regulation of urine
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
Where does ultrafiltration take place
In the nephrons’ renal capsule
What is ultrafiltration powered by
The high hydrostatic pressure from the blood coming through into the renal artery from the aorta then into the renal arteriole
How does blood enter the renal capsule
Through the afferent arteriol
How does the blood leave the renal capsule
Through the efferent arteriole
How does the afferent arteriole differ from the efferent arteriole and how does it aid ultrafiltration
The lumen of the efferent arteriole is much smaller than the afferent arteriole so causes a build up of hydrostatic pressure of the highly convoluted capillaries of the glomerulus inside the renal capsule
What are the three layers through which the glomerular filtrate passes through
endothelium of the capillary
The basement membrane
The epithelium cells of the capsule (podocytes)
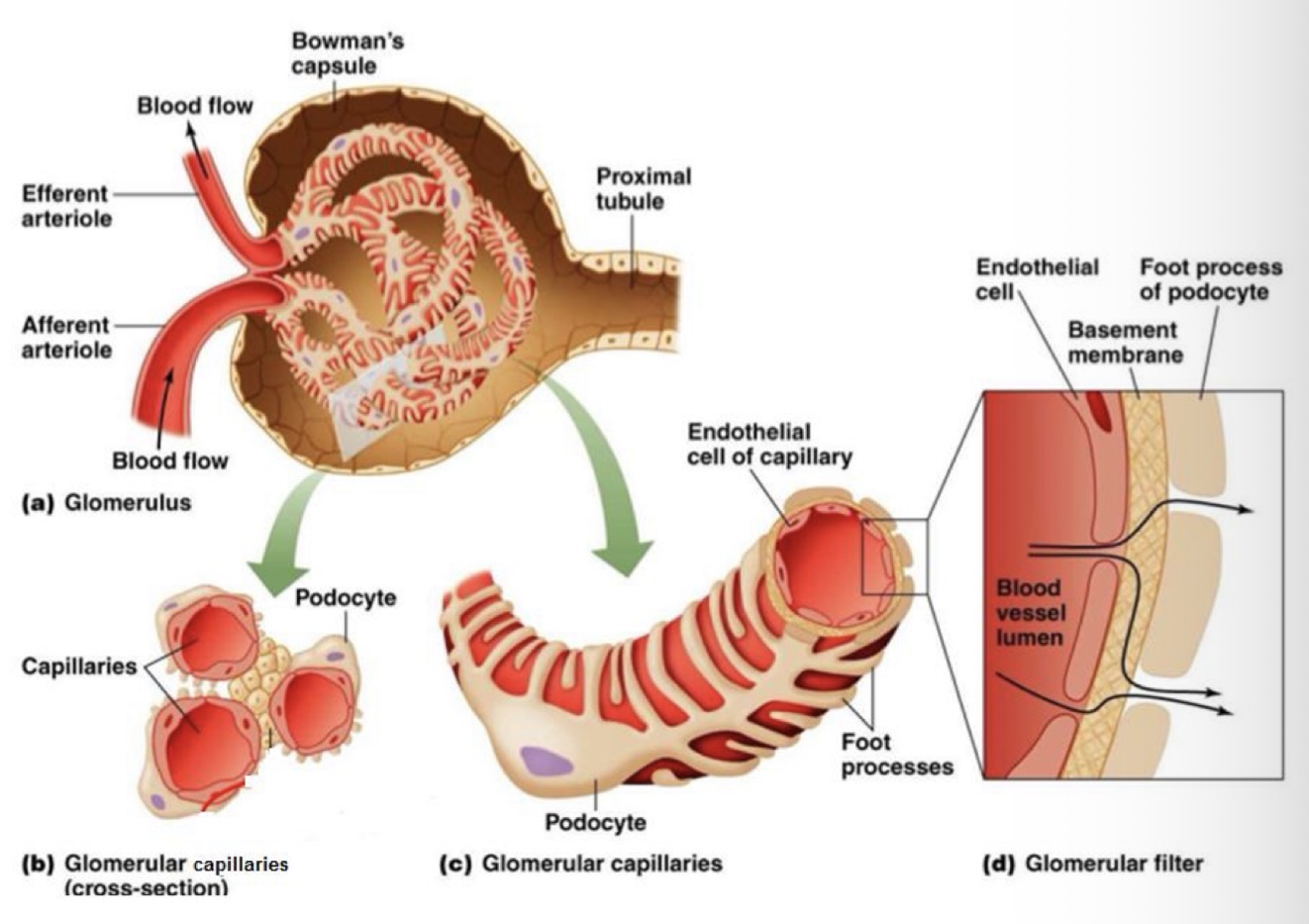
How is the endothelium of the capillary adapted for ultrafiltration of the blood
It has tiny pores (fenestrations) which are too small for cells and plasma proteins to leave the blood.
