transport of O2 and CO2
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
What are erythrocytes
Red blood cells
What is the role of erythrocytes
Transport oxygen around the body
What is haemoglobin
a pigment in red blood cells
Globular protein made of four polypeptide chains (2 α-alpha chains and 2 β- chains)
Each chain has a haem prosthetic group contain iron
Oxygen binds to haemoglobin to form oxyhemoglobin in a reversible reaction
What are the three ways which carbon dioxide is transported in the blood
5% dissolved in blood plasma
10-20% combines with haemoglobin to form carbaminohaemoglobin
75-85% converted into hydrogen carbonate ions (HCO3-) in the cytoplasm of erythrocytes
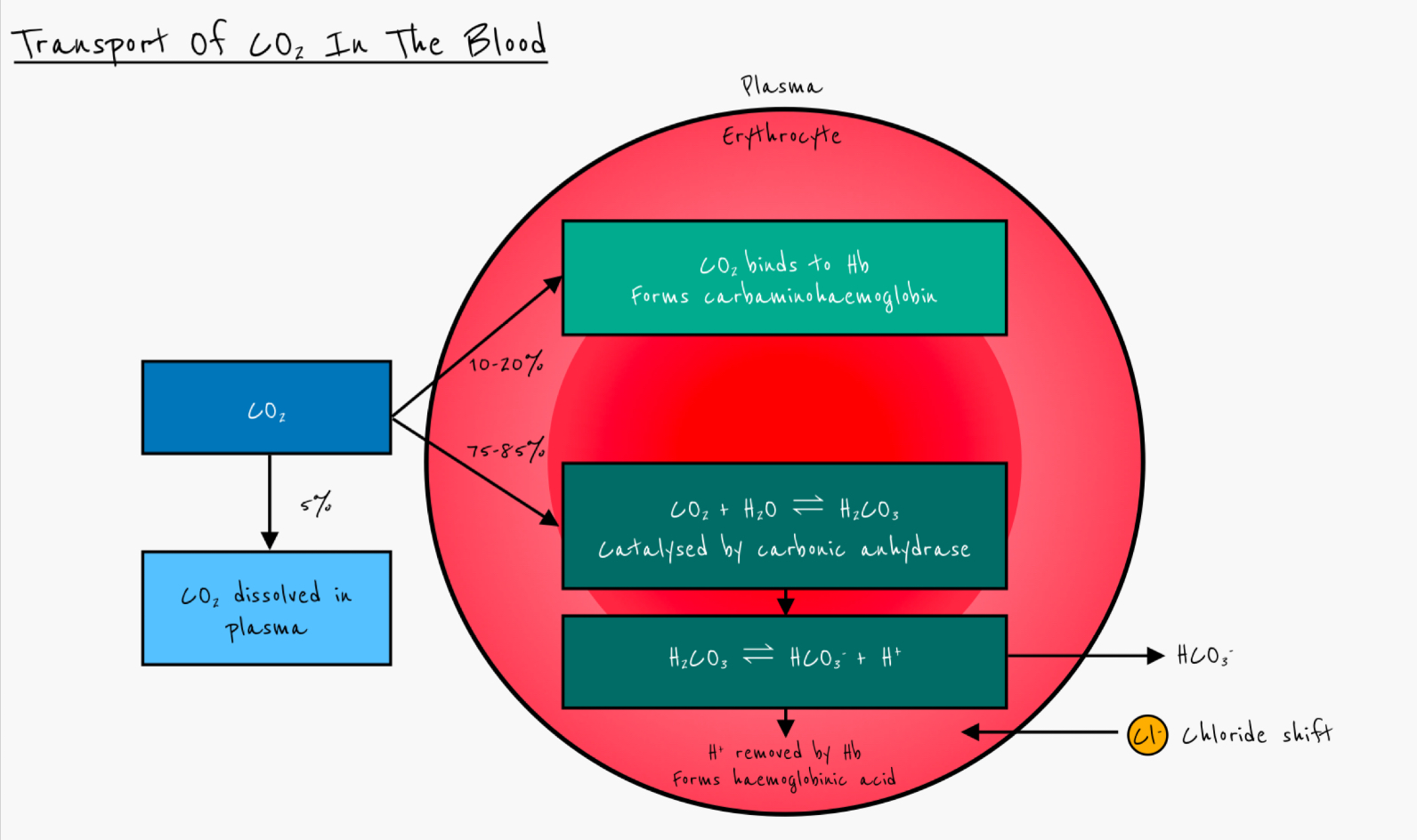
Which enzyme catalyses the production of hydrogen carbonate ions
Carbonic anhydrase
Describe how hydrogen carbonate ions are produced in erythrocytes
carbon dioxide diffuses into erythrocytes
Reacts with water, catalysed by carbonic anhydrase
Forms carbonic acid (H2CO3)
Carbonic acid dissociates to form hydrogen carbonate ions and hydrogen ions
Give the equation for the conversion of CO2 to HCO3-
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3-
What happens to hydrogen carbonate ions after they have been produced
diffuse down concentration gradient
Out of red blood cells and into plasma
What is the chloride shift
The movement of Cl- ions into erythrocytes to balance the electrical change due to the negative hydrogen carbonate ions leaving.
