General Pathology and Microbiology
1/188
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
189 Terms
What is one of the most important triggers of vasodilation?
a. Release of endothelin
b. Activation of angiotensin II
c. Production of prostaglandins
d. Increased sympathetic stimulation
Production of prostaglandins
What prostaglandings are in charge for vasodilation?
a. PGD, PGE, PGF
b. PGE, PGI, PGD
c. PGI, PGF, PGE
d. PGF, PGI, PGD
b. PGE, PGI, PGD
PGD, PGI, PGE
vasoDIElation
Vasoconstriction - PGF, TXA (Thromboxane)
What is the predominant response when there’s inflammation?
a. Rubor, Calor, Tumor
b. Rubor, Calor, Tumor, Dolor
c. Rubor, Calor, Tumor, Dolor, Functio laesa
d. Rubor, Calor
a. Rubor, Calor, Tumor
What is the predominant WBC in acute inflammation?
a. Eosinophil
d. Monocyte
c. Neutrophil
d. Histocyte
c. Neutrophil or Polymorphonuclear leukocytes (PMNs)
The following are the patterns of acute inflammation EXCEPT:
a. Serous
b. Fibrinous
c. Granulomatous
d. Ulcerative
c. Granulomatous
Granulomatous is a pattern of chronic inflammation.
Patterns of acute inflammation are the following:
Serous
Fibrinous
Suppurative
Ulcerative
What phase of wound healing is seen on 7th-12th days?
a. Inflammatory
b. Proliferative
c. Maturation
b. Proliferative
Phases of wound healing (takes 18-21 days)
Inflammatory: ~7 days
Proliferative: ~7-12 days
Maturation
The following are mediators of inflammation that produces pain, EXCEPT:
a. Prostaglandin
b. Bradykinin
c. Histamine
d. Kallidin
c. Histamine
Mediators of inflammation:
Prostaglandin, Bradykinin, and Kallidin - produces pain
Histamine - most important mediator of inflammation
produced primarily by Mast cells
Lymphocytes
WBC enzymes
Note: they cause vasodilation and increase vascular permeability
Most important mediator of inflammation
a. Prostaglandin
b. Bradykinin
c. Histamine
d. Lymphocytes
c. Histamine
Which of the following best distinguishes an exudate from a transudate?
a. Exudate has low protein content; transudate has high protein content.
b. Exudate results from increased hydrostatic pressure; transudate results from inflammation.
c. Exudate is associated with inflammation and has high protein; transudate is non-inflammatory and has low protein.
d. Exudate is always clear; transudate is always cloudy.
c. Exudate is associated with inflammation and has high protein; transudate is non-inflammatory and has low protein.
Which of the following best describes the process of diapedesis?
a. Engulfing and digesting bacteria
b. Release of chemical mediators from mast cells
c. Movement of white blood cells through the blood vessel wall into tissues
d. Clumping of platelets to form a blood clot
c. Movement of white blood cells through the blood vessel wall into tissues
What structure do white blood cells extend to move through the endothelial gaps during diapedesis?
a. Flagella
b. Cilia
c. Pseudopods
d. Microvilli
c) Pseudopods
Pseudopods (or “false feet”) are temporary, actin-driven cell membrane projections that allow the WBC to crawl between endothelial cells.
This is essential for transmigration into tissues during inflammation.
Phagocytes are 1st line of defense of the innate immunity.
a. True
b. False
b. False
Non-specific/Passive/Innate Immunity
Barriers- 1st line of defense (skin, HCl in stomach, etc.)
Phagocytes - 2nd line of defense
If a healthcare worker is accidentally punctured by a needle contaminated with HIV-positive blood, what is the approximate average risk of acquiring HIV from this single exposure?
a. 0.03%
b. 0.3%
c. 3%
d. 30%
b. 0.3%
Which of the following best describes the process of opsonization?
a) Movement of white blood cells through blood vessel walls
b) Coating of pathogens to enhance phagocytosis
c) Formation of a blood clot to stop bleeding
d) Activation of complement to produce antibodies
b) Coating of pathogens to enhance phagocytosis
Which of the following is a major function of the complement system?
a) Production of antibodies by plasma cells
b) Direct killing of pathogens by cytotoxic T cells
c) Enhancing phagocytosis, inflammation, and cell lysis
d) Preventing blood clotting
c) Enhancing phagocytosis, inflammation, and cell lysis
How do plasma cells contribute to the activation of the complement system?
a) They release cytokines that directly form the membrane attack complex (MAC).
b) They produce antibodies that bind to antigens and activate the classical complement pathway.
c) They engulf pathogens coated with complement proteins.
d) They produce complement proteins directly.
b) They produce antibodies that bind to antigens and activate the classical complement pathway.
All of the following cells are associated with chronic inflammation except one. Which one is the exception?
a. Macrophages
b. Neutrophils
c. T lymphocytes
d. B lymphocytes
e. Plasma cells
b. Neutrophils
Impetigo caused by Staphylococcus aureus is most commonly characterized by:
a) Deep necrotic ulcers
b) Painless vesicles on the palms and soles
c) Honey-colored crusted lesions
d) Bullous lesions on mucous membranes
c) Honey-colored crusted lesions
Impetigo/Pyoderma

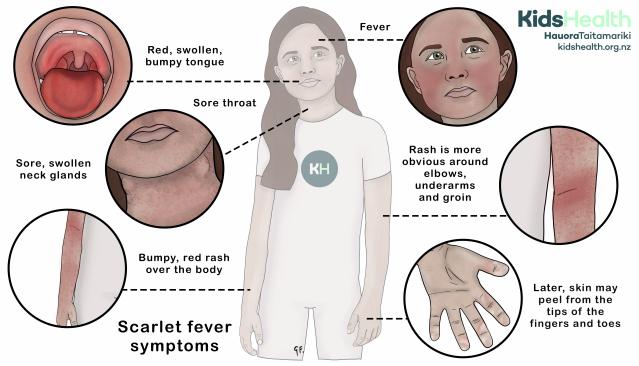
Which of the following is NOT a common manifestation of Staphylococcus aureus infection?
a) Folliculitis
b) Carbuncles
c) Scarlet fever
d) Osteomyelitis
c) Scarlet fever (this is associated with Streptococcus pyogenes)
What is the primary laboratory test used to differentiate Staphylococcus aureus from other staphylococcal species?
a) Catalase test
b) Coagulase test
c) Hemolysis on blood agar
d) Novobiocin sensitivity test
b) Coagulase test
Which of the following is the most common cause of infective endocarditis in general?
a) Staphylococcus aureus
b) Staphylococcus epidermidis
c) Streptococcus viridans group
d) Enterococcus faecalis
c) Streptococcus viridans group
Infective Endocarditis
Acute - more severe
Common cause: Staph. aureus
Subacute - more common, ~less acute
common cause: Strep. viridans
Which type of horizontal gene transfer is most susceptible to damage in the external environment?
a) Conjugation
b) Transduction
c) Transformation
d) Transposition
c) Transformation
At what age is the risk for dental staining from tetracycline greatest?
a) Before birth and up to 8 years old
b) Only during adolescence (12–18 years old)
c) After age 18
d) After permanent teeth have fully erupted
a) Before birth and up to 8 years old
Tetracycline stains has effect until 8 years old only.