What is the role of the basement membrane
Acts as a filter
What is the limit of Mr for molecules to pass through the basement membrane
68000g/mol
What is the name of the cells that line the capsule wall
Podocytes
What is the role of podocytes and how are they adapted to their role
They have feet like extensions that form a network with tiny slits between them called filtration slits through which fluid can pass into the lumen of the renal capsule (the glomerular filtrate is very similar to blood plasma but with protein molecules missing)
What is the glomerular filtration rate
The rate at which fluid filters from the capillary to the renal capsule (125cm³/min)
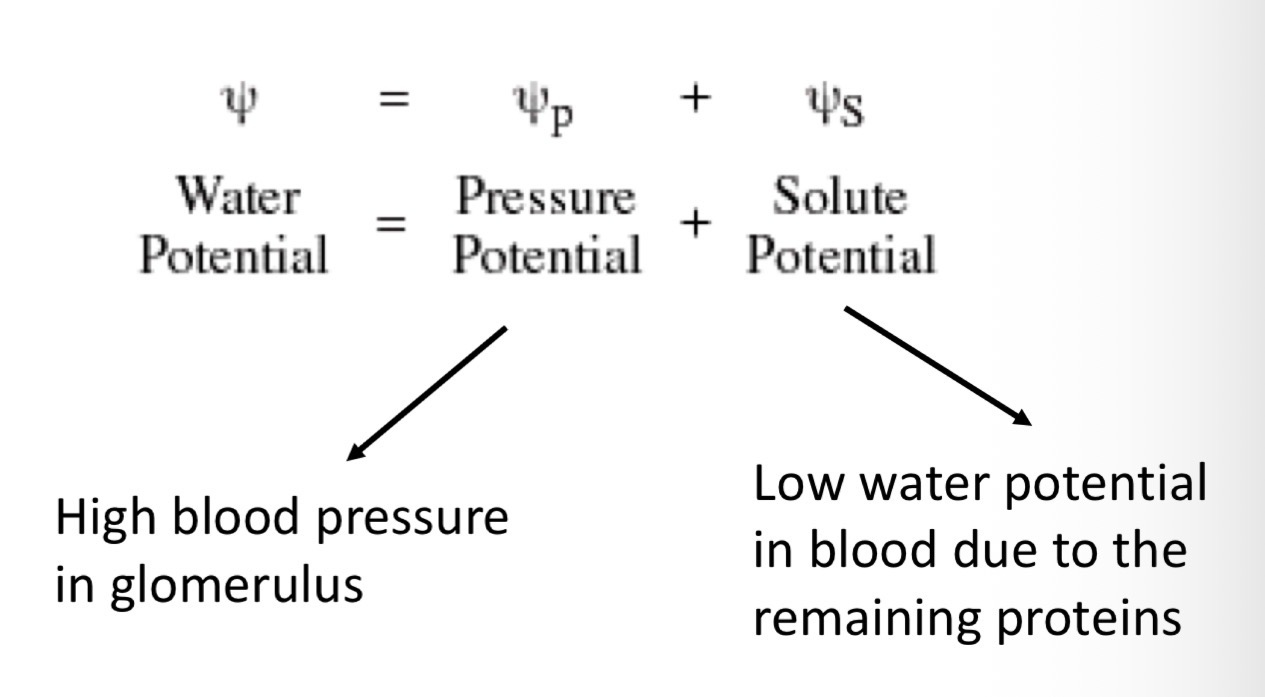