How does haemoglobin act as a buffer
Prevents changes in pH by accepting 3 H+ ions to form haemoglonobic acid
Define partial pressure
The contributing pressure of a single gas to the total pressure of a mixture of gases
What happens to hydrogen carbonate ions at the lungs
low partial pressure of carbon dioxide (pCO2) at lungs
HCO3- diffuses back to erythrocytes
Reacts with H+ to form H2CO3
Carbonic anhydrase catalyses conversion of H2CO3 back into water and CO2
CO2 diffuses out of blood into lungs
Cl- ions diffuse out of erythrocytes into plasma
Describe the movement of oxygen in the lungs
high partial pressure of oxygen (pO2) in alveoli
Lower partial pressure of oxygen in blood in capillaries
Oxygen diffuses from alveoli to blood
Describe the movement of oxygen at respiring tissues
high partial pressure of oxygen in blood
Lower partial pressure of oxygen in respiring tissues
Oxygen diffuses from blood to respiring cells
Describe the role of haemoglobin in transporting oxygen around the body
Haemoglobin has a high affinity for oxygen so it binds to haemoglobin in lungs (high pO2) forming oxyhemoglobin.
Oxygen is released in respiring tissues (low pO2)
By what process does oxygen bind to haemoglobin to produce the sigmoidal shape of the oxygen dissociation curve
Cooperative binding
Explain how the binding of one oxygen molecule to a haem group affects haemoglobin