Fluorosis too
Which of the following is an example of a Type II hypersensitivity reaction?
a) Anaphylactic shock
b) Hemolytic anemia due to mismatched blood transfusion
c) Serum sickness
d) Contact dermatitis from poison ivy
b) Hemolytic anemia due to mismatched blood transfusion
Hemolytic anemia aka Erythroblastosis fetalis
Which disease is an example of a Type III hypersensitivity reaction?
a) Asthma
b) Graves’ disease
c) Systemic lupus erythematosus (SLE)
d) Allergic rhinitis
c) Systemic lupus erythematosus (SLE)
Which cells primarily mediate Type IV hypersensitivity reactions?
a) IgE antibodies
b) Complement proteins
c) Cytotoxic T lymphocytes and macrophages
d) Mast cells
c) Cytotoxic T lymphocytes and macrophages
Which of the following is an example of a delayed-type hypersensitivity?
a) Asthma attack
b) Contact dermatitis due to nickel jewelry
c) Hemolytic disease of the newborn
d) Pernicious anemia
b) Contact dermatitis due to nickel jewelry
Which hypersensitivity type is responsible for acute transplant rejection?
a) Type I
b) Type II
c) Type III
d) Type IV
d) Type IV
Which of the following best describes hydropic (cloudy) swelling?
a) Accumulation of fat within cells
b) Increase in cell size due to protein synthesis
c) Accumulation of water within the cytoplasm due to failure of ion pumps
d) Deposition of abnormal proteins in extracellular spaces
c) Accumulation of water within the cytoplasm due to failure of ion pumps
Fatty change (steatosis) is most commonly seen in which organ?
a) Brain
b) Heart
c) Liver
d) Pancreas
c) Liver
Usually in alcoholics; can also happen to too much intake of drugs for tubeculosis
Which intracellular pigment indicates wear-and-tear degeneration due to free radical injury?
a) Bilirubin
b) Melanin
c) Lipofuscin
d) Hemosiderin
c) Lipofuscin
Usually comes with aging
Which of the following describes the hyaline accumulation in the glomerulus that leads to sclerosis and is commonly associated with diabetes mellitus?
a) Amyloidosis
b) Fibrinoid necrosis
c) Hyaline arteriolosclerosis
d) Kimmelstiel-Wilson nodules
d) Kimmelstiel-Wilson nodules
aka Diabetic glomerulosclerosis
Diabetic glomerulosclerosis, also known as Kimmelstiel-Wilson disease, is a kidney disease caused by diabetes that leads to the thickening and scarring of the glomeruli(the kidney's filtering units). This scarring, or sclerosis, is characterized by hyaline deposits and the formation of nodules within the glomeruli. It's a progressive complication of diabetes, potentially leading to chronic kidney disease and end-stage renal failure.
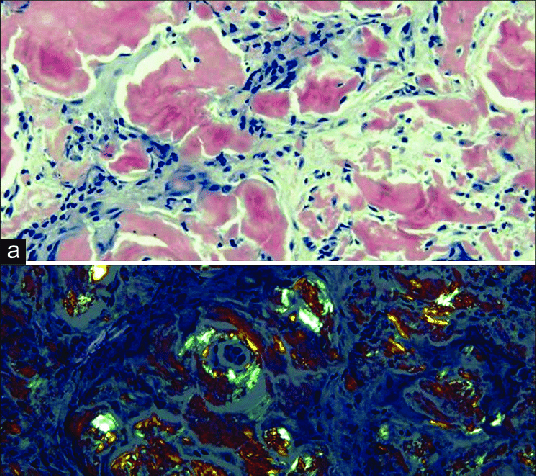
Which condition is characterized by extracellular hyaline-like material that shows apple-green birefringence on Congo red staining?
a) Fibrinoid necrosis
b) Lipofuscin accumulation
c) Kimmelstiel-Wilson nodules
d) Amyloidosis
d) Amyloidosis
Which pigment can accumulate due to massive destruction of red blood cells (hemolytic anemia)?
a) Bilirubin
b) Lipofuscin
c) Melanin
d) Anthracotic pigment
a) Bilirubin
Which of the following Streptococcus species is beta-hemolytic and sensitive to bacitracin?
a) Streptococcus pneumoniae
b) Streptococcus pyogenes
c) Streptococcus agalactiae
d) Streptococcus viridans
b) Streptococcus pyogenes
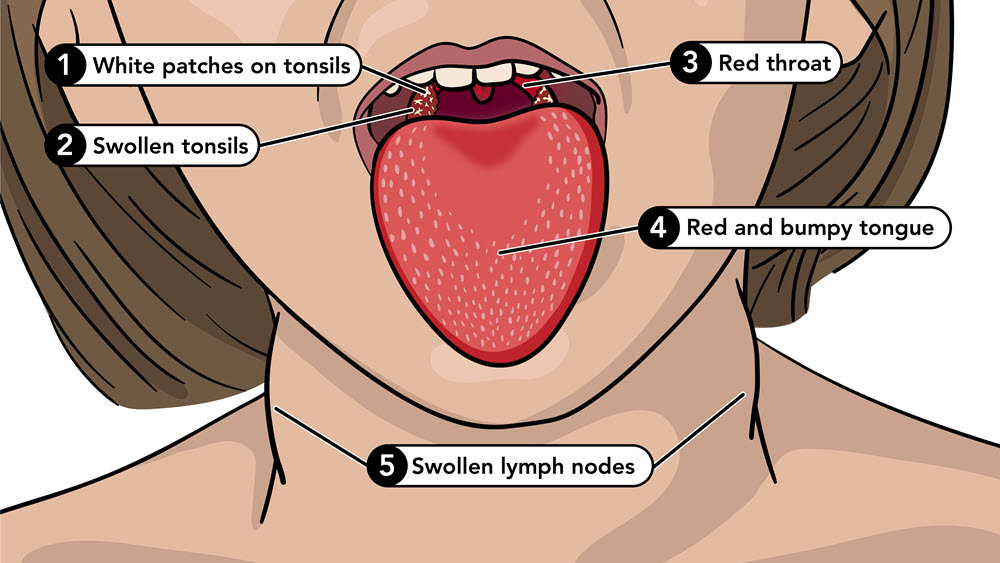
Which is the primary cause of strep throat (pharyngitis)?
a) Streptococcus pneumoniae
b) Streptococcus mutans
c) Streptococcus pyogenes
d) Streptococcus agalactiae
c) Streptococcus pyogenes
Which virulence factor allows Streptococcus pyogenes to resist phagocytosis?
a) M protein
b) Streptolysin O
c) Hyaluronidase
d) Streptokinase
a) M protein
The M protein is a surface-expressed protein that extends outward from the cell wall like hair-like projections.
