Week 1: Course Intro and Anesthesia Equipment
1/105
Earn XP
Description and Tags
by MissKrisMarie
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
Who first demonstrated the use of nitrous oxide as an anesthetic in dentistry?
- Horace Wells
Who first discovered ether as an anesthetic?
- William Morton
Who was the first physician anesthetist?
- John Snow
Describe how the first, most basic form of barbiturates was developed.
- Barbituric acid was discovered by Adolf von Baeyer (1864) by combining urea and malonic acid. His discovery came on the feast day of St. Barbara (Dec. 4), so it is said he chose the name "barbiturate" as a combination of St. Barbara and "urea"
How is "The Manhattan Project" related to veterinary anesthesiology?
- It led to significant advances in the chemistry of halogenated hydrocarbons, which led to the development of our current inhalant anesthetics
What is anesthesia?
- A reversible state in which the patient is unconscious and unaware of painful sensations
What are the 3 types of anesthesia? What are the two methods?
- Types: Local, regional, general
- Methods: Injectable, inhalant
What is anesthesiology?
- The branch of medicine specializing in the use of drugs or other agents that causes insensibility to pain
What is an anesthetist?
- A nurse or technician trained to administer anesthetics (note the difference from an anesthesiologist - a physician or veterinarian who is specialized in the practice of anesthesiology)
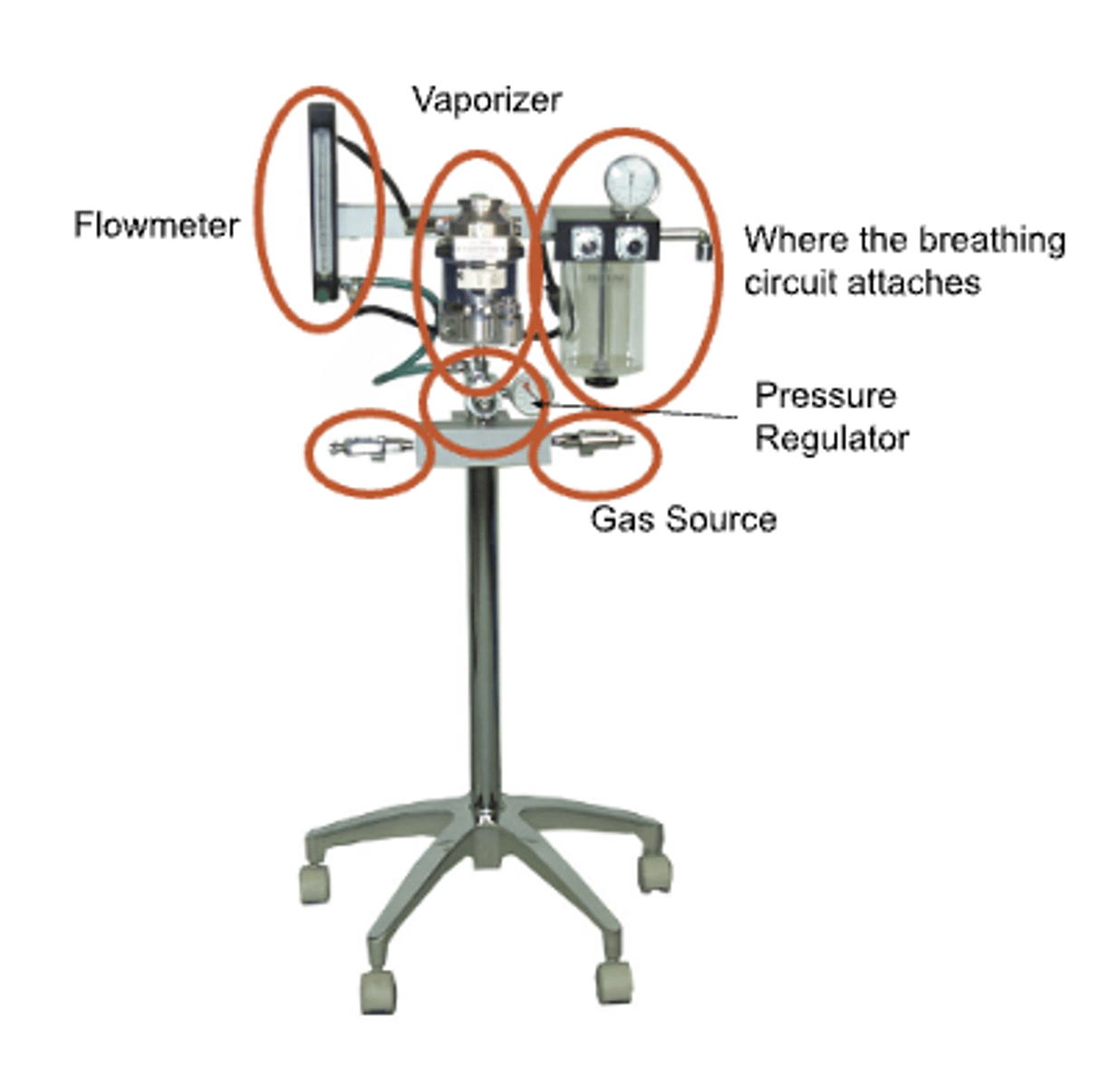
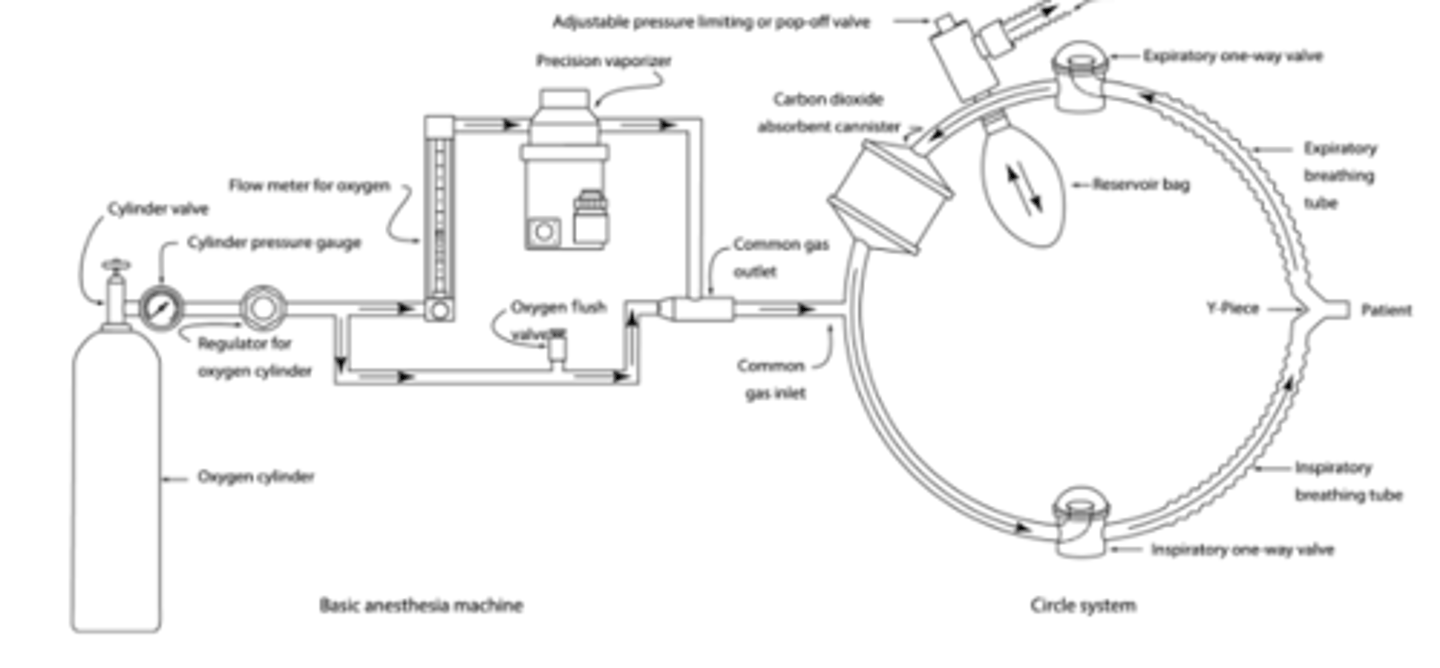
What are the four basic components of an anesthesia machine?
- A gas source (either a direct compressed gas chamber or vents in the facility)
- A pressure regulator
- A flowmeter
- A vaporizer
In veterinary medicine, anesthesia machines often come used from human medicine. What is the key difference between human and veterinary anesthesia machines?
