4. Innate Immunity II: Cellular
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
The innate immune system contains multiple specialised cell types, including ____________ (professional phagocytes derived from monocytes), ____________ (professional phagocytes with segmented nuclei and antimicrobial granules), ____________ (cells effective against large parasites), ____________ and ______ ______ (granulated cells that release mediators in acute inflammation), and _______ ______ ______ (cells that kill virus-infected and tumour cells).
The innate immune system contains multiple specialised cell types, including macrophages (professional phagocytes derived from monocytes), neutrophils (professional phagocytes with segmented nuclei and antimicrobial granules), eosinophils (cells effective against large parasites), basophils and mast cells (granulated cells that release mediators in acute inflammation), and natural killer cells (cells that kill virus-infected and tumour cells).
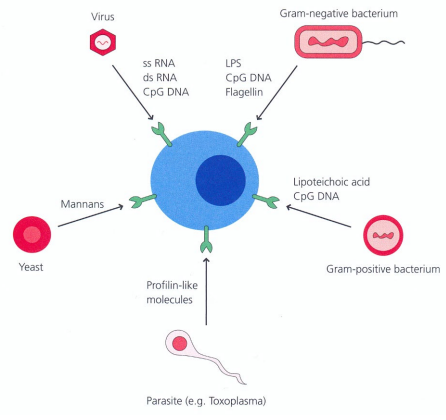
Innate immunity differentiates between “self” and “non-self” by recognising ____________ ____________ ____________ ____________ (PAMPs), such as ____________ (Gram-negative bacteria), ____________ _____ (Gram-positive bacteria), and _______ (fungal cell walls).
Innate immunity differentiates between “self” and “non-self” by recognising pathogen associated molecular patterns (PAMPs), such as lipopolysaccharide (Gram-negative bacteria), lipoteichoic acid (Gram-positive bacteria), and mannans (fungal cell walls).
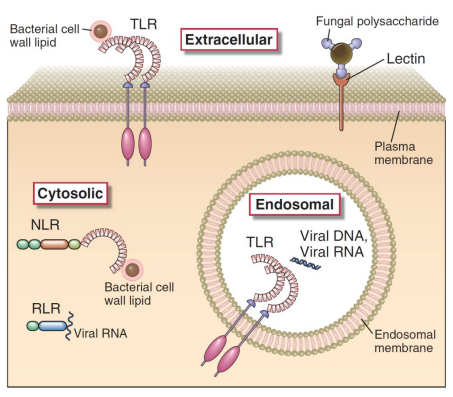
Host structures that detect PAMPs are called ____________ ____________ ____________ (PRRs); the largest family consists of ____________ ____________ ____________ (TLRs), while some receptors are intracellular or secreted, e.g. _________ ____.
Host structures that detect PAMPs are called pattern recognition receptors (PRRs); the largest family consists of toll like receptors (TLRs), while some receptors are intracellular or secreted, e.g. soluble CD14.
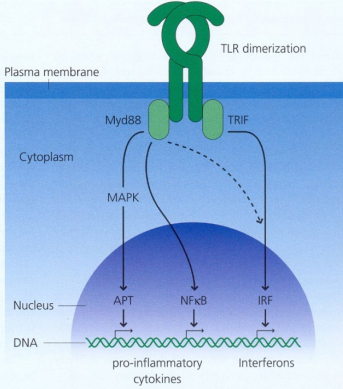
Activation of TLRs causes ____________ of receptors and binding of adaptor molecules such as ________ and ________; signalling = activation of ________ and production of pro-inflammatory ____________, stimulation of adaptive immunity and/or interferon.
Activation of TLRs causes dimerisation of receptors and binding of adaptor molecules such as Myd88 and TRIF; signalling = activation of genes and production of pro-inflammatory cytokines, stimulation of adaptive immunity and/or interferon.
What activates macrophages and what are the effects of this activation?
Activated by microbial products and NK-cell-derived IFN-γ
Activation ↑ transcription of genes for killing, cytokine release, inflammation, and support of adaptive immunity (note: killing requires extra stimulation even after phagocytosis (being engulfed)).
What are cytokines and chemokines?
Cytokines act antigen-non-specifically to drive inflammation and systemic effects (e.g. IL-1, IL-6, IL-8, IL-12, TNF-α)
Chemokines = cytokines for chemotaxis (directed cell movement toward a stimulus) (e.g. CXCL8 / IL-8)
What are the local, systemic, and pathological effects of pro-inflammatory cytokines?