It inhibits phagocytosis by preventing complement activation and opsonization (the process by which pathogens are marked for ingestion and destruction by phagocytes).
It does this by binding factor H, which inactivates complement component C3b.
It also helps the bacteria adhere to host tissues.
Which of the following is the major cause of dental caries?
a) Streptococcus pyogenes
b) Streptococcus pneumoniae
c) Streptococcus agalactiae
d) Streptococcus mutans
d) Streptococcus mutans
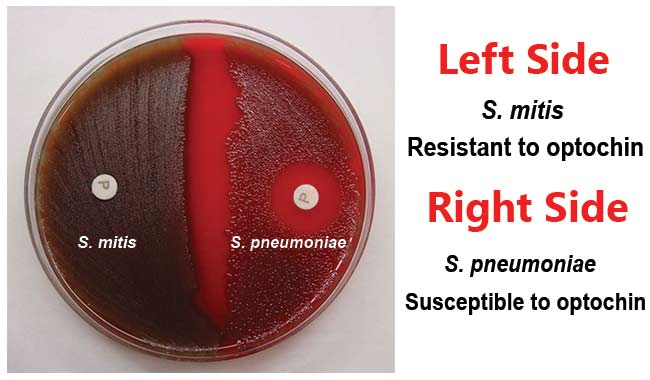
Which Streptococcus species is alpha-hemolytic and optochin sensitive?
a) Streptococcus mutans
b) Streptococcus viridans
c) Streptococcus pneumoniae
d) Streptococcus pyogenes
c) Streptococcus pneumoniae
Optochin is a chemical compound used in microbiology to differentiate Streptococcus pneumoniae from other alpha-hemolytic streptococci.
Which condition is a possible immune-mediated sequela of Streptococcus pyogenes pharyngitis?
a) Scarlet fever
b) Rheumatic fever
c) Pneumonia
d) Impetigo
a) Scarlet fever
Which of the following is the most common cardiac valve affected by rheumatic fever?
a) Aortic valve
b) Pulmonary valve
c) Mitral valve
d) Tricuspid valve
c) Mitral valve
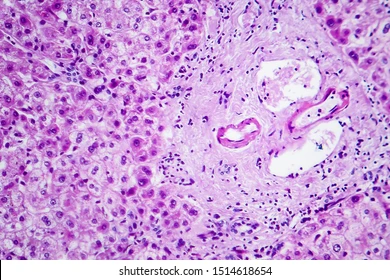
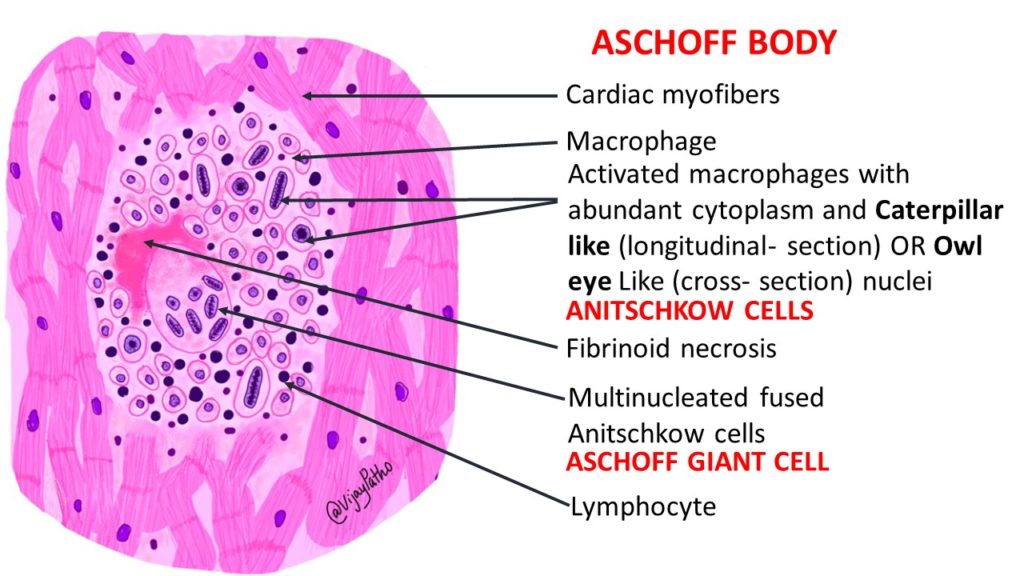
What is the hallmark histological finding in rheumatic carditis?
a) Aschoff bodies
b) Reed-Sternberg cells
c) Councilman bodies
d) Negri bodies
a) Aschoff bodies
(Granulomatous lesions with Anitschkow cells)
Aschoff bodies are granulomatous lesions, specifically nodules, found in the heart tissue of individuals with rheumatic fever.
Which sign in rheumatic fever presents as painless, serpiginous skin rash?
a) Erythema marginatum
b) Erythema multiforme
c) Erythema nodosum
d) Scarlatiniform rash
a) Erythema marginatum
Pink torso rings

Which Jones criterion represents involuntary, purposeless movements, especially in children?
a) Erythema marginatum
b) Subcutaneous nodules
c) Sydenham chorea
d) Polyarthritis
c) Sydenham chorea
The term "chorea" itself comes from the Greek word "choreia," meaning dance, reflecting the jerky, dance-like movements characteristic of the disorder.

