Lecture 25 - Sick Animal Nutrition
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
Yes
Is nutritional support an essential part of managing critically ill patients, especially if they are malnourished? Lack of proper nutrition will worsen the nutritional and metabolic state of critically ill patients, making it more difficult for them to recover, and increasing mortality.
Nutritional
The goals of what type of support are to treat malnutrition when present and to prevent it from developing?
Hypercatabolic
Elevations in endogenous corticosteroids, catecholamines, and inflammatory cytokines promote what type of state?
Simple
What type of starvation will involve decreased metabolic rate, low protein catabolism, high fat catabolism, use of fat and lipolysis for energy, and high levels of ketone production?
Stressed
What type of starvation will involve increased metabolic rate, high protein catabolism, low to no fat catabolism, use of muscle and proteolysis as the main source of energy, and low levels of ketone production?
3
How many days of anorexia are enough to produce severe metabolic changes and immune malfunction?
Energy
Lack of what will be indicated by weakness and recumbency in an ill patient?
Catabolic
The presence of what type of state will indicate an accelerated loss of lean body mass?
Yes
Will decreased tissue healing and increased risk of surgical dehiscence both occur in critically ill patients?
Albumin
Decreased synthesis of what protein in critically ill patients will lead to hypoalbuminemia and compromised drug-carrying capacity?
Yes
Will a compromised immune system and increased risk of nosocomial infections both occur in critically ill patients?
Enteral
Lack of what type of nutrition in critically ill patients will be indicated by gastrointestinal dysmotility, increased enterocyte turnover, and a compromised gut barrier function?
Hyporexia, Anorexia
What two eating habits, which refer to either reduced eating or complete lack of eating, can be caused by diseases of the liver, pancreas, kidney, GI, and endocrine systems? They can be associated or partially caused by electrolyte imbalances, acid-base imbalances, nausea, respiratory distress, inability to smell, pain, drugs like opioids, and CNS problems.
Trauma
Facial or head what can be considered a mechanical impediment leading to anorexia/hyporexia?
Oral
Neoplasia, foreign body, and dental problems are examples of mechanical impediments in the pharynx and what cavity, which can lead to anorexia/hyporexia?
Esophagus
Foreign body, neoplasia, and megaesophagus are examples of mechanical impediments in what structure, which causes hyporexia/anorexia?
Neuromuscular
What diseases can include tetanus, myositis, and myasthenia gravis, which are examples of mechanical impediments which can cause hyporexia/anorexia?
2
In the nutritional assessment, patients with how many or more high-risk factors present should receive nutritional support as soon as they are stabilized? Those with fewer than this many should be closely monitored and re-assessed every few days.
Low
Food intake < 80% RER for < 3 days and an expected course of illness < 3 days are considered what level of nutritional risk factor?
Moderate
Food intake < 80% RER for 3-5 days and an expected course of illness 2-3 days are considered what level of nutritional risk factor?