- Human equipment has to meet a certain standard for safety; this is not true for veterinary use, so an advantage of human machines is additional safety standards
What are the five basic functions of an anesthetic machine and breathing circuit?
1) Provide a source of oxygen for our patients (usually better if greater oxygen content than room air)
2) Provide a means to support ventilation of our patients (manual vs. ventilator)
3) Provide a means of delivering inhalant anesthetics to our patients
4) Provide a means to removed exhaled CO2 from our patients
5) Provide a means to remove inhalant anesthetics from our work environment
The components of an anesthetic machine and breathing circuit can be broken down into the following categories. What pieces of equipment fall into each category?
A. Supply
B. Processing
C. Delivery
D. Disposal
A. Supply: Pipeline, cylinders, regulators
B. Processing: Flowmeters and vaporizer
C. Delivery: Breathing circuits and ventilators
D. Disposal: Scavenging system
Gas cylinders typically come at what pressure?
- 2200 psi
What are the two common types of gas cylinders?
- E cylinders (660 L O2) which are usually mounted to machines
- H cylinders (6900 L O2) which are for larger scale use and are mounted on dollies or chained to a wall.
What is within an oxygen cylinder?
- Oxygen gas under high pressure
What is within a nitrous oxide cylinder?
- Nitrous oxide liquid under high pressure
What is the difference between how oxygen and nitrous oxygen cylinders are depleted and when they need to be replaced?
- With oxygen cylinders, gas pressure falls linearly as oxygen is used (and/or the remaining volume can be calculated). It should be replaced when less than 200 psi
- With nitrous oxide cylinders, pressure doesn't fall until all liquid is depleted (~75% empty), so it should be replaced when pressure starts to fall
Regarding cylinder safety, cylinders are potential _____________.
- Missiles
Given that cylinders are potential missiles, what safety precautions need to be taken in handling them?
- Handle cautiously (prevent them from falling or getting knocked over)
- Store away from heat/fire
- Do not use oils or grease (silicone based lubricants only)
What is the most "economically efficient" way to store/transport oxygen?
- Liquid oxygen tanks which keep oxygen very cold - boiling point -297 F (1 cubic foot of liquid oxygen = 24338 L oxygen gas)
- Note: This is what supplies the VTH
In what context are oxygen concentrators most commonly used?
- Home environments for people who need oxygen support at home (rarely get above 95% oxygen)
What are the 2 primary ways to connect gas sources to the anesthetic machine?
1) Hanger yolks (E cylinders)
2) Pipeline systems
What are PISS and DISS?
- Pin Index Safety System and Diameter Index Safety System which are systems to prevent cross connections of cylinders, pipelines, and machines (i.e., it is impossible to attach an oxygen cylinder to a nitrous oxide hanger yolk and to attach an oxygen hose to an air attachment)
What are the steps for attaching a cylinder to an anesthetic machine?
- Remove the plastic wrap and place the washer on the hanger yoke.
- "Crack" the valve (i.e. open it slowly)
- Use toe to help lift and stabilize the cylinder
- Align pins and gas outlet
- Tighten securely (righty tighty, left loosey)
What is the function of regulators? What are the two types?
- Reduce high pressure from cylinders to lower constant pressure tolerated by the flowmeters
- Cylinder regulators (reduce pressure to 45 psi) and pipeline regulators (reduce pressure to 50 psi)
Describe the relationship between cylinder and pipeline regulators and the flow of gas from the cylinder.
- If the pipeline pressure is 50 and the cylinder is 45, then the pipeline check valve is closed and oxygen will not flow out of the cylinder. This only opens/the cylinder is only used when psi falls below 45 psi.
True or false: Regulators commonly cause mishaps with anesthesia.
- False; Regulators are often not easily visible, and rarely cause machine malfunctions
What is the function of flowmeters?
- Allow precise control of gas flow to the patient
Why is it significant that flowmeter knobs have different "feels" based on the type of gas?
- You can reach over and adjust it and know what you are adjusting without visualizing it.