Which disease is caused by Corynebacterium diphtheriae?
a) Whooping cough
b) Scarlet fever
c) Diphtheria
d) Typhoid fever
c) Diphtheria
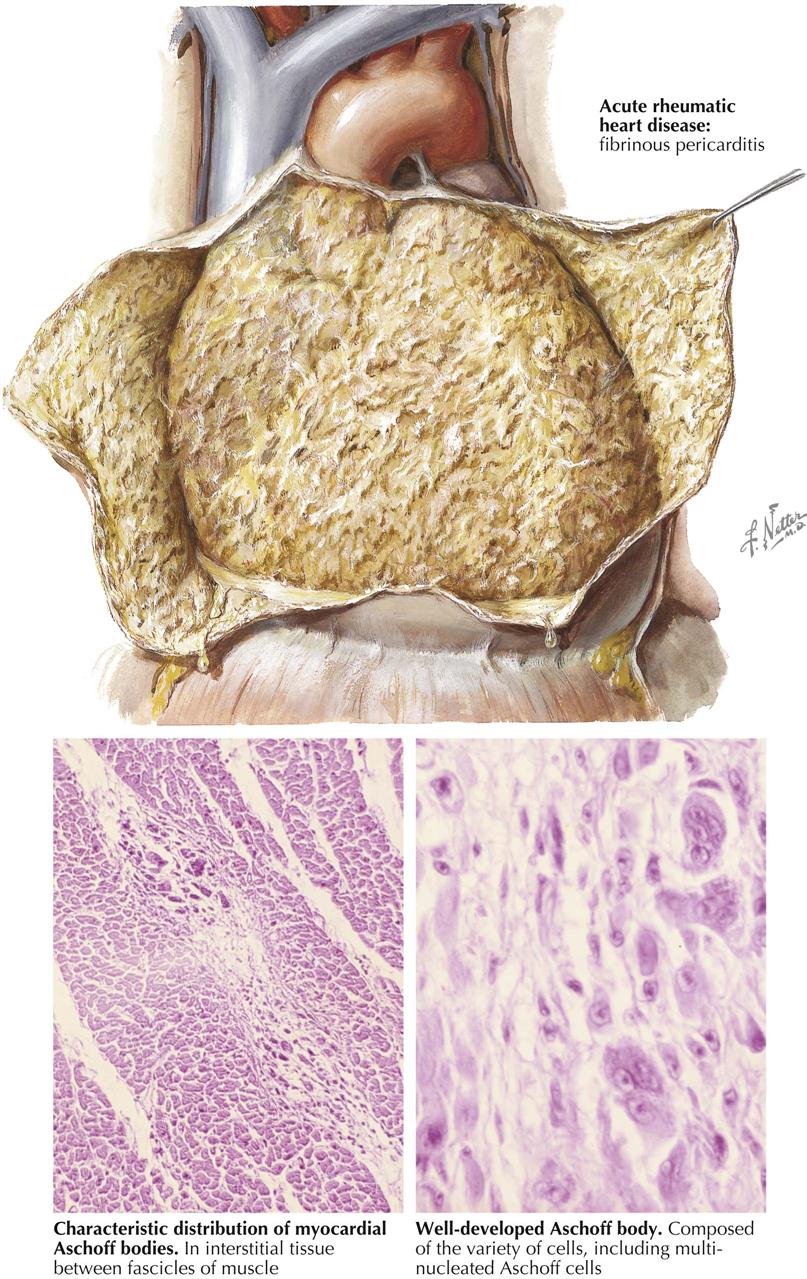
Which type of pericarditis is classically associated with rheumatic fever?
a) Suppurative (purulent) pericarditis
b) Fibrinous pericarditis
c) Hemorrhagic pericarditis
d) Serous pericarditis
b) Fibrinous pericarditis
Fibrinous pericarditis is an inflammation of the pericardium, the sac surrounding the heart, characterized by the presence of fibrin, a protein involved in blood clotting, on the pericardial surface. This results in a roughened, granular appearance of the pericardium, often described as having a "bread and butter" texture.
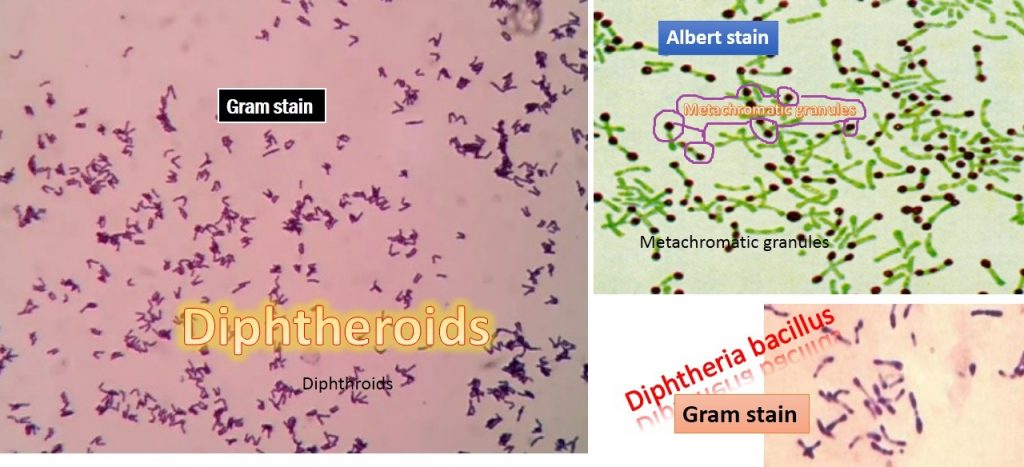
What is the classic microscopic appearance of Corynebacterium diphtheriae on staining?
a) Gram-negative rods in chains
b) Gram-positive cocci in clusters
c) Club-shaped Gram-positive rods with metachromatic granules
d) Gram-negative diplococci
c) Club-shaped Gram-positive rods with red metachromatic granules
Looks like chinese characters in Hx
Which of the following diseases is prevented by the DPT vaccine?
a) Diphtheria, pertussis, and polio
b) Diphtheria, pertussis, and tetanus
c) Diphtheria, plague, and tuberculosis
d) Dengue, pertussis, and tetanus
b) Diphtheria, pertussis, and tetanus
Which of the following clinical signs is described as severe hyperextension and spasticity of the body, causing an arching of the back and neck, and is commonly seen in tetanus?
a) Nuchal rigidity
b) Opisthotonos
c) Chorea
d) Ataxia
b) Opisthotonos
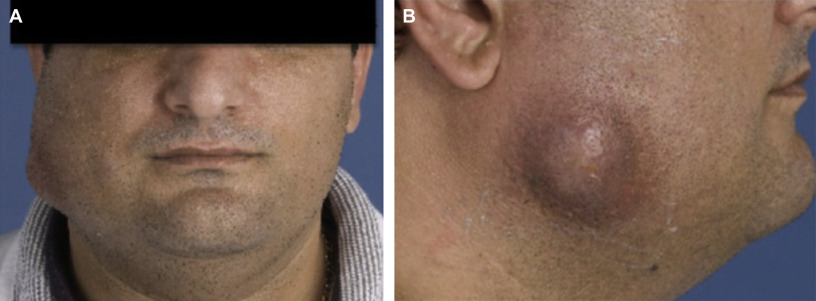
Which clinical condition is most commonly caused by Actinomyces israelii?
