Psych 160D/Bio N165: Exam #3
1/195
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
196 Terms
What are the 3 parts of the somatosensory system?
1) cutaneous senses
2) proprioception
3) kinesthesis
Cutaneous senses
perception of touch and pain from stimulation of the skin

Proprioception
ability to sense POSITION of the body and limbs
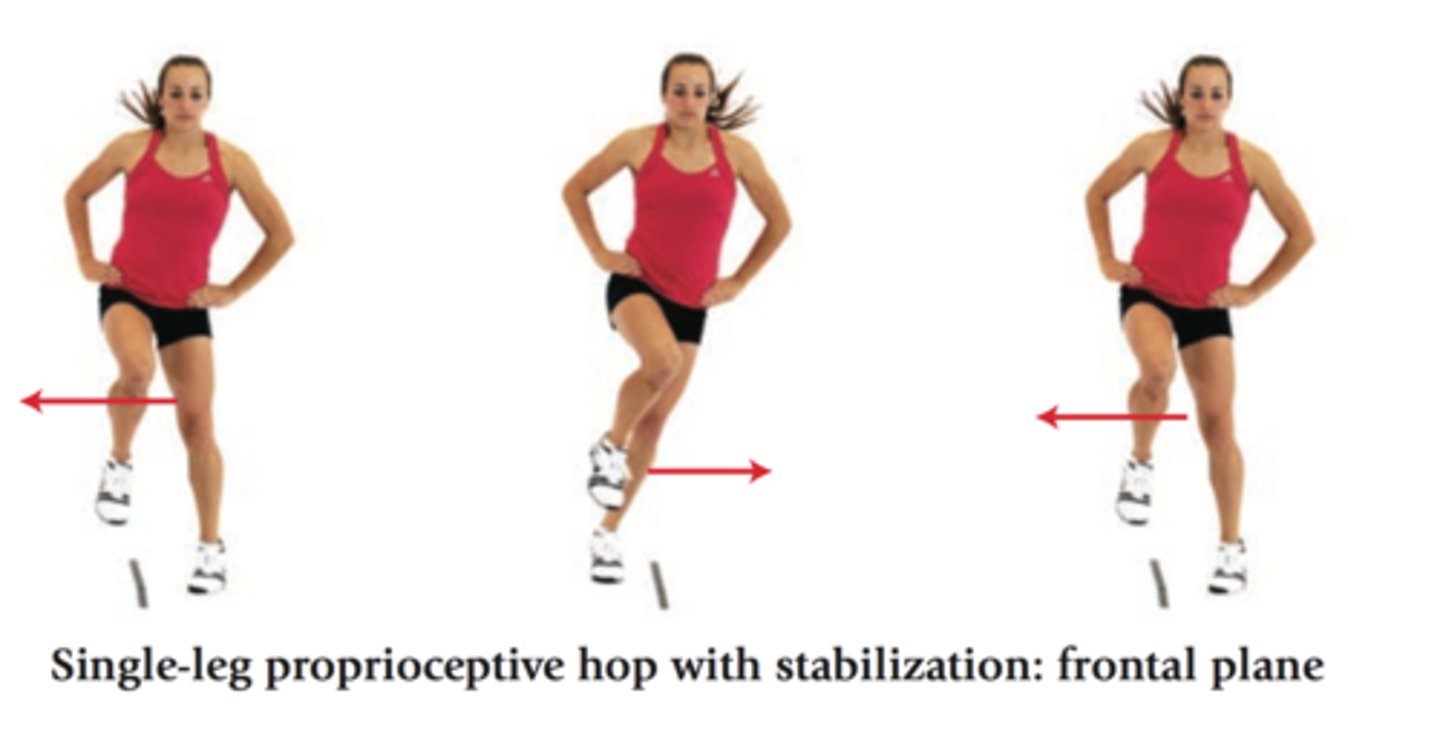
Kinesthesis
ability to sense MOVEMENT of body and limbs
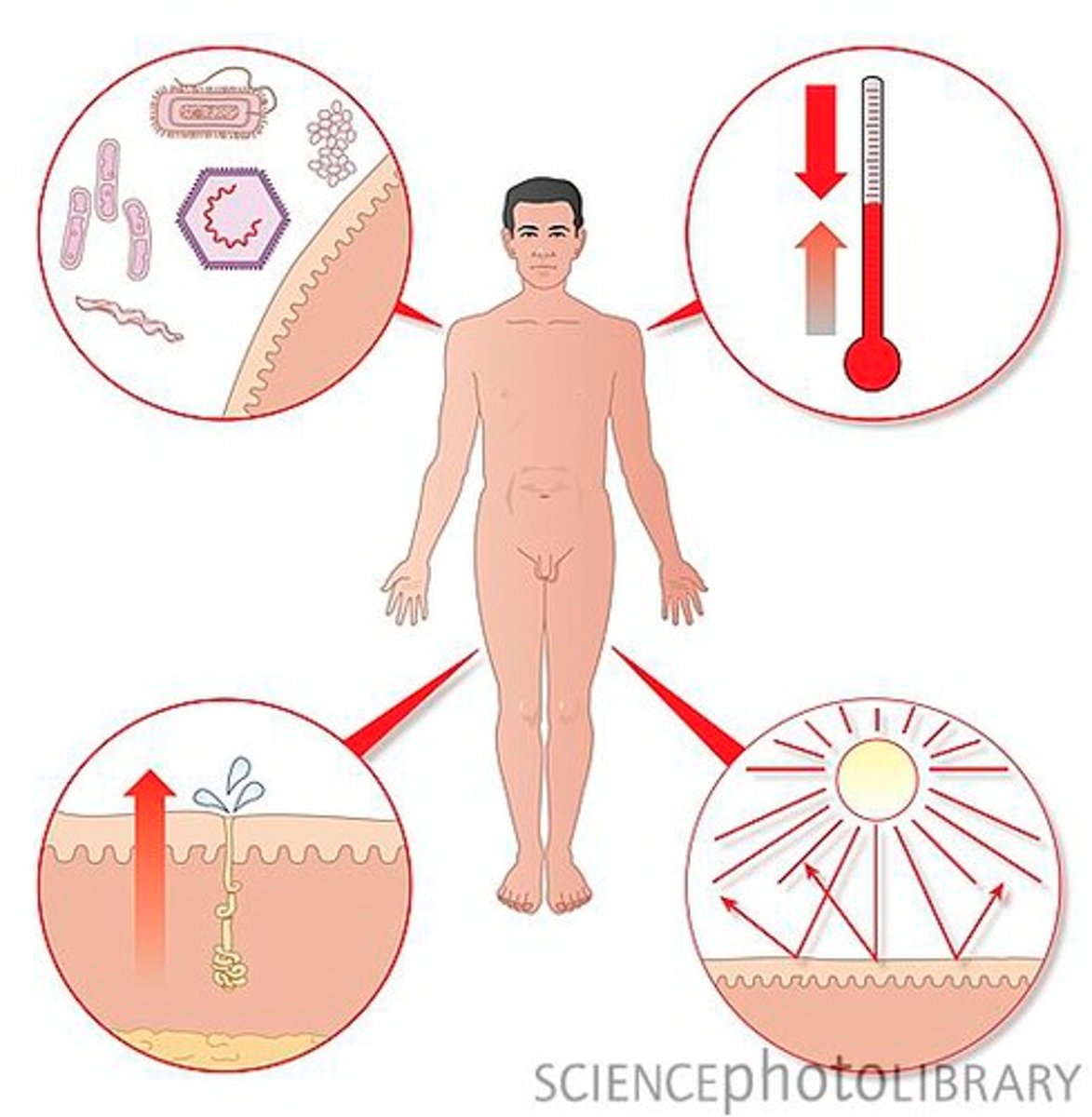
Functions of the skin
- PROTECTION from germs, UV, toxins, etc
- EXCRETION of water/sweat, urea, ammonia, etc
- ENCDORINE; vitamin D production
- REGULATION of temperature and water
- SENSATION; transmits signals to cortex
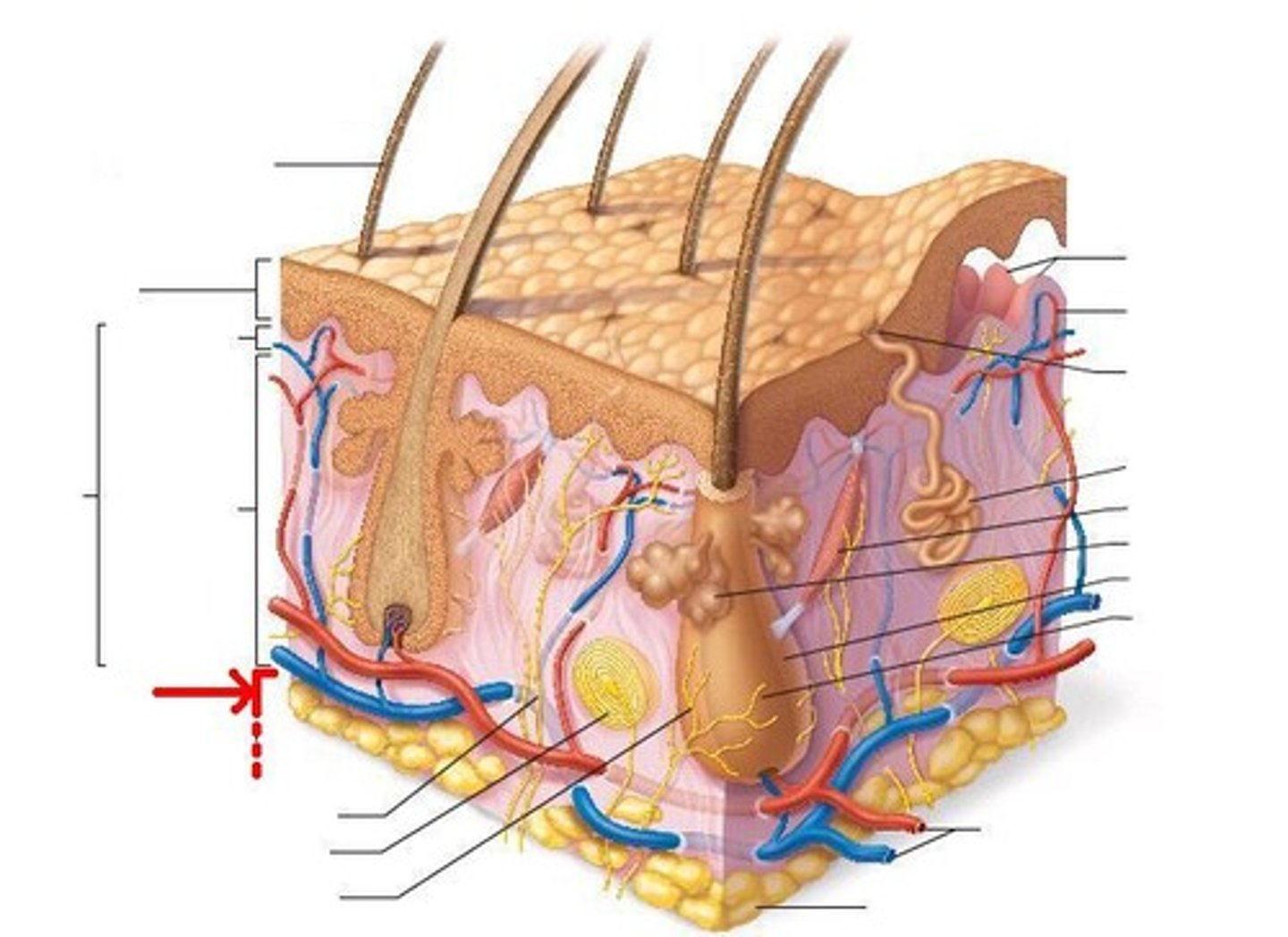
Layers of the skin
Epidermis, basement membrane, dermis, subcutaneous tissue
Epidermis
outermost layer of the skin, mostly composed of dead skin cells
- this is the layer that usually comes in contact with toxins/etc, but the basement membrane protects the dermis from those things
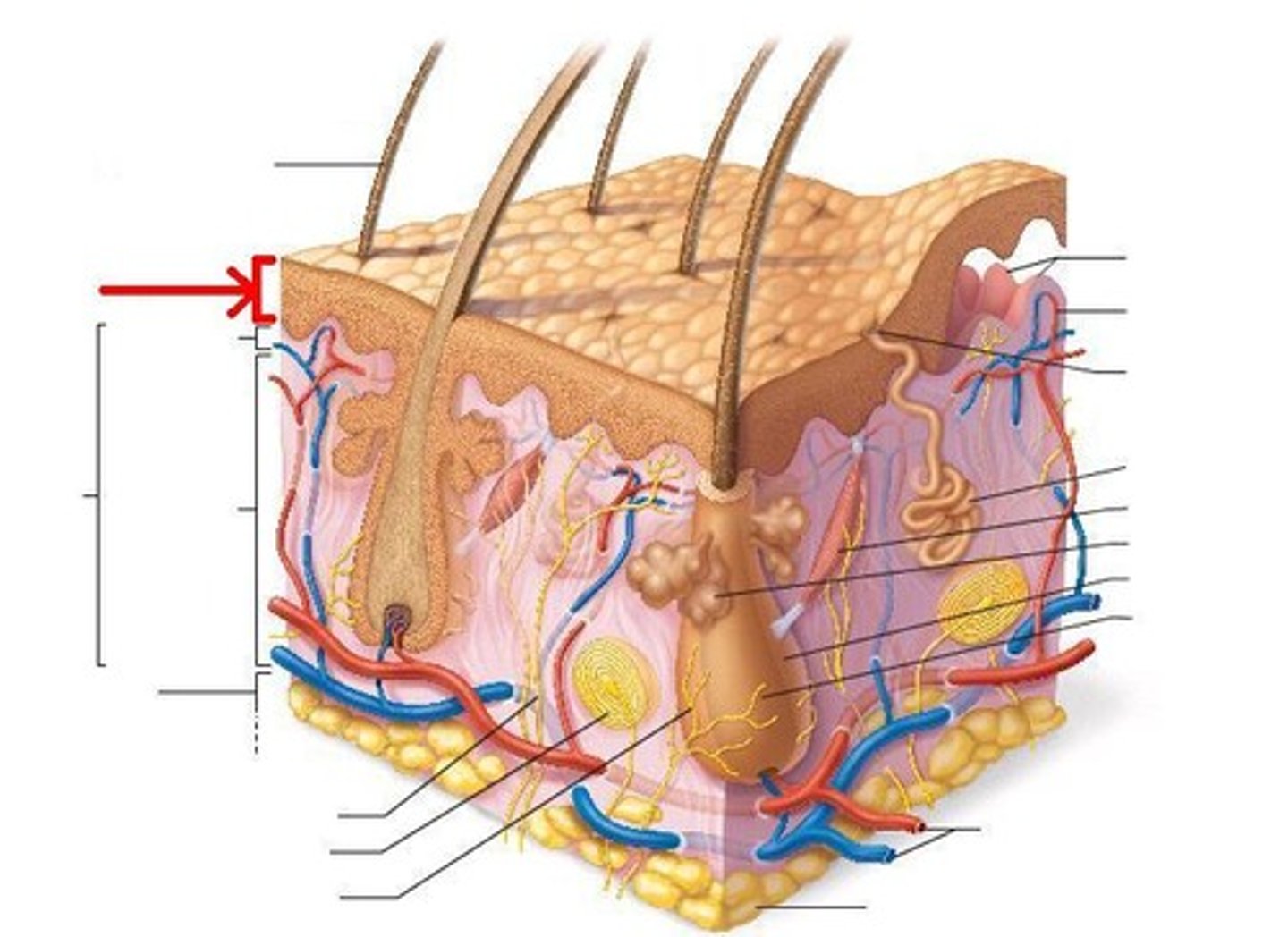
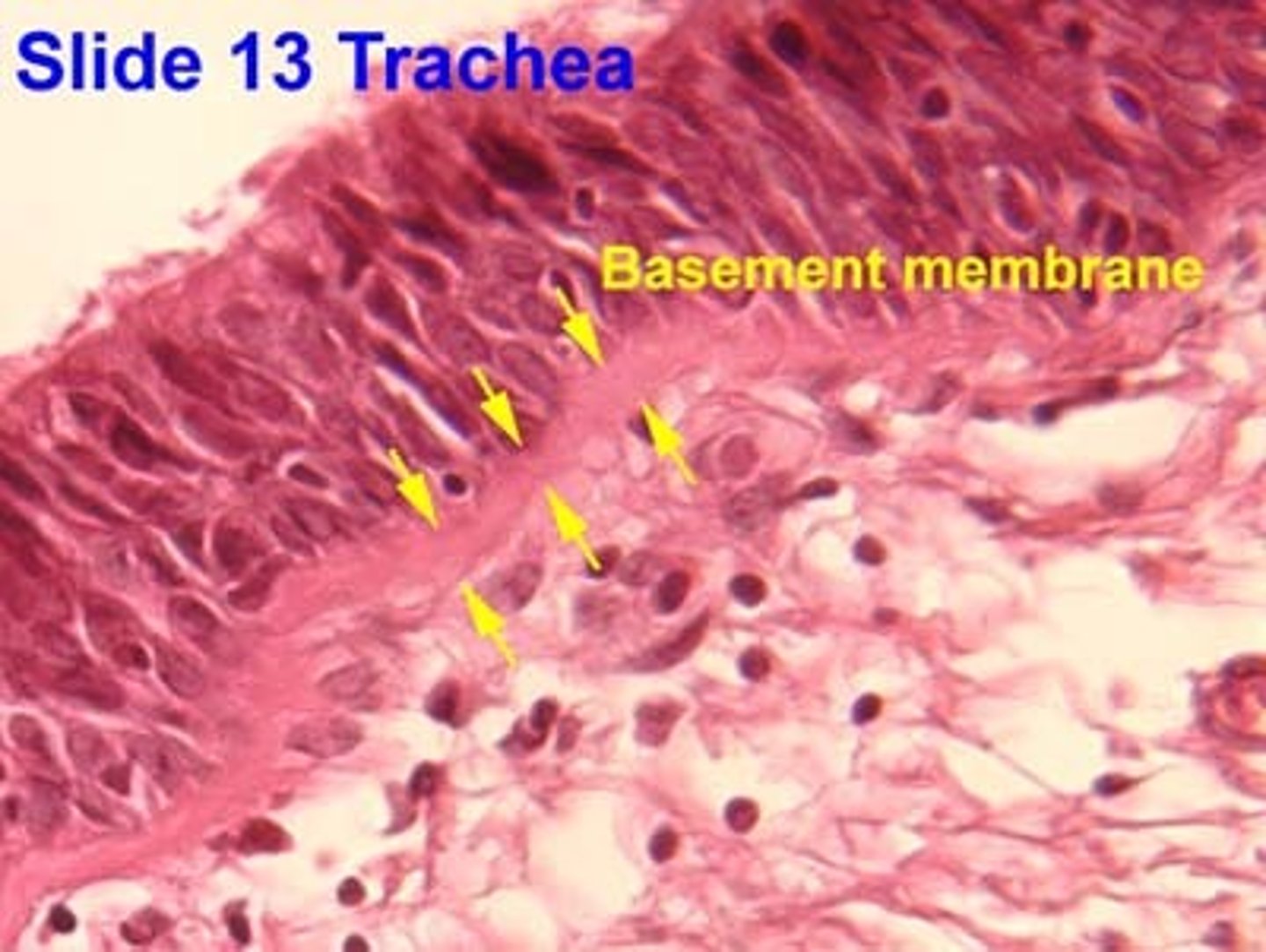
Basement membrane
a thin, specialized structure between the epidermis & the dermis to protect the dermis from outside toxins/UV rays
- kind of like the BBB, but for skin; contains tight junctions & keratinocytes
- once skin cancer surpasses the basement membrane, cancer will spread throughout the body
- if skin cancer is still within epidermis, you can easily cut it out and remove it
Dermis
inner layer of skin where all our receptors, sweat glands, hair follicles, blood capillaries, etc exist; *true skin*
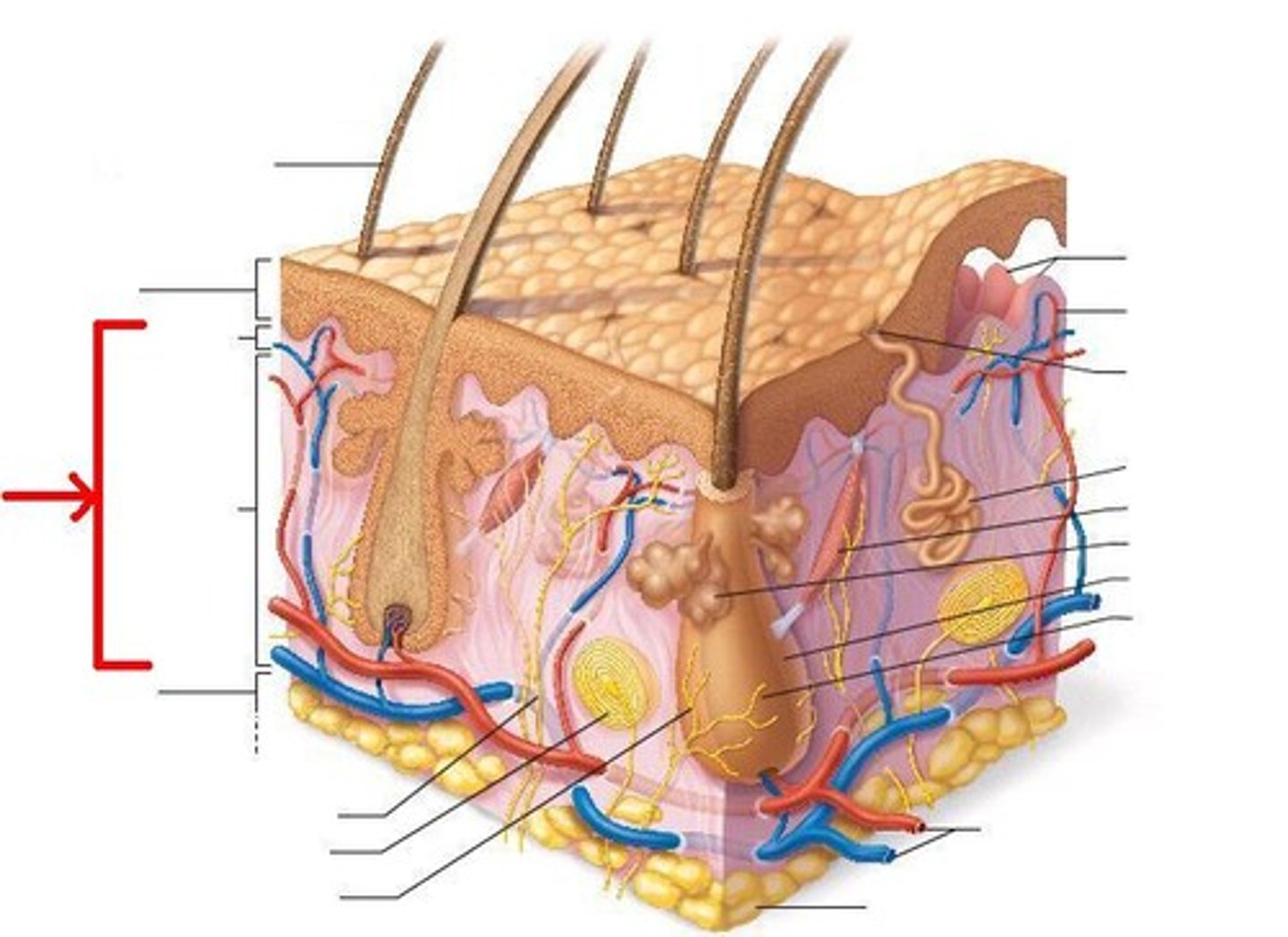
Subcutaneous tissue
deepest layer of the skin; contains vessels, fat, & connective tissue
- *helps regulate temperature!!*
- if you have an eating disorder & lack of fat, cells in subcutaneous layer get too small & therefore cannot properly regulate temperature
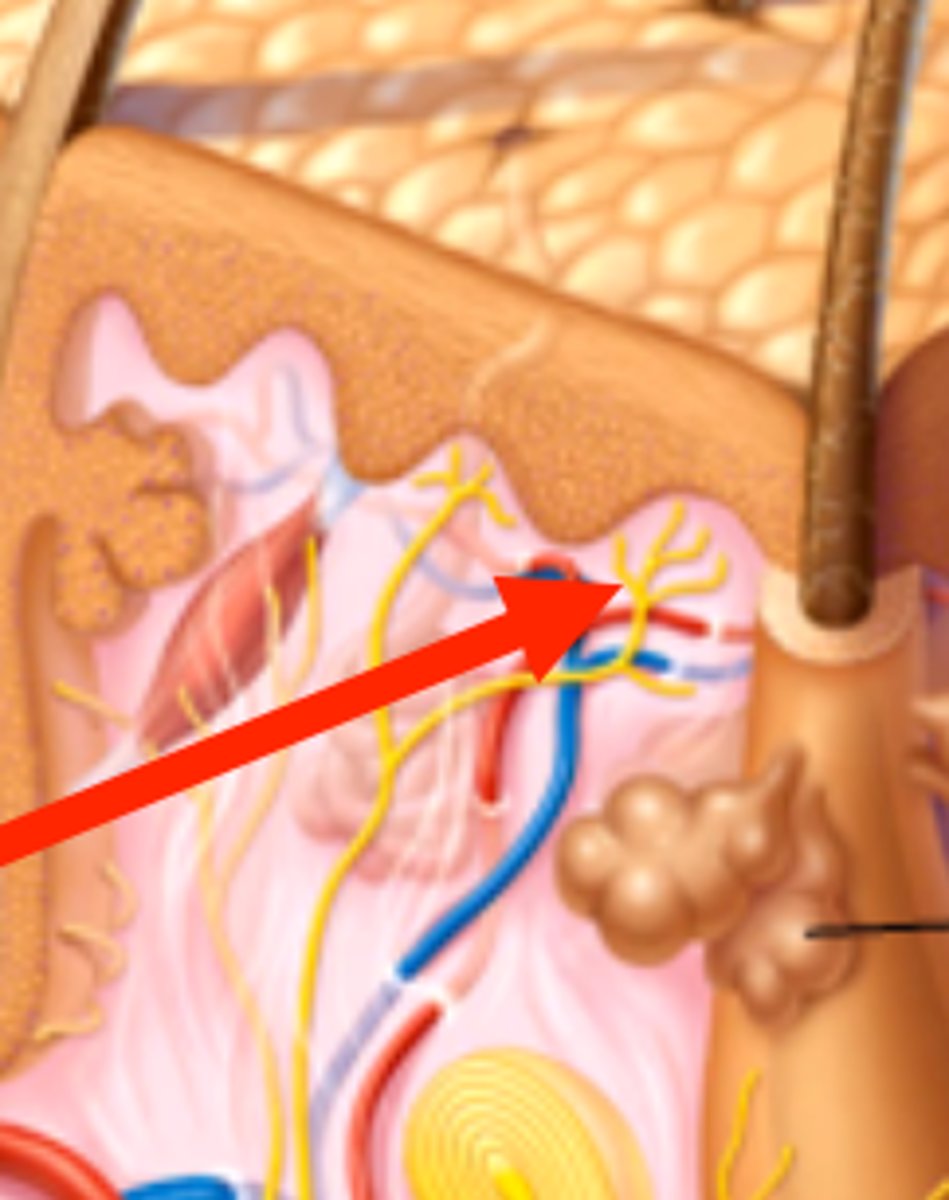
Where is high acuity touch located in the 3 layers of skin?
