cardiovascular and lymphatic systems
1/219
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
220 Terms
circulatory system structures
blood vessels (complex array of tubing)
heart (pump)
circulatory system function
deliver oxygen, nutrients, and other substances to all body cells
remove waste products of cellular metabolism
intrinsic regulators of circulatory system
nervous system
endocrine system
supply nutrients
interaction between circulatory system and digestive system
supply oxygen
remove carbon dioxide
maintain acid-base balance
interaction between circulatory system and respiratory system
waste removal
fluid, electrolyte
acid-base balance
interaction between circulatory system and renal system
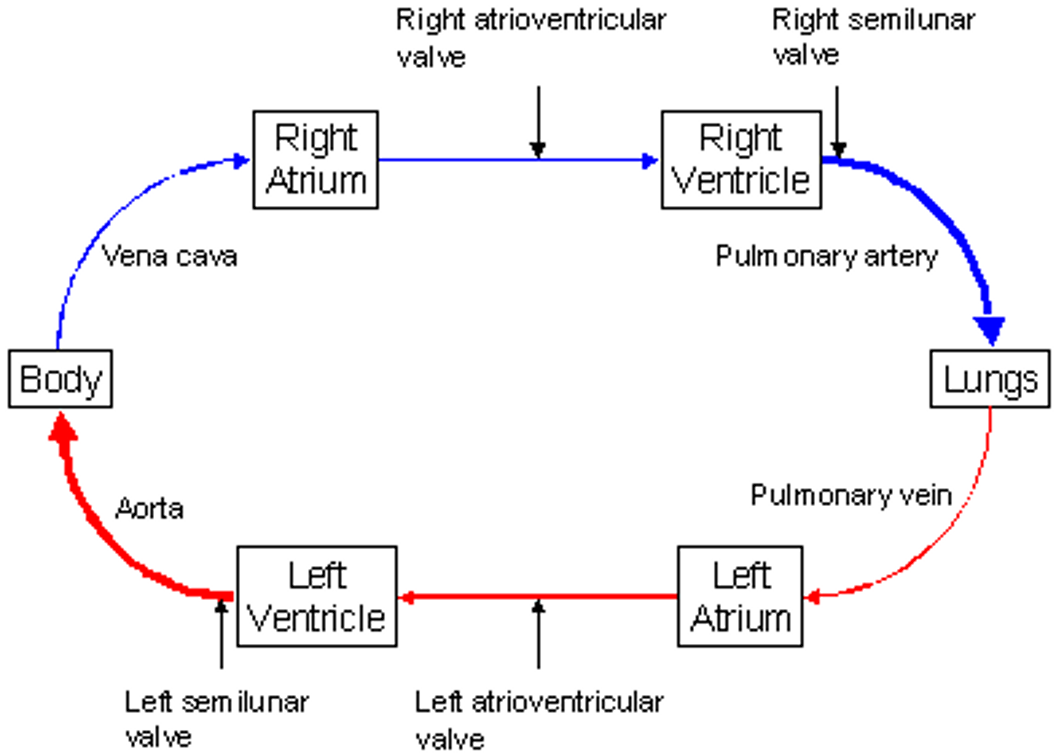
pulmonary circulation
right heart pumps deoxygenated blood to the lungs for gas
systemic circulation
left heart pumps oxygenated blood to the rest of the body for delivery of oxygen & nutrients and removal of wastes & carbon dioxide
arteries
carry blood away from heart
capillaries
allow closest contact and exchange between blood and interstitial space or the cellular environment
veins
carry blood toward the heart
lymphatics
carry plasma from interstitium to heart
heart
weighs < 1 lb, about size of fist
lies obliquely at an angle in the mediastinum (above diaphragm and between lungs)
heart wall/fibrous skeleton
enclose and support heart
divides it into 4 chambers
valves and great vessels
valves
indentations of endocardium that direct flow
separate atria from ventricles & ventricles from aortic/pulmonary arteries
open and close with pressure changes within chambers
great vessels
conduct blood to and from heart
coronary circulation
arteries and veins serve metabolic needs of heart cells
heart’s nerves/muscle cells
direct rhythmic contraction and relaxation → propel blood through pulmonary and systemic circuits
pericardium
double-walled membranous sac that encloses heart
parietal pericardium
outer layer; surface layer of mesothelium over a thin layer of connective tissue
visceral pericardium
aka epicardium (inner layer), folds back and is continuous with the parietal pericardium
allows large vessels to enter/exit the heart w/o breaching layers
pericardial cavity
fluid-containing space between visceral and parietal pericardium
pericardial fluid
secreted by cells of mesothelium to lubricate membranes and minimize friction as the heart beats
pericardium functions
prevents displacement of heart during gravitational acceleration/deceleration
provides physical barrier against infection/inflammation from lungs and pleural spaces
contains pain and mechanoreceptors that elicit reflex changes in BP and HR
myocardium
cardiac muscle
anchored to heart’s fibrous skeleton
thickness of myocardium
varies from one chamber to another
r/t amount of resistance muscle must overcome to pump blood from different chambers
endocardium
internal lining composed of connective tissue and squamous cells
continuous w/ endothelium that lines arteries
creates a continuous closed circuit
atria
smaller w/ thinner walls
R = 2mm, L = 3-5mm
serve as storage units and conduits for blood
offers little resistance of flow of blood into ventricles
ventricles
thicker myocardial layer and make up bulk of heart