a) Gas gangrene
b) Cervicofacial abscess (lumpy jaw)
c) Necrotizing fasciitis
d) Pulmonary tuberculosis
b) Cervicofacial abscess (lumpy jaw)
Which of the following organisms is most commonly associated with root surface caries, especially in patients with gingival recession?
a) Streptococcus mutans
b) Streptococcus sanguinis
c) Actinomyces viscosus
d) Lactobacillus acidophilus
c) Actinomyces viscosus
Lactobacillus species are most strongly associated with which stage of dental caries?
a) Initiation of caries in smooth enamel surfaces
b) Progression of deep carious lesions in dentin
c) Root surface caries
d) Periodontal pocket formation
b) Progression of deep carious lesions in dentin
Where are Lactobacillus species commonly found as part of the normal flora?
a) Skin and hair follicles
b) Nasal cavity
c) Gastrointestinal tract and female genital tract
d) Bloodstream
c) Gastrointestinal tract and female genital tract
They help maintain an acidic environment in the vagina and inhibit pathogens.
Which factor allows Lactobacillus species to contribute to caries progression?
a) High protease production
b) High acid production and acid tolerance (aciduric)
c) Toxin production
d) Capsule formation
b) High acid production and acid tolerance (aciduric)
They produce lactic acid, which contributes mainly to the progression of deep carious lesions
Which bacteria is primarily responsible for initiation of caries, while Lactobacillus contributes more to progression?
a) Streptococcus mutans
b) Actinomyces israelii
c) Clostridium perfringens
d) Staphylococcus aureus
a) Streptococcus mutans
Which of the following statements about Nocardia asteroides is CORRECT?
a) It is an anaerobic, non–acid-fast organism that causes cervicofacial abscesses
b) It is a branching, filamentous, weakly acid-fast bacterium associated with pulmonary infections in immunocompromised patients
c) It is a fungus that produces sulfur granules in the oral cavity
d) It is a strict anaerobe found in the human mouth
b) It is a branching, filamentous, weakly acid-fast bacterium associated with pulmonary infections in immunocompromised patients
Which of the following best describes listeriosis?
a) Gastroenteritis only seen in neonates
b) Foodborne illness that can cause mild diarrhea in healthy people but serious invasive disease in pregnant women, newborns, and immunocompromised patients
c) Strictly a respiratory tract infection
d) Always toxin-mediated with no cellular invasion
b) Foodborne illness that can cause mild diarrhea in healthy people but serious invasive disease in pregnant women, newborns, and immunocompromised patients
Unpasteurized milk, soft cheeses, deli meats, refrigerated ready-to-eat foods → Listeria can grow at refrigerator temperatures!
Which of the following genera includes Gram-positive, spore-forming rods?
a) Staphylococcus and Streptococcus
b) Corynebacterium and Listeria
c) Bacillus and Clostridium
d) Nocardia and Actinomyces
c) Bacillus and Clostridium
Which of the following statements about bacterial spores is CORRECT?
a) Spores are metabolically active forms that grow rapidly under stress
b) Spore formation allows bacteria to survive extreme heat, drying, and disinfectants
c) Spores are seen only in Gram-negative rods
d) Spores are responsible for toxin production
b) Spore formation allows bacteria to survive extreme heat, drying, and disinfectants
Which Gram-positive spore-forming bacterium is aerobic and causes anthrax?
a) Clostridium perfringens
b) Bacillus anthracis
c) Bacillus cereus
d) Clostridium difficile
b) Bacillus anthracis
Features of anthrax:
Central black eschar
Hemorrhagic necrosis and edema of mediastinum
Hemorrhagic pleural effusion
Sepsis
Meningitis

Which of the following standard autoclave settings is recommended to effectively kill bacterial endospores?
a) 100°C for 10 minutes at normal pressure
b) 121°C at 15 psi for 15–30 minutes
c) 60°C for 1 hour at normal pressure
d) 80°C for 20 minutes at normal pressure
b) 121°C at 15 psi for 15–30 minutes

Which spore-forming bacterium is most commonly associated with gas gangrene?
a) Clostridium tetani
b) Clostridium difficile
c) Bacillus subtilis
d) Clostridium perfringens
d) Clostridium perfringens
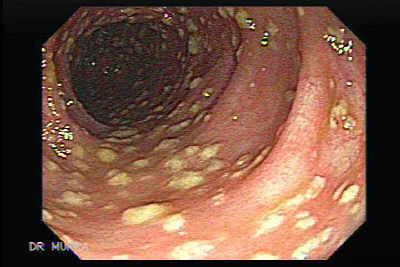
Which spore-forming bacterium causes pseudomembranous colitis following antibiotic use?
a) Clostridium botulinum
b) Clostridium perfringens
c) Clostridium difficile
d) Bacillus anthracis
c) Clostridium difficile
Pseudomembranous colitis is an inflammation of the colon, often caused by an overgrowth of the bacterium Clostridioides difficile (formerly Clostridium difficile), commonly known as C. diff. This overgrowth typically occurs after antibiotic use or a recent hospital stay, and can lead to symptoms like diarrhea, abdominal pain, and fever.
What distinguishes Bacillus species from Clostridium species?
a) Bacillus are anaerobic; Clostridium are aerobic
b) Bacillus are Gram-negative rods; Clostridium are Gram-positive rods
c) Bacillus are aerobic or facultative; Clostridium are strict anaerobes
d) Bacillus are cocci; Clostridium are rods
c) Bacillus are aerobic or facultative; Clostridium are strict anaerobes
Which spore-forming bacterium produces a toxin that blocks release of inhibitory neurotransmitters?
a) Bacillus anthracis
b) Clostridium tetani
c) Bacillus cereus
d) Clostridium perfringens
b) Clostridium tetani
Causes Tetanus (lockjaw)
Muscle spasm due to excitation of neurons due to tetanus toxin
Which of the following statements correctly describes the mechanism of botulinum toxin released by Clostridium botulinum?
a) It blocks the release of GABA in the spinal cord
b) It blocks the release of acetylcholine at neuromuscular junctions
c) It stimulates excessive acetylcholine release
d) It increases acetylcholinesterase activity
b) It blocks the release of acetylcholine at neuromuscular junctions
Causes Botulism
Results to muscle paralysis or muscle relaxation due to botulinum toxin (botox)
Among the following, which is not associated with meningitis:
a. Escherichia coli
b. Haemophilus influenza
c. Streptococcus pneumonia
d. Treponema pallidum
d. Treponema pallidum
E. coli - neonates (0-30 days)
Haemophilus influenza- infants and children
Neisseria meningitidis - young adults
Streptococcus pneumonia - old adults
Which of the following is the main mode of transmission for Neisseria meningitidis?