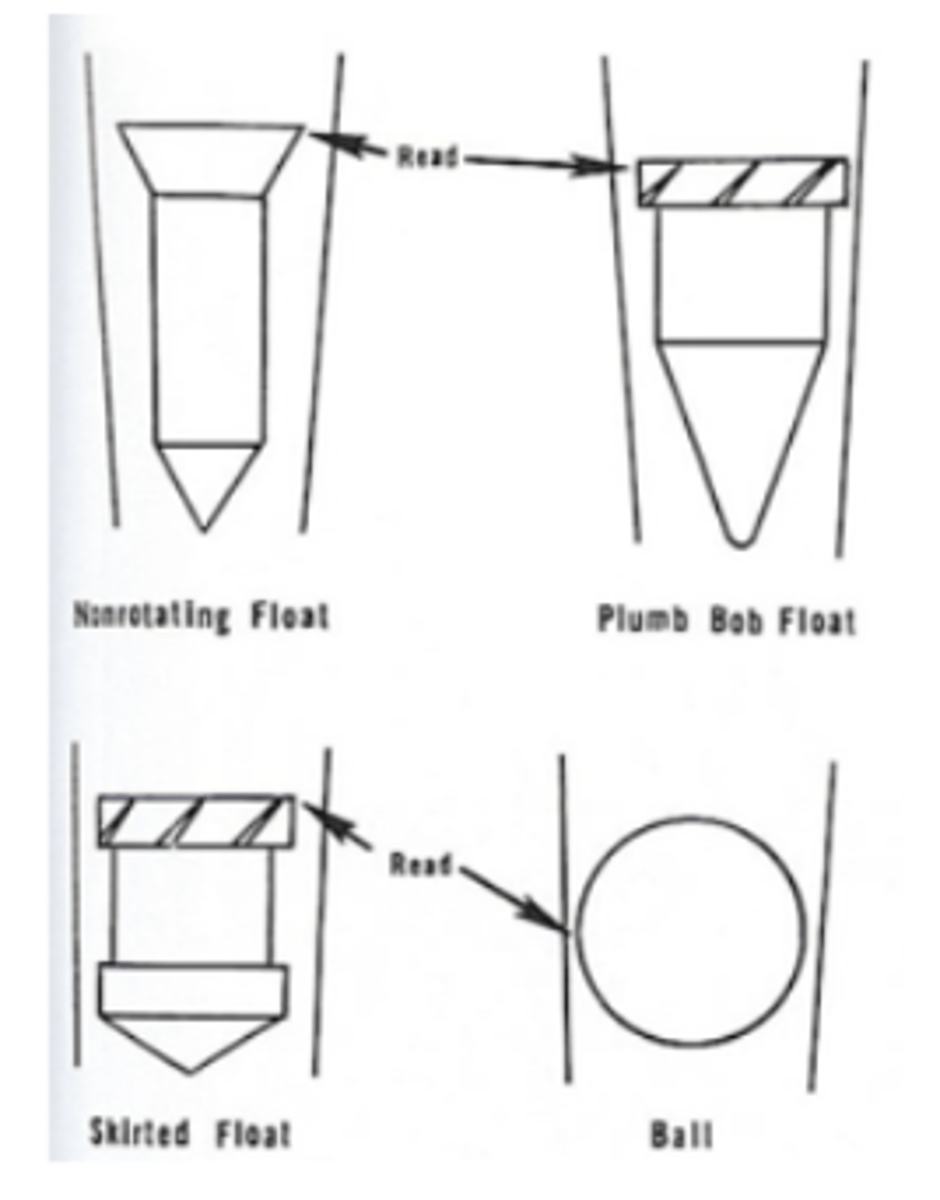
How are flowmeters read?
- Top of the bobbin or middle of the ball
Why must one be careful/gentle when adjusting flowmeters? How tight should these be?
- They are made of brass and if they are cranked down on firmly all the time, the valve will wear and leak.
- They should be finger tight.
What is the function of a vaporizer?
- Convert volatile anesthetics from liquid phase to vapor phase
What are the classifications of vaporizers?
- Prevision vs. non-precision
- Out-of-circuit vs. in-circuit
Most vaporizers are "in" or "out" of circuit? Precision or non-precision?
- "out-of-circuit" and precision
Vaporizers provide compensation for what factors?