must propel blood through pulmonic and circulatory systems
15 mmHg
mean pulmonary pressure
92 mmHg
mean arterial pressure
left ventricle
13-15mm, most muscular
larger, bullet shaped and pumps blood through large valve opening into the higher-pressure systemic circulation
right ventricle
3-5mm
crescent/triangle shaped and acts like a bellows to propel large volumes of blood through a small valve into the low-pressure circulation
interatrial septum
separates R and L atria
interventricular septum
separates R and L ventricles
an extension of fibrous skeleton of the heart
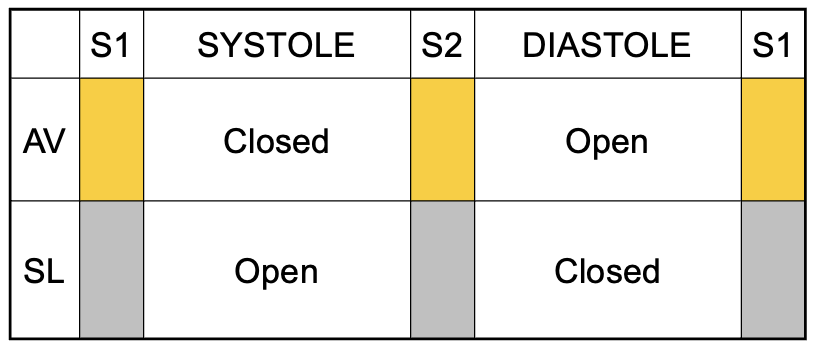
atrioventricular valves
open at the beginning of systole and allow blood to fill ventricles
close at beginning of ventricular contraction to prevent backflow of blood into atria
semilunar valves
open at end of ventricular contraction when the pressure in the ventricles exceed the pressure in the pulmonary artery & aorta
close at the beginning of ventricular relaxation as the pressure in the chambers drops below the pressure in the pulmonary artery & aorta to prevent backflow of blood into the ventricles
chordae tendinae
connect valve leaflets or cusps to papillary muscle
papillary muscle
extensions of myocardium that pulls cusps together and downward at beginning of ventricular contraction
prevent backward expulsion of AV valves into atria
tricuspid valve
AV valve with 3 cusps (largest diameter)
mitral valve
AV valve with 2 cusps — left heart, resembles a cone shaped funnel
aortic/pulmonic valves
have 3 cup-shaped cusps
behave like one-way swinging doors
pulmonic is thinner than aortic
superior/inferior vena cavae
enter the right atrium
pulmonary artery
carries deoxygenated blood from right ventricle to the lungs
pulmonary vein
carries oxygenated blood from lungs to the left atrium
aorta
delivers blood to systemic vessels which carry it to the rest of the body
diastole
relaxation phase, blood fills ventricles
systole
contraction phase, blood pumped out of the ventricles into the circulation
ejection on right occurs slightly earlier than left d/t pressure changes
R atrial contraction
blood enters the atria from inferior and superior vena cavae and coronary sinus
L atrial contraction
blood enters through 4 pulmonary veins (2 from each side)
atrial contraction
atria fill and distend → opens AV valves
blood passively fills ventricles
provides “atrial kick” → actively pumps additional blood into ventricle
cardiac cycle phases
phase 1: isovolumetric contraction
phase 2
phase 3: isovolumetric relaxation
phase 4
phase 1
ventricular volume is constant
increase in ventricular pressure closes AV valves
phase 2
increase in ventricular pressure opens SL valves and blood is ejected to the circulation → intraventricular volume and pressure decrease
phase 3
decrease in ventricular pressure closes SL valves
ventricles continue to relax
phase 4
decrease in ventricular pressure opens AV valves
permits ventricular filling from atria
diastole: isovolumetric ventricular relaxation/filling
(0.4 sec)
as the ventricles relax following systole, the pressure drops below that in the arteries and the semilunar valves close.
when the pressure in the ventricles drops below that in the atria, the AV valves open and allow for ventricular filling.