a) Sexual contact
b) Contaminated food
c) Respiratory droplets
d) Fecal–oral route
c) Respiratory droplets
A college student presents with sudden fever, headache, and a petechial rash. Which pathogen is most likely?
a) Neisseria gonorrhoeae
b) Neisseria meningitidis
c) Streptococcus pneumoniae
d) Escherichia coli
b) Neisseria meningitidis
Which of the following diseases can not be caused by Escherichia coli?
a) Traveler’s diarrhea
b) Urinary tract infection (UTI)
c) Whooping cough
d) Neonatal meningitis
c) Whooping cough
Which of the following statements about Neisseria gonorrhoeae infection (gonorrhea) is TRUE?
a) It is caused by a Gram-positive diplococcus with a capsule.
b) It commonly causes urethritis in men and can lead to pelvic inflammatory disease (PID) in women.
c) It is mainly transmitted by respiratory droplets.
d) It produces a potent exotoxin that causes spastic paralysis.
b) It commonly causes urethritis in men and can lead to pelvic inflammatory disease (PID) in women.
Gonorrhea - venereal disease (STD); tulo
Which disease is caused by Treponema pallidum?
a) Gonorrhea
b) Syphilis
c) Chlamydia
d) Trichomoniasis
b) Syphilis
What is the most common mode of transmission of Treponema pallidum?
a) Fecal–oral route
b) Respiratory droplets
c) Sexual contact and vertical transmission
d) Contaminated food
c) Sexual contact and vertical transmission
(It can cross the placenta → congenital syphilis)
Which of the following is a characteristic feature of primary syphilis?
a) Painless genital ulcer (chancre)
b) Maculopapular rash on palms and soles
c) Gummas and neurosyphilis
d) Severe watery diarrhea
a) Painless genital ulcer (chancre)
A patient with syphilis develops a non-itchy rash on the palms and soles. Which stage is this?
a) Primary syphilis
b) Secondary syphilis
c) Latent syphilis
d) Tertiary syphilis
b) Secondary syphilis
Stage | Main signs/symptoms |
|---|---|
Primary | Painless chancre, non-tender lymph nodes |
Secondary | Rash (palms/soles), condylomata lata, mucous patches, lymphadenopathy |
Latent | No symptoms; Early phase - contagious ; Late phase - non-contagious |
Tertiary | Gummatous necrosis, cardiovascular syphilis, neurosyphilis |
A newborn has interstitial keratitis, Hutchinson’s incisors, and deafness. Which condition is this?
a) Primary syphilis
b) Secondary syphilis
c) Congenital syphilis
d) Tertiary syphilis
c) Congenital syphilis

Treponema denticola is strongly associated with which dental condition?
a) Dental caries
b) Acute necrotizing ulcerative gingivitis (ANUG) and chronic periodontitis
c) Herpes labialis
d) Apical cyst formation
b) Acute necrotizing ulcerative gingivitis (ANUG) and chronic periodontitis
Periodontitis
Vincent’s disease (Trench mouth/Necrotizing Ulcerative Gingivitis)
Presence of painful punched-out grayish pseduomembrance in the gingiva; fetid odor
Treatment:
Debridement - removal of damage tissue
Irrigation
Antibiotics (penicillins)

What is the primary source of Leptospira infection in humans?
a) Respiratory droplets from infected people
b) Contaminated food
c) Contact with water or soil contaminated with urine of infected animals (e.g., rodents, dogs)
d) Sexual transmission
c) Contact with water or soil contaminated with urine of infected animals
Penetration through broken skin or mucous membranes
Which organs are commonly affected in severe leptospirosis (Weil’s disease)?
a) Brain and spinal cord
b) Lungs and pancreas
c) Liver and kidneys
d) Skin and eyes only
c) Liver and kidneys
Can cause jaundice, renal failure, hemorrhage.
Which of the following is a classic sign of severe leptospirosis?
a) Painless chancre
b) Bull’s-eye rash
c) Jaundice and renal dysfunction
d) Pseudomembrane in the throat
c) Jaundice and renal dysfunction
A hospitalized patient develops pneumonia. Culture grows a non-lactose fermenting Gram-negative rod with fruity odor. What is the most likely organism?
A. Klebsiella pneumoniae
B. Escherichia coli
C. Pseudomonas aeruginosa
D. Haemophilus influenzae
C. Pseudomonas aeruginosa
Pseudomonas is non-lactose fermenting, emits a grape-like or fruity odor, and is common in hospital-acquired pneumonia, especially in ventilated patients. Klebsiella and E. coli ferment lactose, and H. influenzae is a coccobacillus.
Which of the following correctly matches the pathogen to the most commonly associated nosocomial infection?
A. Pseudomonas aeruginosa – Catheter-associated urinary tract infection
B. Staphylococcus aureus – Ventilator-associated pneumonia
C. Escherichia coli – Surgical site infection
D. Pseudomonas aeruginosa – Surgical site infection
B. Staphylococcus aureus – Ventilator-associated pneumonia
Staphylococcus aureus is a leading cause of nosocomial pneumonia, especially in ventilator-associated cases, as well as surgical site infections.
Pseudomonas aeruginosa is more associated with ventilator-associated pneumonia, burn wound infections, and nosocomial bloodstream infections, but less with surgical sites directly.
Escherichia coli is the most common cause of catheter-associated urinary tract infections (CAUTIs), not surgical site infections.
While Pseudomonas can infect surgical sites, it's not the most common cause — S. aureus is.
Prevotella and Porphyromonas are most commonly associated with which of the following clinical conditions?
A. Gastroenteritis
B. Periodontal disease
C. Urinary tract infection
D. Meningitis
B. Periodontal disease
These pigmented anaerobes are part of the oral microbiota and are involved in chronic periodontitis, gingivitis, and other oral cavity infections. They can also be involved in aspiration pneumonia and peritonsillar abscesses.
Which of the following best explains how Bacteroides species such as Prevotella and Porphyromonas contribute to alveolar bone resorption in periodontal disease?
A. By producing exotoxin A that inhibits protein synthesis
B. By hydrolyzing hemoglobin to release iron for their metabolism
C. By secreting collagenases that degrade periodontal connective tissue
D. By forming spores that destroy bone matrix
C. By secreting collagenases that degrade periodontal connective tissue
Prevotella and Porphyromonas are known to produce collagen-degrading enzymes (e.g., collagenases, proteases) that break down the extracellular matrix of periodontal tissues.
