Adrenal glands, parathyroid hormone and calcium homeostasis
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
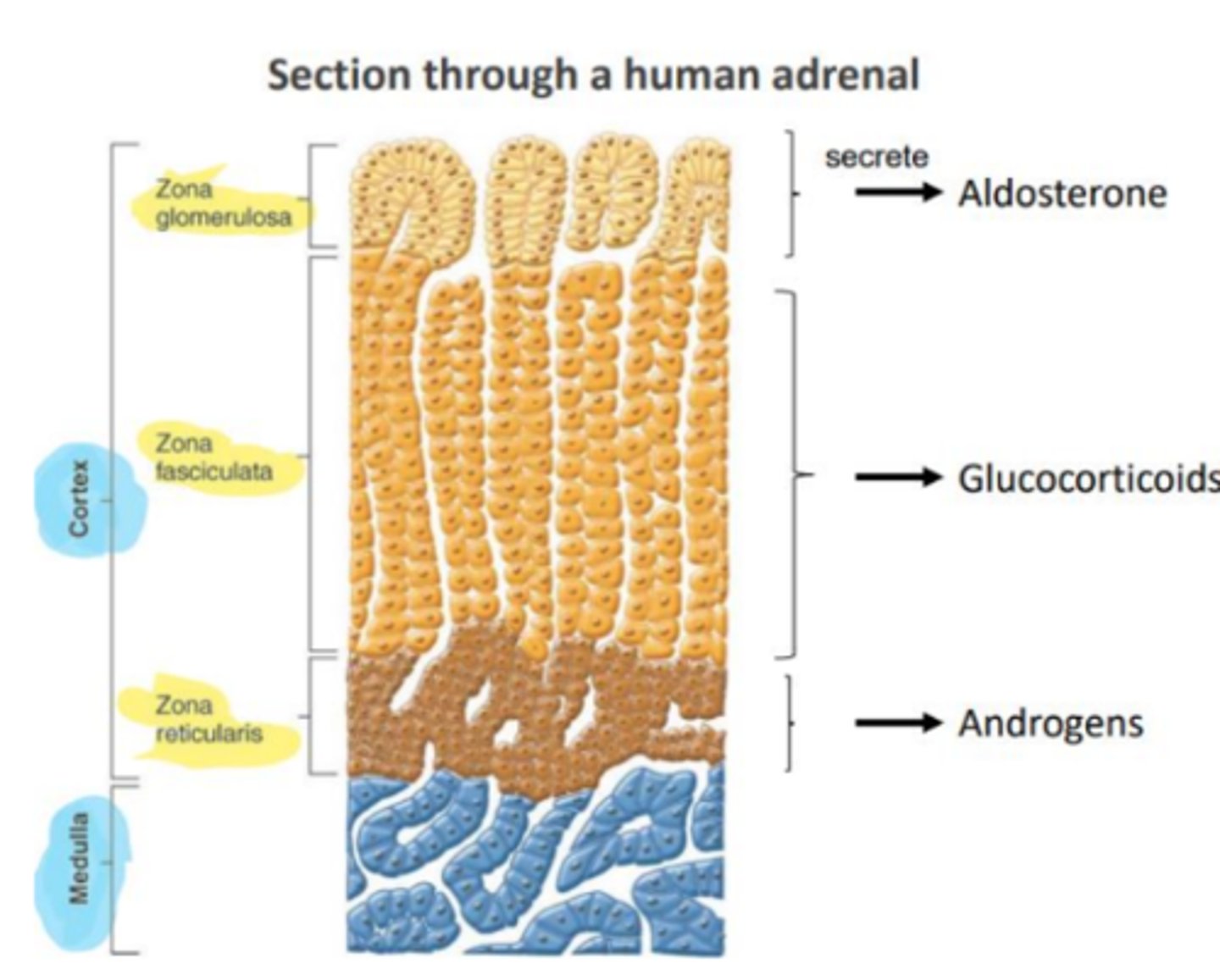
Describe the structure of adrenal glands
Describe the synthesis of steroid hormones
Cholesterol is converted to pregnenolone by Desmolase
and can we further converted by
hydrogenase enzyme to progesterone and
after a few steps to aldosterone, cortisol
and Testosterone, which can be converted
to Oestradiol by Aromatase enzyme
Describe the physiological action of mineralcorticosteroid aka aldosterone
control of electrolyte homeostasis
Increases sodium reabsorption and potassium excretion in kidney
- Regulated by renin-angiotensin
system
- Increases blood volume and
pressure
Describe the physiological action of glucocorticoids aka cortisol
response to "stress"
metabolism:hyperglycemia, gluconeogenesis and decrease in glucose uptake into cells
muscle: protein catabolism and reduced synthesis
bones: osetoporosis due to reduced Ca absorption and osteoblast activity
Inflammatory & immune systems to:
- inhibition of inflammatory responses, reduce wound healing, repair and proliferation long term and short term reduce redness, pain, swelling
reduce COX2, cytokines, complement, NO, histamine and IgG
increase annexin-1, which inhibits PLA2 that produces Arachidonic acid
Describe the physiological actions of androgens aka testosterone
involved in the development of secondary sexual characteristics at puberty
• role in preventing degenerative changes in ageing
How do you regulate mineralocorticoid function
Renin released by kidney
nephrons in response to
reduced plasma volume
- Renin converts
angiotensinogen into
angiotensin I
- Angiotensin 1 is converted
to angiotensin II (ATII) in
tissues
- ATII acts on glomerulosa
cells to stimulate
aldosterone production
- Aldosterone increases Na+
reabsorption and so
increases plasma volume
How do you regulate glucocorticoid function
stimuli such as pain, stress etc release CRH in hypothalamus, which causes the release of ACTH in anterior pituitary, which stimulates the release of glucocorticoids and androgens in the adrenal cortex
glucocorticoids inhibit CRH and ACTH via negative feedback
Describe Addison's disease
primary adrenal insufficiency due to adrenal cortex or secondary due to lack of ACTH
- Severe illness with hypotension, tiredness,
weakness, anorexia, hyperpigmentation, GI effects, salt craving
- Treated by Fludrocortisone replacement
Describe Cushing's syndrome
ACTH dependant-pituitary tumour producing excess
ACTH independant= adrenal adenoma, hyperplasia, carcinoma
Weight gain, redistribution of fat to abdomen,
face & posterior neck, diabetes, glucose resistance
acne, hirsutism, more likely to get infections and bruising, osteoporosis, skin thinnening, high blood pressure
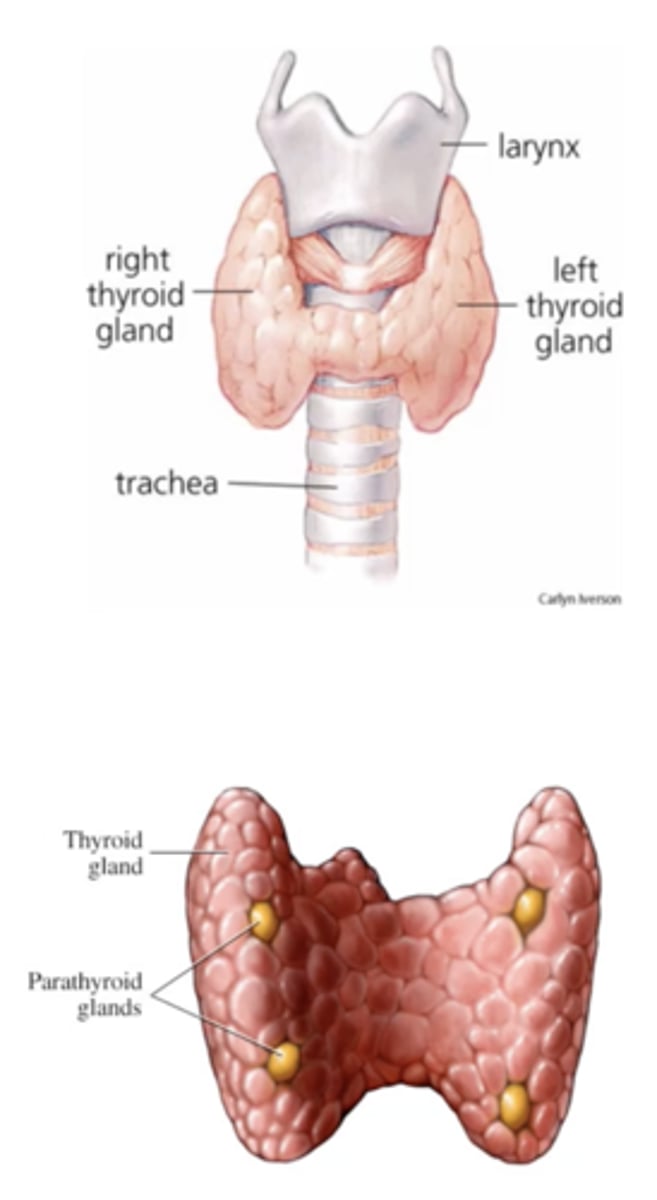
Describe the anatomy of the parathyroid gland
Chief cells produce parathyroid hormone