Local inflammation (site of infection):
↑ vascular permeability (allows plasma proteins + cells to enter tissue)
↑ expression of adhesion molecules on endothelium
Recruitment of neutrophils + monocytes to infection site
Systemic protective effects:
Fever (↑ body temp)
↑ production of acute-phase proteins (e.g. CRP, MBL, fibrinogen)
Leukocytosis (↑ WBC production in bone marrow)
Systemic pathological effects:
↓ heart rate (septic shock effect)
↑ vascular permeability = ↓ blood pressure (hypotension)
Insulin resistance (TNF-α mediated)
What are the key features of phagocytic cells in innate immunity?
Large ____________ & smaller _______________ _________ (PMNs) are the major cells that phagocytose material
Macrophages exist in different forms with different ________ depending on body site
Not every phagocytic event leads to digestion; macrophages may need activation by ________
Macrophages can present antigen to _ cells; ______ cells are specialised APCs
Large macrophages & smaller polymorphonuclear leucocytes (PMNs) are the major cells that phagocytose material
Macrophages exist in different forms with different names depending on body site
Not every phagocytic event leads to digestion; macrophages may need activation by IFNγ
Macrophages can present antigen to T cells; dendritic cells are specialised APCs
What are the key features of neutrophils in innate immunity?
Produced in ______ _____; differentiate from stem cells in ~ weeks
Known as ____________ (PMN) leukocytes due to segmented nuclei
Granulated; granules contain antimicrobial substances for killing ________, ________, & ________
~5% enter peripheral blood with a half-life of ___ hours
During infection, neutrophil numbers ↑ to ______ new cells per day
Produced in bone marrow; differentiate from stem cells in ~2 weeks
Known as polymorphonuclear (PMN) leukocytes due to segmented nuclei
Granulated; granules contain antimicrobial substances for killing bacteria, fungi, & protozoa
~5% enter peripheral blood with a half-life of 6.5 hours
During infection, neutrophil numbers ↑ to 10¹² new cells per day
What is neutrophil margination & how are neutrophils recruited to tissues?
In healthy individuals, neutrophils are rarely seen in ________
In blood vessels they roll along the margin = ________
A ________ ________ on neutrophils interacts weakly with endothelial ________
Tissue damage or infection releases ________ that attract neutrophils to the site
In healthy individuals, neutrophils are rarely seen in tissues
In blood vessels they roll along the margin = margination
A selectin ligand on neutrophils interacts weakly with endothelial glycoproteins
Tissue damage or infection releases mediators that attract neutrophils to the site
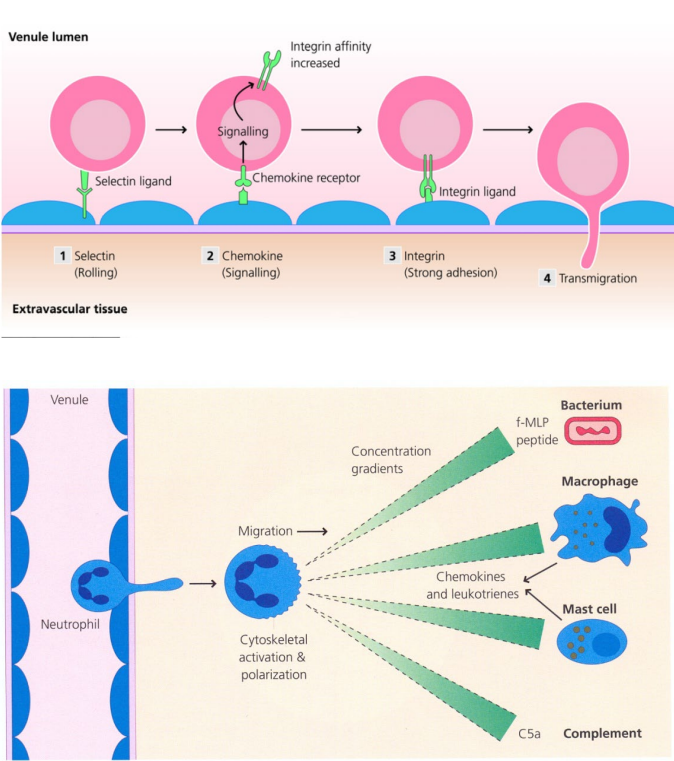
How do neutrophils undergo diapedesis in response to tissue distress?