This leads to connective tissue destruction and bone resorption, characteristic of chronic periodontitis.
These bacteria do not produce exotoxin A (that's Pseudomonas aeruginosa), and they are non-spore-forming.
Iron metabolism is involved in pigment formation but is not directly related to bone resorption.
Which of the following best describes Rickettsia species?
A. Gram-positive, spore-forming rods
B. Gram-negative, obligate intracellular bacteria
C. Acid-fast, facultative intracellular bacteria
D. Gram-negative cocci, extracellular
B. Gram-negative, obligate intracellular bacteria
Rickettsia are Gram-negative bacilli that must live inside host cells to survive and replicate. They infect endothelial cells, causing vascular damage and are transmitted via arthropod vectors (e.g., ticks, lice, fleas).

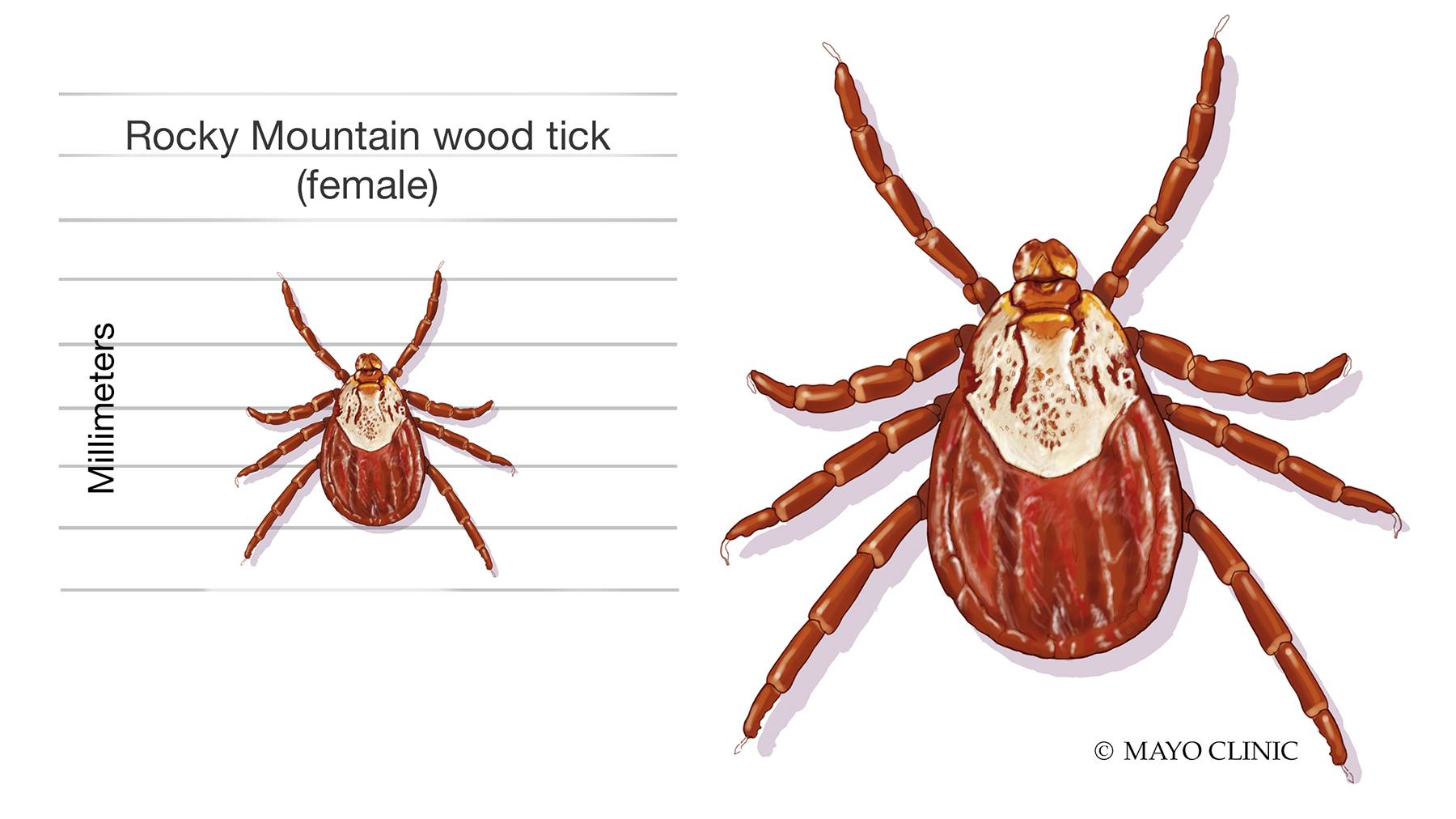
What is the most common vector for Rickettsia rickettsii, the causative agent of Rocky Mountain spotted fever?
A. Flea
B. Louse
C. Mosquito
D. Tick
D. Tick
Rickettsia rickettsii is transmitted by ticks, primarily the Dermacentor species in the U.S. It causes Rocky Mountain spotted fever (RMSF), which features fever, rash (starting on wrists/ankles), and vasculitis.

What is the primary vector for Rickettsia prowazekii, the causative agent of Louse-borne / epidemic typhus?
A. Flea
B. Tick
C. Human lice
D. Mosquito
C. Human lice
R. prowazekii is transmitted by the human lice/body louse (Pediculus humanus corporis). The louse defecates infected feces on the skin while feeding, and scratching inoculates the organism into the skin. This causes epidemic typhus, typically associated with crowded, unhygienic conditions like refugee camps and prisons.


Which of the following best describes the transmission of Rickettsia typhi, the agent of Murine / endemic typhus?
A. Flea bite from infected rodents
B. Aerosolized rodent urine
C. Tick bite
D. Direct contact with human feces
A. Flea bite from infected rodents
R. typhi causes endemic (murine) typhus, transmitted via rat fleas (Xenopsylla cheopis). It’s associated with rodent populations, particularly in urban settings, and is typically milder than epidemic typhus.
Murine = relating to or affecting mice or related rodents

Which feature helps distinguish epidemic from endemic typhus clinically or epidemiologically?
A. Epidemic typhus is transmitted by fleas
B. Endemic typhus has higher mortality
C. Epidemic typhus is associated with poor sanitation and crowding
D. Endemic typhus causes a rash starting on the wrists and ankles
C. Epidemic typhus is associated with poor sanitation and crowding
Epidemic typhus (R. prowazekii) occurs during wars, famines, and refugee crises, where body lice infestations are common. Endemic typhus (R. typhi) is more sporadic, with lower mortality, and often associated with flea-infested rodents.