What is the glomerular filtration rate determined by
The difference in water potential between the plasma in the glomerular capillaries and filtrate in Bowman’s capsule
Overall the effect of pressure outweighs the effects of solute concentration so fluid continues to move out of capillary into capsule
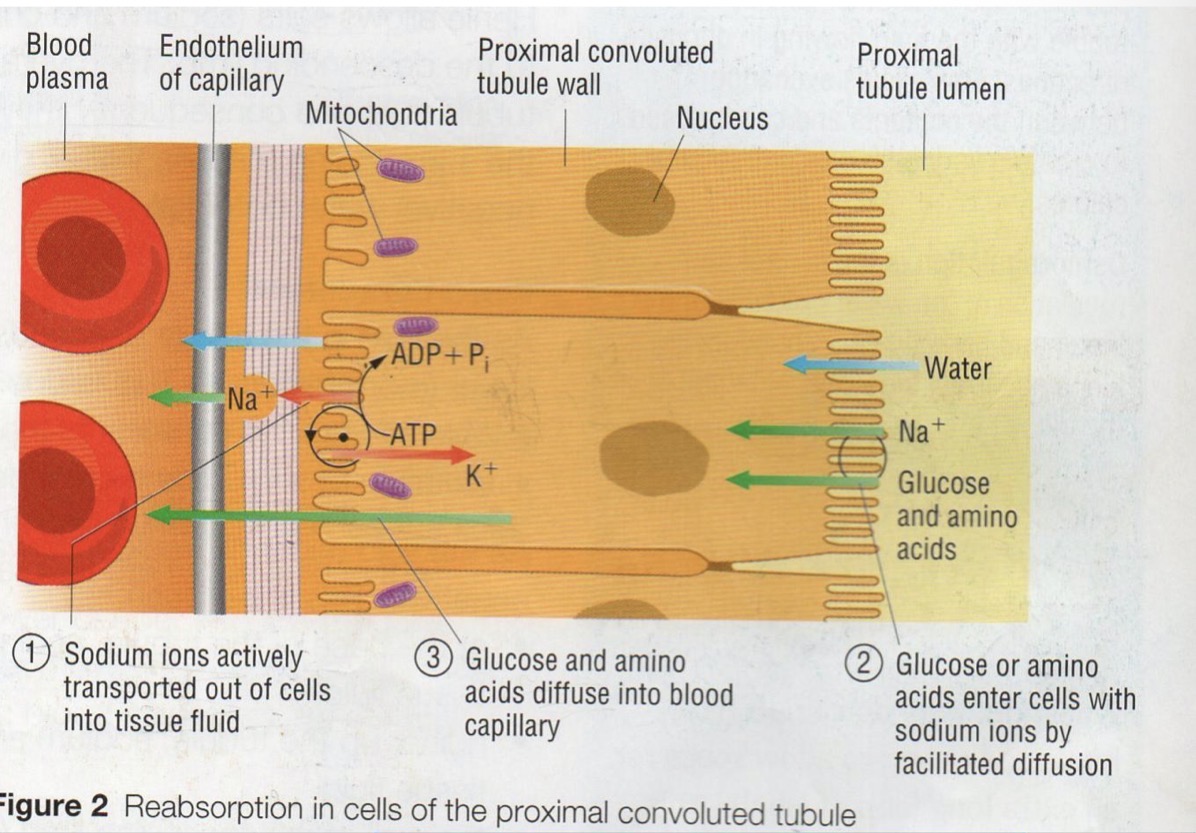
What happens in selective reabsorption
Some of the molecules in the glomerular filtrate are reabsorbed into the blood
Where does most reabsorption of water (and solutes) occur
The proximal convoluted tubule
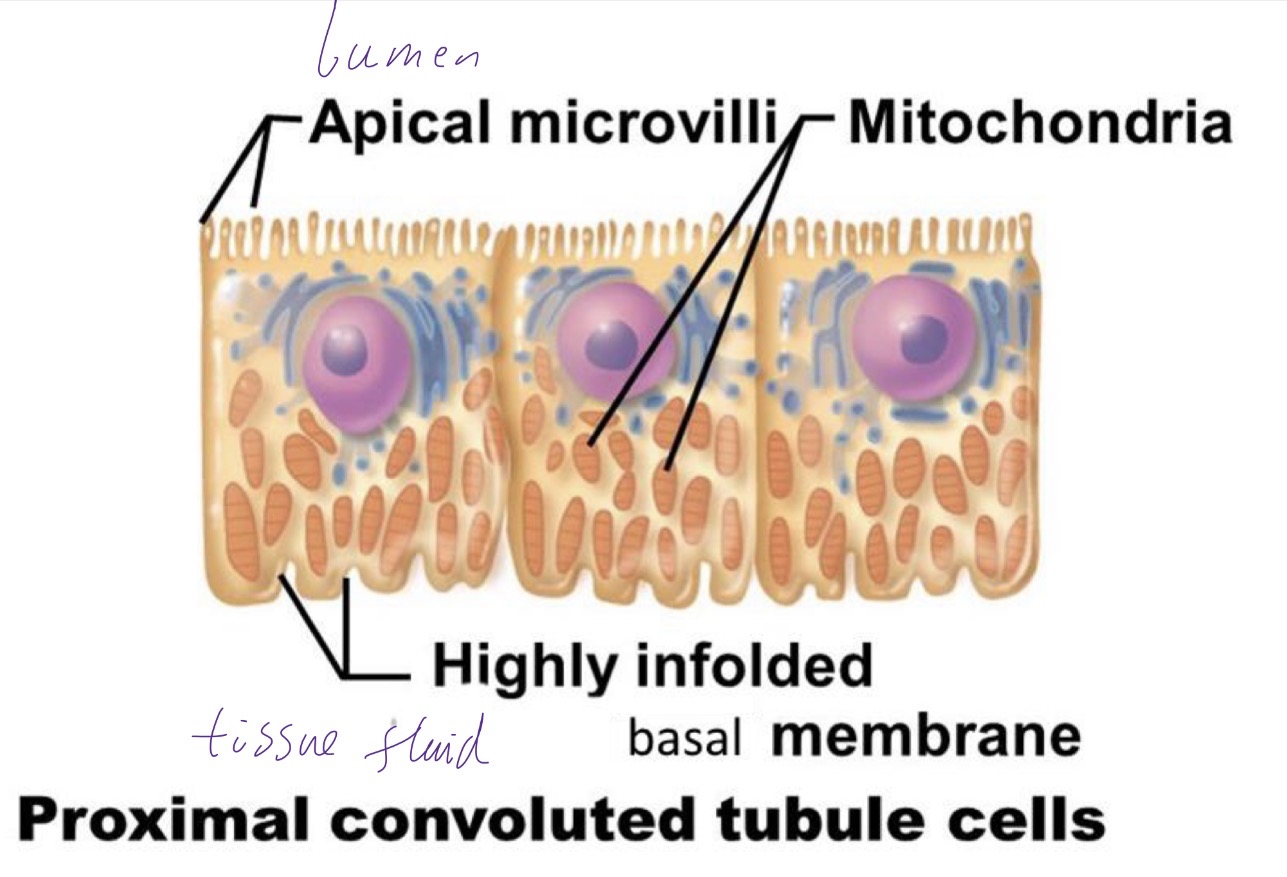
How are the cells of the proximal convoluted tubule adapted to their role
many mitochondria
Apical microvilli on apical membrane (facing lumen) on brush border, increases SA
Tight junctions hold cells together so fluid can’t pass between them, must go through
May co-transporter proteins (and aquaporins) on apical membrane
Basal membrane folded to increase SA
How does selective reabsorption work?
basal membranes (nearest capillaries/tissue fluid) contain sodium-potassium pumps
Pumps sodium ions out of cell, decreasing its concentration inside cells
Na+ passively diffuses through special co-transporter proteins into cells from glomerular filtrate across apical membrane
Co-transports glucose/amino acids etc
Na+ conc gradient provides energy to move glucose out of filtrate against concentration gradient (secondary active transport).