What is the function of Ca in the body
1-2kg calcium in the adult human body
- 99% resides in bone and teeth as hydroxyapatite crystals, providing structural integrity
of skeleton and teeth
- Calcium ions in intracellular (0.9%) and extracellular (0.1%) fluids play key roles in :
- Bone growth and remodelling
- Blood coagulation (enzyme co-factor)
- Muscle contraction (required for actin:myosin interactions)
- Neuronal function(regulates excitability)
- Enzyme action
- Exocytosis of hormones and neurotransmitters (triggered by Ca2+ influx)
- Intracellular signalling (second messenger)
Describe parathyroid hormone synthesis PTH
Produced by parathyroid Chief cells :
- Synthesized from the precursor molecule pre-pro-PTH (115 amino acids)
- Precursor (pre-pro-PTH ) is subsequently cleaved to pro-PTH (90 amino acids)
- PTH is a biologically active 84 amino acid peptide (the first 34aa are fully active)
How is PTH secreted and inhibited
• Inhibited by Vitamin D Secondary mechanism-negative feedback
inhibited by high Ca levels
• Low Ca2+-> detected by calcium-sensing receptor (CaSR) on the surface of chief cells PTH binds to the G-protein coupled receptor PTH-R -> Activation of PTH-R causes increases in cAMP and release of Ca2+ from intracellular stores
Describe the physiological action of PTH
- promote bone resorption and increase Ca2+
concentration in blood
- PTH inhibits PO4 reabsorption in kidneys, so more free plasma
Ca2 and PTH Stimulates Ca2+ reabsorption on distal convoluted tubule, so more in plasma
- PTH stimulates Ca2+ reabsorption via activation of vitamin D through stimulating renal 1α-hydroxylase
Describe vitamin D synthesis
Synthesised in skin keratinocytes from 7-dehydrocholesterol via action of ultraviolet light
• Ingested in food and absorbed into blood stream
• Metabolised in liver to 25-hydroxycholecalciferol and in kidneys to activated form: 1,25-
dihydroxyvitamin D3 /Calcitriol by 1α-hydroxylase
Describe the action of Vit D
Calcitriol acts on nuclear receptors (VDR) in the small intestines, which increases gene transcription
• Increases in Ca2+ transport proteins→ increased rate of Ca2+ absorption; rapid uptake of Ca2+ from the gut
• Increases bone resorption and reduces urinary Ca2+ loss at the kidney
Describe calcitonin
Peptide hormone produced by parafollicular cells ( C-cells) in the thyroid gland
Released in directly response to increased Ca2+ in extracellular fluid
Describe the action of calcitonin
Inhibits osteoclasts (release Ca2+ from bone)→protective effect on bone Ca2+
• Stimulates Ca2+ release from kidneys (opposite effects of PTH)
• No significant effect on Ca homeostasis, PTH and D3 are main
What could be the causes of hypocalcemia
Vitamin D Deficiency: lack of sunlight/dietary sources
- Chronic Renal Failure: reduced hydroxylation of vitamin D
- Pseudohypoparathyroidism: tissue resistance to PTH
- Iatrogenic: damaged or removed during thyroid surgery