- Temperature
- Flow
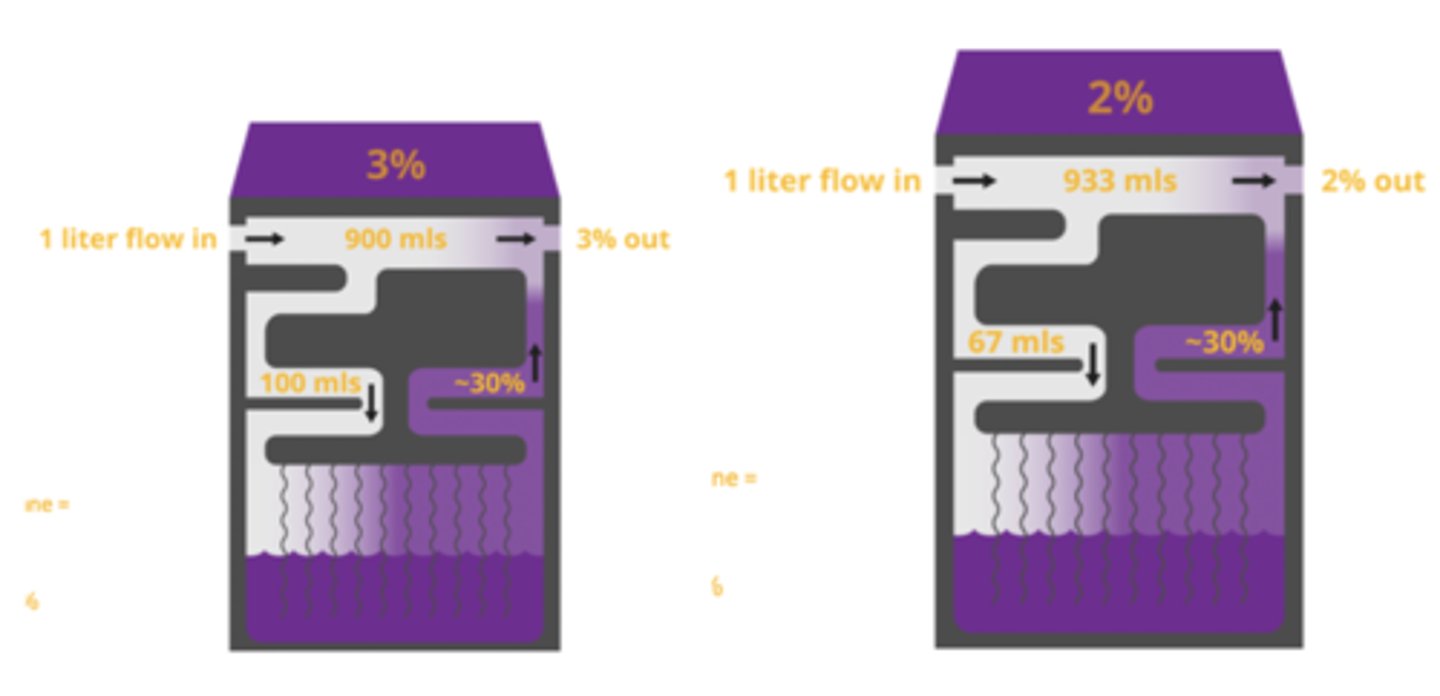
When gas enters the vaporizer and picks up anesthetic, what percentage anesthetic is the gas which picks it up?