In response to distress signals (e.g. complement & cytokines like ____-) the endothelium expresses _________ __________
These adhesion molecules (ICAMs) cause neutrophils to bind _________ to endothelial cells
_________ cause neutrophils to cross endothelial junctions = __________
Neutrophils then enter extravascular tissue towards the site of _________ or _________
In response to distress signals (e.g. complement & cytokines like TNF-α) the endothelium expresses adhesion molecules
These adhesion molecules (ICAMs) cause neutrophils to bind tightly to endothelial cells
Chemotaxins cause neutrophils to cross endothelial junctions = diapedesis
Neutrophils then enter extravascular tissue towards the site of infection or injury
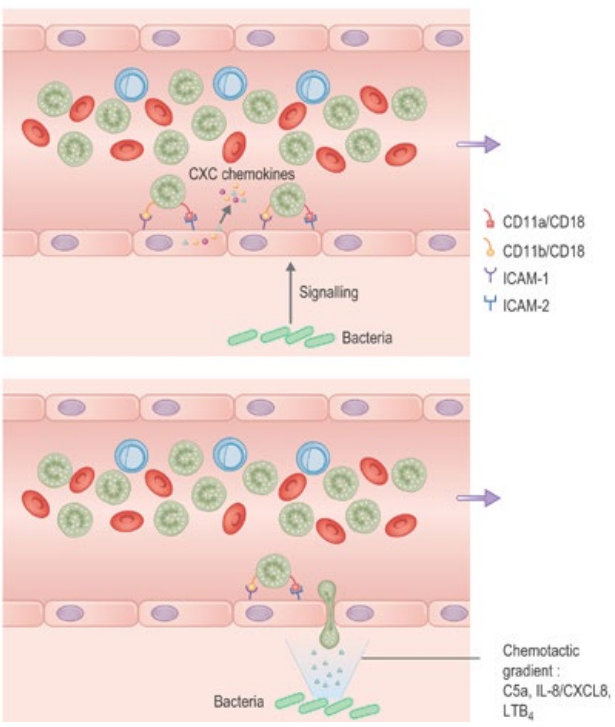
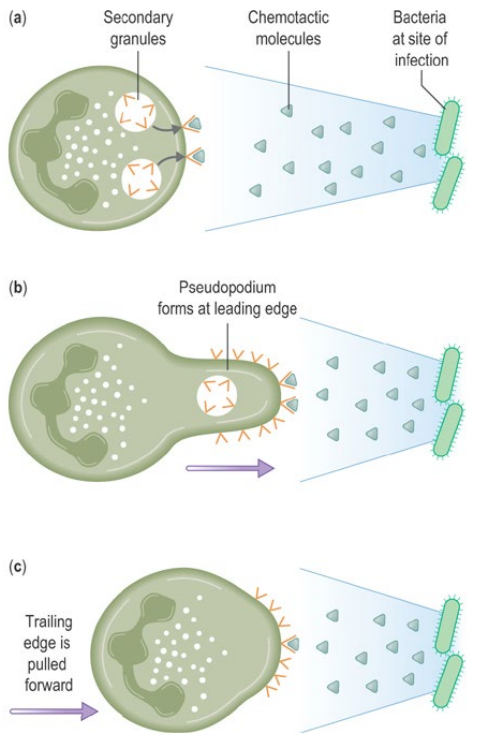
What guides neutrophils toward pathogens during chemotaxis?
Neutrophils follow __________ __________ within tissues to reach pathogens
Potent chemotactic factors include complement ______ , chemokine ______ (IL-8), bacterial -______ peptides & leukotriene ______
Chemotactic factors bind receptors on one cell edge → ____________ formation → forward movement
Neutrophils follow chemotactic gradients within tissues to reach pathogens
Potent chemotactic factors include complement C5a, chemokine CXCL8 (IL-8), bacterial N-formylated peptides & leukotriene LTB4
Chemotactic factors bind receptors on one cell edge → pseudopodium formation → forward movement
How do neutrophils use opsonisation & phagocytosis to kill organisms?
Neutrophil phagocytosis requires ________ to ↑ efficiency; key examples include _____, _-_______ ________ & ________. Binding of these to neutrophil receptors triggers ________ formation ∴ engulfment into a ________; organisms are killed via oxygen-dependent & oxygen-independent pathways.
Neutrophil phagocytosis requires opsonins to ↑ efficiency; key examples include C3b, C-reactive protein & antibody. Binding of these to neutrophil receptors triggers pseudopodia formation ∴ engulfment into a phagosome; organisms are killed via oxygen-dependent & oxygen-independent pathways.
What are the key features of oxygen-independent neutrophil killing?
Oxygen-independent killing involves release of ________ from granules into the phagosome, including ________, ________ & ________ ________ ________; components may act ________ & this mechanism is important in ________ ________ such as deep abscesses.
Oxygen-independent killing involves release of toxic compounds from granules into the phagosome, including lysozyme, lactoferrin & antimicrobial cationic proteins; components may act synergistically & this mechanism is important in anaerobic conditions such as deep abscesses.