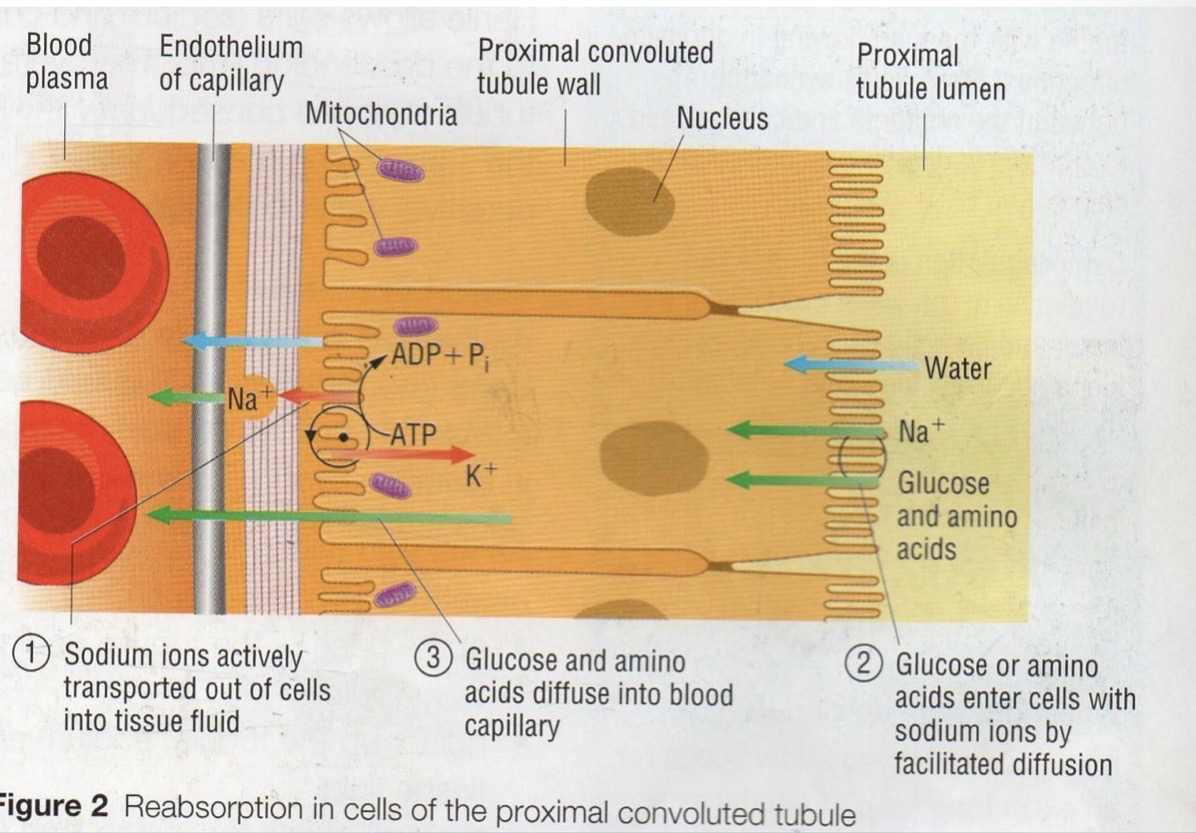
What happens to glucose once it is in the cells of the proximal convoluted tubule.