binding of first oxygen molecule causes conformational change altering tertiary structure of haemoglobin (slightly)
Affinity for oxygen increases so further loading of oxygen molecules is easier
Explain how removal of the first oxygen at respiring tissues affects haemoglobin
removal of first molecule causes conformational change
Affinity for oxygen decreases (next molecule can leave more easily)
Explain the significance of the oxygen dissociation curve
High pO2 in lungs so haemoglobin rapidly loaded with oxygen
Relative small drop in pO2 at respiring tissues leads to rapid dissociation of oxygen so it is free to diffuse into cells.
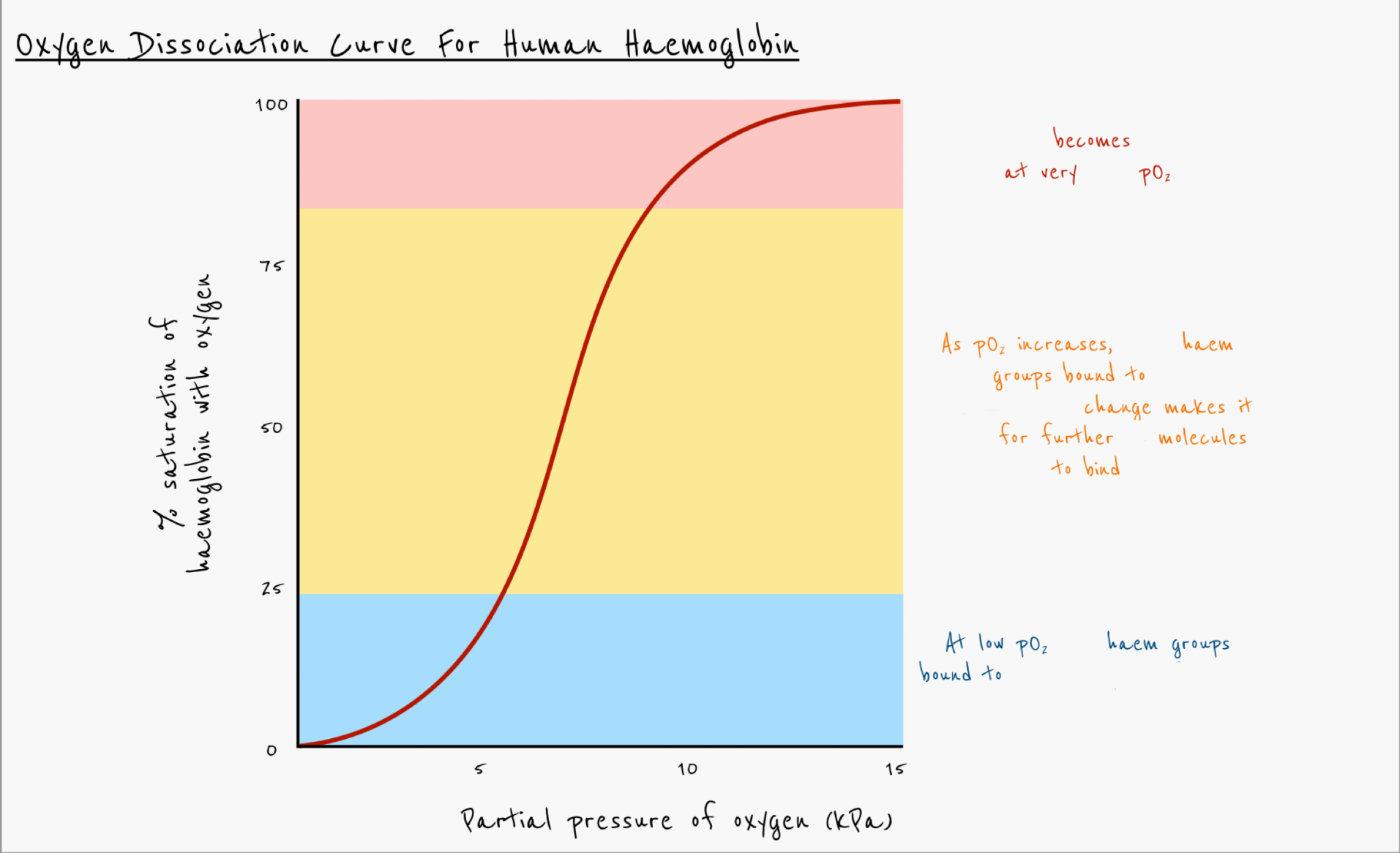
Explain the oxygen dissociation curve for human haemoglobin
Haemoglobin becomes saturated at very high pO2
As pO2
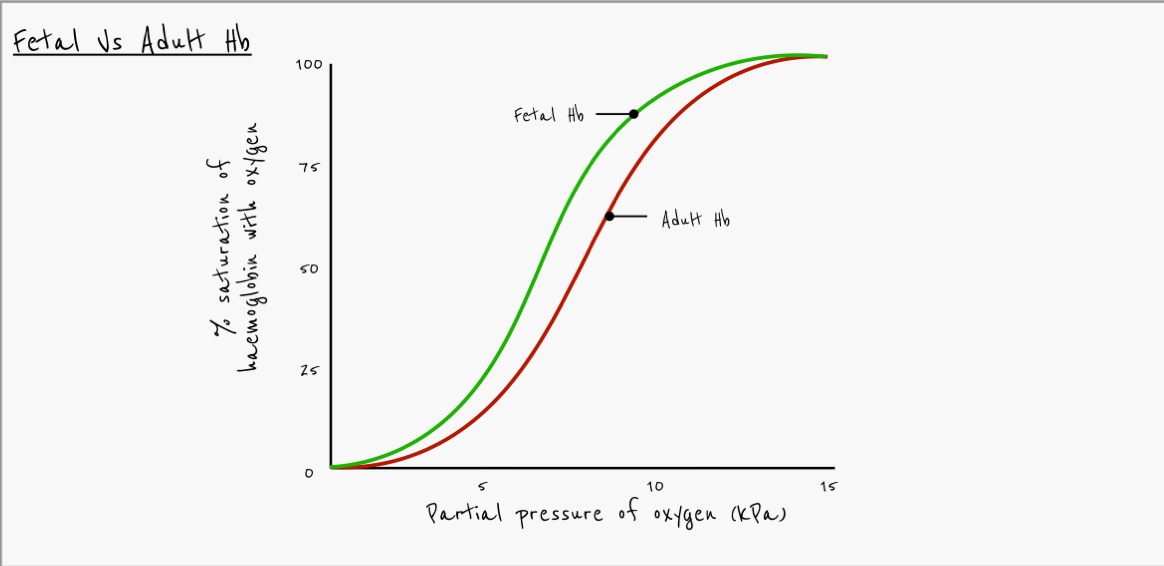
Describe difference in oxygen affinity between fetal haemoglobin and adult haemoglobin
Fetal haemoglobin has a higher affinity for oxygen
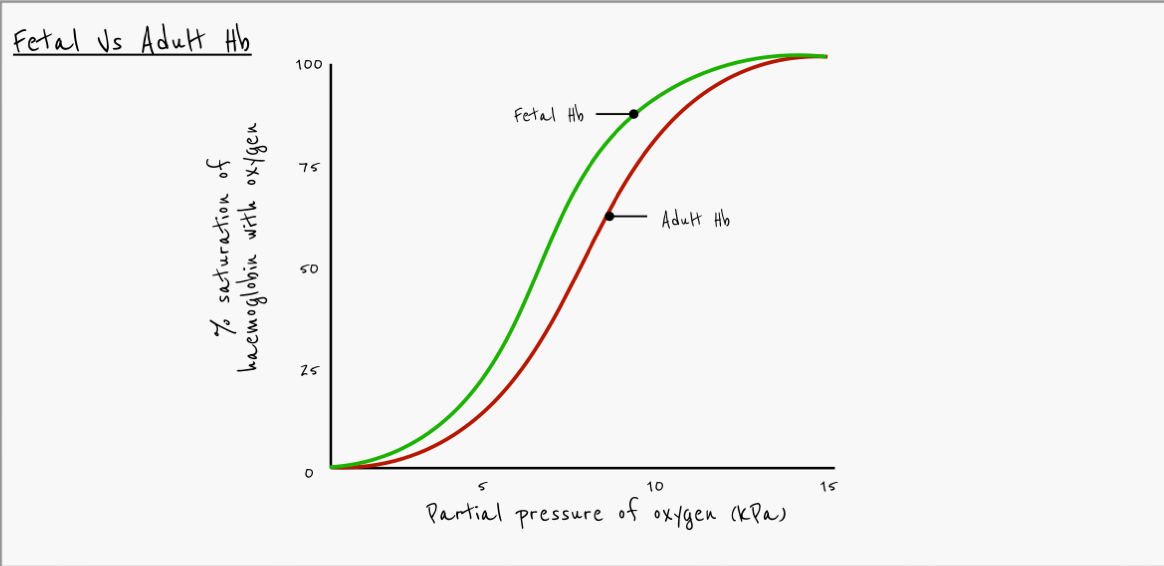
Explain why fetal haemoglobin curve is to the left of the adult haemoglobin curve
placenta has low pO2
Adult haemoglobin will release O2 at the placenta
Foetal haemoglobin has a higher affinity for oxygen at low pO2
It is able to take up oxygen in the placenta
What effect does carbon dioxide have on haemoglobin