toward the end of diastole, the atria contract and eject 0-30% more blood volume into the ventricles (0.1 sec)
systole: isovolumetric contraction/ejection
(0.3 sec)
as the pressure in the ventricles becomes greater than the atria, the AV valves shut
isovolumetric contraction of the ventricles
as the pressure increases and becomes greater than the arteries, the SL valves open → blood is ejected into the pulmonary and systemic circulation
first heart sound
AV valves shut at beginning of systole due to increasing pressure in the ventricles
surrounding tissue vibrates and blood flow becomes turbulent = sound
second heart sound
SL valves shut at end of systole due to falling pressure in the ventricles
physiologic split
physiologic split
aortic valve precedes pulmonic valve closure by 0.02-0.04 sec during expiration and 0.04-0.06 sec during inspiration
valve closure and cardiac cycle
third heart sound
may be heard if ventricular wall compliance is decreased and structures in ventricular wall vibrate
can occur in congestive heart failure or valvular regurgitation
may be normal in those younger than 30
fourth heart sounds
may be heard on atrial systole if resistance to ventricular filling is present
abnormal
causes of S4
cardiac hypertrophy, disease or injury to ventricular wall
blood flow
coronary circulation
branch that supplies heart; done by vessels of systemic circulation
blood within chambers does NOT supply oxygen and nutrients to heart cells
coronary arteries
receive blood through aortic openings (coronary ostia)
traverse epicardium and branch several times
R coronary artery
supplies blood to
posterior septum
posterior heart
SA, AV node
cardiac veins
empty into the right atrium through another ostium called the coronary sinus
conus
(R coronary artery) supplies blood to upper right ventricle
marginal branch
(R coronary artery) traverses right ventricle to apex
posterior descending
(R coronary artery) supplies smaller branches to both ventricles
left anterior descending artery
(L coronary artery) blood to portions of R and L ventricles and much of the interventricular septum
anterior septum, anterior L ventricle
circumflex artery
(L coronary artery) supplies blood to left atrium and lateral wall of left ventricle
collateral arteries
connections or anastomoses between 2 branches of same coronary artery OR connections of branches between R and L coronary arteries
circulation protects the heart
collateral artery locations
interventricular/interatrial septa
apex of heart
anterior surface of R ventricle
around sinus node
more in epicardium than endocardium
gradual coronary occlusion
results in growth of coronary collaterals under effects of nitric oxide and endothelial growth
coronary capillaries
(3000 per mm², or 1 capillary per muscle cell) where exchange of oxygen and nutrients takes place
ventricular hypertrophy (coronary)
capillary network does not expand with muscle fiber size → same # of capillaries must perfuse larger area → decreased exchange of oxygen and nutrients
coronary veins
most venous drainage occurs through veins in visceral pericardium
smaller veins feed into great cardiac vein → empties into R atrium through coronary sinus
coronary lymphatic vessels
drain fluid to lymph nodes in the anterior mediastinum that eventually empty into superior vena cava with cardiac contraction
impt for protecting myocardium
conduction system
specialized cells that enable heart to generate its own action potentials w/o stimulation from nervous system
muscle fibers uniquely joined so that action potentials pass very quickly
cardiac action potentials
transmission of electrical impulses, affects cardiac cycle
electrical impulse → fibers shorten → muscular contraction → systole
after action potential → fibers relax → return to resting length → diastole
nodes
concentrations of specialized cells in the heart
factors that affect conduction system
ANS provides regulation that affect HR and diameter of coronary vessels
nutrition/oxygen needed for survival and normal function
hormones/biochemicals affect strength and duration of myocardial contraction/relaxation
pacemakers
sinus (SA) node → 70-75 bpm
AV node → 50 bpm (atrial contraction)
bundle of his
bundle branches → R and L
purkinje fibers → 15-30 bpm (ventricular contraction)
depolarization
(activation) inside of cell becomes less negatively charged
repolarization
deactivation of action potential, becomes more negative again
membrane potential
electrical (voltage) difference across the cell membrane
r/t changes in permeability of cell membranes (Na+ and K+)
threshold
point at which the cell membrane’s selectively permeability to Na and K is temporarily disrupted → depolarization
determined by Ca2+
hyperpolarization
resting membrane potential becomes more negative aka hypokalemia
pacemaker cells
more permeable to Na and start off more positively charged → reach threshold and fire sooner
depolarization (cardiac AP)
voltage-sensitive Na channels open & allow rapid influx of Na then rapidly close
K channels close then reopen slowly
voltage-sensitive Ca channels have delayed & slowed opening relative to Na
Ca responsible for contraction of cardiac muscle
normal circumstances: < max amt of Ca released which permits modulation of contractile strength
repolarization (cardiac AP)
return to resting membrane potential is delayed
makes it impossible to fire a second action potential before the first is complete
prevents summation and tetany
60-100 bpm
normal heart rate
> 100 bpm
sinus tachycardia
< 60 bpm
sinus bradycardia
increased heart rate
= less time for the heart to fill and cardiac output decreases aka increased oxygen consumption
sympathetic stimulation
releases norepinephrine →
increased HR
increased conduction speed through AV node
increased atrial & ventricular contractility, & peripheral vasoconstriction
stimulation occurs when a decrease in pressure is detected