- (240/760)*100 = 31.6%
- Note: Not all the gas entering the vaporizer picks up anesthetic
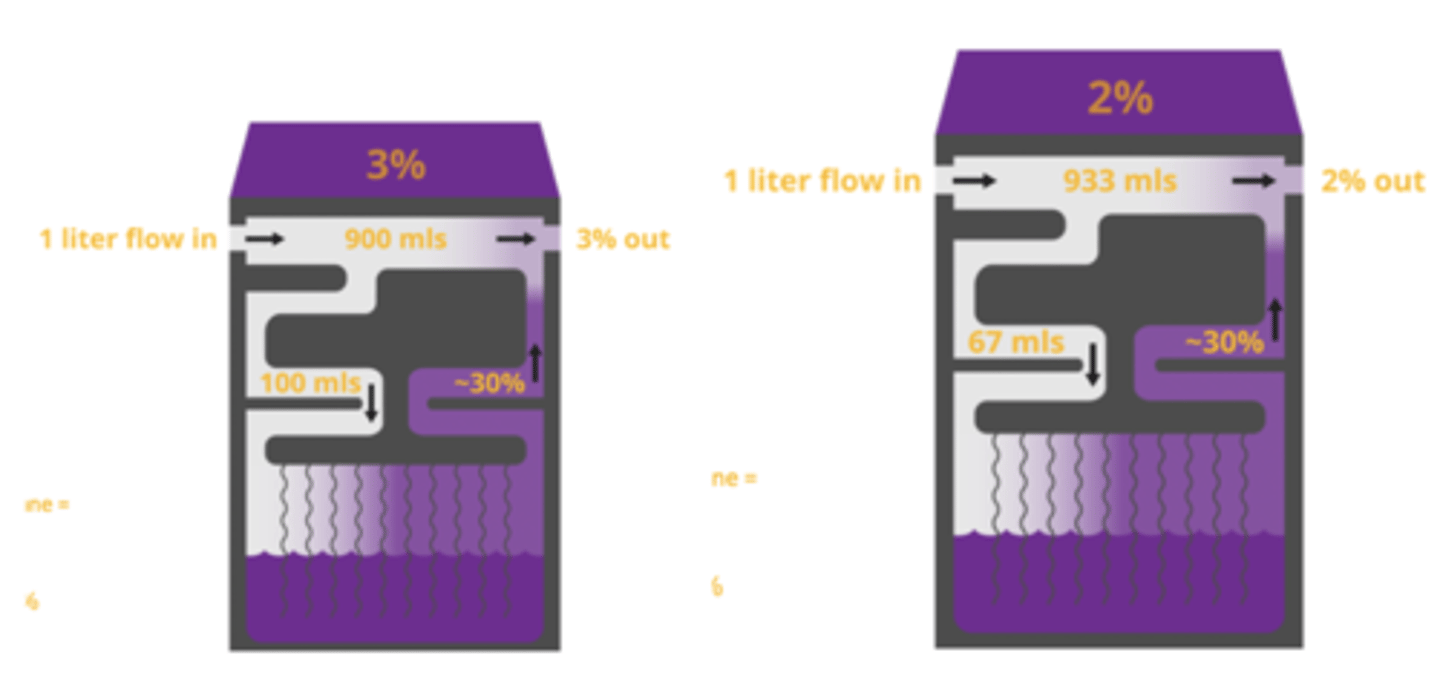
What changes within the vaporizer when adjusted?
- The amount of gas flowing to pick up anesthetic
What is the primary reason Desflurane is not commonly used in veterinary medicine?
- Requires the Tec-6 vaporizer (more complicated, more expensive vaporizer)
What is the purpose of Keyed filling devices of vaporizers?
- Makes it virtually impossible to fill a vaporizer with the wrong gas (there are some vaporizers that don't have this and simply have funnels)
What is the function of the flush valve?
- Bypasses the vaporizer and deliver a high flow rat of oxygen directly to the patient's breathing circuit used to rapidly decrease the inhalant concentration in the breathing circuit ("wake up" button)
Should the oxygen flush valve be used to fill the reservoir bag at the start of anesthesia?
- No; Use normal oxygen flow as this will maintain the inhalant anesthesia concentration
Using the oxygen flush valve leaves potential for ___________ in small patients, especially on non-rebreathing circuits.
- Barotrauma
What is the common gas outlet?
- The interface between an anesthetic machine and the patient breathing circuit where blended anesthetic agent an carrier gas exit the machine
- Note: It has a universal fitting to connect to various types of breathing circuits
What do breathing systems (Circuits) provide?
- Delivery of O2 and inhalant to the patient
- Elimination of CO2 from the patient
- A means of ventilation
What is the definition of a "rebreathing" system?
- "Circle system" -> Inhalation of gases that have been recently exhaled.
What are some benefits of a circle ("rebreathing") system?
- Rebreathe O2 & inhalants (reduce $$$ and environmentally friendly)
- Decreased heat and moisture loss
- Larger volume with buffers from barotrauma (especially when hitting the flush valve)
- Any type of vaporizer will work
- Wider range of flow rates
- Greater familiarity for most people
What oxygen flow rates should be used for a circle system?
- Higher flows initially (first 10-20 minutes) at 50-100 mL/kg/min
- Lower flows for maintenance at 20-50 mL/kg/min with changes as needed
What is the basic reaction involved in carbon dioxide absorption? How can you tell when the reaction is completed?