Glucose diffuses down its concentration graident through a transport protein in the basal membrane and into the blood
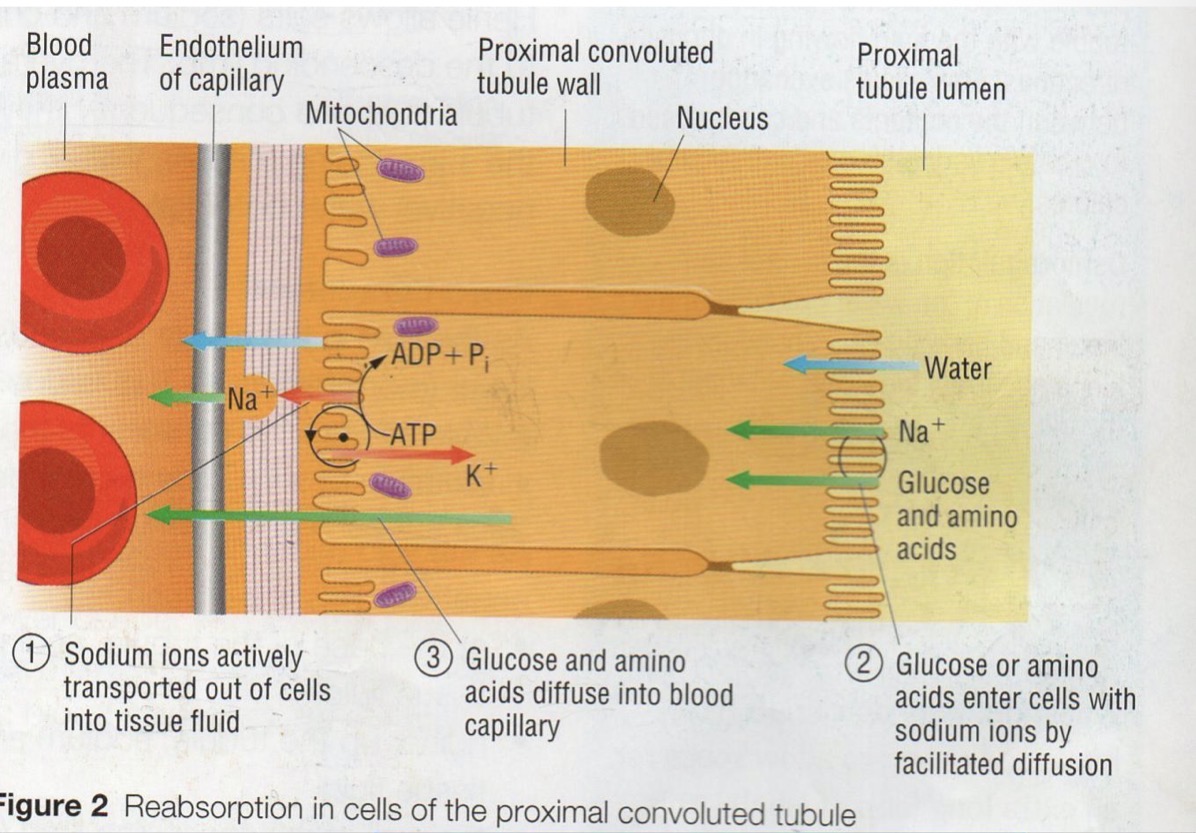
How does a sodium-potassium pump work
2K+ ions actively transported into cell
3Na+ ions transported out of cell
Creates an decrease of Na+ concentration inside cells
Na+ re-enters via co-transporter proteins on other side of cell
K+ re-exits cell by facilitated diffusion down conc gradient
Repeats
Define osmoregulation
The control of water content in the blood (and therefore the whole body) achieved by negative feedback mechanisms
How does the body detect changes in blood water potential
hypothalamus detects changes in the water potential of blood passing through capillaries within the hypothalamus
What are the names of the cells which detect changes in water potential, and how are they affected
Osmoreceptors in the hypothalamus shrink when there is less water in the blood
Describe the journey of ADH from where it is produced to where it is secreted
ADH made by the hypothalamus
Travels down in neurosecretory cells
To the posterior pituitary gland
Stored in the vesicles at the end of the neurosecretory cells in the posterior pituitary ready to be secreted
How is ADH released into the bloodstream
Hypothalamus detects that water potential of the blood is too low
Sends a nervous impulse to the pituitary
Releases the ADH into the bloodstream
Where are the target cells of ADH
In the wall of the collecting duct and te distal convoluted tubule of the kidneys
How are the cell surface membranes of the collecting duct cells adapted for reabsorption of water
contain lots of channel proteins called aquaporins
How can aquaporins be found within the cell
Either embedded in the cell surface membrane or stored in vesicles within the cell
Describe the action of ADH on target cells
ADH binds to receptor proteins in cell surface membrane of cells in collecting duct wall
Triggers formation of cAMP, acts as a second messenger
Causes an enzyme cascade
Triggers the movement of vesicles containing aquaporins towards the cell surface membrane
Vesicles fuse to membrane and insert extra aquaporins
What happens when blood water potential returns to set point
once water potential of the blood rises, ADH is stopped
Membrane pinches off vesicles containing the aquaporins towards
Water does not leave the collecting duct but instead continues to bladder
More dilute urine, copious in volume