Topic 10: Adrenergic Agonists
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Adrenergic receptors are __ transmembrane segment __.
7; GCPRs
Epinephrine and norepinephrine are __ catecholamines, whereas levonordefrin is __.
natural; synthetic
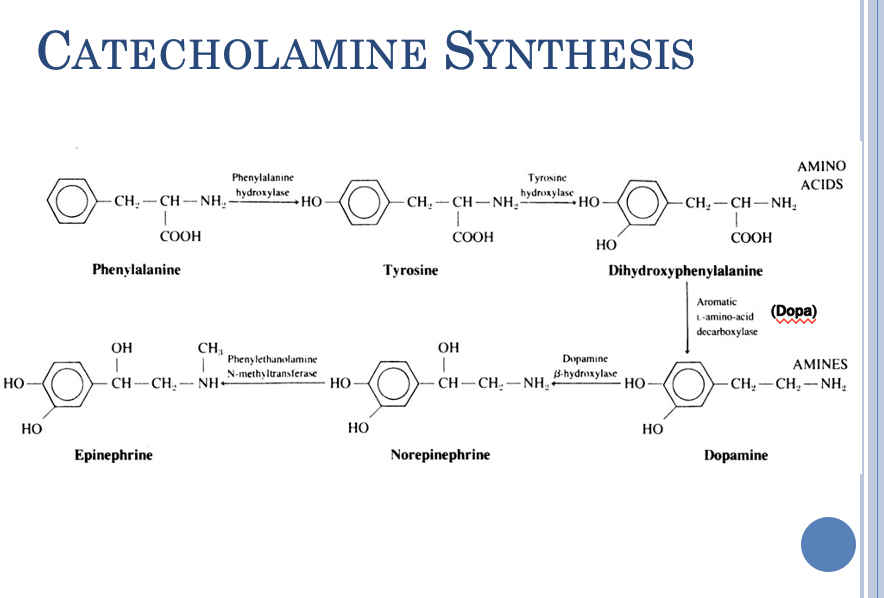
How are catecholamines synthesized?
tyrosine —> L-DOPA —> Dopamine —> norepinephrine —> epinephrine
Which catecholamines are natural? (3)
norepinephrine, epinephrine, dopamine
Which catecholamines are synthetic? (3)
levonordefrin, isoproterenol, dobutamine
What receptors are activated by norepinephrine?
alpha 1, alpha 2, beta 1
What receptors are activated by epinephrine?
alpha 1&2, beta 1&2
What receptors are activated by dopamine?
dopamine, alpha 1, beta 1
What receptors are activated by levonordefrin?
alpha 2, beta 1
What receptors are activated by isoproterenol?
beta 1, beta 2
What receptors are activated by dobutamine?
beta 1
Epinephrine does not discriminate between __.
adrenoceptor subtypes
Where are catecholamines released from?
post-ganglionic sympathetic neuron terminals & adrenal glands (epi and some NE)
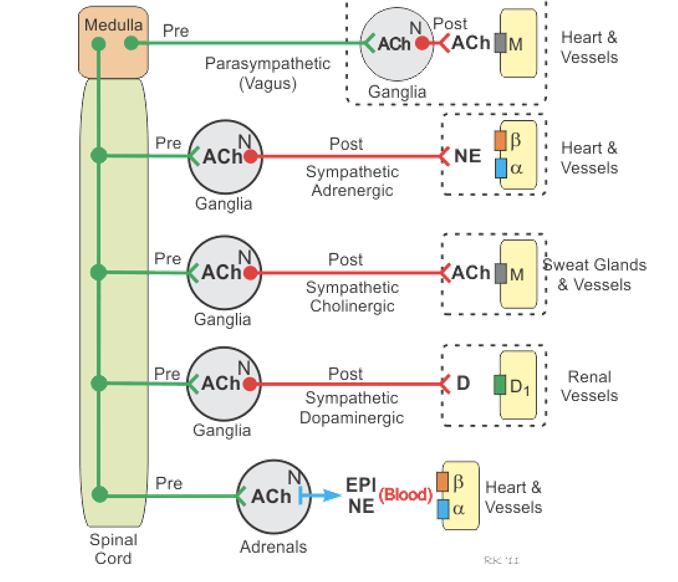
What are the 3 classes of non-catecholamines? How do they work?
