, drowsiness, increased risk for bleeding, SUICIDAL IDEATION!!
uPossibility of serotonin toxicity (e.g., Serotonin Syndrome)-more common if co-administered with other medications that impact Serotonin, or those that inhibit the CYP450 enzyme (Ketoconazole)
Serotonin Symptons
Hyperactivity or restlessness
Tachycardia
Fever
Elevated BP
Altered mental status
Irrationality, mood swings
Seizures
Myoclonus, incoordination
Abdominal pain, diarrhea
Apnea
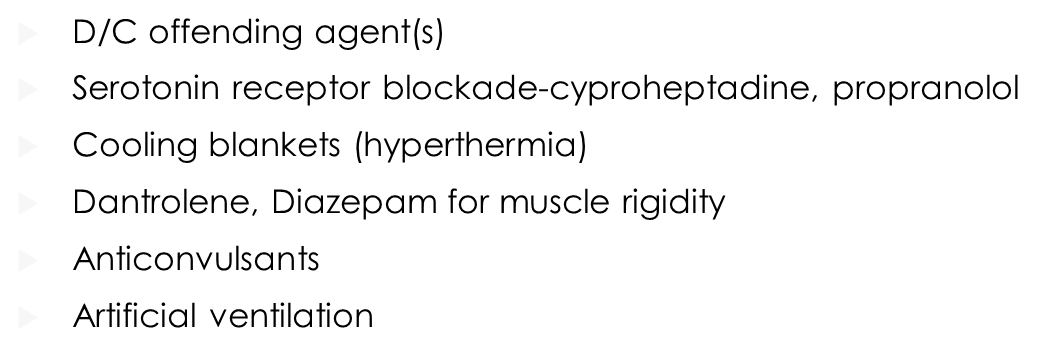
Serotonin Syndrome
uD/C offending agent(s)
uSerotonin receptor blockade-cyproheptadine, propranolol
uCooling blankets (hyperthermia)
uDantrolene, Diazepam for muscle rigidity
uAnticonvulsants
Artificial ventilation
Nursing Implications Tricyclics
uAnticholinergic effects (dry mouth, blurred vision, tachycardia, constipation, reflux, urinary retention)
uPostural hypotension: increased risk for falls
uSedating effects
uCardiovascular adverse effects: dysrhythmias, tachycardia, MI, and heart block
uRisk for lethal overdose
uPatient teaching important
Nursing implications: Beta Blockers
Nor risk for withdrawl, as with benzo
avoid use with alcohol
bradycardia, heart block, chf
Rare at lower anxiety doses
Dizziness, fatigue, hypotension
SJS
Buspar Side effects
EPS, Akathisia, nasuea, headache, fatigue, dizziness, drowsiness nausea
Buspar Nursing Implications
Non Habit-forming;no risk for dependance
less sedating, can drive/operate machinery more safely than with benzos
BUSPAR IS NOT IMMEDIATE ACTING, MAY TAKE UP 2-4 WEEKS TO FEEL THE FULL BENEFIT
Nursing Implications: Alpha Agonists ADVERSE Side Effects
Hypotension
Syncope
AV Block
Headaches
Dizziness
Somnolence
Anticholinergic effects
(dry mouth, blurred vision, tachycardia, constipation, reflux, urinary retention)
CAM for anxiety
Kava Kava: thought initially to elevate mood, well-being, contentment, and relaxation. Now, thought to increase psychiatric symptoms
Valerian: used for anxiety, but also for insomnia
Safe for most people when used on a short-term basis; however, can cause headaches, excitability, uneasiness, and insomnia (ironic)