in the peaks of the dermis, right below the basement membrane
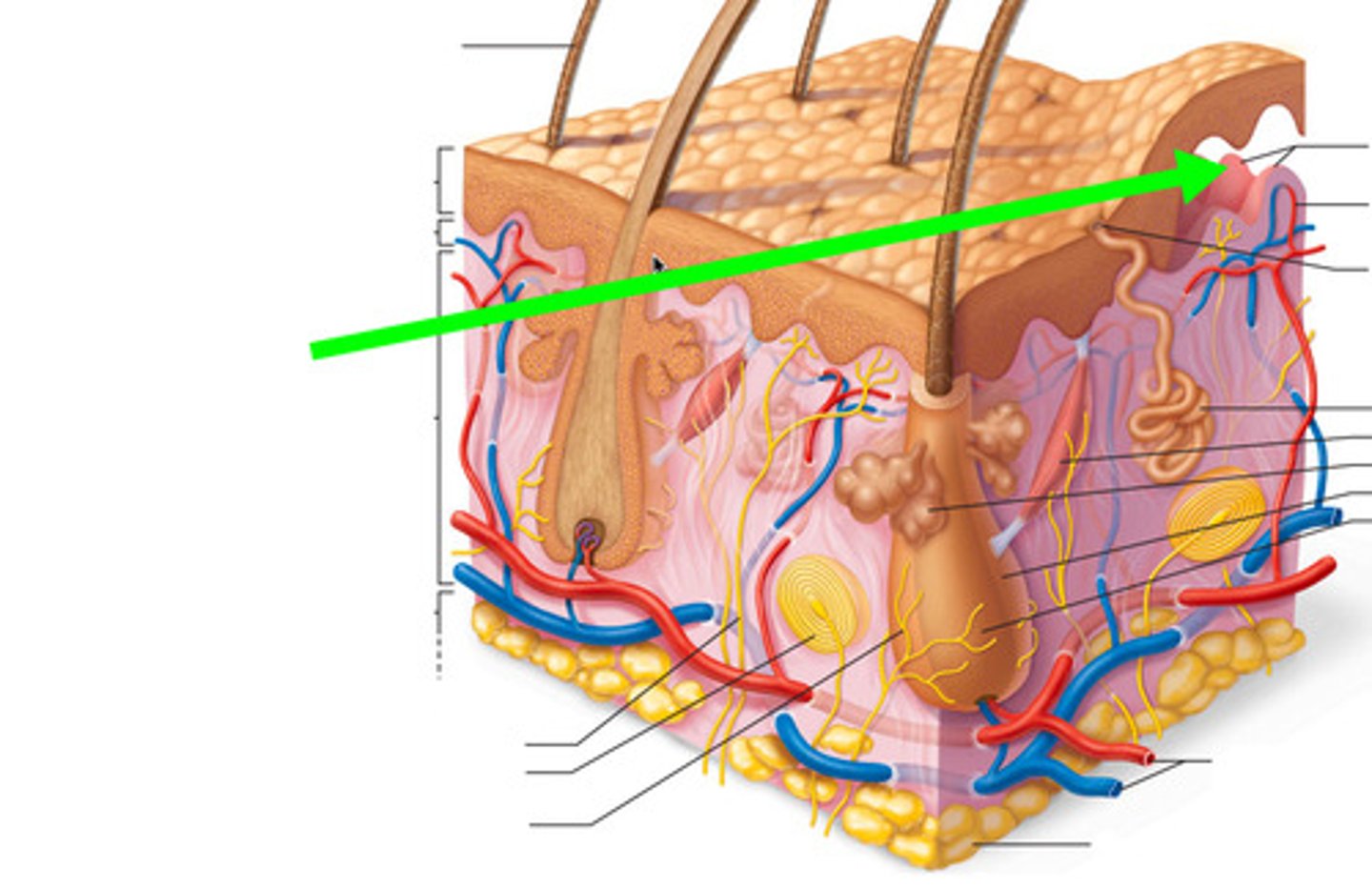
Glabrous skin
hairless skin
- palms
- soles of feet
- lips
- genitals
*more specialized mechanoreceptors!!; meissner, merkel, ruffini, pacinian*
Hairy skin
skin with hair; covers MOST of our body
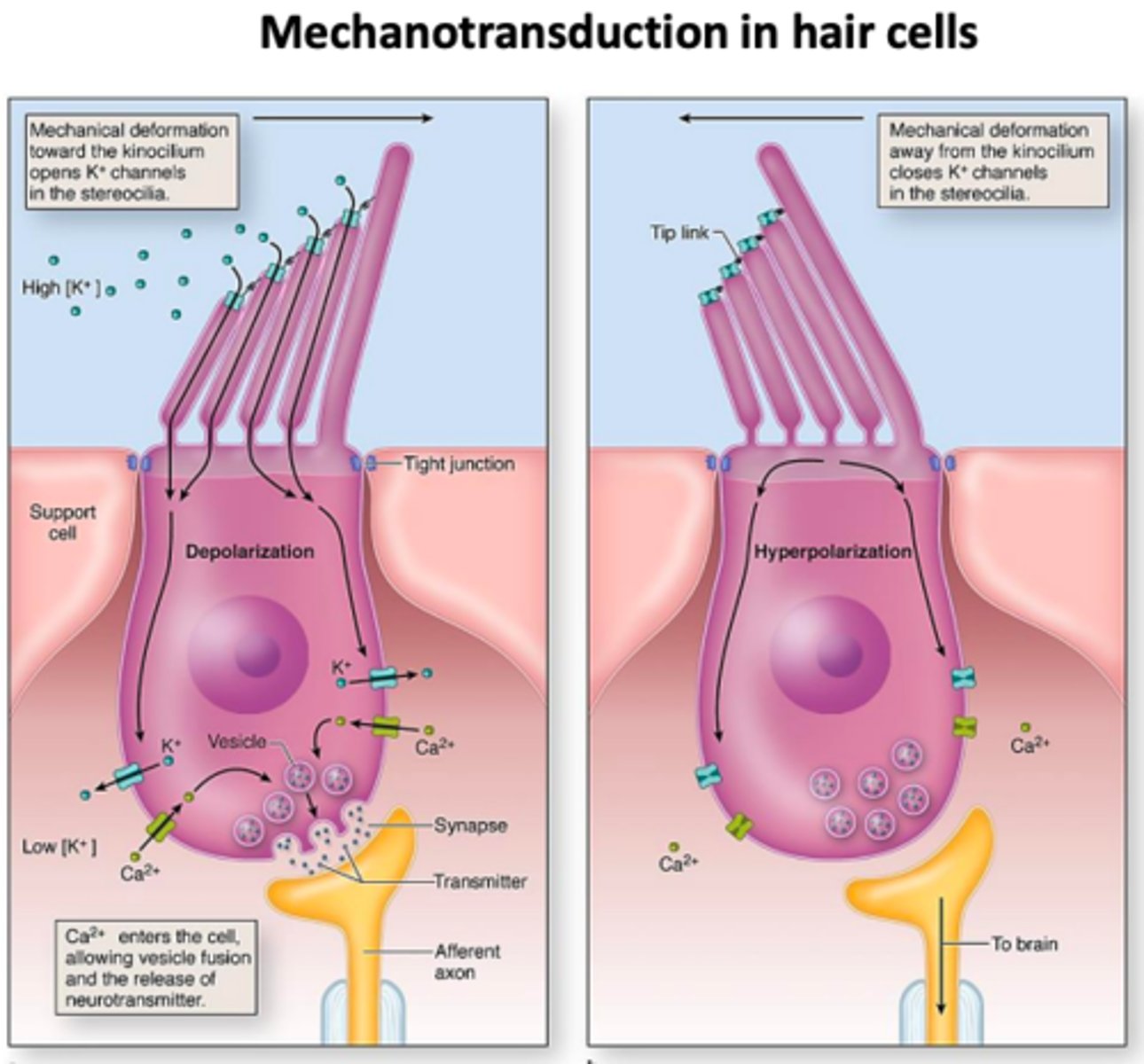
- mechanoreceptor: hair follicle nerve plexus; physical movement of the hair themselves triggers a signal (mechanotransduction)
as hairs move proteins are being pulled open and closed

Mechanoreceptors
receptors that respond to PHYSICALLY pulled open & closed ion channels in the membrane by movement of the hair follicle itself via pressure, touch, etc.
differ in morphology, location in skin, rate of response adaptation, frequency selectivity, spatial receptive field, and perceptual task (fine details, skin stretching)
Somatosensory receptors differ by which of the following characteristics?
a) location in skin layers
b) morphology (shape)
c) perceptual task
d) temporal properties
e) all of the above
e) all of the above
Nerve plexus
group of nerves surrounding the hair follicle
- PRIMARY mechanoreceptor in hairy skin
- triggered via distortion/movement
Upper skin mechanoreceptors
Merkel's disks: top layer of upper skin
Meissner's corpuscles: bottom layer of upper skin
^ BOTH are involved in *high acuity/fine touch*
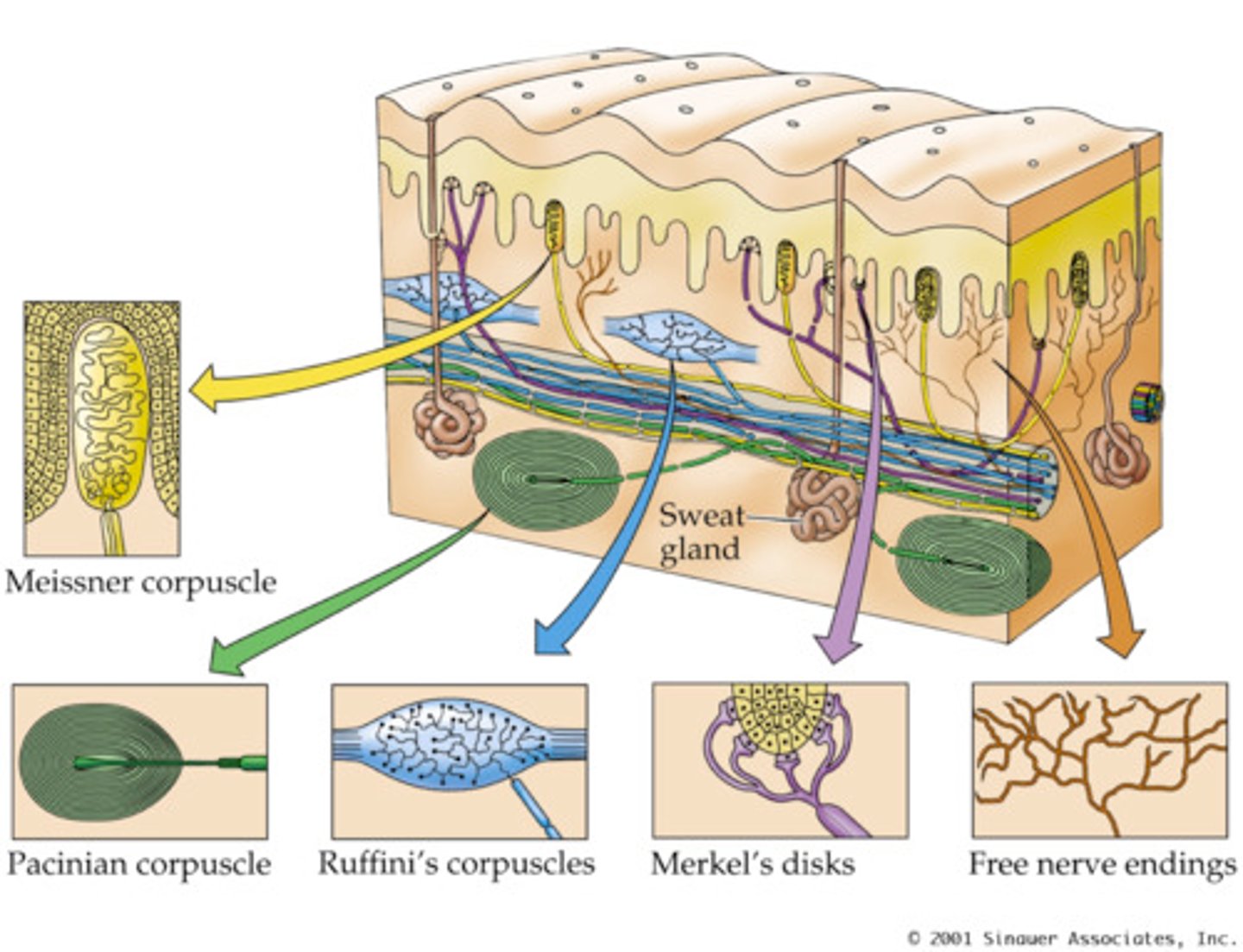
Deeper skin mechanoreceptors
Ruffini cylinders: top layer of deeper skin
Pacinian corpuscles: bottom layer of deeper skin
^ BOTH are involved in *picking up broader distortions/vibrations*’
on/off
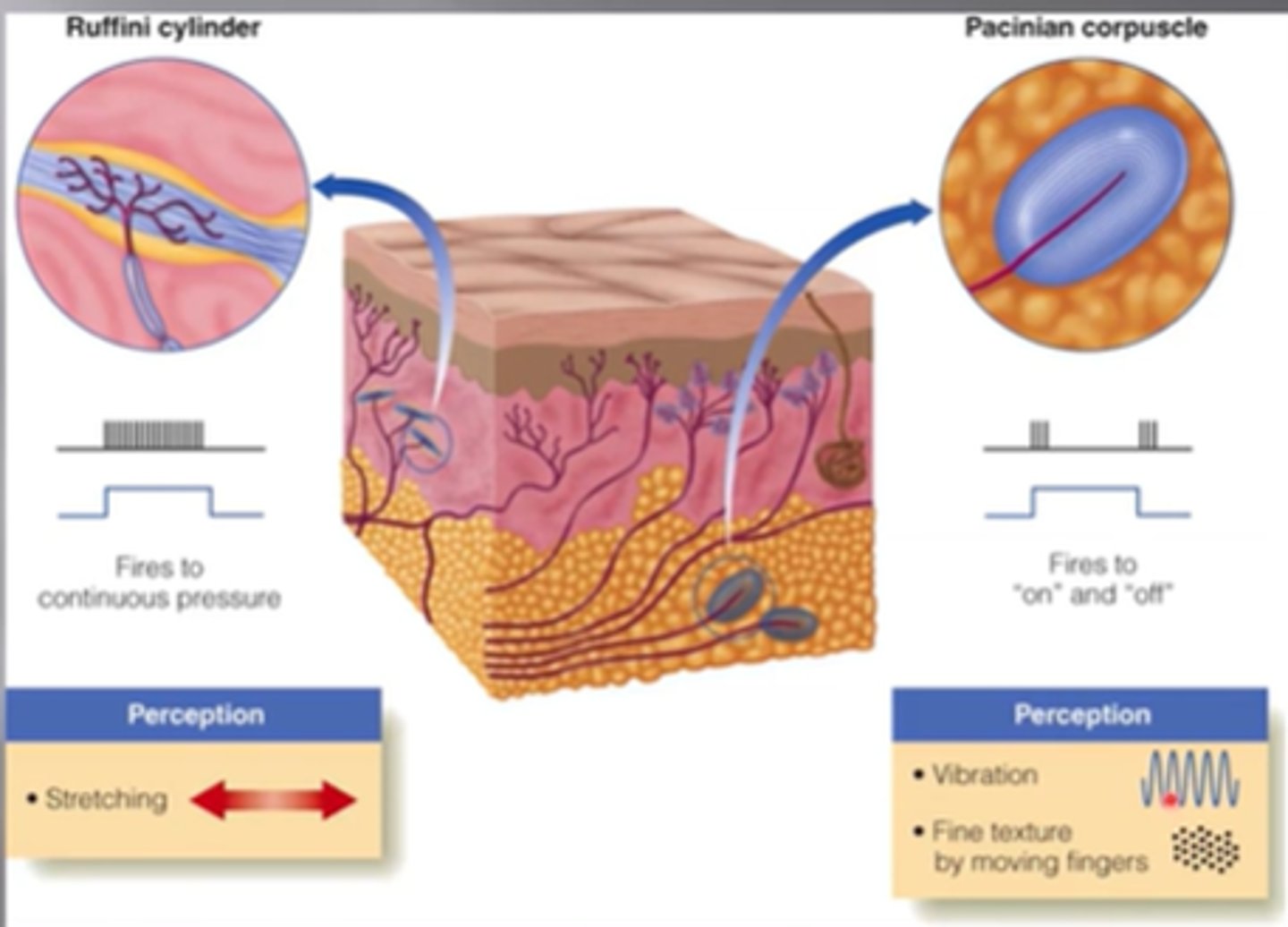
Slowly adapting fibers (SA)
found in top layer of upper skin (Merkel's) & top layer in deeper skin (Ruffini)
- fire CONTINUOUSLY as long as pressure is applied to provide high acuity info
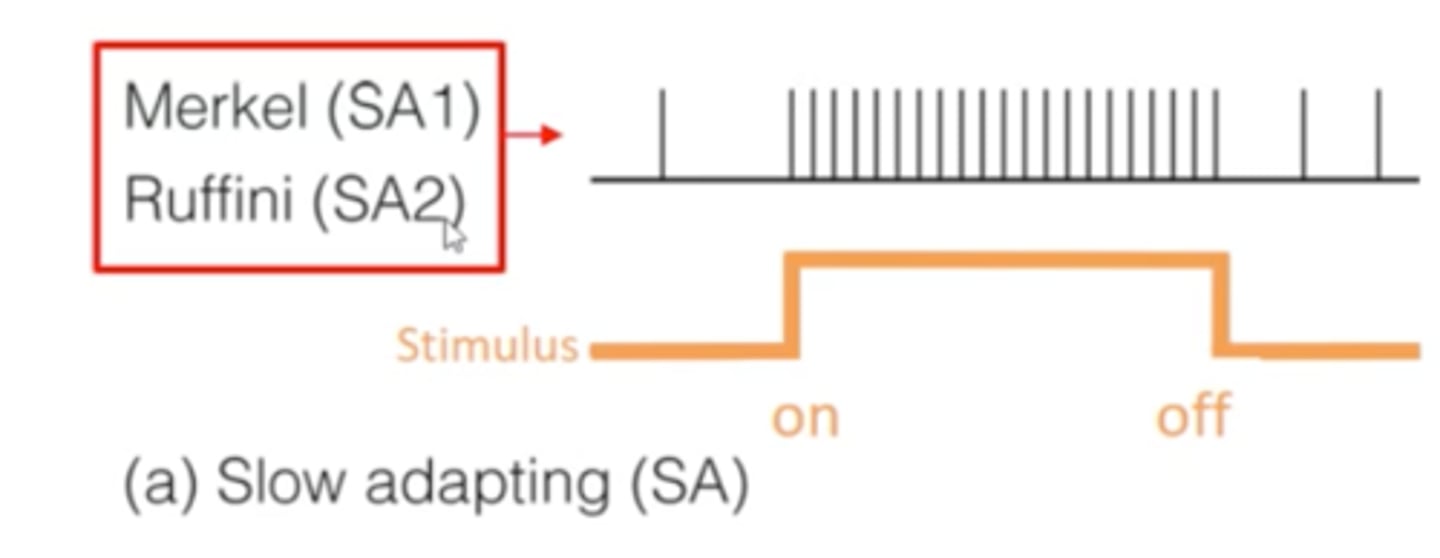
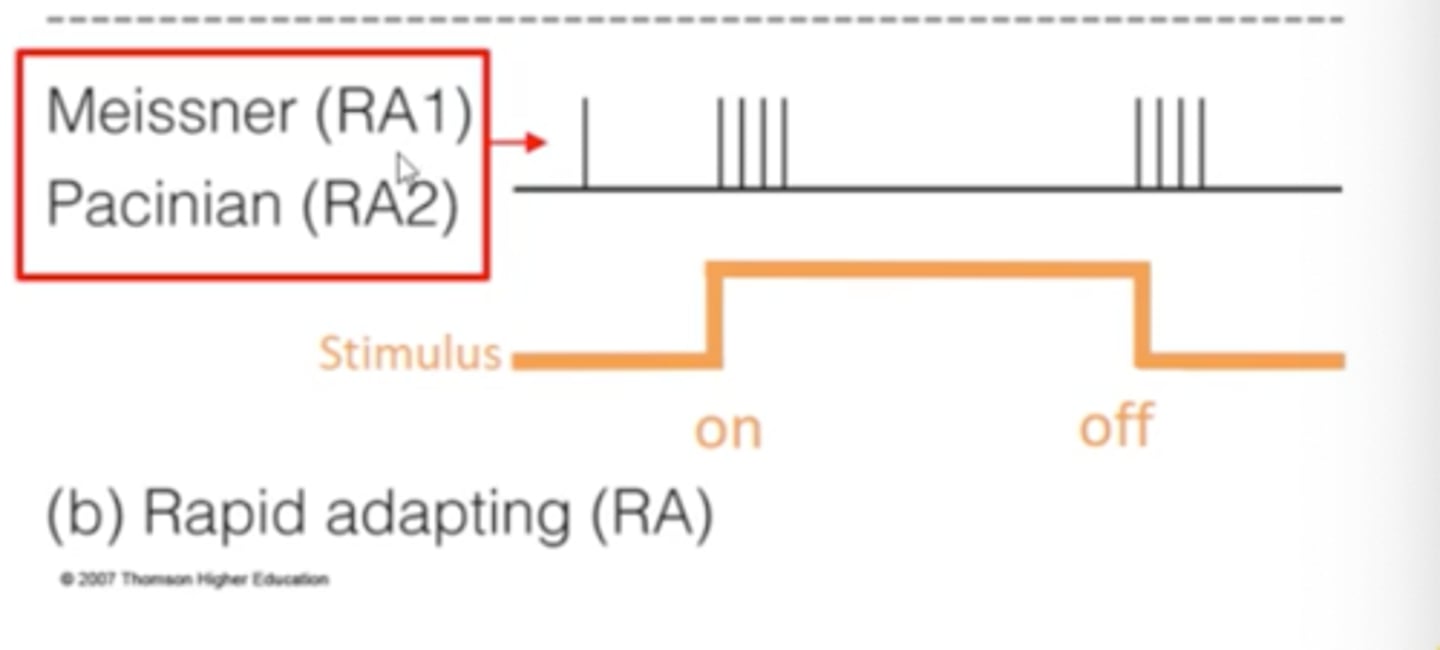
Rapidly adapting fibers (RA)
found in bottom layer of upper skin (Meissner) & bottom layer of deeper skin (Pacinian)
- fire ON/OFF of stimulus; tells us when it starts/stops