direct acting: act on receptors directly
indirect-acting: causes NE release or blocks reuptake of NE
mixed-acting: both direct and indirect effects
What are examples of direct-acting non-catecholamines? What receptors do they activate? (3)
albuterol- beta 2
clonidine- alpha 2
phenylephrine- alpha 1
What are examples of indirect-acting non-catecholamines? What receptors do they activate?
tyramine- alpha 1&2, beta 1
amphetamine- alpha in CNS, beta 1; can also cause dopamine and serotonin (5-HT) release centrally
What is an example of mixed-acting non-catecholamines? What does it do?
ephedrine: alpha in CNS, beta, and NE release
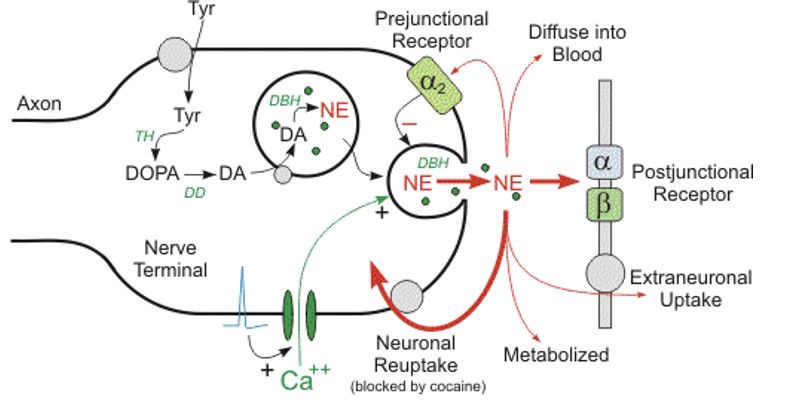
Norepinephrine release is dependent on __.
calcium
NE release can have 5 paths. What are they?
activation of postjunctional receptor (alpha and beta receptors)
extraneuronal uptake
diffuse into blood
metabolized
neuronal reuptake
prejunctional receptor (alpha 2): inhibits NE release
What pharmacologic effects do catecholamines have? (3)
no direct central effects (meaning have no effect in CNS)
not effective orally (bc rapidly broken down, don’t usually make it to target area)
short-acting (bc have efficient rapid reuptake and metabolic mechanism)
What pharmacologic effects do non-catecholamines have? (4)
many have central effects
many are effective orally
many are longer acting
many are more selective in action
How do indirect-acting sympathetics have a role on NE?
enhance release of NE, decrease its reuptake, or decrease its metabolism
**NE needs to be present to produce effects
Why do catecholamines have no direct central effects?
they are polar, aqueous, and soluble —> can’t cross the blood brain barrier
Responses to administration of sympathomimetic drugs are influenced by: (5)
influence of route of administration
distribution of drug
receptors activated
autonomic nervous system adjustments
tachyphylaxis with indirect-acting drugs (tachyphylaxis = sudden dec in receptor response)
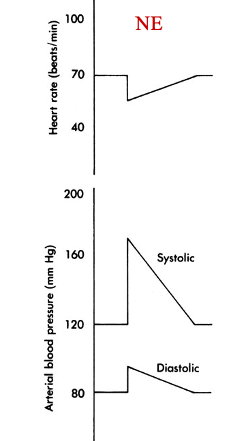
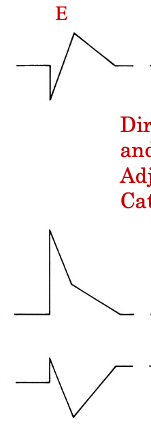
How does NE affect heart rate, systolic pressure, and diastolic pressure? Why?
