Physiological Control when Breathing
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
12 Terms
Average breaths per day
~20,000 taken unconsciously
How does unconscious contraction of respiratory muscles occur?
Respiratory muscles are skeletal (voluntary) muscles.
However, their contractions are controlled within the respiratory centre of the brain stem.
Medulla oblongata & pons
Medulla neurons:
2 groups
dorsal respiratory group (DRG)
ventral respiratory group (VRG)
Medulla neurons:
dorsal respiratory group (DRG)
Maintain the rhythm of normal, quiet breathing
When inhaling:
Increase DRG activity → contraction of diaphragm/external intercostals.
When exhaling:
Decrease DRG activity → relaxation of diaphragm/external intercostals.
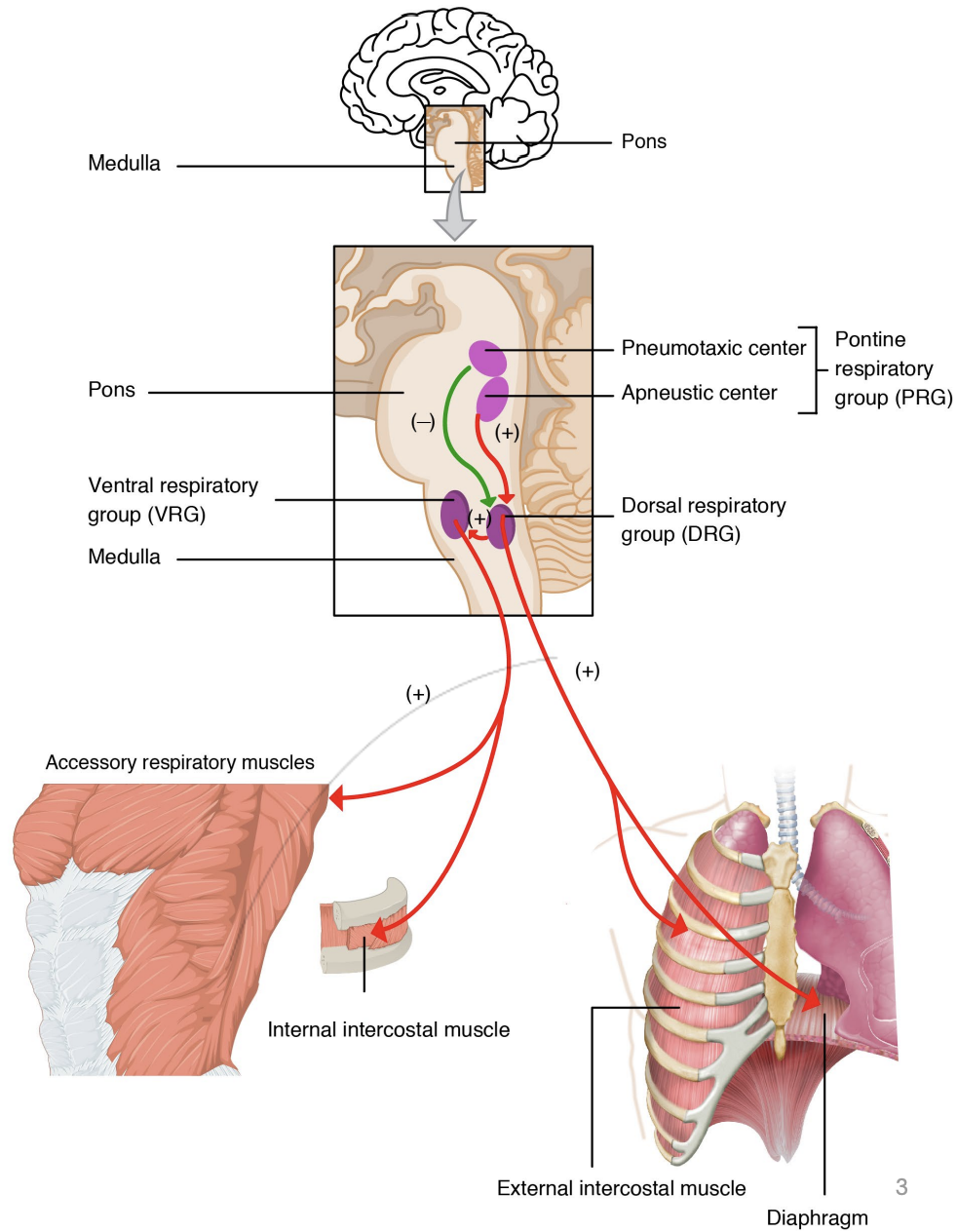
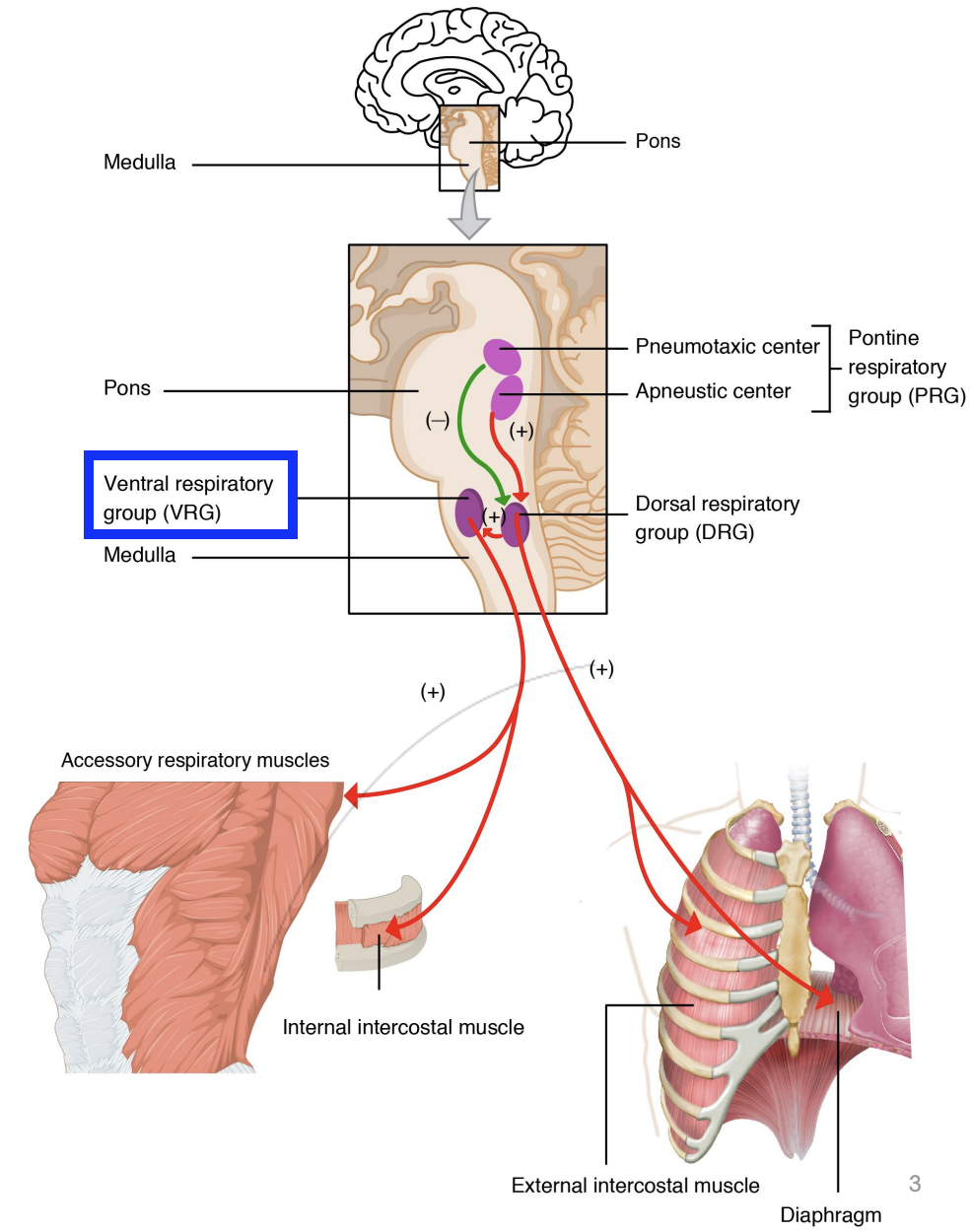
Medulla neurons:
ventral respiratory group (VRG)
Active during forced, controlled breathing.