- ex: when you put clothes on you are initially aware, after that you are not hyperaware of wearing a shirt --> fire again when you take clothes off
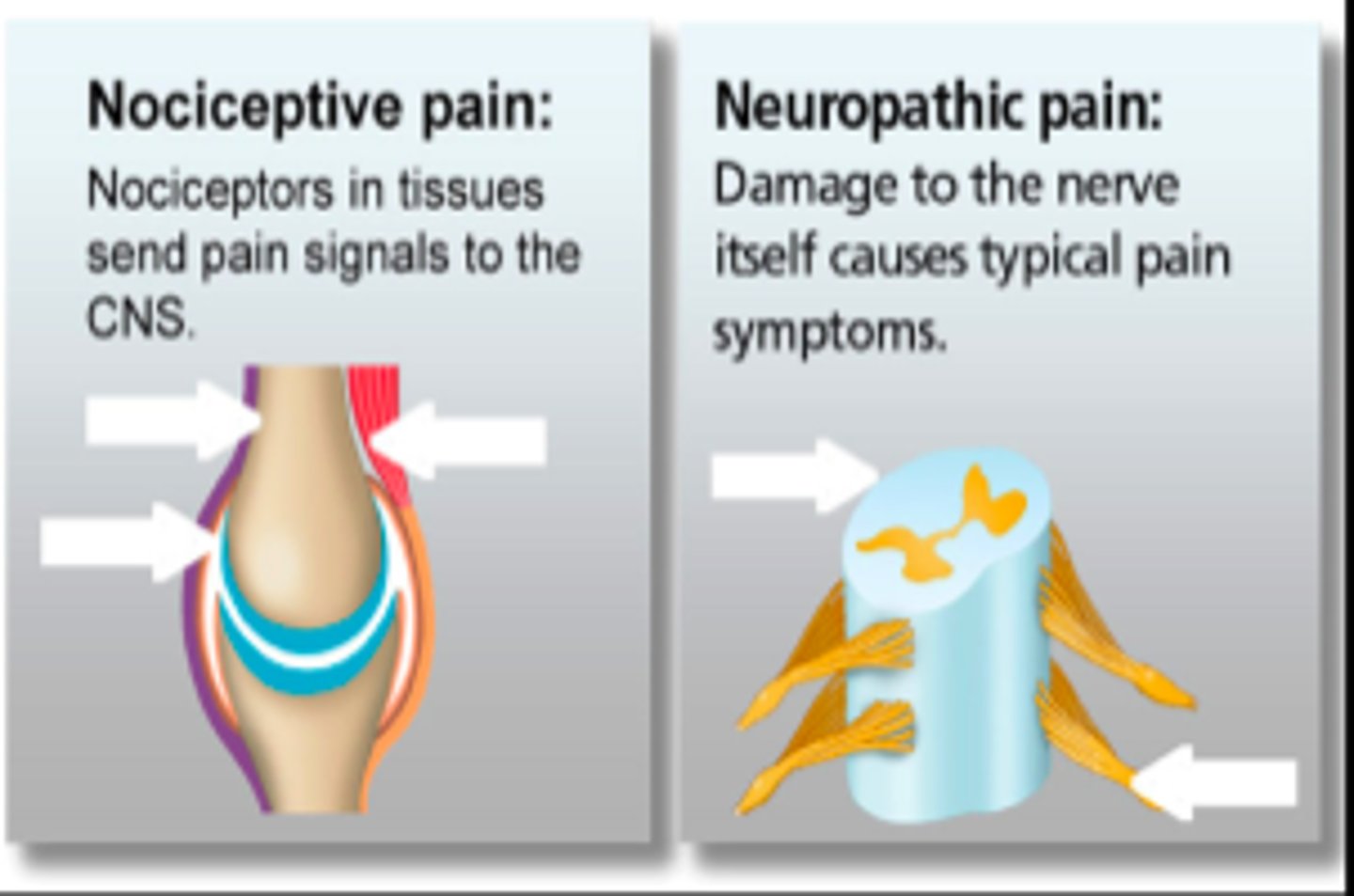
3 types of pain
1. acute nociceptive pain
2. chronic inflammatory pain
3. chronic neuropathic pain
Acute nociceptive pain
RAPID WARNING RELAY
- instructs motor neurons of CNS to minimize the detected physical harm (you're touching something hot, quickly remove your hand!)
- mediated by nociceptors in A-beta & C fibers
QUICK START and end
Nociceptors
free nerve endings just below the skin that help detect cutaneous pain, somatic pain, & visceral pain
- SPECIALIZED for heat, chemicals, severe pressure, cold
^ that's why sometimes something thats really cold can feel like its "burning"
Hot and cold sensations are carried via?
thermoreceptors
Chronic inflammatory pain
damage to tissues/joints that illicits an immune response causing swelling/pain
- immune system responses causes fluid to shift to damaged area causing SWELLING & chemicals are released activating the PAIN sensation
- the longer you are in pain, your system remodels to be MORE SENSITIVE to the pain
immune system overcompensated for pain

Chronic neuropathic pain
damage to neurons in the PNS/CNS themselves = sensitization of these systems
- PERIPHERAL SENSITIZATION: increase in stimulation of peripheral nociceptors = amplified pain signals
- CENTRAL SENSITIZATION: hyperstimulation of dorsal horn neurons = amplified pain
damage to nerves themselves rather than tissues
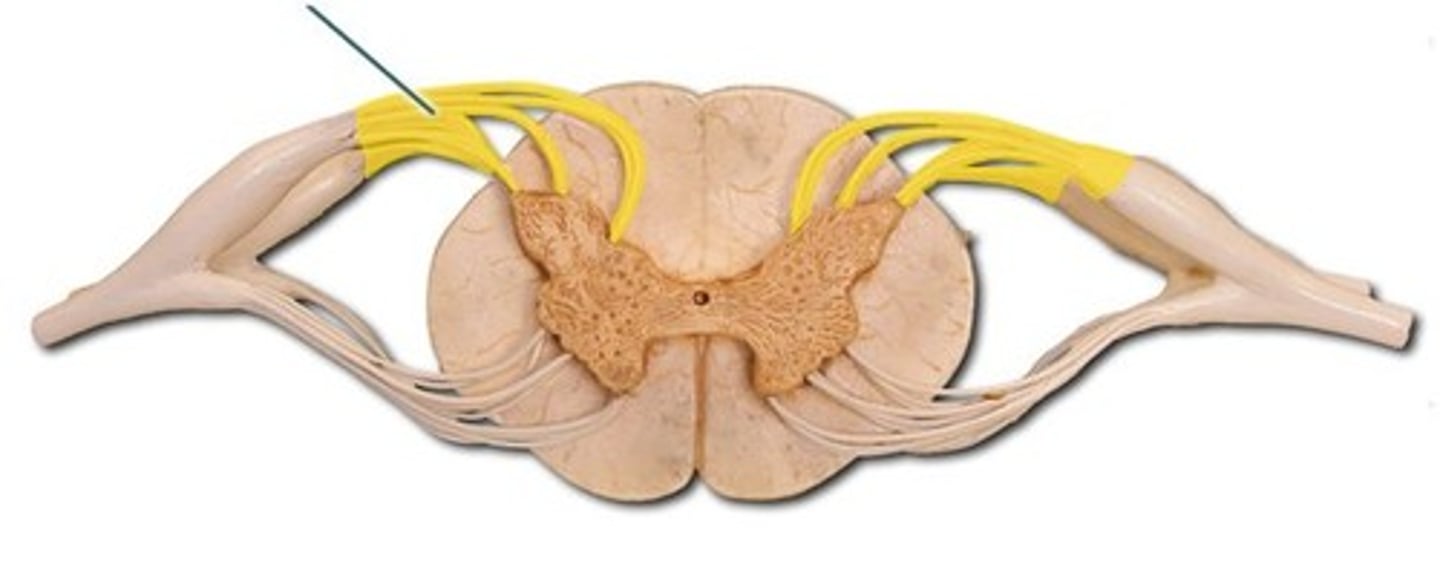
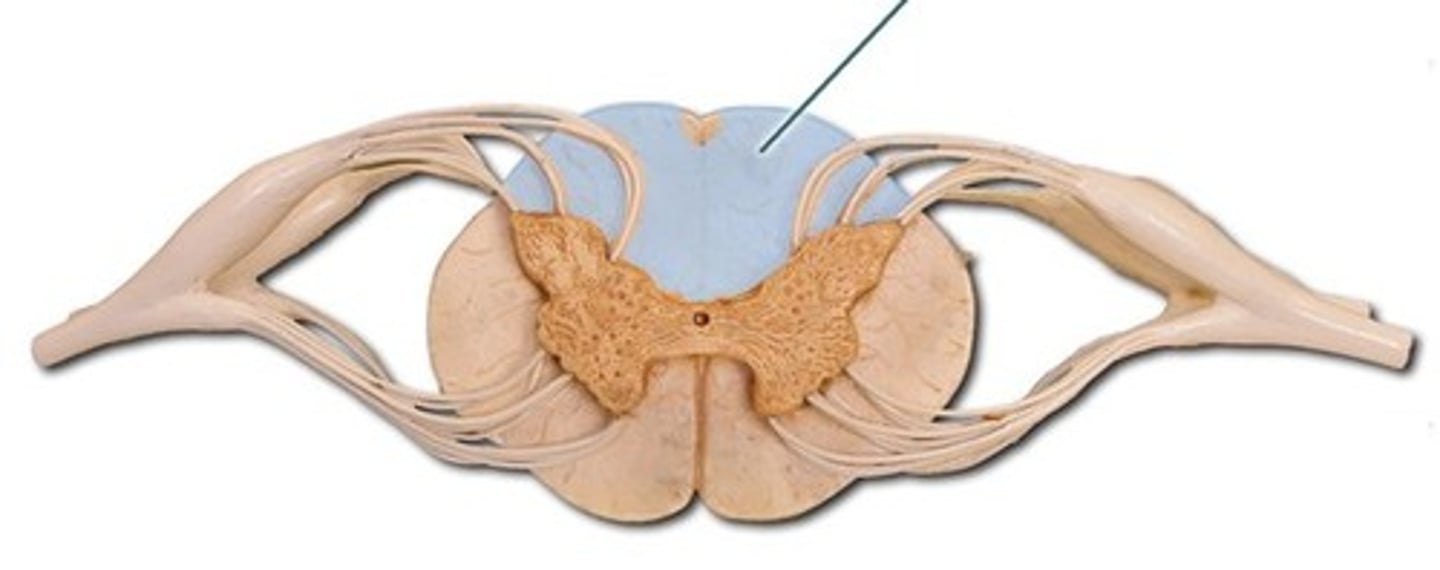
Spinal chord organization
long bundle of nervous tissue extending from medulla oblongata --> lumbar region, surrounded by vertebral column
- grey matter is INSIDE/CENTER of spinal chord
- white matter surrounds it; bringing info up to cortex & back down to muscles
- SOMATOSENSORY information goes IN to the spinal chord
- MOTOR information goes OUT to muscle
- communication/synapsing between the 2 occurs in the grey matter
- also involved in REFLEXES
usually white matter is inside
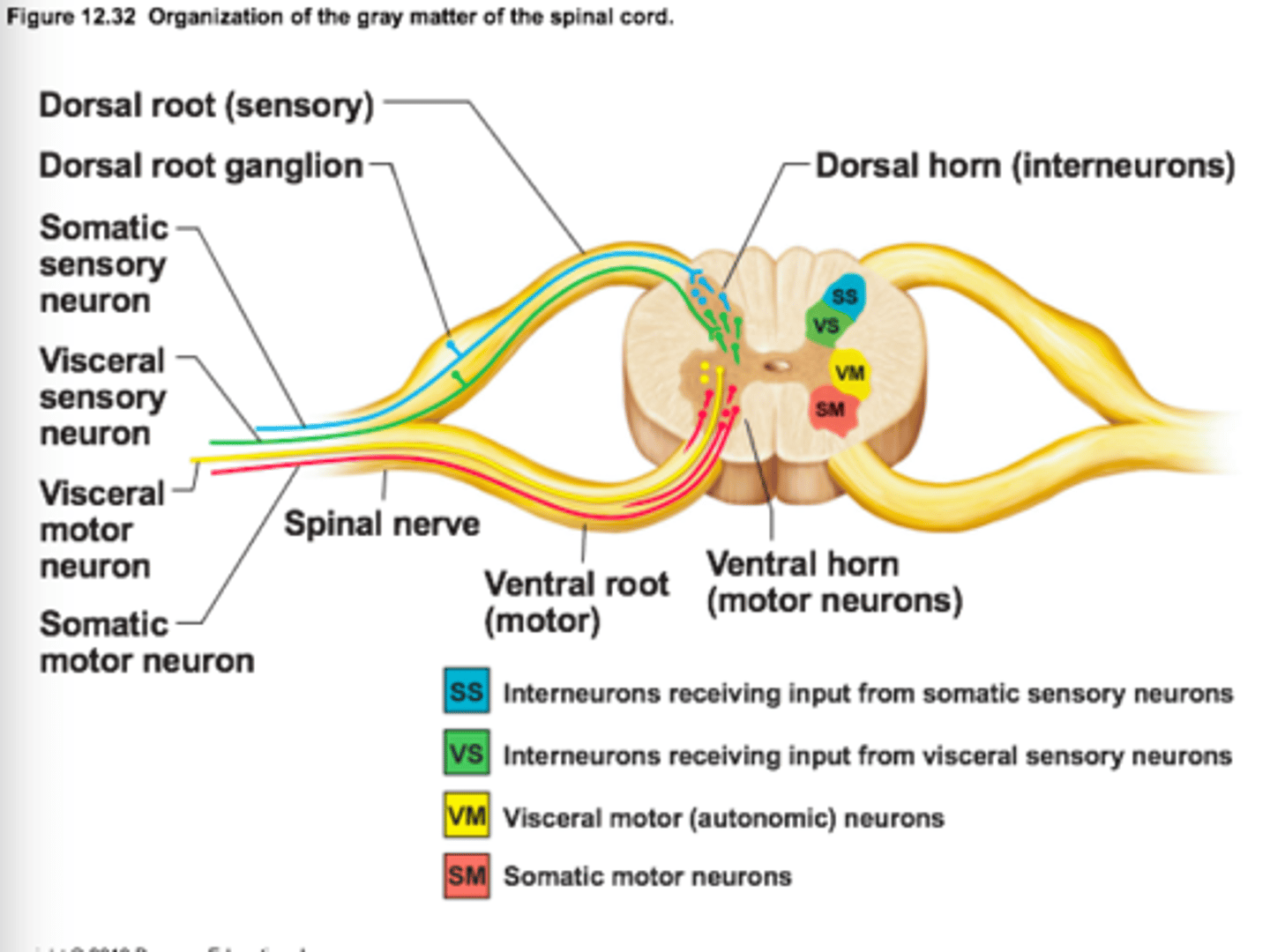
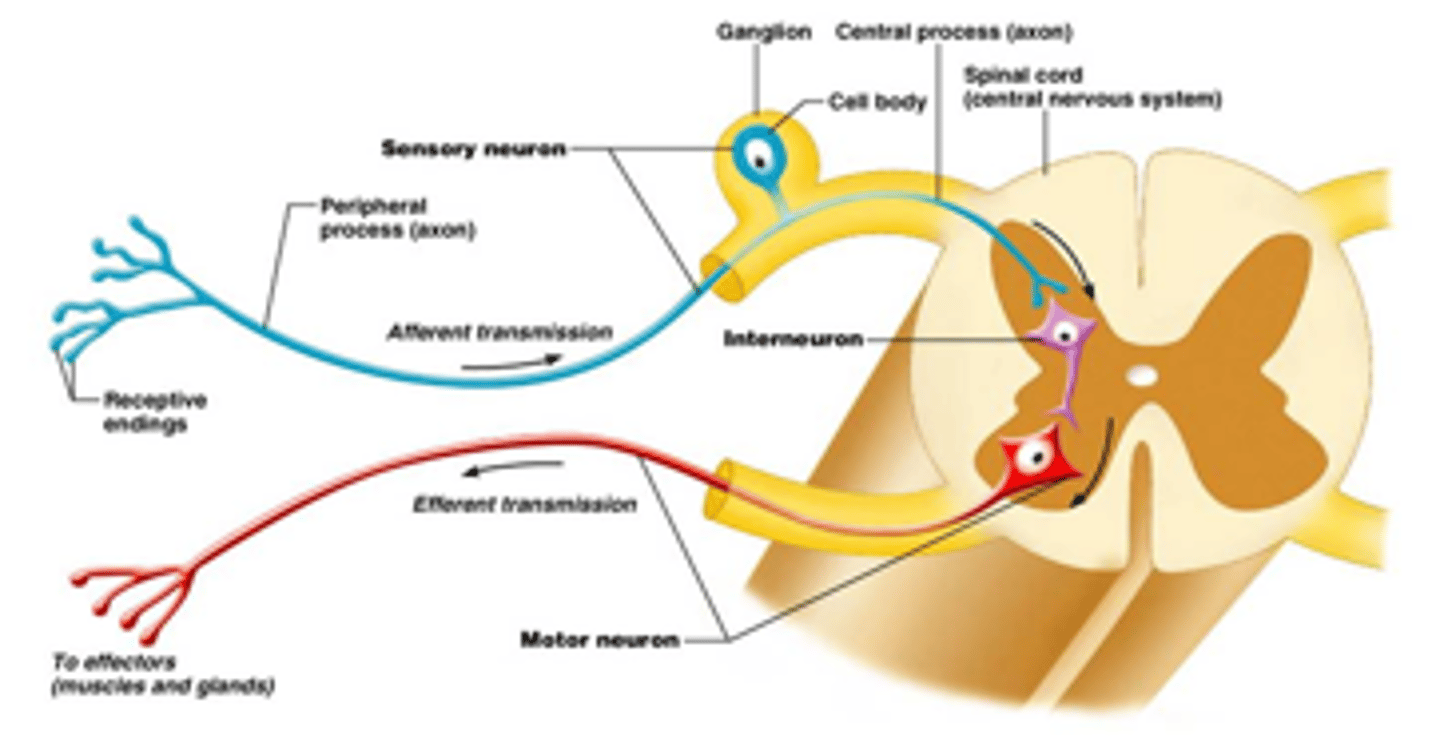
Where do sensory nerves of the PNS have cell bodies?