High
Food intake < 80% RER for > 5 days, anorexia > 3 days, presence of weight loss, severe vomiting/diarrhea, BCS < 4/9, muscle mass score < 2, hypoalbuminemia, and an expected course of illness of > 3 days are considered what level of nutritional risk factor?
Yes
Is it possible that catabolism of lean tissue may not be noted using standard BCS scoring systems if the patient has normal or excessive body fat?
Voluntary
What type of feeding must be assessed to ensure the adequate number of calories is being eaten? Caloric goals based on RER, food selection, and feeding plans are all used if this type is successful.
Assisted
What type of feeding includes enteral, parenteral, and combination feeding?
No
Should you ever do force feeding?
Yes
Before beginning feeding in an ill patient, should you address hydration status, electrolyte, and acid-base disturbances, and ensure that it is hemodynamically stable (not hypotensive or hypothermic)?
Enteral
What type of feeding is the preferred route, is more physiologic, less costly, and safer? It requires a functional digestive system, can be used even if only a small amount of food can be given, and should only be supplemented with parenteral nutrition when at least 50% RER cannot be met with this. This prevents intestinal villous atrophy, helps with maintenance of intestinal mucosal integrity, and preserves GI immunologic function.
No
Is enteral feeding indicated in cases of uncontrolled, incoercible vomiting, GI obstruction, ileus, severe IBD, and inability to protect the airway, such as in dysphagia, comatosity, and recumbency?
Enteral
The patient’s medical and nutritional status, anticipated length of time required for nutritional support, and consideration of the advantages/disadvantages presented by each route will influence selection of the route of which type of feeding to be used?
Proximal
Generally, enteral feeding should be given as what (relative location) as possible in the GI tract?
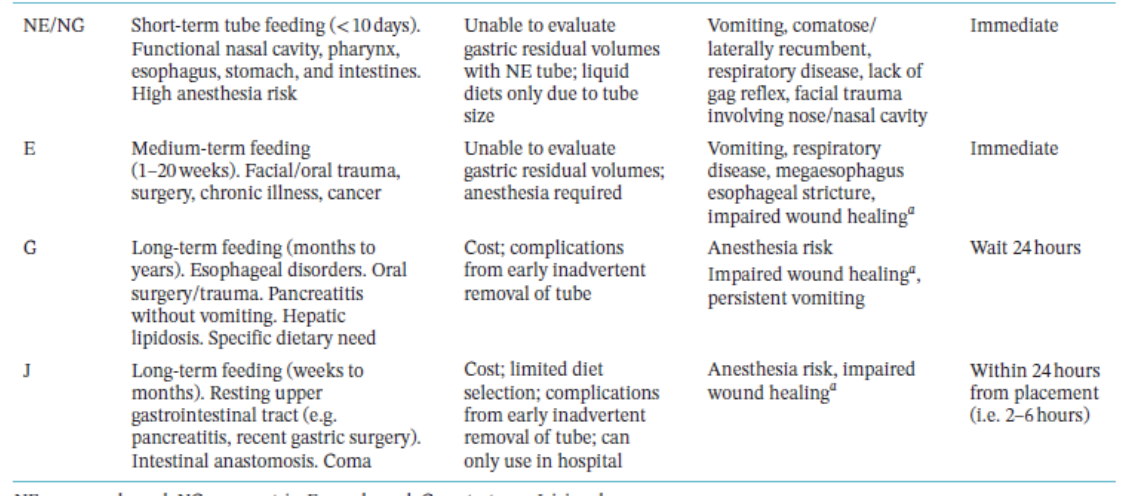
Nasogastric, Nasoesophageal
Which two tubes used for enteral feeding are easy to place, inexpensive, do not require general anesthesia, allow gastric decompression, and can be used immediately after placement? However they can only be used short term (< 7 days), can use only a liquid diet, can be dislodged, are prone to obstruction, and can cause nasal irritation. They can be used in cases of functional GI tract, short term feeding, and poor candidates for general anesthesia, but cannot be used in cases of nasal/facial trauma, respiratory diseases, comatosity, and lack of a gag reflex.
Nasogastric
What tube used for enteral feeding allows gastric decompression?
Nasoesophageal
What type of tube used for enteral feeding must be placed carefully to avoid lower esophageal sphincter incompetence, which may cause gastric reflux?
Aspiration
What technique is done with a syringe to ensure that a nasoesophageal/nasogastric tube is placed correctly? If it is negative, it is in the esophagus, if there is air and liquid, it is in the stomach, and if there is only air, it is in the trachea. X-rays (L-L) and injection of 3-5 ml sterile saline/water for injection not under sedation can also be done for confirmation.