When inhaling & exhaling:
Innervates accessory respiratory muscles
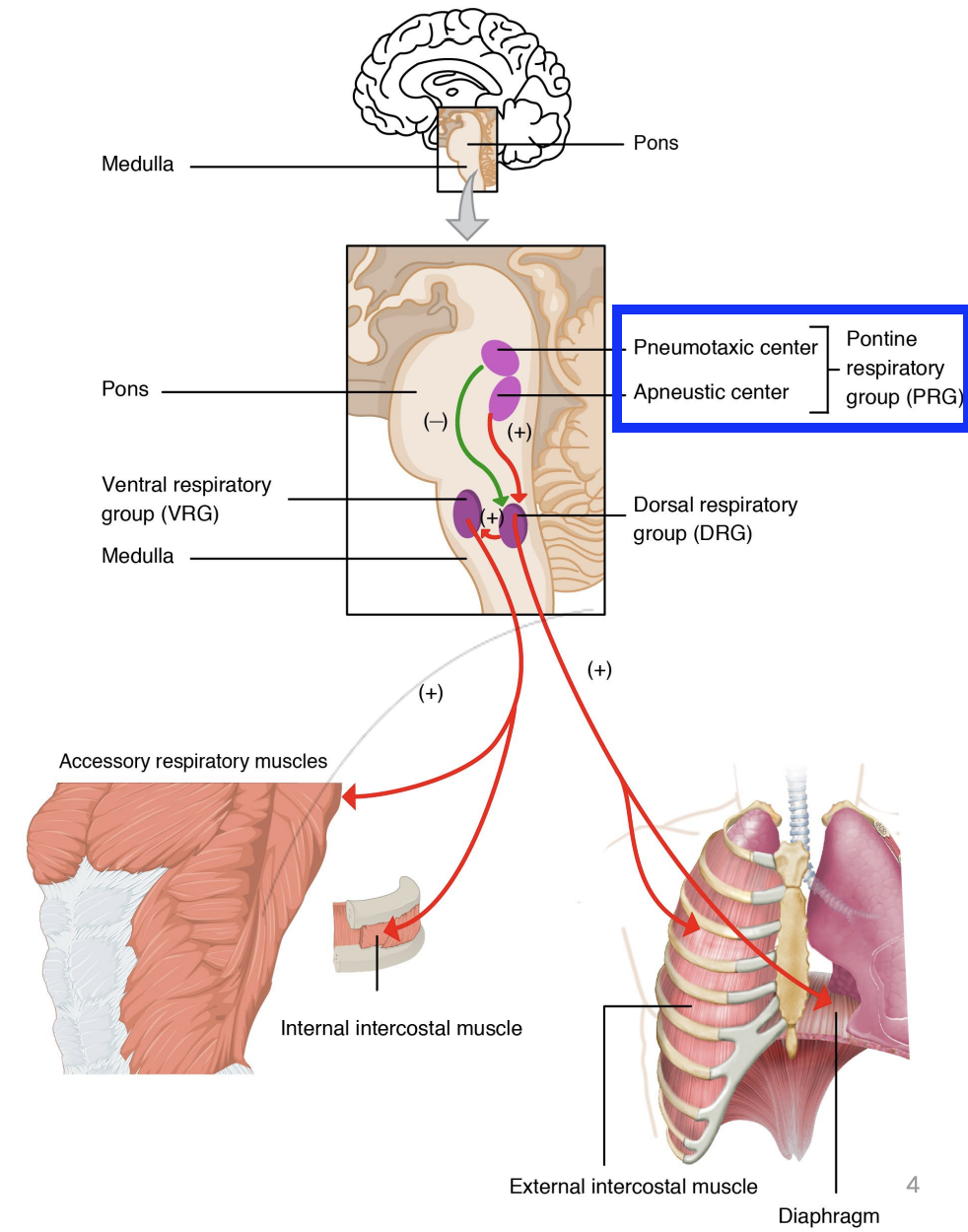
Pons neurons:
1 group
pontine respiratory group (PRG)
Pons neurons:
pontine respiratory group (PRG)
Modifies activity of the DRG based on inputs from various receptors/brain regions (sensory information received)
What information is sent to the brain to control breathing?
Chemoreceptors
Higher brain centres
Conscious control of things
Varying emotions (being frightened)
Irritant receptors in lungs
senses irritants, can cause coughing
Stretch receptors in lungs
Reason why after holding breath for too long, feels like lungs are being stretched too far (not actually stretching)
Proprioceptors in muscles/joints
Chemoreceptors in lungs:
2 types
Central chemoreceptors (in brainstem)
Peripheral chemoreceptors (carotid arteries & aortic arch)
Central chemoreceptors
Brainstem
Respond to changes in pH/pCO2 in cerebrospinal fluid (CSF)
Detects changes in H+ ions
Not sensitive to changes in pO2
If pCO2 goes up, H+ ions go up, pH decreases.
Signals for more breathing to occur, so CO2 exits the body
Peripheral chemoreceptors
Carotid arteries & aortic arch
respond to changes in pCO2, pH and pO2 in blood
We are much less sensitive to changes in pO2 and it can drop a long way before peripheral chemoreceptors detect a problem (needs to drop below ~60 mmHg)
Stimulates brain to have more breathing occur
Mainly because RBCs/Hb are so good at binding/delivering O2, they can do it efficiently even if pO2 drops
Peripheral chemoreceptors are STILL more responsive to increases in CO2 than drops in O2
Does the brain moniter pO2 or pCO2 more attentively?
pCO2 is the primary determinant of breathing rate
Why?
Because the Carbonic anhydrase reaction:
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3-
Changes H+ ion concentration, which controls pH.
The body reacts strongly to changes in pH, a certain level of pH must be maintained for optimal activity.
Haemoglobin is very forgiving which changes in pO2 (can drop from 100 mmHg to 75 mmHg without a steep decline in haemoglobin saturation). changes in pO2 are much more forgiving than changes in pCO2