in the dorsal root ganglion of the spinal chord
- somatosensory nerves enter spinal chord through here
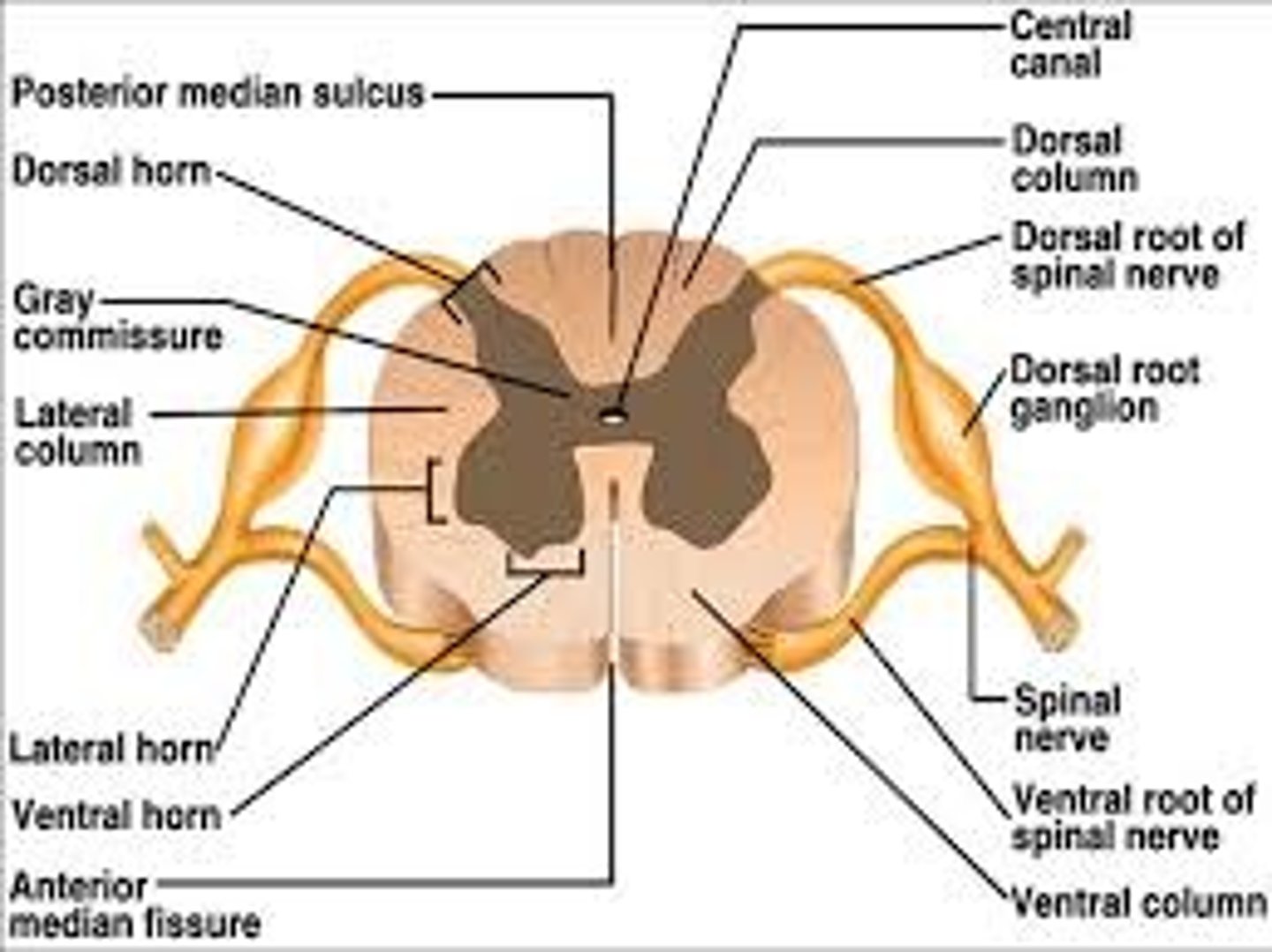
What is the ventral root?
axons of MOTOR NEURONS exiting the spinal chord to the muscle fibers
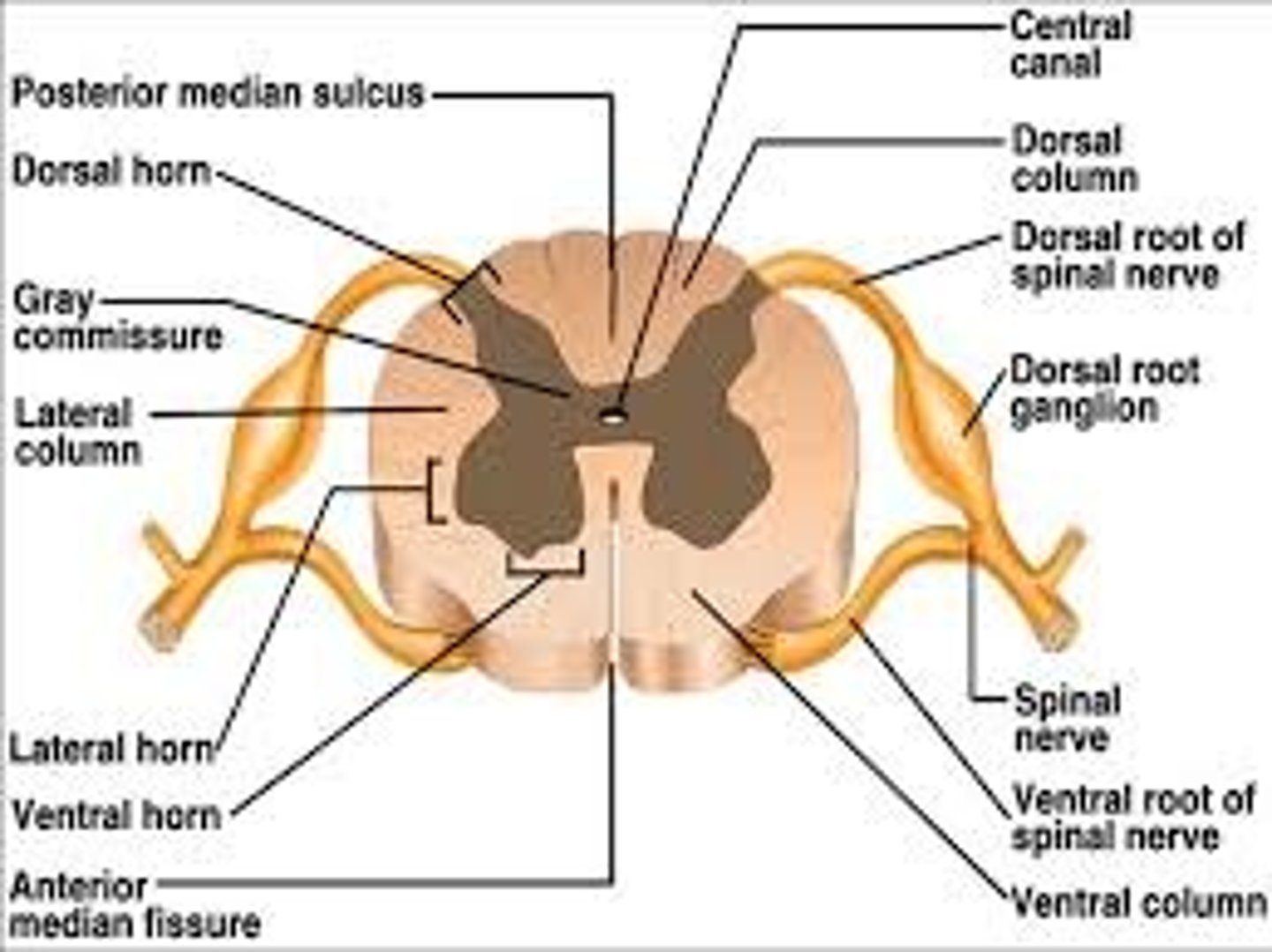
Dorsal root
projections from the dorsal root ganglion that carry sensory information into the spinal chord
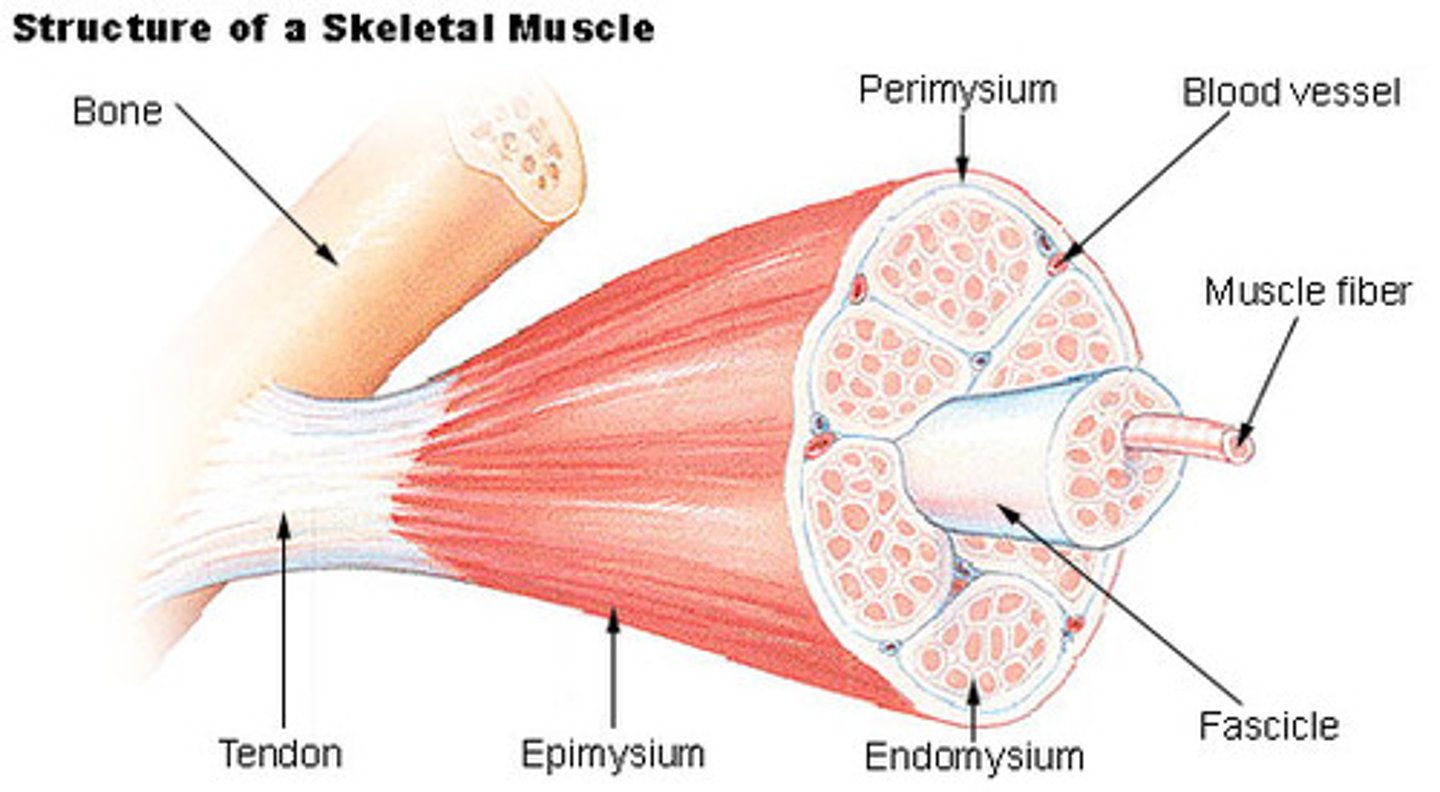
Fascicle
bundle of axons surrounded by connective tissue
- grouped based on what TYPE OF INFORMATION they carry; ex: motor, sensory, reflex, etc.
Where do majority of sensory neurons synapse?
most synapse in the spinal chord
- but not all
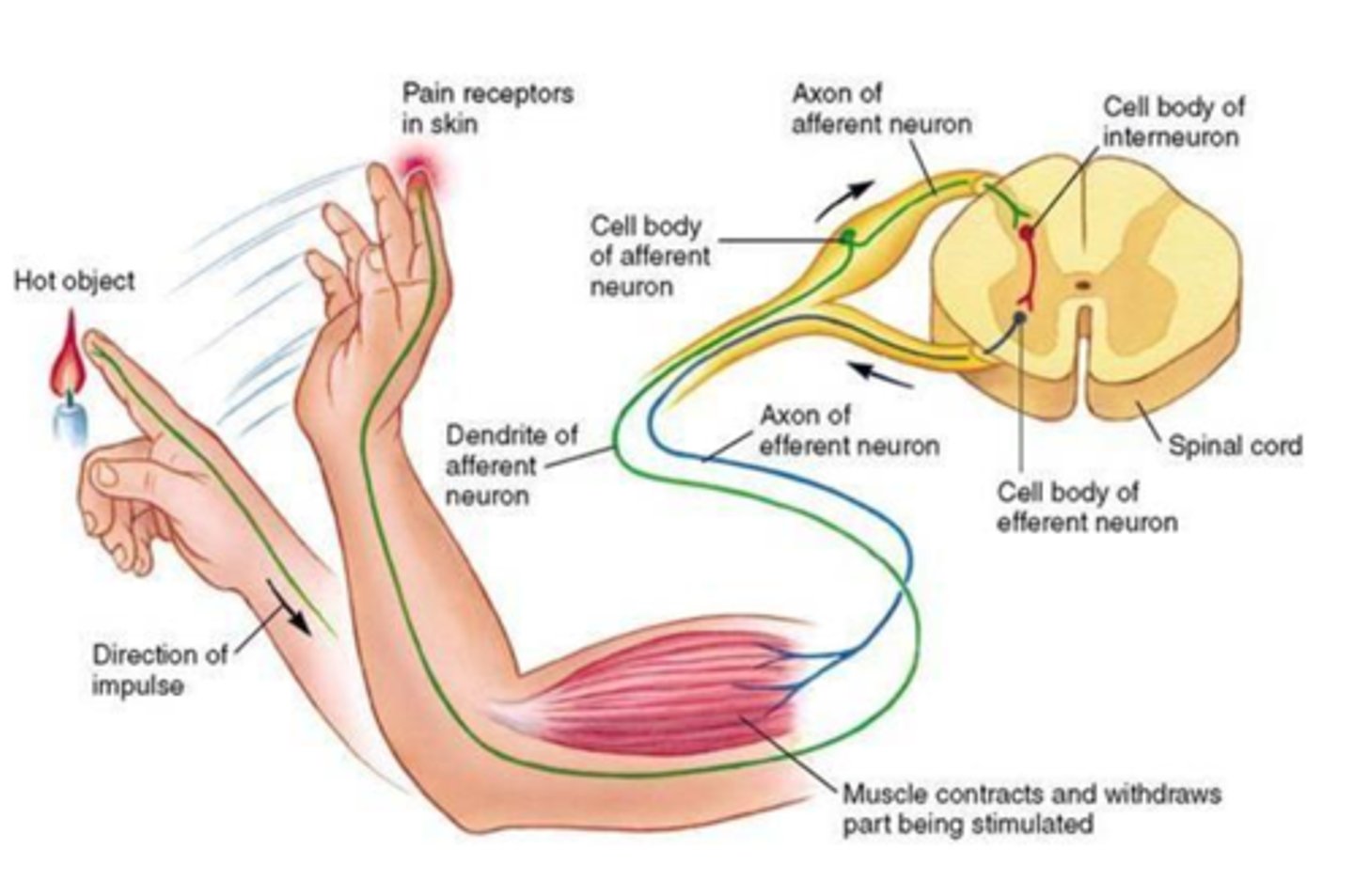
Spinal motor neurons
surpass that long process of waiting for signals to be sent to cortex first then back down to muscle fibers in order to active
- *withdrawal reflex!*
- pain is sensed, instead of going up to cortex an interneuron quickly synapses sensory neurons to motor neurons --> muscle contraction
- reflexes are acted out while info is sent to the brain
input pain, output muscle contraction
Posterior columns
somatosensory white matter tracts in the posterior/rear spinal chord carrying information from the spinal chord to the thalamus to S1
- fine touch, vibration, pressure, joint position
- crosses over in brainstem (second order neuron)
When the posterior column reaches the brainstem, what is it called?
medial lemniscus
Where does posterior column cross over to contralateral side?
when the tract reaches the brain stem
What disease attacks posterior columns of the spinal chord? What does it cause?