- CO2 + H2O + CaOH -> CaCO3 + H20 + energy (heat)
- The active ingredient is CaOH (soft, crushable compound) while CaCO3 (limestone) is hard. Once the material is hard and non-crushable, you will know it's done.
Describe how color indicators are used in determining when carbon dioxide absorbent needs to be changed.
- The color changes with blue or violet when used up, but it will return to white with lack of use so if it goes bad and is not checked until the next morning, it may be missed. When exposed to CO2 again, the color will again become blue/violet.
As a rule of thumb, carbon dioxide absorbent needs to be changed how frequently?
- Every 8 hours of use (highly variable)
If the carbon dioxide absorbent has expired and is used for a patient's anesthesia, you would expect the inspired CO2 to ________________.
- Potentially increase
What is the function of reservoir bags?
- Provide reservoir of gas from which the patient can breathe (Peak tracheal inspiratory flow is greater than the fresh gas flow, so the patient takes gas from the reservoir when taking a breath)
What size should a reservoir bag be?
- 3-6x the patient's tidal volume (most people say 6) -> Must be big enough so when the patient takes a deep breath, the reservoir bag isn't emptied/sucked flat.
Generally speaking, what size reservoir bag is fit for each of the following patients?
A. Cat/toy breed dog
B. Medium to large breed dog
C. Large animals
A. 0.5 liters
B. 1-3 liters
C. 5-30 liters
What are the benefits of a "non-rebreather" system?
- Simple and valveless (minimal resistance to ventilation)
- Rapid changes in anesthetic depth (changes in vaporizer setting rapidly reflected in the patient)
- Fewer connections/parts for leaks to develop
- No CO2 absorbent to become exhausted
Why are changes in anesthetic depth reflected more rapidly after changing the vaporizer settings with a non-rebreather system compared to a circle system?
- Patient is taking gas essentially straight from the anesthetic machine; with the circle system you have wash-in to build up the concentration, so things happen a bit faster on a non-rebreathing system
What are the most common types of "non-rebreather" systems?
- Modified Bain
- Jackson-Rees
What are the components of a "non-rebreather" system?
- Hose with ET tube adapter
- Breathing bag
- Hose to connect to common gas outlet on machine
- Option: Pressure gauge and pressure relief valve
How do "non-rebreather" systems prevent rebreathing?
- Dependent on adequate fresh gas flow so when the patient expires, the exhaled gas is pushed far enough down the exhalatory limb, when the patient inhales, it may move back toward the patient, but not enough for them to inhale the alveolar gas.
What is a potential limitation of "non-rebreather" systems?
- Disconnection of the inner tube leading to huge amounts of dead space and tons of inspired CO2
- Inefficient method of delivery anesthesia
What is the recommended oxygen flow rate for "non-rebreather" systems?
- Same flow rate used throughout anesthesia at about 100-200 mL/kg/min
Why are "non-rebreather" systems generally only used in patients under a certain size?
- It is a hugely inefficient way to deliver anesthetic to larger patients and flow rates don't go as high as would be necessary
What are some things to consider when deciding whether a patient is a good candidate for a "non-rebreather" system?
- Consider using when patient is under a certain weight (i.e. 5 kg)
- However, consider special circumstances. For instance, an obese cat weighing 8 kg may still be a good candidate as it has the lungs of a 5 kg cat
What is involved in a basic machine checklist prior to use?
- Connect and check oxygen supply
- Check vaporizer fill levels
- Leak check the breathing system
- Check the scavenging system
How do you leak check a breathing system?
- Close pop-off, occlude patient connection (only two sources gas can leave the system), pressurize to 30 cmH2O, should hold for > 10 sec
- Notes: Use the flowmeter to pressurize the system (not the flush valve) and When you release pressure, do it by opening the pop-off valve, not by removing the occlusion of the patient connection (this demonstrates the pop-off valve can open appropriate and leaves the pop-off valve in the open position, which it needs to be during induction/anesthetic maintenance).
If a breathing system is found to be leaking, what is the next step?
- Spray the system with water and look for bubbles to find the leak
What does APL valve stand for?
- Adjustable Pressure-Limiting Valve
Where is the APL or pop-off valve located?
- Located at interface between breathing circuit & scavenging system
What does the APL or pop-off valve control?
- Control's "fill" of breathing circuit
When providing positive pressure ventilation ("giving a breath"), what should be done with the pop-off valve?
