AMI - Lecture 5 - Immunometabolism
1/9
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
10 Terms
Describe the M1 state of macrophages
M1 → host defense, pro inflammatory, kills tumor cells, chronic inflammation, short lived
metabolism;
rely on glycolysis to produce ATP
TCA cycle broken at specific points (isocitrate dehydrogenase) → leading to intermediates used for inflammatory molecules.
Less fatty acids produced than M2.
some AA made
Explain the M2 stage of macrophages
M2 → homeostasis, slow, anti inflammatory, tissue repair, wound healing, promote tumor growth, long lived
metabolism;
cells rely on oxphos for sustained ATP,
glycolysis downregulated,
TCA cycle active → support oxphos
PPP active (NADH production)
fatty acid synthesis (membrane repair)
aa production
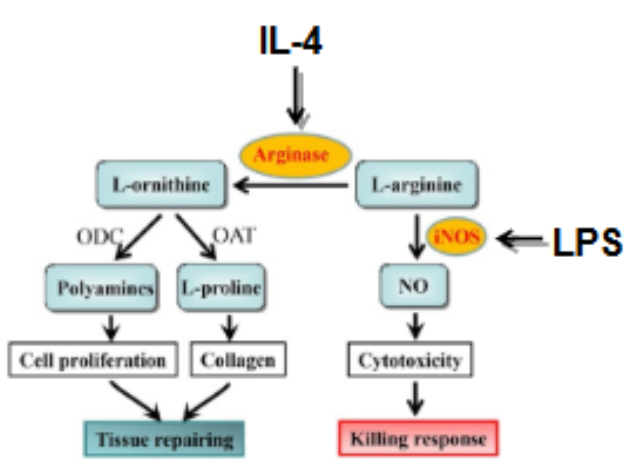
Explain the arginine metabolism in M1 and M2
the balance between inducible nitric oxide synthase (iNOS) and arginase is how you determine if MQ are in M1 or M2 phase
M1 → iNOS is dominant, iNOS converts L-arginine into nitric oxide (NO), NO plays microbial + tumor killing role
in M1 the aa metabolism supports proliferation + NO production
LPS promotes M1
M2 → arginase dominance, arginine metabolizes L-arginine into → ornithine + urea
ornithine further used to produce → proline + polyamines (both needed for tissue repair + cell proliferation)
aa metabolism in M2 supports arginine pathway activity
IL4 is anti inflammatory, promotes M2
GAPDH importance in M1, M2
M1 → increased GAPDH supports glycolysis, powers pro inflammatory responses
M2 → decreased reliance on GAPDH, because M2 is dependent on OXPHOS + TCA
GAPDH activated when there is stress / cellular damage
GAPDH → key enzyme in glycolysis
in resting MQ low glycolysis → GAPDH present, can bind mRNA in T cell → mRNAs not translated into pro inflammatory cytokines
When t cell / MQ is activated → GAPDH will be post translationally modified → mRNA will be translated → pro inflammatory cytokines formed (TNFalpha, IL1beta)
explain the broken TCA cycle in M1 in more detail
disruption TCA cycle leads to → accumulation succinate + citrate
citrate drives production NO + inflammatory mediators
succinate stabilizes HIF1alpha, this promotes expression of glycolytic enzymes + inflammatory genes (IL1beta)
succinate is secreted by M1 and reuptaken through GPR91 receptor → GPR91 activation amplifies inflammatory response.
when GPR91 receptor (succinate) was knocked out → tissue inflammation reduced in arthritis.
thus broken TCA cycle → fuel the glycolytic + pro-inflammatory metabolism of M1
What role does itaconate play in macrophage metabolism
itaconate is derived from citrate in LPS activated MQ.
it exhibits anti inflammatory + antimicrobial properties
it’s produced when citrate accumulates in cytosol by enzyme IRG1
IRG1 KO MQ → itaconate production absent → inflammatory response
normal MQ itaconate produced → tempering of inflammatory response
Explain the 4 mechanisms through which itaconate work
itaconate inhibits succinate dehydrogenase (under debate) leading to less succinate accumulation → no stabilization HIF1alpha → less inflammation
itaconate activates NRF2 by freeing it from KEAP1, resulting in NRF2 moving to nucleus → initiating transcription of anti oxidant + anti inflammatory genes → protects MQ from damage ROS
itaconate inhibits bacterial enzymes (isocitrate lyase) preventing bacterial survival
itaconate activates MAPK pathway leads to expression of ATF3. this is a transcription factor known to suppress pro inflammatory genes (IL1)
NRF2 activation also promotes transcription of ATF3
Explain how the seahorse extracellular flux analysis is used for studying cellular metabolism
can be used to differentiate between M1 and M2 state
ECAR → reflects glycolysis rate by measuring protein production
increase ECAR, increase glycolysis (more CO2 + lactate)
M1 → increased ECAR
M2 → lower ECAR
OCR (oxygen consumption rate) → reflects oxphos by measuring the rate at which O2 is consumed
M1 → low OCR, NO production inhibits mitochondrial respiration, thus M1 rely on glycolysis
M2 → high OCR, depend on OXPHOS
adding glucose to seahorse → increase ECAR in M1 MQ
limitations seahorse → AA metabolism not directly measured as well as PPP
explain if and how M1 can go to M2 state
M1 → M2 difficult
induced by anti-inflammatory cytokines (IL4, IL13, IL10)
can only be done by iNOS inhibition (reduces level of NO).
this pathway is difficult because M1 have high NO production, this inhibits oxphos (crucial for M2).
need to shift from TCA + glycolysis →oxphos
explain if and how M2 can go to M1 state
M2 → M1 happens more often. M2 relies on oxphos, can switch to aerobic glycolysis under inflammatory stimuli → LPS, IFNgamma
upregulation iNOS → production NO → increased expression pro-inflammatory cytokines