late stage syphillis
- affects walking & ability to properly move
Spinocerebellar tract
somatosensory white matter tracts in the posterior/lateral spinal chord carrying information from spinal chord to the cerebellum; anterior & lateral
- joint position, muscle fiber tension, balance/coordination
- axons synapse/cross immediately in spinal chord
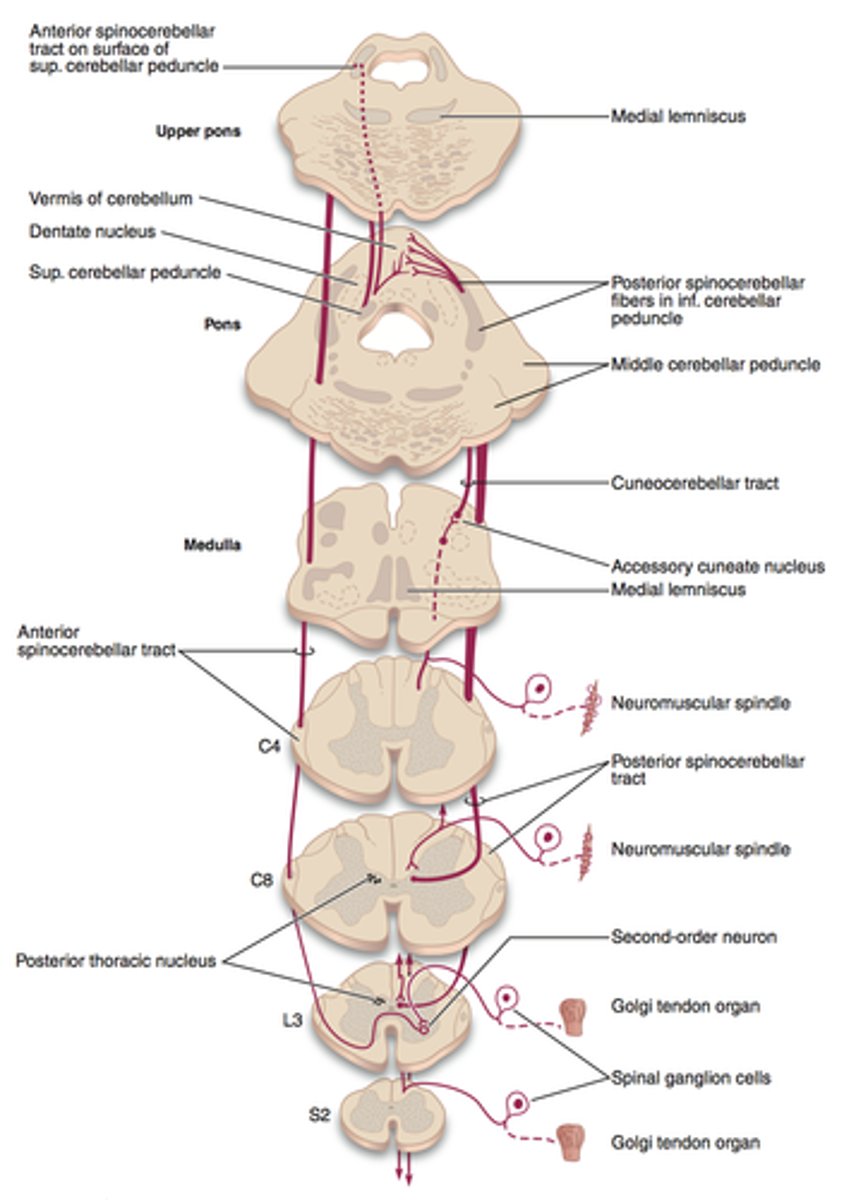
Lateral spinocerebellar tract
somatosensory white matter tracts in the lateral spinal chord carrying information from spinal chord to the thalamus then to cortex
- pain, temperature
- axons synapse/cross immediately in spinal chord before going up
Anterior spinocerebellar tract
somatosensory white matter tracts in the anterior spinal chord carrying information from spinal chord to the thalamus then to cortex
- crude touch, pressure
- axons synapse/cross immediately in spinal chord
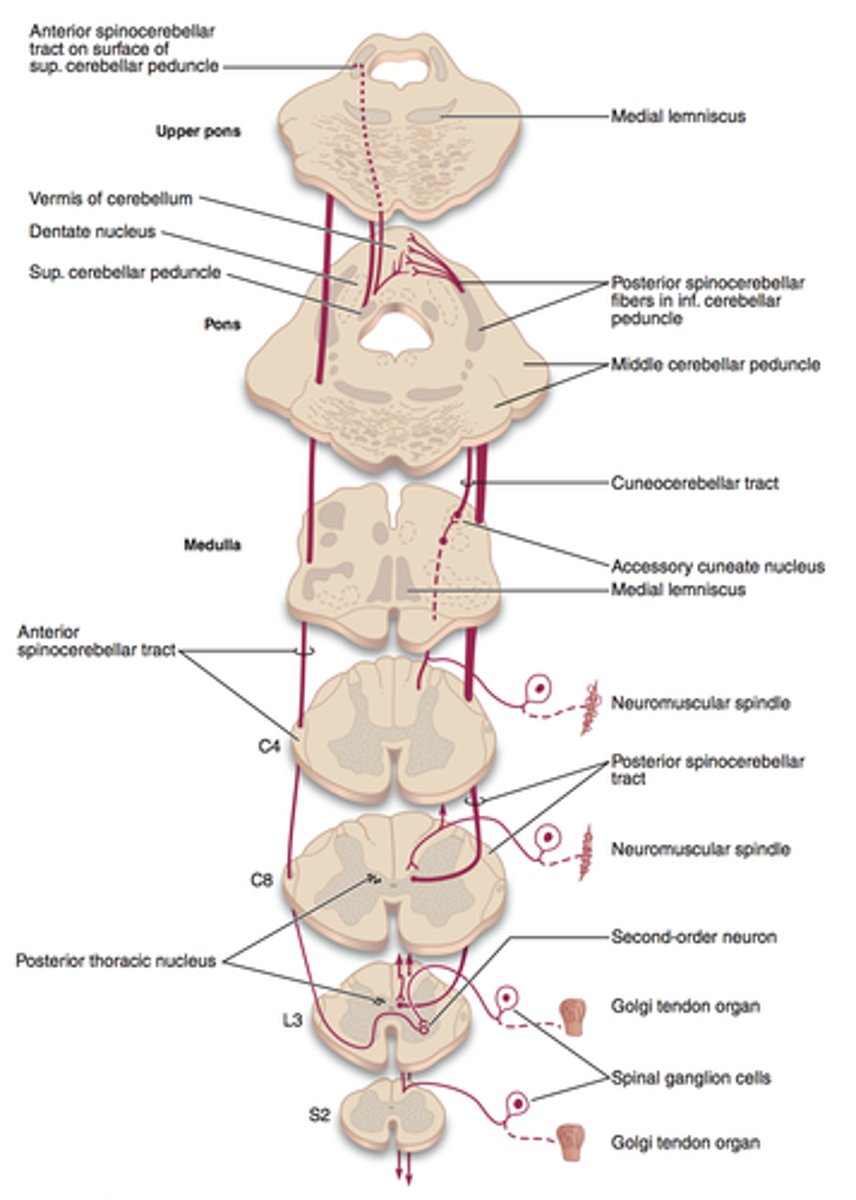
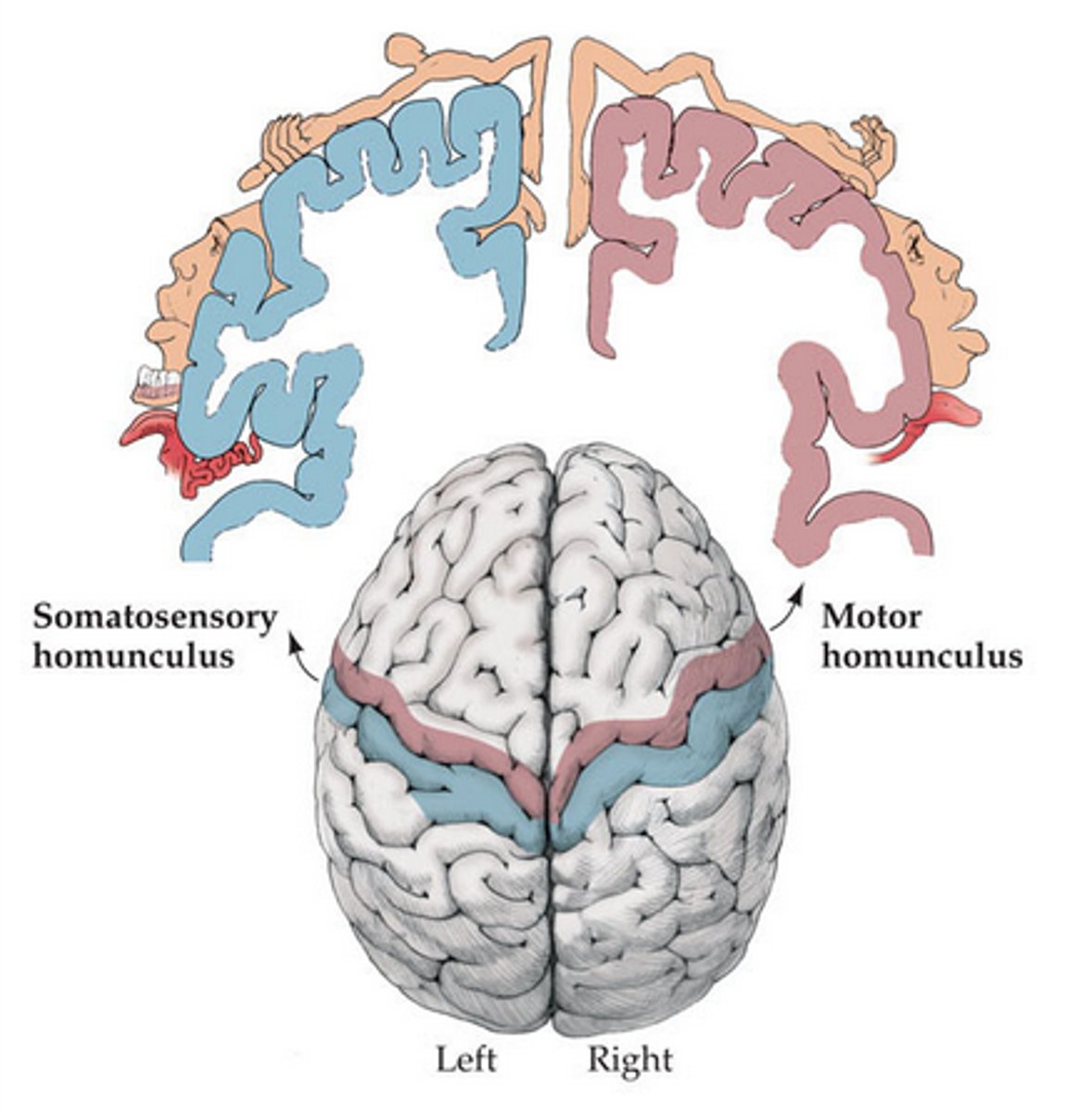
Location of S1 & M1 in respect to the central sulcus
M1: in front of/anterior to central sulcus
S1: behind/posterior to central sulcus
^^both organized somatotopically (body-map representation)
Nociceptors travel up which pathway from the spinal chord to the cortex?
spinothalamic pathway
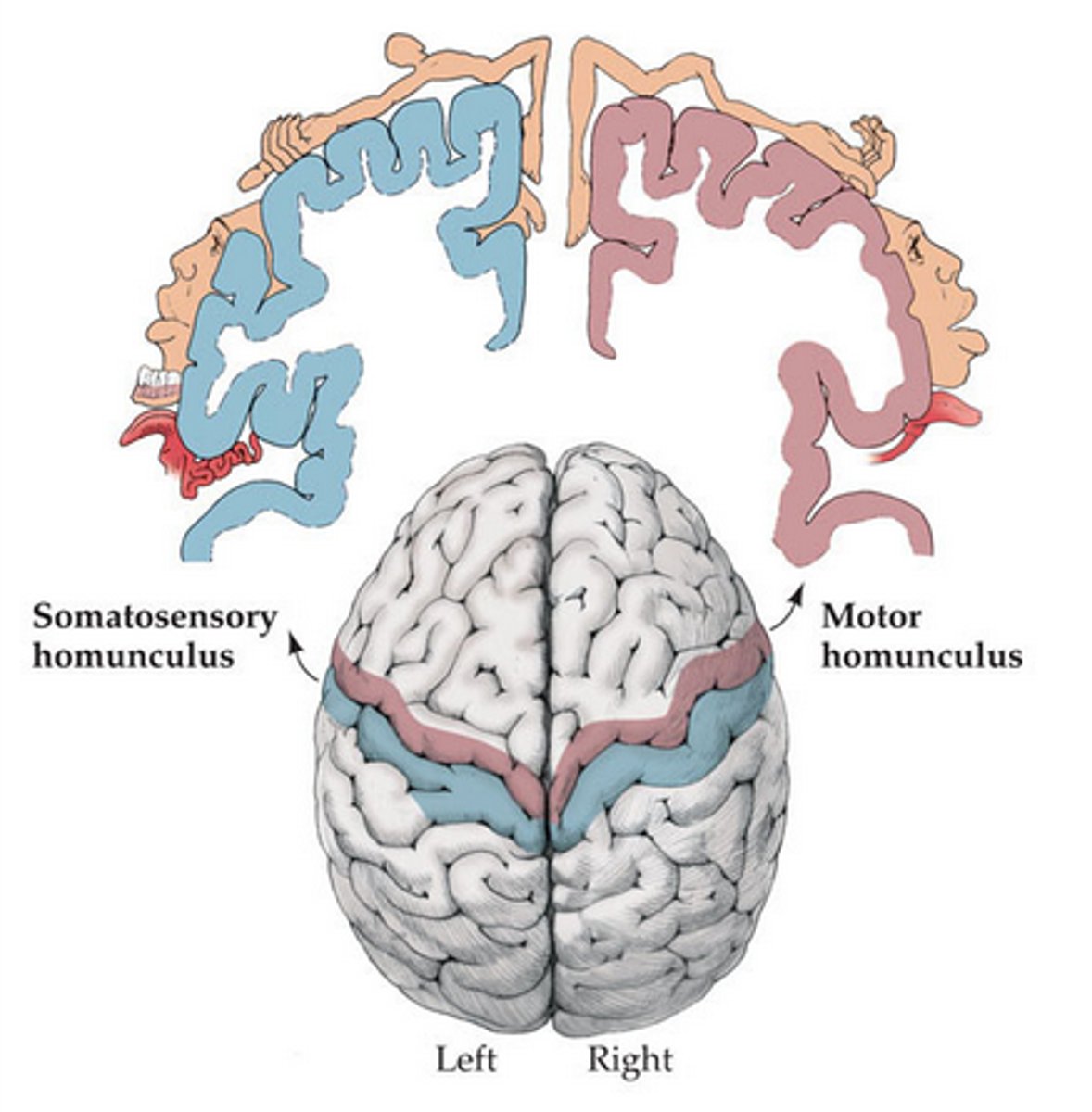
Pain matrix
a number of different regions in the brain involved in pain perception
- hypothalamus, thalamus, limbic system, S1, S2
Pain & temp are carried by different pathways than light touch
a) True
b) False
a) True
Tactile agnosia
inability to identify objects by touch
- can identify with visual information
- damage to S1/S2

Cotard syndrome/walking corpse syndrome
rare neuropsychiatric disorder believing one is dead, is dying, lost blood/internal organs' delusional misidentification syndrome about ONESELF
- depression, schizophrenia, BD, meds
- disconnect between sensation & emotional cortex

Possible treatment of Cotard syndrome?
electro-convulsive shock therapy
- specifically targeting depression (bc depression usually contributes to this syndrome)
Congenital analgesia
congenital insensitivity to pain; due to INCREASED ENDORPHINS or MUTATED SODIUM CHANNELS
1. Insensitivity to pain
2. Indifference to pain

Congenital analgesia: Insensitivity to pain
pain stimulus is NOT EVEN DETECTED
- leads to major injury
- most common in children because child cannot inform parent when they are experiencing discomfort
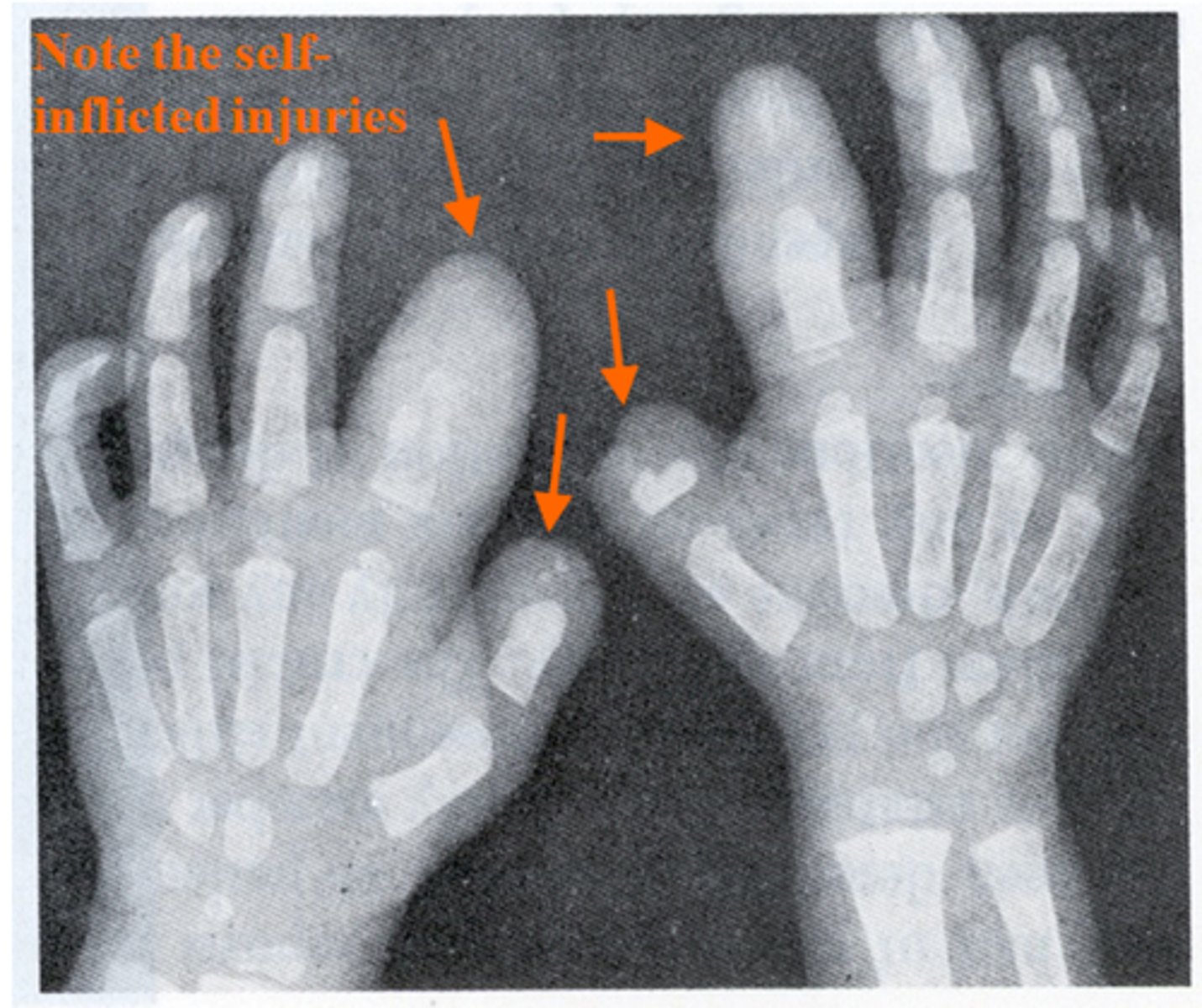
Congenital analgesia: Indifference to pain
pain stimulus is perceived but INAPPROPRIATE RESPONSE to pain
- doesn't flinch/withdraw hands when exposed to pain

Chronic pain
pain extends past typical period of healing
- affects 1/3 of Americans
- major impact on daily life
- patients are severely undertreated

Chronic pain affects more people than what groups of people?
cardiovascular disease, cancer, and diabetes COMBINED
Other side effects of chronic pain other than the pain itself
- comorbid diseases/disorders
- "invisible disabilities"
- loss of 10 years on life
- risk of suicide
- increased rate of depression/anxiety/sleep problems
Chronic pain treatment
hard to treat
- over the counter (advil, tylenol)
- antidepressants, anticonvulsants
- 8% get addicted to opioids; it helps alleviate their pain so they develop an addiction
Do chronic pain patients easily get addicted to opioids?
NO!; majority do NOT become addicted, only about 8%
How does the opioid crisis affects chronic pain patients?
due to the opioid crisis it is much harder to obtain meds, which affects chronic pain patients
- limits doctors from prescribing, puts a toll on patients as they have to now come in person to be assessed which is already difficult
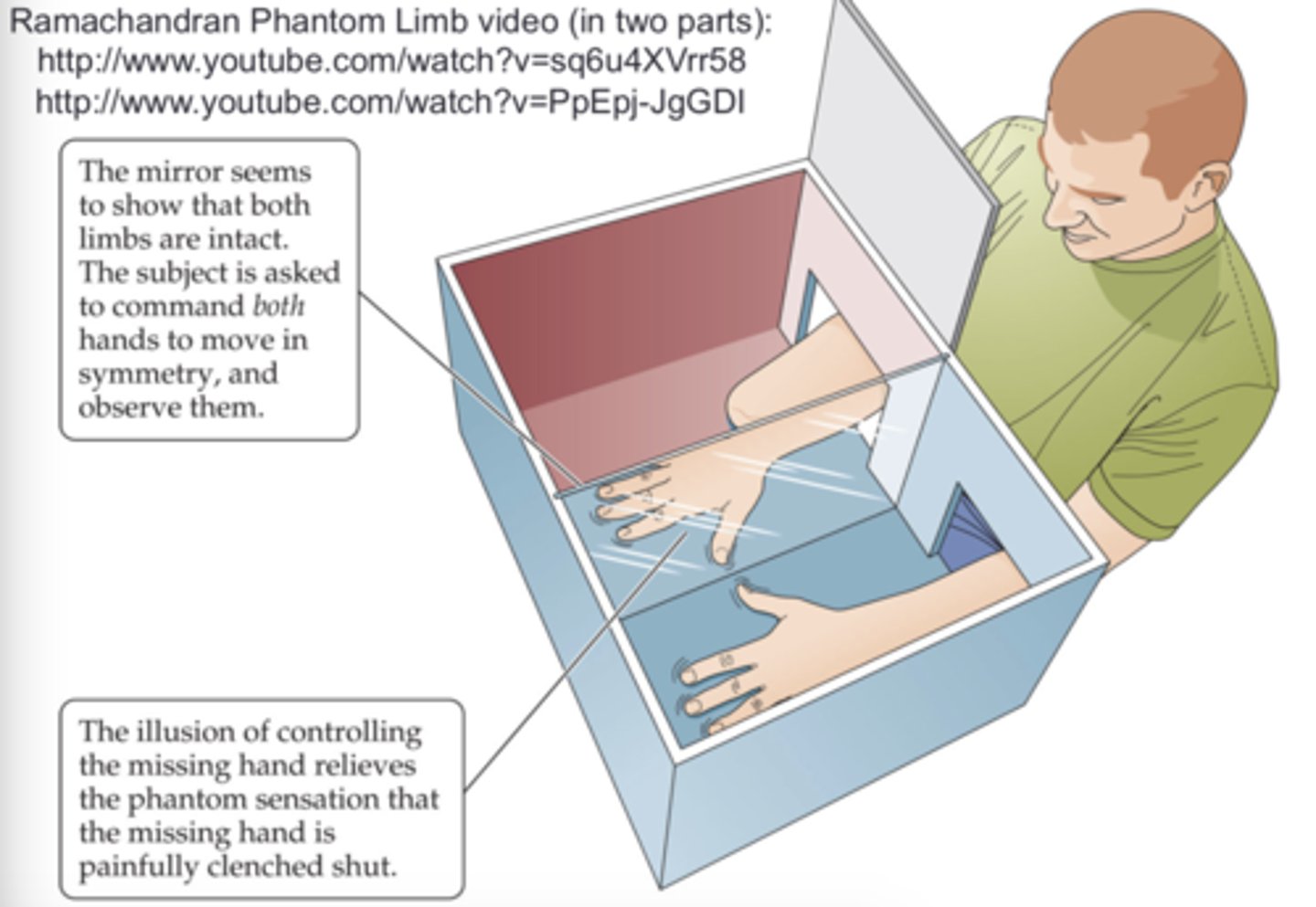
Phantom limb syndrome
the perception of sensations, including pain, in a limb that has been amputated
- peripheral inputs are missing due to lack of limb, nerves try to regrow but cant --> freak out = pain!