- Autoimmune disorders: auto-antibodies destroy tissue
What are the symptoms of hypocalcaemia
tetanic muscle contractions: spasms laryngeal muscle (laryngeal stridor)
- seizures (brain)
- cardiac effect (repolarization is delayed with prolonged QT
interval)
- cataract (protein accumulation)
- dry & flaky skin; brittle nails
- tetany in the hand (Trousseau sign of latent tetany)
- Osteoporosis ( fragile& brittle bones)
- Rickets ( bones bended inwards)
What can cause hypercalcemia
Adenoma (90%) or hyperplasia, more common in
women(benign tumour)
Chronically elevated plasma PTH
What are the symptoms of hypercalcemia
Psychic Moans - depression of nervous system; slow reflex;
depression
- Abdominal Groans - decreased appetite; anorexia;
constipation; vomiting
- Bones - osteitis fibrosa/arthritis; cystic area in bone, may
contain fibrous tissue; marrow fibrosis.
- Stones - calcium phosphate crystals throughout body; kidney stones (deposit in kidney
What are the treatments for Cushing syndrome
Inhibit steroid biosynthesis:
- Metyrapone-11b-hydroxylase inhibitor
- Ketoconazone -17a-hydroxylase & 11b-hydroxylase
inhibitor
Inhibit ACTH release:
- Pasireotide-SSTR5 agonist (somatostatin analogue,
inhibits release from anterior pituitary)
- Cabergoline- dopamine D2 agonist( can supress
secretion of ACTH)
Inhibition of glucocorticoid receptor :
-Mifeprestone (also progestogen receptor antagonist)
Describe the release of cortisol
Pro-opiomelanocortin (POMC) is the archetypal polypeptide precursor of ACTH, this
allows to save energy (4 for 1) and allows to have better regulation of ACTH
- ACTH acts on a G-protein coupled receptor (melanocortin 2 receptor, MC2R) to activate
adenyl cyclase which leads to an increase in cAMP levels and the activation of protein
kinase A (PKA), this leads to:
- Activation of cholesteryl ester hydrolase (CEH) which liberates cholesterol from lipid
droplets.
- Uptake of cholesterol into the mitochondria.
- Stimulation of cholesterol desmolase/CYP11A1 (rate limiting step in steroid hormone
biosynthesis) which results in increased synthesis of cortisol.
- ACTH has little effect on aldosterone synthesis, which is driven primarily by angiotensin
II
Describe how cortisol binds to affects gene transcription
Inactive Glucocorticoid receptor molecule is kept in the cytosol through binding to
HSP90 Heat shock proteins, HSP bind to a region on the receptor that binds DNA
- Transcription activation domain (once receptor is sitting on DNA it recruits proteins to
synthesise mRNA), DNA binding domain (recognises and binds to DNA), ligand binding
domain (hormone binds to receptor)
- Once hormone binds there is a conformational change in receptor, it will kick off HSP90
and transport receptor from cytosol to nucleus, which will allow it to bind hormone
response elements, which recruit transcription factors (co-activator/ suppressors) and
promote/supress genes