decreases heart rate, inc systolic and diastolic pressure
alpha receptors —> increase systolic and diastolic BP
baroreceptor reflex —> bradycardia (decreased heart rate)
despite beta 1 receptor activation which tends to increase heart rate
baroreceptor reflex is activated by an increase in BP (it’s the compensatory mechanism for BP increase)
How does epinephrine affect heart rate, systolic pressure, and diastolic pressure? Why?
initially: heart rate dec, systolic and diastolic BP increase
same initial response as NE bc activation of alpha receptors & baroreceptor reflex
then: heart rate increases, systolic and diastolic bp decrease
beta 2 receptors causes vasodilation —> decreased diastolic BP
beta 1 receptors —> increase heart rate
returns back to baseline
Alpha 1 and alpha 2 cause __.
vasoconstriction
How is epinephrine and levonordefrin used in dentistry? Why?
added into local anesthetics
anesthetics on their own cause vasodilation, which increases redistribution away from site of intended action & increases bleeding —> vasoconstrictors like epinephrine & levonordefrin oppose the vasodilation
—> increases duration & efficacy, delayes and reduces blood levels, causes local hemostasis (helps bleeding stop)
In refractory asthma and anaphylactic shock, __ can be used as a treatment.
epinephrine
How do receptors activated in epinephrine relate to CV effects?
alpha 1 & some alpha 2 —> peripheral vasoconstriction —> increases BP
beta 1 —> increased heart rate and force of cardiac contraction
beta 2 —> vasodilation in skeletal muscle —> decreases BP
Epinephrine’s CV effect depends on __.
adrenoreceptor subtype activation
Levonordefrin in the CV system can increase __ due to __ receptors. This causes reflex __.
blood pressure; alpha; bradycardia
Sometimes, __ is preferred over epinephrine because of less changes in __.
levonordefrin; heart rate
What precautions must be considered when using catecholamines, like epinephrine, clinically? (2)
if pt has cardiovascular disease, excessive CV stimulation can cause HTN, arrhythmias, stroke, myocardial infarction
central acting sympathomimetics can also result in excessive CNS stimulation, causing tremors, seizures, psychotic reactions
What drug interactions are present for catecholamines? (3) What do they do?
NE reuptake inhibitors (antidepressants, amphetamines, ADHD meds)
COMT (catechol-o-methyl-transferase) inhibitors (common in parkinson’s)
adrenergic antagonists
these can make sympathomimetic effects of epi or levonordefrin more enhanced
Antidepressants that inhibit the reuptake of serotonin and norepinephrine can be thought of as __.
indirectly-acting sympathomimetic drugs (enhance actions of epinephrine or levonordefrin by blocking NE)
The metabolic inactivation of most injected catecholamines depends on __.
COMT
What are 5 therapeutic uses for catecholamines?
vasoconstriction (alpha receptors)
cardiac stimulation (beta receptors)
bronchial dilation (beta 2)
ocular effects (alpha 1)
CNS effects (alpha, D)
Alpha receptors allow for __ in therapeutic uses.
vasoconstriction
Beta receptors allow for __ in therapeutic uses.
cardiac stimulation (in bradycardia, hypotension)
What effect do alpha receptor antagonists have?
vasodilation
What effect do B1 & B2 receptor antagonists have?
decreased HR
When effect do beta 1 receptor antagonists have on the kidney?
decreased renin release
In benign prostatic hyperplasia (BPH), beta 1 blockade leads to__.
relaxation of prostatic smooth muscle
How does beta 1 receptor antagonists affect blood pressure?
decreases BP by decreasing HR & contractility & decreasing renin release
How do nicotinic-receptor antagonists decrease hypertension?
block parasympathetic and sympathetic outflow —> ANS can’t regulate blood pressure —> decreases heart rate & constriction of blood vessels
How do drugs that reduce adrenergic transmission decrease hypertension?