- pain comes from S1 & pain matrix
Treatment for phantom limb pain
mirror therapy & virtual reality
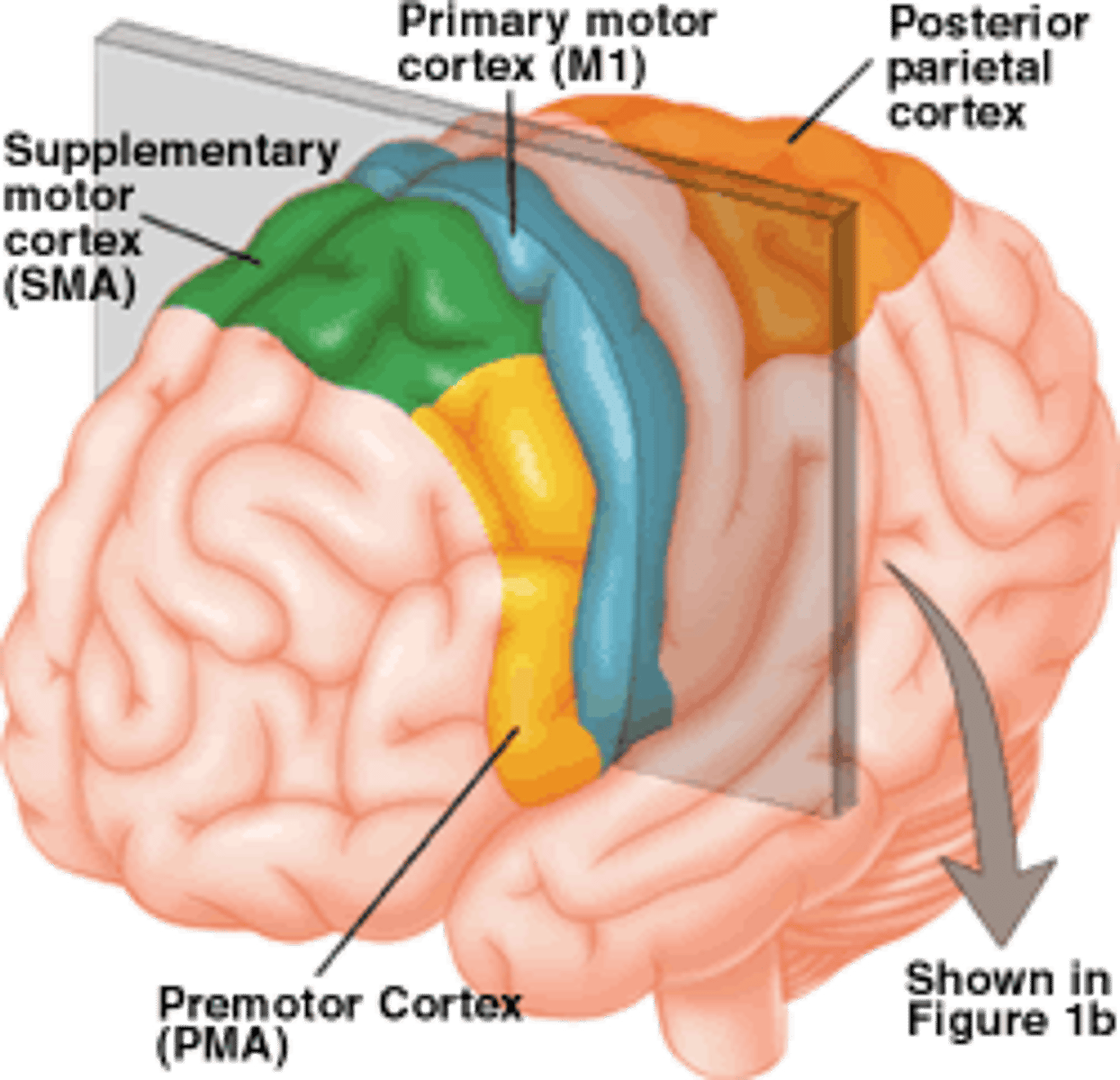
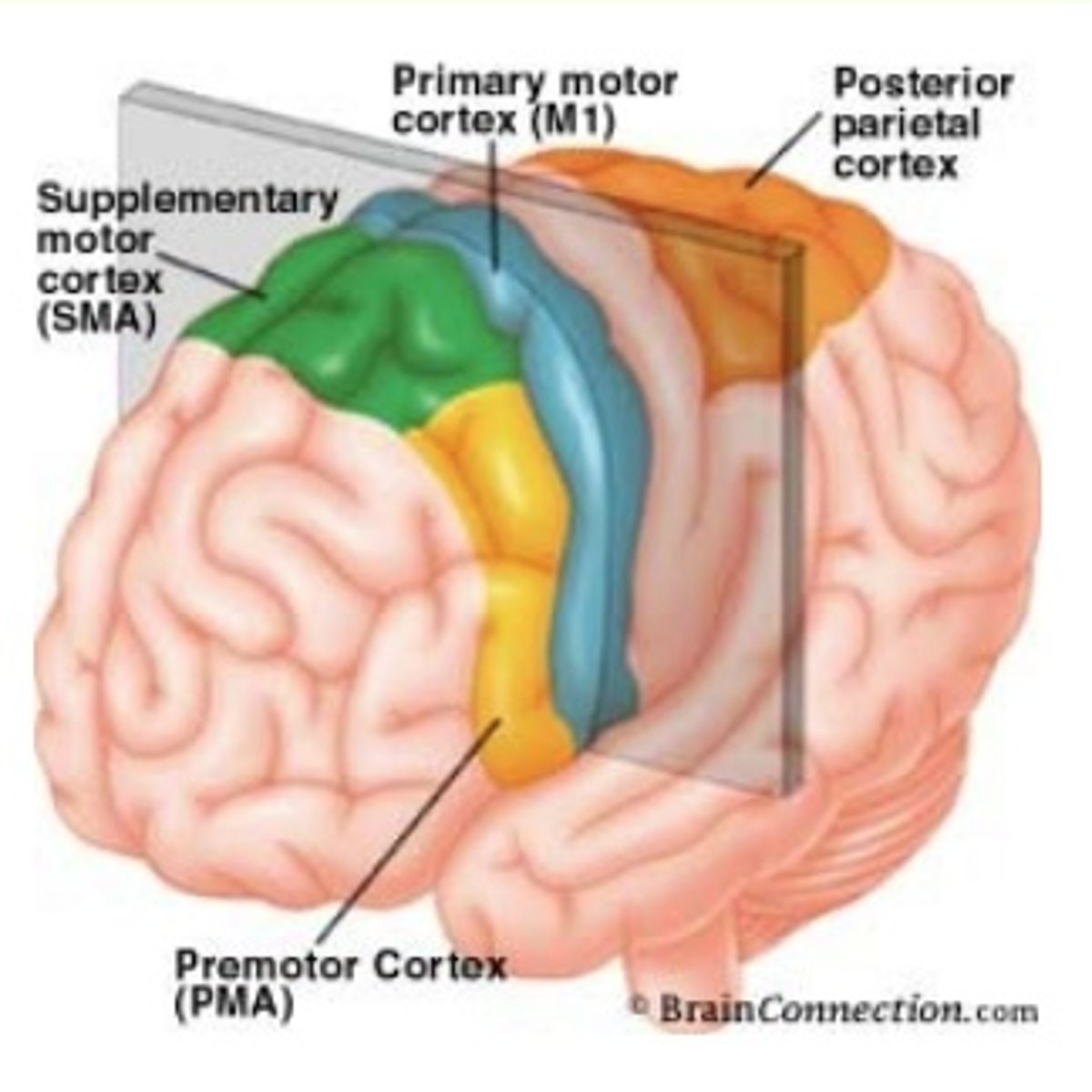
Posterior Parietal Cortex (PPC)
brings all sensory/visual information TOGETHER & transforms them into MOTOR commands
- attention & working memory are also involved
- ex: looking at the location of a cup --> motor neurons needed to properly grab that cup
Lesions/damage to PPC
- visuo-spatial coordination deficits
- attention deficits
- neglect syndromes; hemispatial neglect
Premotor Cortex (PMA)
complex planning of movement of postural/trunk & large limb muscles (torso, shoulders, abdomen)
- anterior to M1 & inferior to SMA; sends info to SMA
- anti-gravity control; keeping ourselves UPRIGHT
- planning/refining movements based on sensory input
- how to start & stop
- oops! center for motion; "did we execute that movement correctly? or does it need to be refined/updated?"
Lesions/damage to PMA
disruption of LEARNED RESPONSES to visual cues
- if you watch someone show you how to make a certain motion, it may be hard to replicate
Supplementary Motor Area (SMA)
planning *SEQUENCES* of movements
- anterior to M1 & superior to PMA; sends info to M1
- active JUST PRIOR to the movement itself
- ex: knowing the sequence of motion for properly spiking a volleyball
- ex: sequence of motion needed to reach out and grab the cup to your left
Unilateral lesion/damage to SMA
difficulty in learning the SEQUENCE of movements necessary
Bilateral lesion/damage to SMA
inability to move
- receiving signals from PMA but there is no signal to send to M1 if SMA is damaged on both sides
Stimulation to SMA
strong urge to move
- no movement yet because that occurs in M1, but the urge to move is very strong (like the urge to sneeze!)
Anterior PPC
somatosensation (close to S1)
Posterior PPC
sensorimotor integration & attention
Primary Motor Cortex (M1)
primary control/execution of motor movement occurs
- anterior to central sulcus; last region (pit stop)
- organized stomatotopically; body-based mapping
!! *LARGE OUTPUT LAYER (LAYER 5)*
Lateral side of M1
motor control for face, mouth, upper limbs
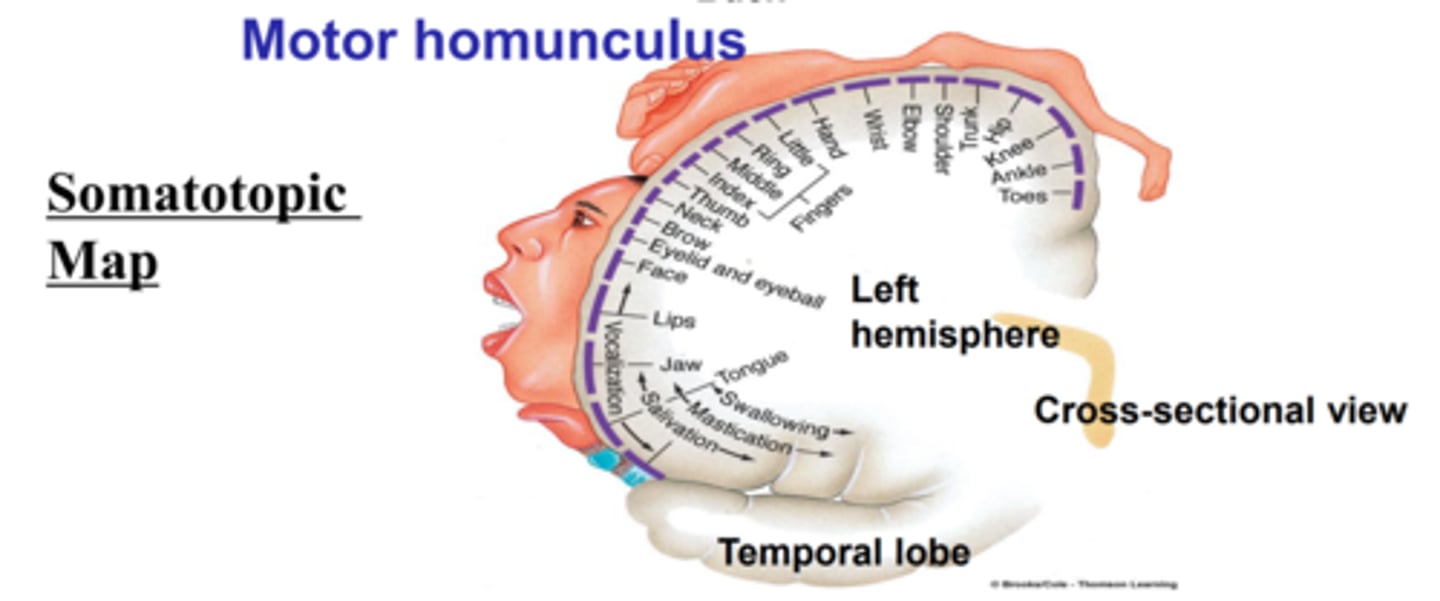
Medial wall of M1
largely attuned to lower limbs, legs, feet
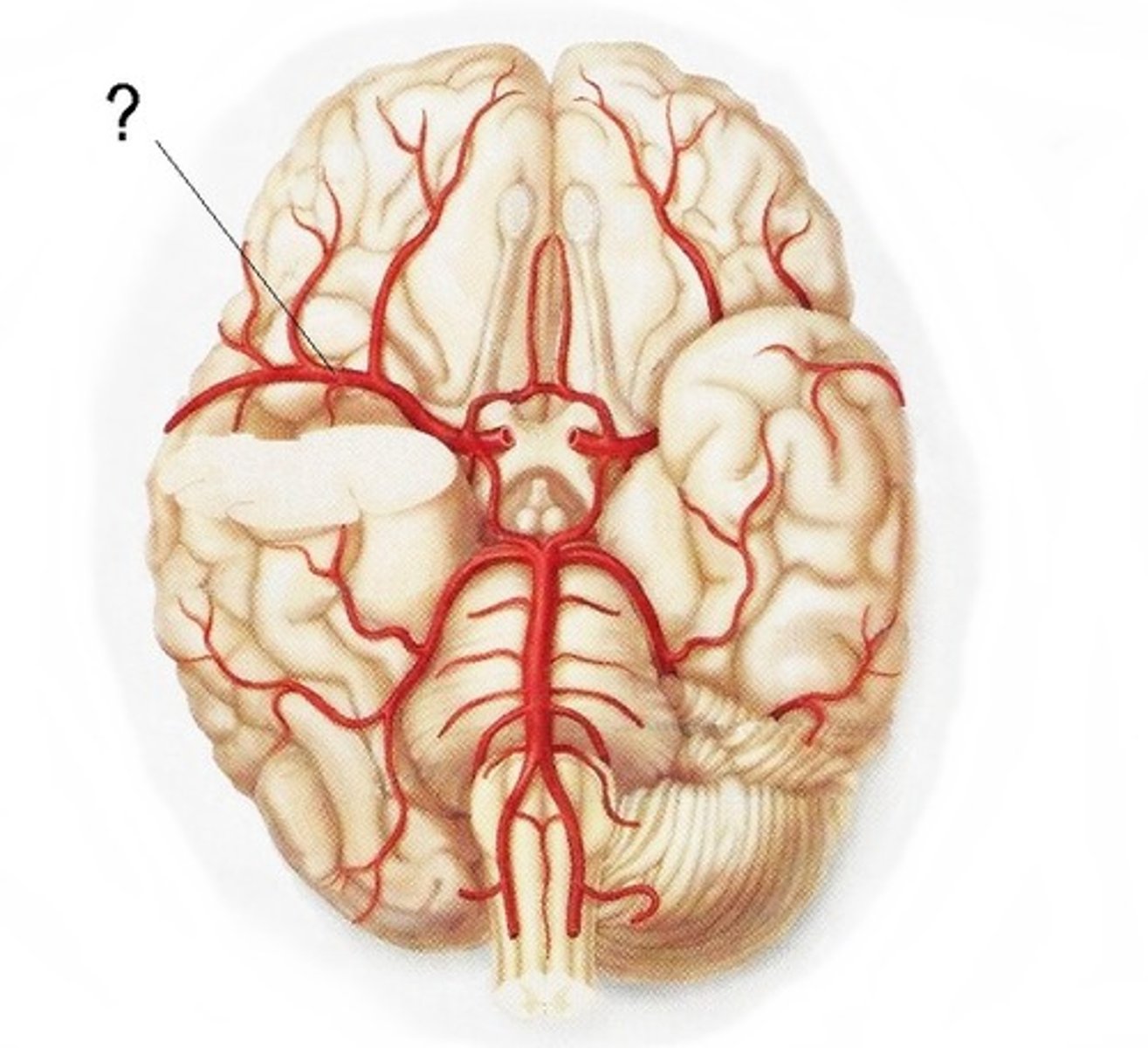
Anterior cerebral artery
runs through anterior/frontal medial wall
- supplies blood to regions that control leg/lower body
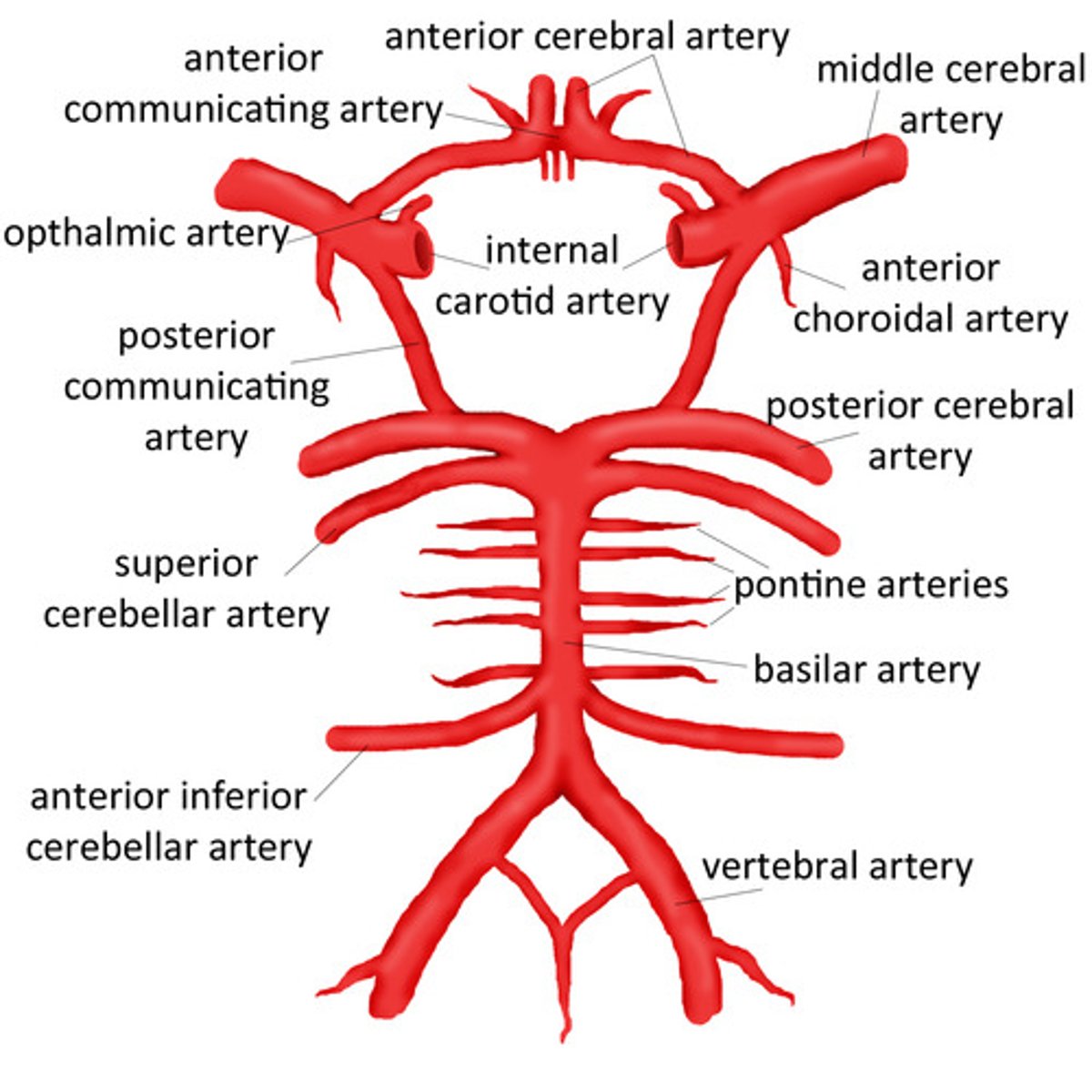
Middle cerebral artery
runs through anterior/lateral cortex
- supplies blood to upper torso, face, arms
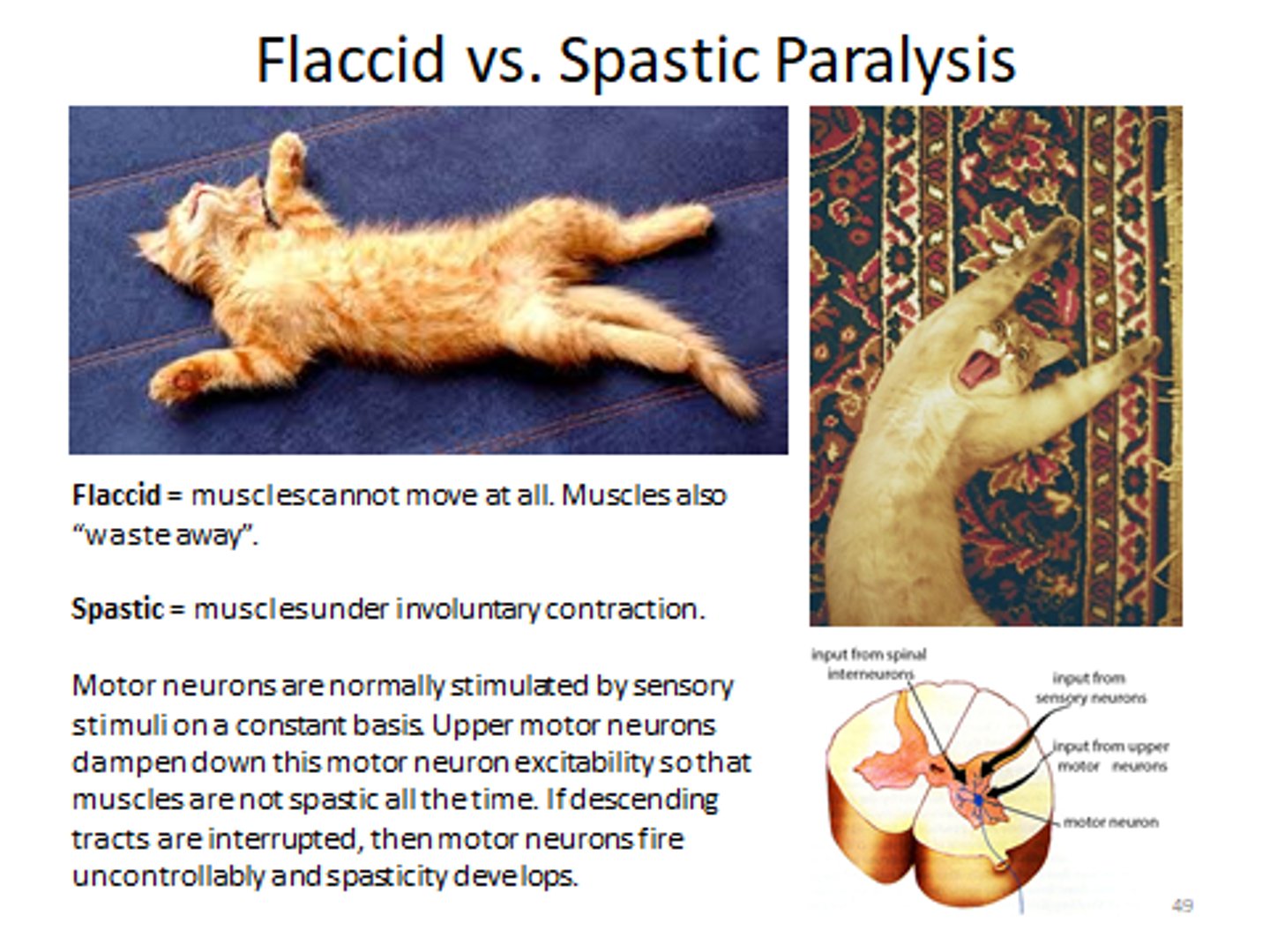
Lesion/damage to M1
spastic paralysis
- due to deficits in inhibiting motion
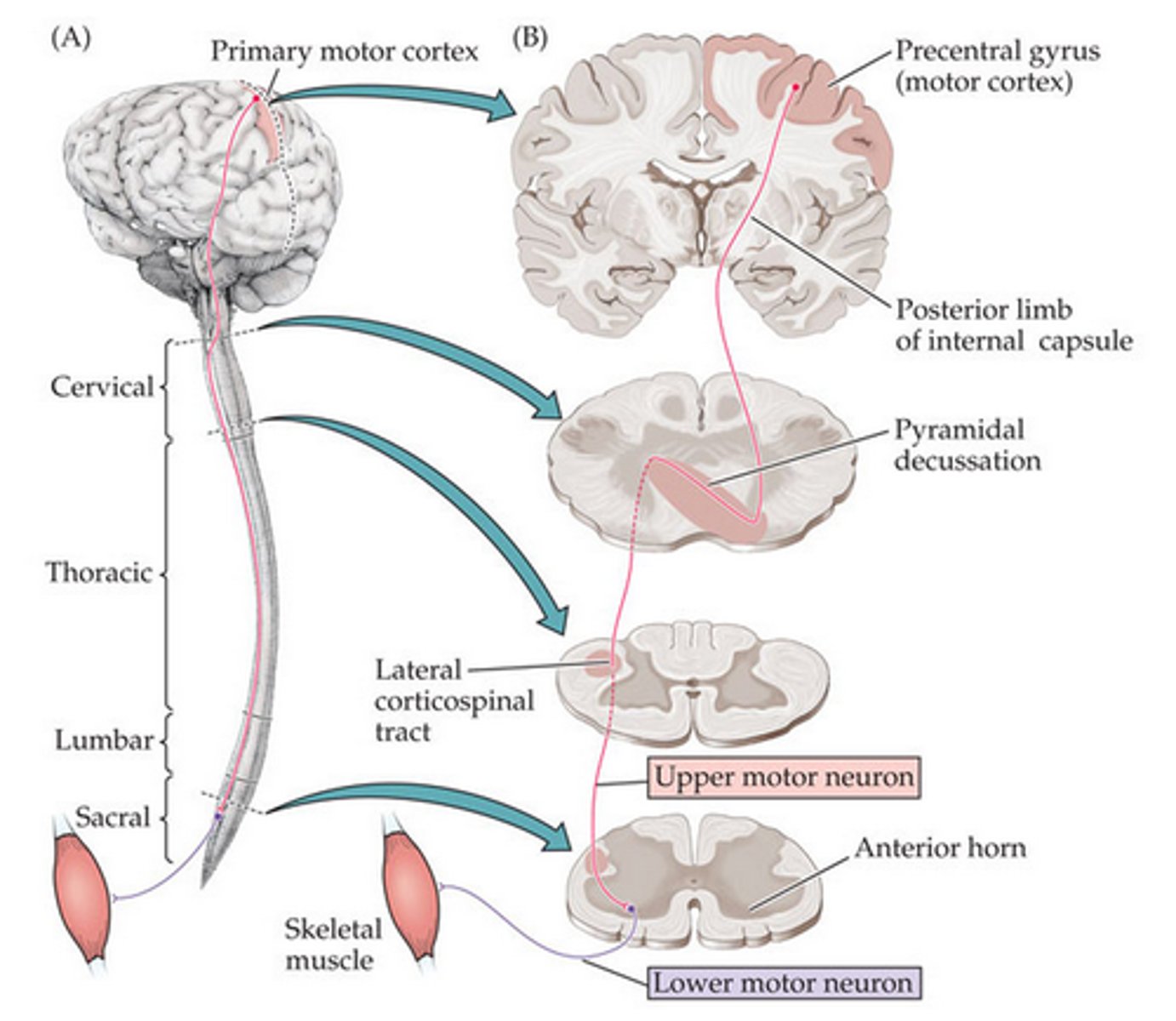
Corticospinal tract (C.S.)