- It should be closed, but then immediately opened again once done
What is an easy visual assessment of whether there is excessive pressure
- Look for creases on the reservoir bag (if there are creases, there is no excessive pressure in the circuit)
What are some potential/certain sequelae of leaving a pop-off valve closed?
- Barotrauma (but most likely the patient would be dead before this happens because of the next sequelae)
- Collapse of the great veins secondary to increased intrathoracic pressure -> Cardiovascular collapse and cardiac arrest due to reduced venous return -> BP drops -> Apnea
What is a "pop-off occlusion valve"?
- A device which acts as a button to hold down over the pop-off valve to hold it closed transiently (not sufficient for pressure checking a breathing system).

Mechanical ventilators are essentially glorified what?
- Mechanical breathing bags; Always attach to the same place as the reservoir bag on a breathing circuit
Ventilators are limited by what?
- They can be volume limited, pressure limited, or both
Ventilators have a built-in ______________________.
- Pop-off valve
What needs to be done with the pop-off valve when switching to using a ventilator and when weaning off of a ventilator?
- When switching to a ventilator, close the pop-off valve on the breathing circuit
- When you wean off the ventilator, make sure you open the valve again
When the ventilator is in use, what forces open/close the bellows?
- Drive gas closes the bellows
- Patient's alveolar air opens the bellows
What is the function of a scavenging system?
- Evacuate waste to the outside environment
What are the two types of scavenging systems?
- Active
- Passive
How can activated charcoal be used as a scavenging agent?
- It is inexpensive and absorbs halogenated hydrocarbons (not nitrous oxide) and can be used for portable anesthesia (i.e. moving patient from room to room) but must be changed routinely (keep track of canister weight which can hold up to X grams)
According to normal anatomy, is the epiglottis located behind or in front of the soft palate?
- Behind
Why is it important to always use a laryngoscope?
- While you may not always need one, once in a while you may seriously need one. If it is not used routinely, it will have to be found, may be uncharged/burned out. When used routinely, they are consistently in working order and everyone is familiar with how to use them.
When performing endotracheal intubation, it is best to avoid touching the ___________, especially in cats who are more prone to laryngospasm.
- Epiglottis
Lidocaine spray/drops is most commonly used in cats during intubation for what purpose?
- To reduce laryngospasm (not obliterate)
Once lidocaine spray has been applied to the larynx, can you intubate immediately?
- No; Lidocaine doesn't work instantly on mucosal membranes (takes 15-30 seconds)
How inflated should ET cuffs be?
- Inflation should be titrated to prevent a leak at 20 cm H20 and no more.
When performing an intubation using an ET tube, place the tip of the laryngoscope at the base of the ____________ (but avoid touching the epiglottis itself) which pulls it down from behind the ___________________ ____________________. Then you can visualize the ____________________ ____________________.
- Epiglottis
- Soft palate
- Arytenoid cartilages
What are the different types of laryngoscope blades?
- Miller
- Macintosh
- Cranwell (Preferred by Dr. M)
If you are gonna error in the length of your laryngoscope blade, error on the side of too __________.
- Long
What are the different types of ET tubes?
- Murphy (Has the eye in it)
- Magill
- Cole
What are the different material types for ET tubes?
- Silicone (larger than size 10 at the VTH)
- Polyvinyl chloride (Up to size 10 at the VTH)
- Red rubber
What are the different types of cuffs for ET tubes?
- Low volume/high pressure
- High volume/low pressure
Why are Murphy ET Tubes preferred?
- If the tube is positioned in such a way that the bevel is positioned against the tracheal wall, this can lead to airway occlusions. The murphy eye prevents this.
What are some method for choosing a properly sized ET tube?
- Nasal septum width
- Charts based on weight
- Tracheal palpation
- Clinical experience
- Visualization of the glottis
What is particular about choosing ET tubes for brachycephalic dogs?
- Brachycephalic dogs may have a hypoplastic trachea -> Be prepared with smaller than normal sizes
When selecting an ET tube, you want to chose the largest or smallest size possible? Why?
- Largest
- The tube is the largest source of resistance in the anesthetic system
Where should the proximal and distal ends of an ET tube be located?
- Proximal end should be at the level of the incisors/tip of the nose
- The distal end should be between the larynx and the thoracic inlet (should not extend beyond the carina)
What happens if the ET tube is too long?
- Excessive dead space