at higher pCO2, haemoglobin gives up oxygen more easily
What effect does higher pCO2 have on the oxygen dissociation curve
shifts to the right
Bohr shift
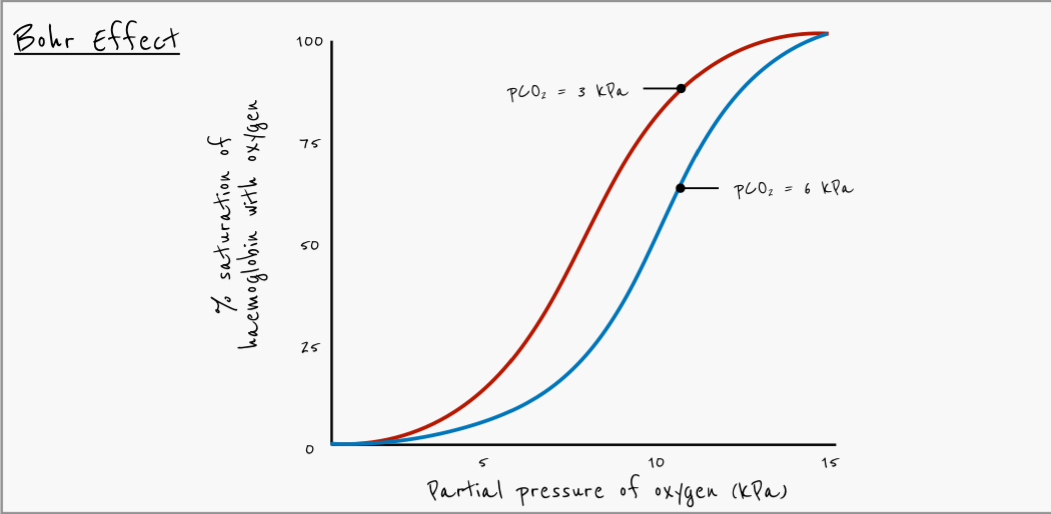
Why is the bohr effect important
Actively respiring tissues have high pCO2, haemoglobin gives up oxygen more easily
Lungs have lower pCO2, haemoglobin binds to oxygen more easily
Explain how an increase in CO2 in the blood leads to the release of more O2 from red blood cells
more carbon dioxide diffuses in to red blood cells
More carbonic acid is formed by carbonic anhydrase
More hydrogen ions formed
Haemoglobin has a high affinity for hydrogen ions
Haemoglobin binds to hydrogen ions to form haemoglobinic acid (HHb)
Formation of HHb decreases the affinity of haemoglobin for oxygen
Carbon dioxide binds to -NH2 of polypeptides to form carbaminohaemoglobin
Causes change in tertiary structure, releasing more oxygen
Outline the benefits of the bohr shift to actively respiring tissue
Actively respiring tissue requires more oxygen for aerobic respiration
Actively respiring tissue produces more CO2
Haemoglobin involved in transport of CO2 so there’s less haemoglobin available to combine with O2
Bohr shift causes more oxygen to be released
What effect does pH have on Hb’s affinity for oxygen?
Affinity decreases as pH decreases (more H+ ions)