connects motor neurons in cortex to motor neurons throughout the body
- primary white matter tract
- made up of UPPER NEURONS
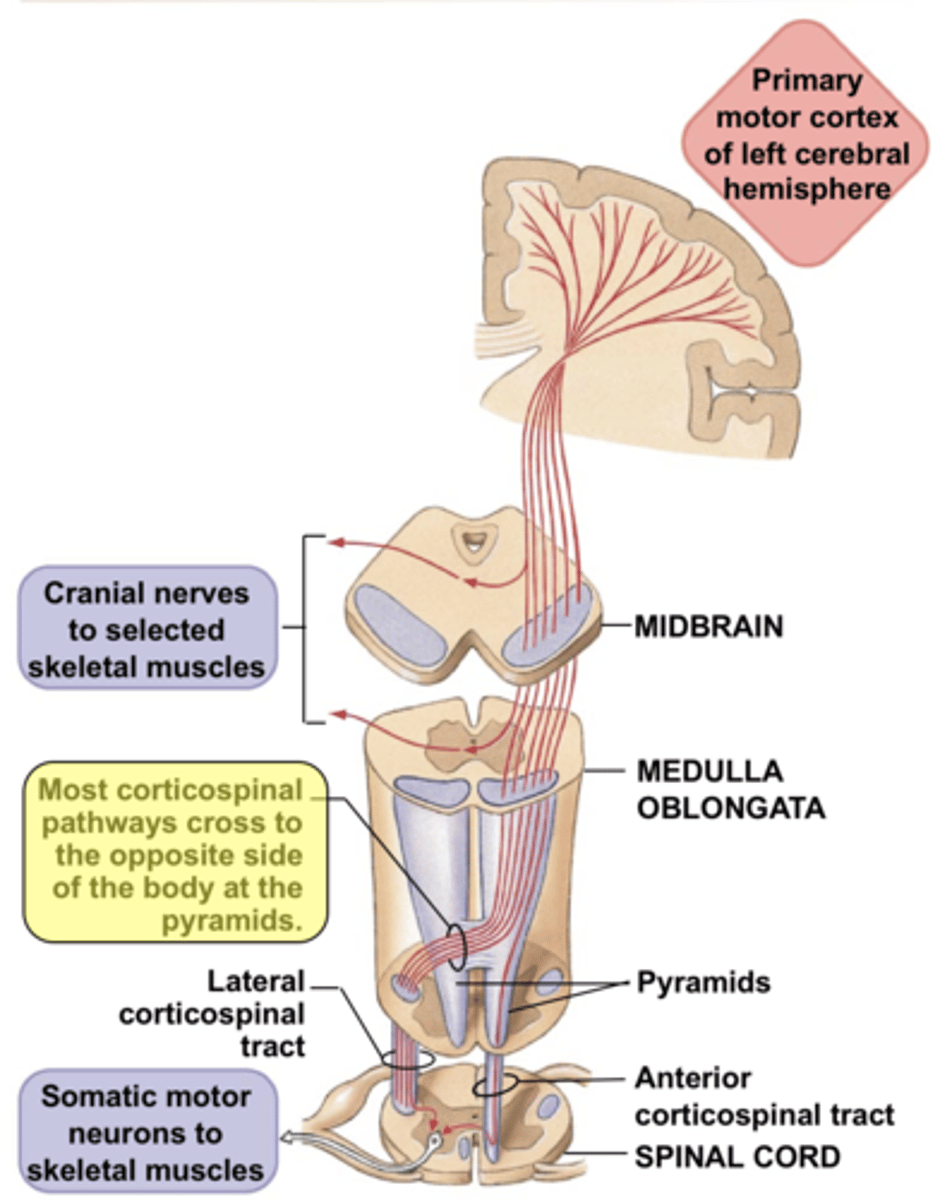
Lateral corticospinal tract
80% of the C.S., crosses to other side
- these go to LIMBS
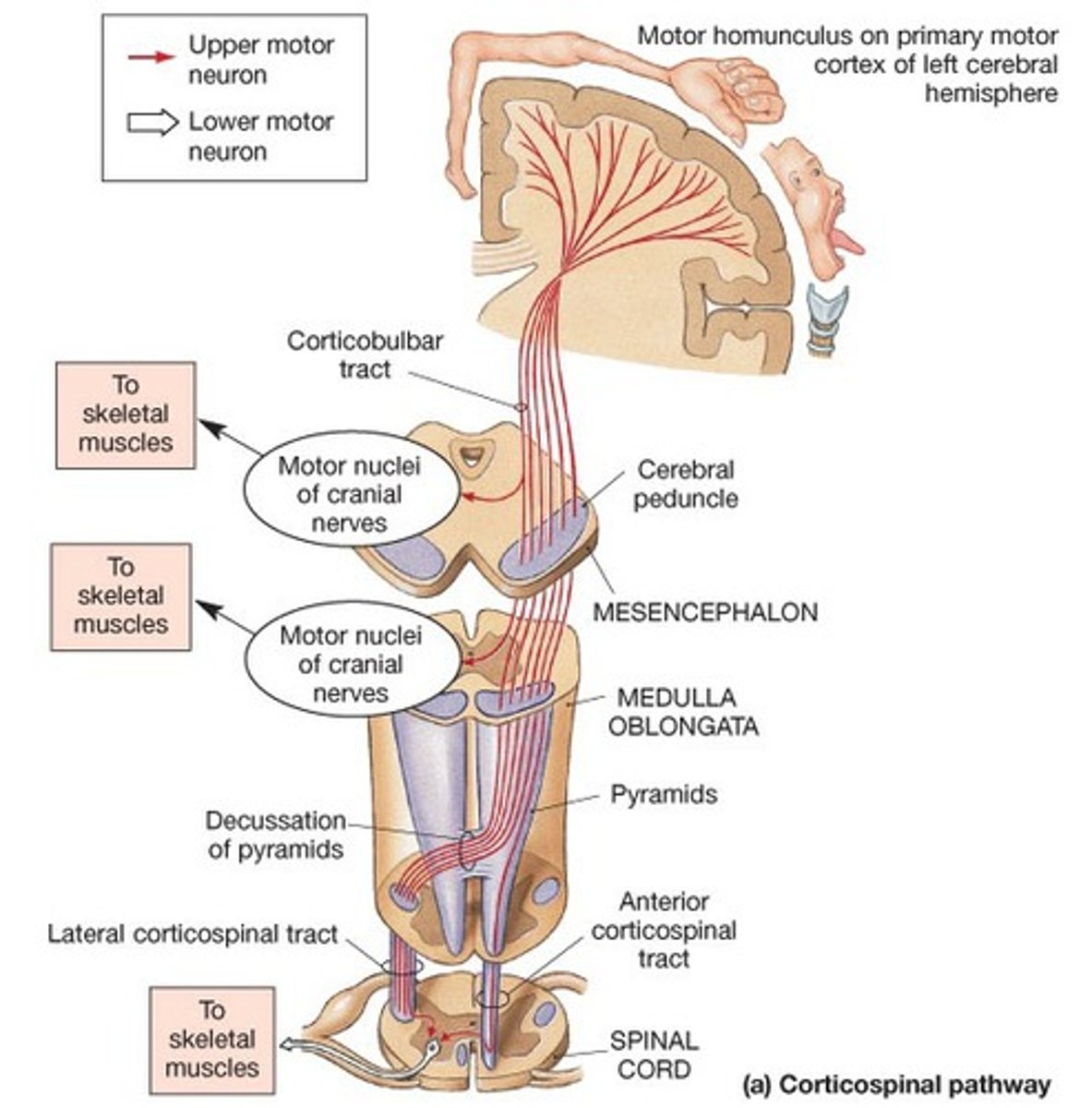
Anterior corticospinal tract
20% of C.S., does NOT cross to other side
- these got to the TRUNK
Why is correct anticipatory strength crucial?
you are able to properly anticipate how heavy/light something is by pre-contraction, therefore your muscles are well prepared to AVOID STRAIN/TEAR
What happens when you over-anticipate how much strength is needed to pick something up?
we make a bigger muscle movement than necessary
- properly squatting and grabbing a brown box thinking it may be filled with a lot of things and using the proper muscles in your legs to pick it up, but realizing its very light since it is completely empty
What happens when you under-anticipate how much strength is needed to pick something up?
this is dangerous because we are not properly prepping our muscles/body to pick up something heavy which can result in tears/strain
Stretch fibers
muscles contract/move to anticipate weight in order to prevent muscle tears/strain
Upper motor neurons
motor neuron cell bodies located in M1/cortex that carry information to a certain part of the spinal chord
- cortex overall is an inhibitory system
What neurons make up the corticospinal tract?
UPPER motor neurons
What happens when upper motor neurons are damaged?
function/movement INCREASES
- spastic paralysis, stronger/intense reflexes
Lower motor neurons
motor neuron cell bodies are in the spinal chord
- receive information from upper neurons & sends them OUT TO MUSCLES
- what makes the movement/action happen
What happens when lower motor neurons are damaged?
function/movement DECREASES
- this is what actually carries out the movement so if this is damaged no movement will occur --> atrophy of muscles since they are not being used
- flaccid paralysis, muscle atrophy, decreased reflexes
What neurons make up the peripheral nerves?
lower motor neurons
Hemiplegia
completely paralysis of one half of the body
- due to contralateral damage/lesion
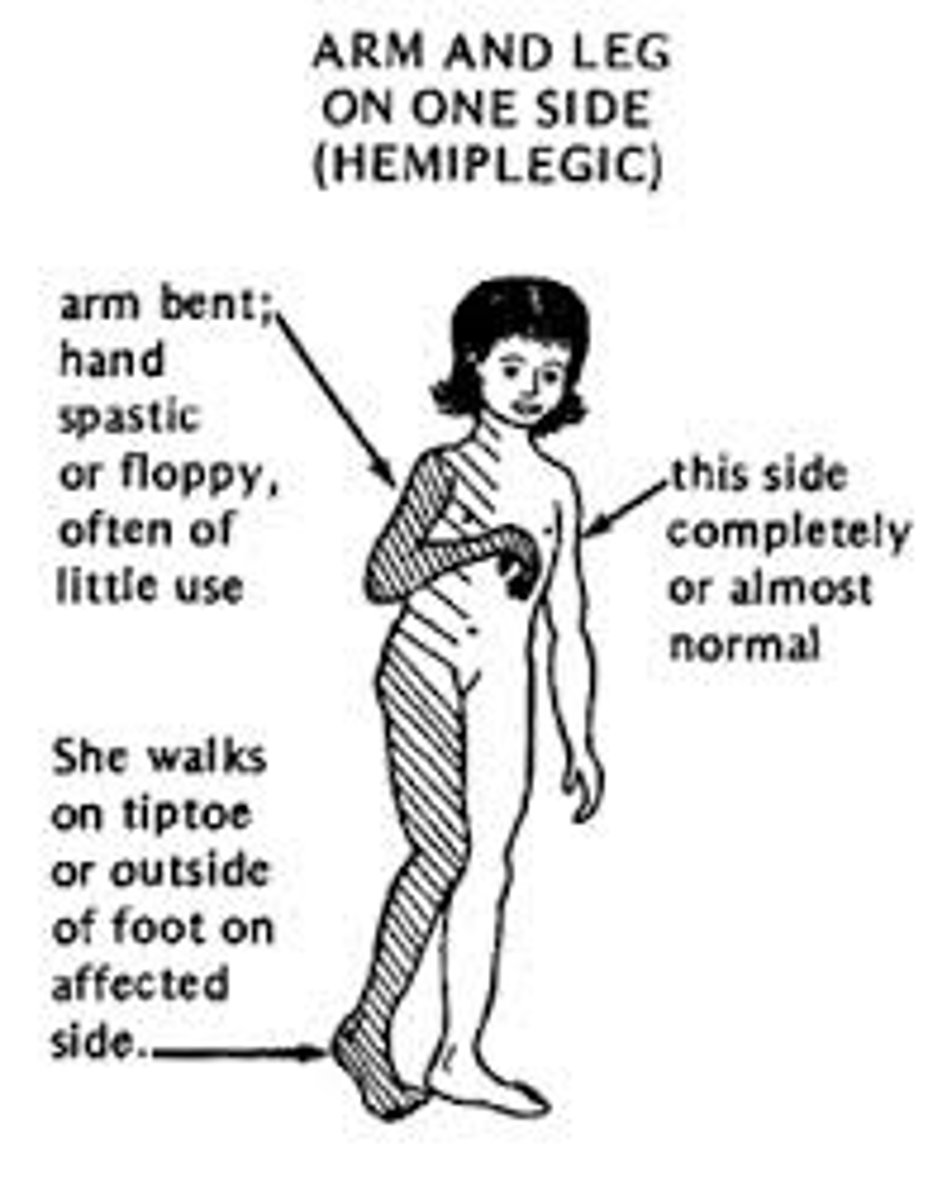
Hemiparesis
weakness of one half of the body
- due to contralateral damage/lesion; just not as severe to cause paralysis

Anosognosia
lack of awareness that something is abnormal/wrong; basically "in denial" of their disorder
- *confabulation*: lying about why they may not be able to do/see something; they are not aware that they are lying they just deny that the cause of the inability is due to a disorder
ex: cant move their arm --> "well i just dont want to theres nothing wrong with it"
- associated with paralysis

What causes anosognosia?
right dorsal parietal lobe damage
Anton's syndrome
blindness & anosognosia of their blindness
- blindness & lack of awareness that they are blind
- changes their perception of the world & themselves
- can lead to eating disorder bc it affects how they see themselves --> body dysmorphia
What causes Anton's syndrome?