What are the key features of oxygen-dependent neutrophil killing?
nvolves generation of radicals & toxic species via the respiratory burst & the H₂O₂–myeloperoxidase–halide system.
NADPH oxidase reduces O₂ → superoxide → H₂O₂.
Myeloperoxidase uses H₂O₂ + Cl⁻ to form highly toxic hypochlorous ions.
H₂O₂ & HOCl both = potent bactericidal agents.
Neutrophils protect themselves using antioxidant/scavenger molecules (vitamins C & E)
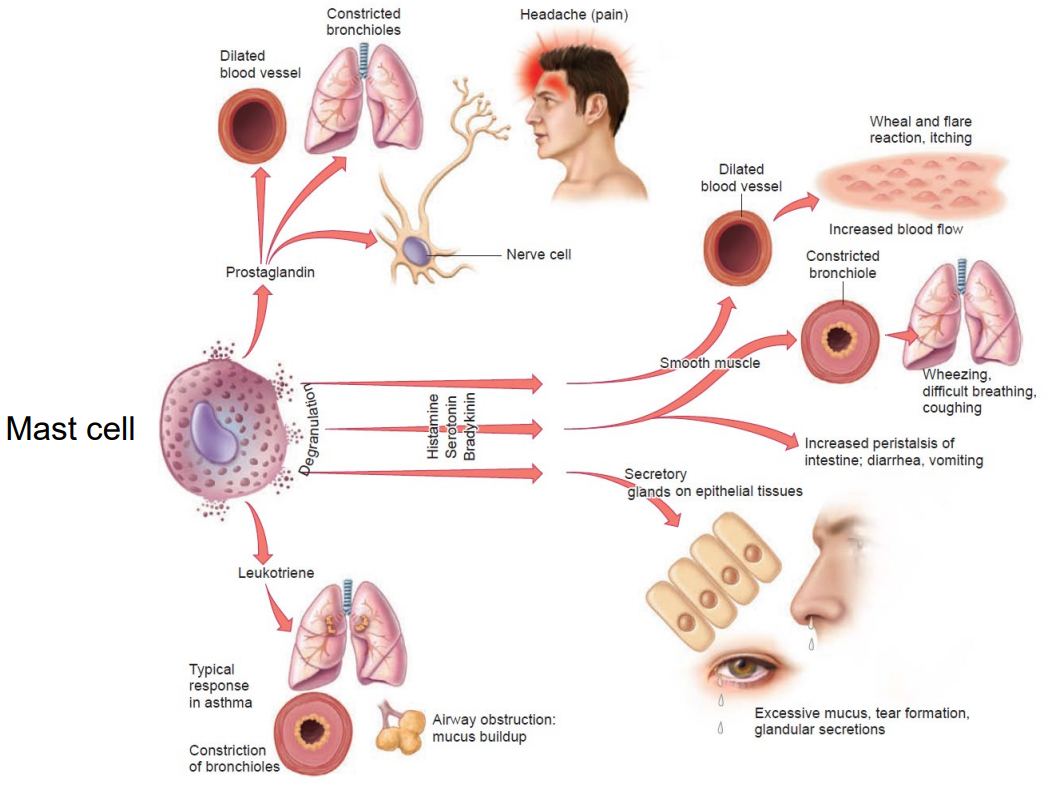
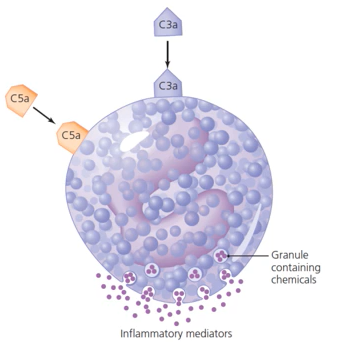
What are the key roles & activation features of mast cells & basophils?
Mast cells are prominent in the ________, around ________ ________ & in the ________; basophils are similar but found in the ________. Both contribute to acute inflammation & contain granules with ________ & ________ that ↑ vascular permeability. They express high-affinity receptors for ________; degranulation is triggered by damage, IgE or complement (C3a/C5a), leading to reactions from ________ & ________ to anaphylactic shock.
Mast cells are prominent in the skin, around blood vessels & in the gut; basophils are similar but found in the blood. Both contribute to acute inflammation & contain granules with histamine & leukotrienes that ↑ vascular permeability. They express high-affinity receptors for IgE; degranulation is triggered by damage, IgE or complement (C3a/C5a), leading to reactions from wheal & flare to anaphylactic shock.
What symptoms arise from mast-cell mediator release & which mediators cause each effect?