decrease synthesis, prevent release, or deplete norepinephrine from adrenergic terminals
Centrally acting drugs reduce hypertension by:
reducing sympathetic outflow
What are the two classes of alpha receptor antagonists? Give examples of both.
nonselective
phentolamine (reversible)
phenoxybenzamine (irreversable)
selective
prazin, doxazosin, terazosin
What are potential uses of alpha blockers? (5)
hypertension
benign prostatic hyperplasia
pheochromocytoma
male impotence
reversal of local anesthesia
Limitations of __ include: orthostatic hypotension, reactive tachycardia, intraoperative floppy iris syndrome.
nonselective alpha blockers
Limitations of __ include orthostatic hypotension in Prazosin and cardiovascular stimulation or anxiety in Yohimbine.
selective alpha blockers
What are the 4 classes of beta receptor antagonists?
nonselective (Beta 1&2)
cardioselective (mainly beta 1)
beta blocker with intrinsic sympathomimetic activity (partial agonists)
alpha 1 and beta receptor blockers
What are partial agonists?
drugs taht bind to and activate a given receptor but only have partial efficacy at the receptor compared to a full agonist
When are partial agonists used?
used to activate receptors to give submaximal responses when insufficient endogenous ligand is present or to reduce overstimulation of receptors when excess endogenous ligand are present
__ is used for: hypertension, angina pectoris, cardiac arrhythmias, myocardial infarction, congestive heart failure, glaucoma, migraine headache, thyrotoxicosis, stage fright, or tremors.
beta receptor antagonists
The limitations of __ include: congestive heart failure, bronchial asthma, insulin-dependent diabetes and hypoglycemia, and rebound hypertension.
beta receptor antagonists
What two vasoconstrictors have interactions in dental local anesthetics?
non-selective beta blockers
alpha blockers
In the sympathetic nervous system, alpha 1 and some alpha 2 receptors cause __, which increases __.
vasoconstriction; blood pressure
vasoconstricted blood vessels = narrower = higher pressure and force needed to pump blood
In the sympathetic nervous system, beta 1 receptors increase __.
heart rate and force of contraction
In the sympathetic nervous system, beta 2 receptors cause __ in the skeletal muscle, which decreases __.
vasodilation; blood pressure
What do non-selective beta blockers block? What is an example?
both beta 1 and 2
ex: propranolol, nadolol, timolol
What do cardioselective beta blockers block? What is an example?
beta 1 only
ex: atenolol, metoprolol
What is an example of combined alpha and beta blockers?
labetalol, carvedilol
How is blood pressure or heart rate affected in non-selective beta blocker interactions?
increased blood pressure —> hypertension and reflex bradycardia
beta blocker = blocks beta 1 (increases HR) and beta 2 (decreases BP)
There is likely no __ with cardioselective beta1 agents or combined alpha and beta blockers.
interaction
In an alpha blockade, how is heart rate and blood pressure affected? What is this called?
increased heart rate (from beta1), decreased BP (from beta2) —> hypotension & tachycardia
called epinephrine reversal
What are alpha blockers mainly used for?
BPH (benign prostatic hyperplasia)
What are 3 types of alpha blocking drugs?
alpha blockers (prazosin)
phenothiazines (thorazine)
butyrophenones (Haldol)
What adrenergic agonist is really an antagonist?
alpha-2 agonists (prejunctional receptor)
What do alpha-2 agonists do?
decrease overall sympathetic tone by decreasing release of natural NT from presynaptic terminals
__ is used for hypertension, opioid withdrawal, analgesia/anesthesia, and to counteract amphetamine insomnia.
alpha2 agents
Clonidine, dexmedetomidine, guanfacine, guanabenz, alpha-methyldopa are examples of __ agents.
alpha 2
The limitations of __ agents are cardiovascular depression, somnolence, rebound hypertension with cessation of therapy.
alpha 2