dorsal occipital damage
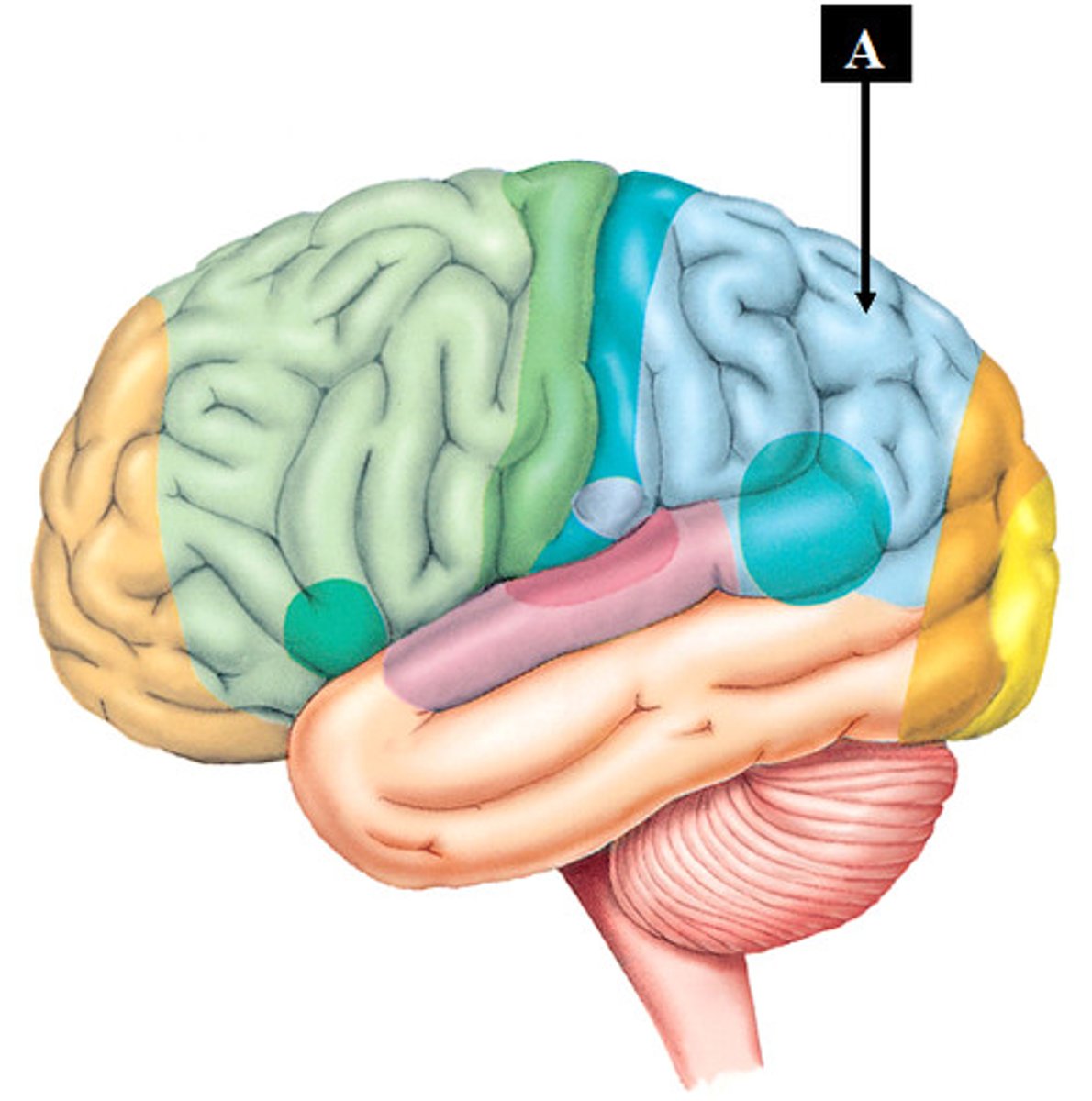
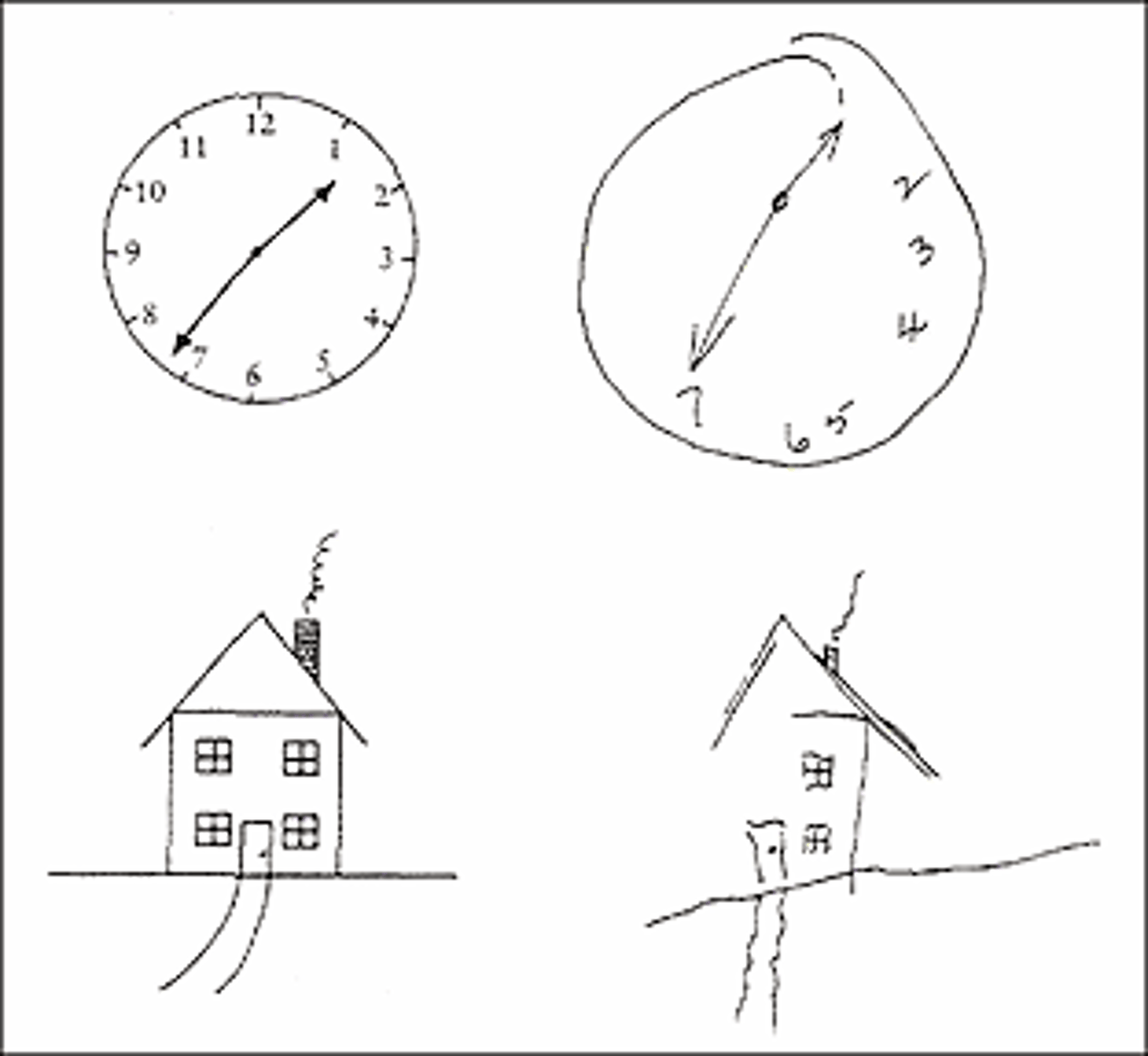
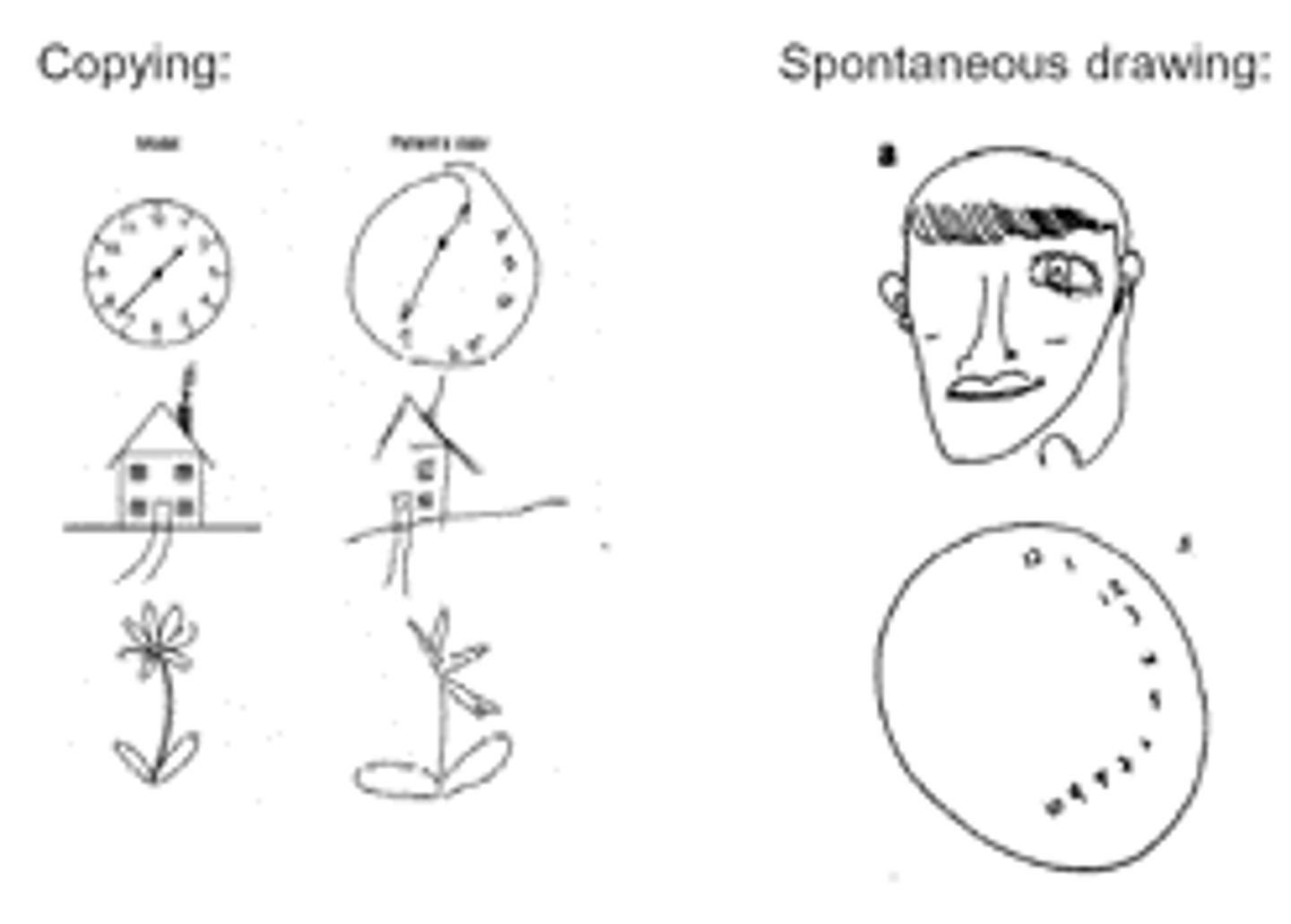
Hemispatial neglect
patients are UNAWARE of one half of the world; they are NOT BLIND they just do not direct any attention to that space
- lack of visual attention
- includes anosognosia (they don't think anything's wrong with them; ex: im full theres no more food on my plate; when in reality there is a whole half plate of food left)
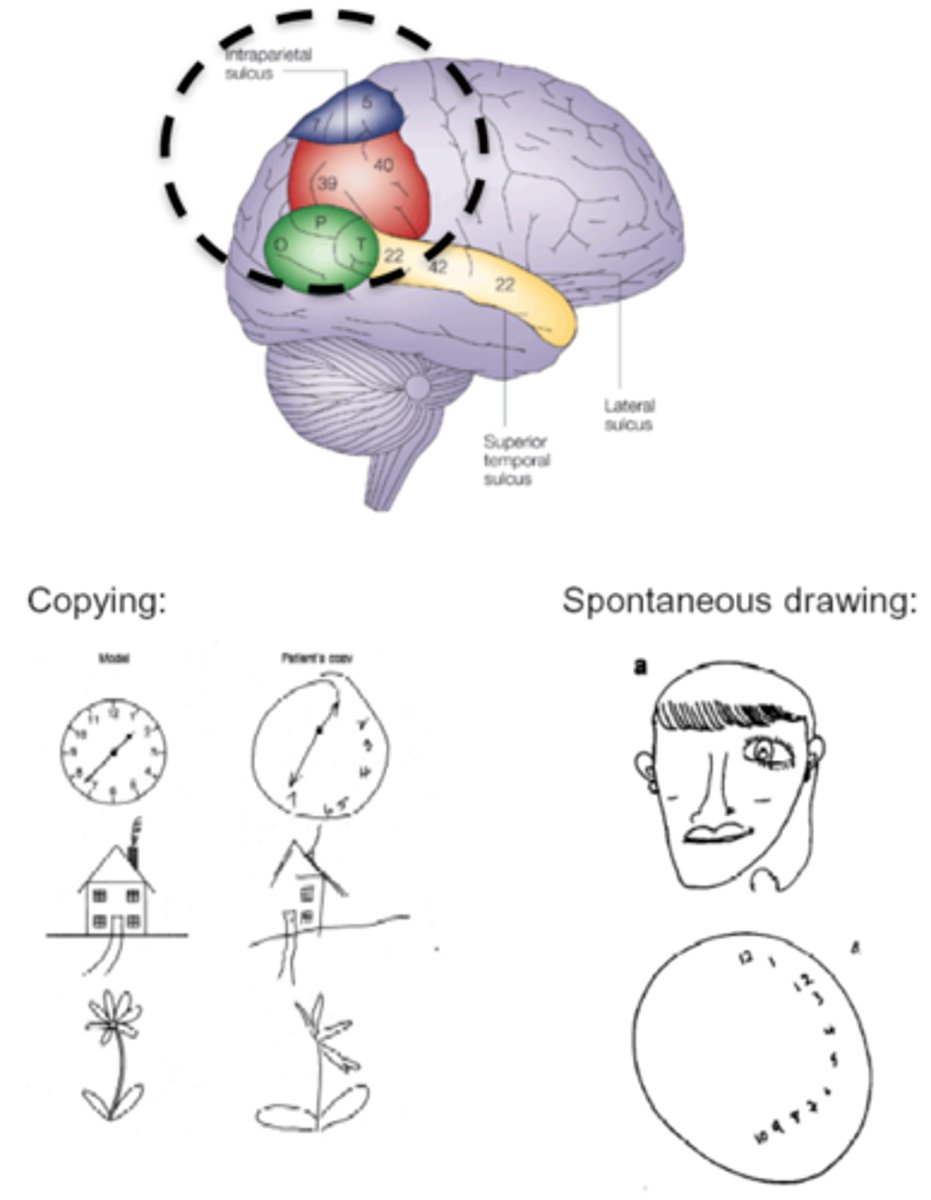
2 neglect syndromes
anosognosia (& Anton's syndrome) and hemispatial neglect
What causes hemispatial neglect?
usually damage to right dorsal PPC (typically right bc there is much more emphasis to right cortex for visual attention; js something i learned in a previous neuro class) --> causes contralateral deficits
- left visual field neglect is most common
Gerstmann's syndrome
cluster of symptoms:
- finger agnosia: patients will identify other objects as their fingers/toes & vice versa
- hard to differentiate between left & right
- dsycalculia: problems with calculations
- dsygraphia: problems with writing (can read but cannot write)
- anosognosia
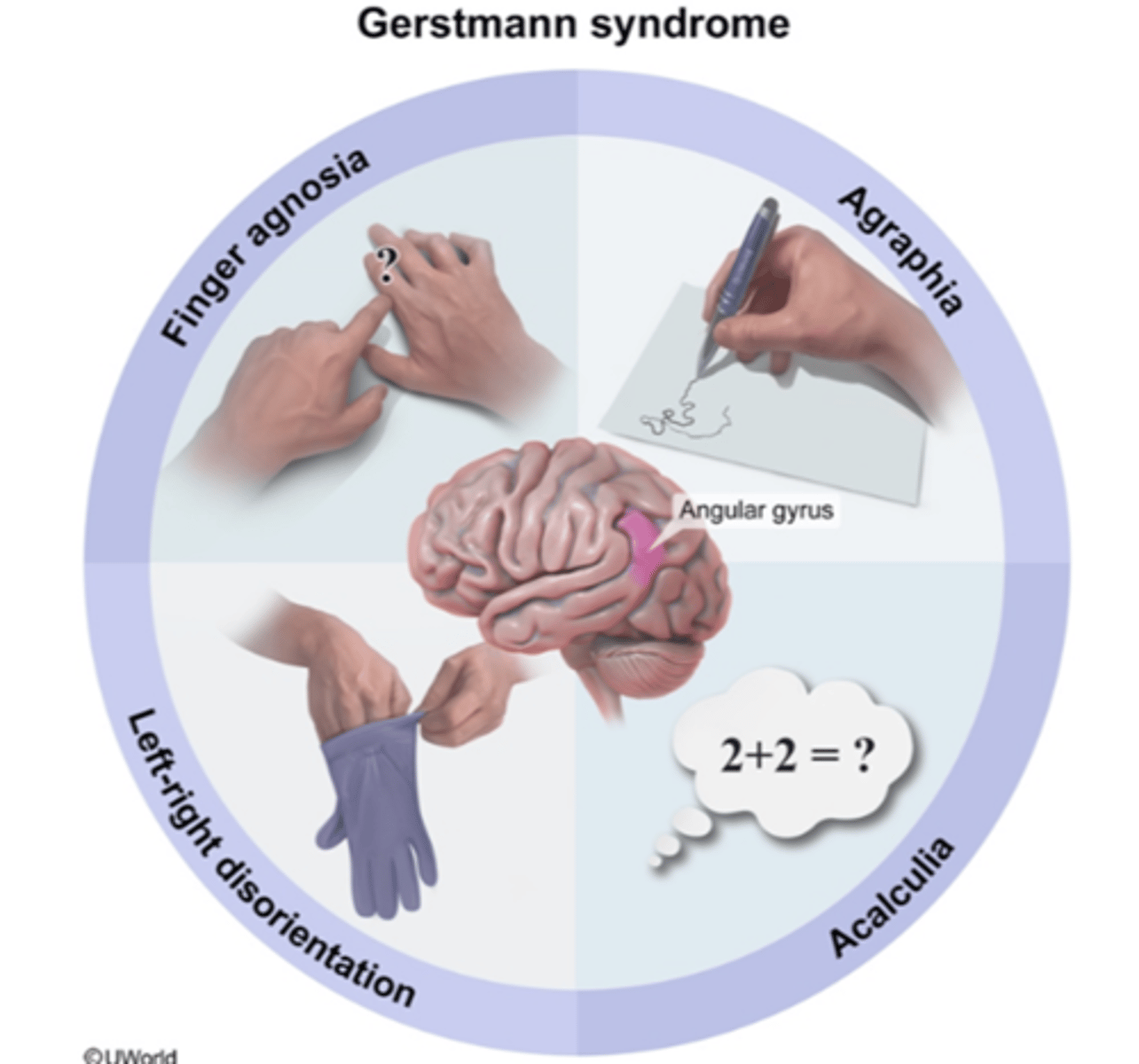
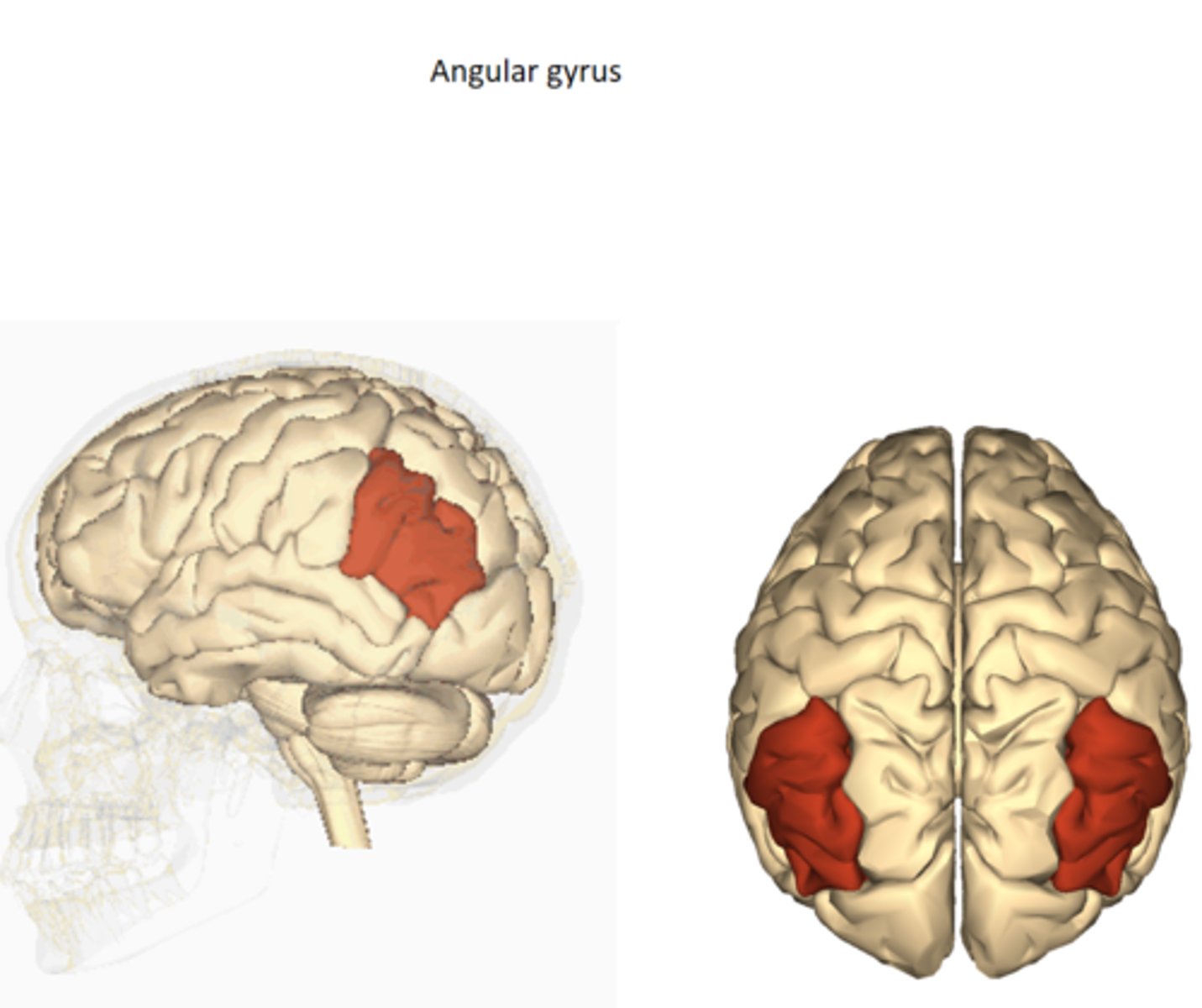
What causes Gerstmann's syndrome?
damage/lesion to inferior parietal cortex
OR
developmental
- usually on more dominant side; if you are right handed your left cortex is more dominant
- left cortex dominant --> affects right finger/toes/hands/etc
Apraxia
deficit in higher order motor planning
- LOSS of ability to CARRY OUT LEARNED/PURPOSEFUL MOVEMENTS
- they know the proper movement and what they need to do but they cannot execute it
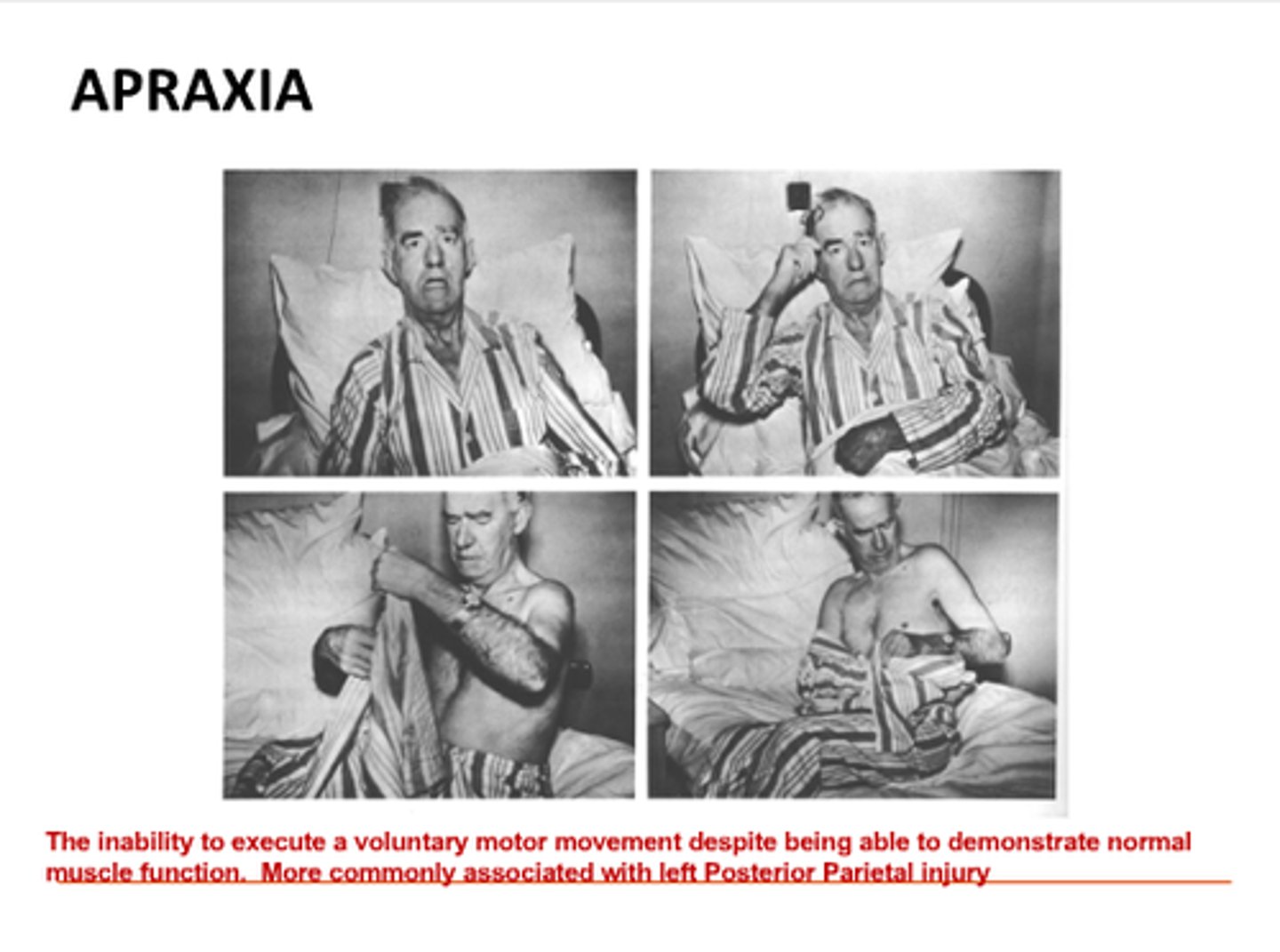
What causes apraxia?
damage/lesion in dominant parietal cortex