Esophagostomy
What tubes used for enteral feeding are easy to place, can use semi-liquid diets, can be placed long term (20 weeks), can be used once the patient is awake, are well-tolerated, and can be given outpatient? They do require general anesthesia, can produce cellulitis or infection at the stoma site, can be dislodged, and are prone to obstruction.

Gastrostomy
What type of tube used for enteral feeding is a good long term option, is well-tolerated, and can be used with blenderized pet food? It is expensive, requires general anesthesia, can cause cellulitis or infection at the stoma site, includes risk of peritonitis, must be placed for 24 hours before using, and must be placed 10-14 days before being removed. It is good for animals with esophageal diseases. Surgical placement, endoscopic guidance, and blind technique can all be used.

Jejunostomy
Which tubes used for enteral feeding are used to feed distal to the pylorus and pancreatic duct? They are used only in hospital, are expensive, require general anesthesia, can cause cellulitis/infection at stoma site, cause risk of peritonitis, must be placed 24 hours before using, require CRI feeding, use only monomeric liquid diets, and cannot be removed before 7 days. Surgery, laparoscopy, nasojejunal, or gastrojejunal placement can all be used.

Enteral
These methods are all used for what type of feeding?
Resting Energy Requirement
What does RER stand for? It is used to determine the amount to be fed and is calculated by 70 x body weight (kg) ^ 0.75. It is measured in kcal/day. It should be used as a starting point, and animals receiving nutritional support should be closely monitored for tolerance of nutritional interventions. A continuing decline in body weight or body condition should prompt the clinician to reassess and perhaps modify the nutritional plan.
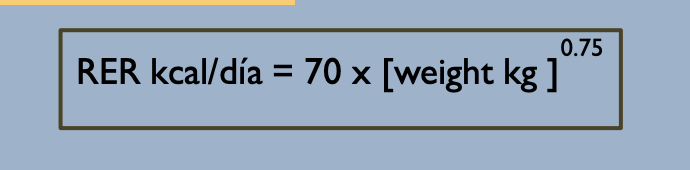
25
Feeding for critically ill patients should start with what percentage of RER? Gradual increments of this amount each day should be given if feeding is improving.
Underweight
What type of weight/condition is the ideal weight to estimate the RER?
25
The protein needs of dogs will be what percentage of total energy?
35
The protein needs of cats will be what percentage of total energy?
Rapid
What method/rate of feeding should be avoided because animals that have not eaten for several days have significant delays in gastric emptying and compromised overall intestinal motility, with signs like abdominal pain, distention, regurgitation, and vomiting? Hormonal disturbances may also be associated with poor food intake, causing metabolic derangements.
Bolus
What type of feeding uses no jejunal tubes, is given 4-6 times per day, no more than 10 ml/kg can be given, can tolerate 30-40 ml/kg per feeding, and depends on the maximum gastric capacity (dogs 50-90 ml/kg, cats 45-60 ml/kg)? Slow feeding over 15-20 minutes should be done, warm food should be given, the tube should be flushed with 5-10 ml of water before and after using, and the patient must be in a sitting position, sternal recumbency, and with the head higher than the body.
CRI
What type of feeding uses only jejunal tubes, and decreases malabsorption and diarrhea?
Refeeding
What syndrome can occur during tube feeding, when a sudden spike in insulin concentrations occurs? Prolonged anorexia with electrolyte imbalances, rapid shift of electrolytes from extracellular to intracellular space, hypokalemia, hypophosphatemia, and hypomagnesmia can occur.
Tubes
Feeding methods using what can include complications such as obstruction, migration, GI intolerance, aspiration pneumonia, and refeeding syndrome?
Micro-enteral
What type of nutrition is given only to feed the gut? This provides energy for enterocytes and immune cells, prevents villous atrophy, stimulates mesenteric blood flow, stimulates mucus secretion, stimulates digestive enzyme secretion, avoids ileus, uses nasogastric and nasoesophageal tubes, uses CRI at 0.25-2 ml/kg/hr, uses liquid diets, glutamine, and oral electrolyte solutions with dextrose of 2.5%.
Parenteral
What type of nutrition is given to patients that cannot tolerate enteral feeding, use a mixture of amino acids, glucose, and lipids, uses dedicated catheters, aseptic technique, is expensive, has high risk complications like sepsis and metabolic problems, and requires intensive monitoring and specialized equipment? It gives nutrients IV.

Total
What type of parenteral nutrition uses osmolality over 1000 mOm/L and a central line, and provides 100% RER?
Partial
What type of parenteral nutrition uses osmolality under 1000 mOsm/L and a peripheral catheter, and provides 70% RER?
Compounding
The solution used for parenteral nutrition is called what PN, and is ready made for this purpose?