Which of the following best describes Chlamydia trachomatis?
A. Gram-positive, facultative intracellular bacterium
B. Gram-negative, obligate intracellular bacterium
C. Acid-fast, extracellular bacterium
D. Spore-forming aerobic bacillus
B. Gram-negative, obligate intracellular bacterium
Chlamydia trachomatis is a Gram-negative, obligate intracellular pathogen. It cannot make its own ATP and relies on host cell energy, making it an energy parasite. It is non-spore-forming and nonmotile.
Which of the following is the most common bacterial sexually transmitted infection (STI) in the world?
A. Neisseria gonorrhoeae
B. Treponema pallidum
C. Chlamydia trachomatis
D. Haemophilus ducreyi
C. Chlamydia trachomatis
Chlamydia trachomatis is the most prevalent bacterial STI worldwide. It can cause urethritis, cervicitis, PID, and infertility. Many infections are asymptomatic, especially in women.
What distinguishes Chlamydia from Rickettsia in terms of metabolism?
A. Chlamydia lacks peptidoglycan and relies entirely on host ATP
B. Chlamydia is not an obligate intracellular organism
C. Chlamydia can generate its own ATP
D. Chlamydia grows on standard bacterial media
A. Chlamydia lacks peptidoglycan and relies entirely on host ATP
Chlamydia is an energy parasite, relying completely on host ATP. It lacks a true peptidoglycan layer, making it resistant to beta-lactam antibiotics. Unlike Rickettsia, which can make some of its own ATP (though still an obligate ntracellular bacteria), Chlamydia cannot survive outside host cells or be grown on standard media.
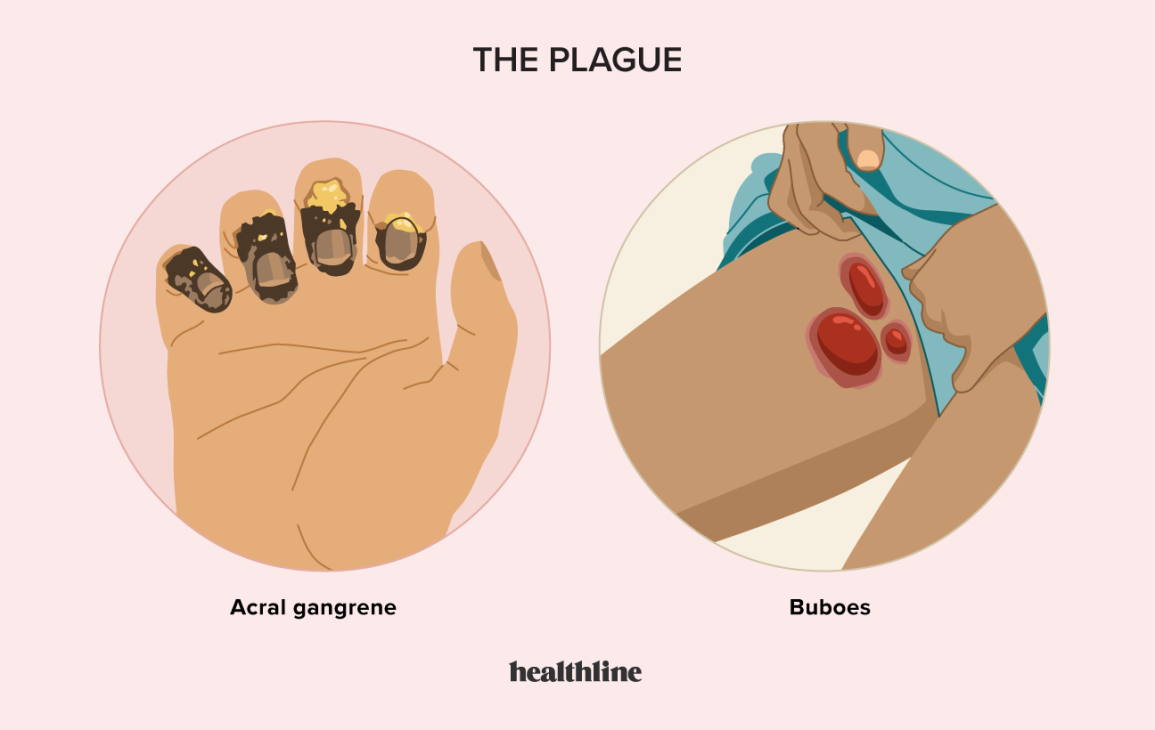
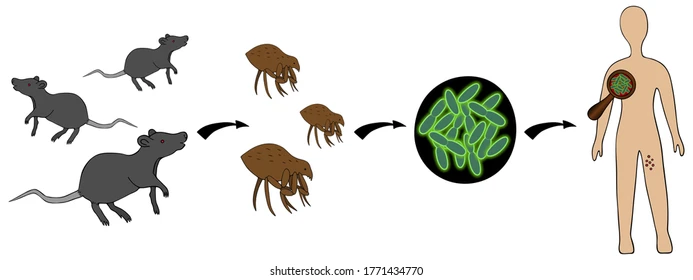
Which statement best differentiates bubonic from pneumonic plague caused by Yersinia pestis?
A. Bubonic plague spreads through respiratory droplets.
B. Pneumonic plague presents with lymphadenopathy ("buboes").
C. Bubonic plague is vector-borne, pneumonic plague is airborne.
D. Both are caused by flea-borne transmission.
C. Bubonic plague is vector-borne, pneumonic plague is airborne.
Bubonic plague is spread by flea bites and presents with painful swollen lymph nodes (buboes). Pneumonic plague is more severe and spreads via aerosolized droplets, allowing human-to-human transmission.
Which is a key distinguishing feature of Shigella dysenteriae infection?
A. Watery diarrhea without leukocytes
B. Bloody diarrhea due to enterotoxin
C. Vomiting and dehydration within 6 hours
D. Toxin-mediated hemolysis and paralysis
B. Bloody diarrhea due to enterotoxin
Shigella dysenteriae produces Shiga toxin, which damages the intestinal mucosa, leading to inflammatory, bloody diarrhea. It can also lead to hemolytic uremic syndrome (HUS) in severe cases.
Shigellosis - results to bloody diarrhea (red bloody stool = hematochezia)
DYK: black tarry stool = “melena”
Which of the following best describes the most likely routes of transmission for Salmonella typhi, the causative agent of typhoid fever?
A. Inhalation of airborne droplets from infected patients
B. Consumption of undercooked meat or contact with contaminated food or hands
C. Bite of a mosquito carrying the organism
D. Transfusion of infected blood products
B. Consumption of undercooked meat or contact with contaminated food or hands
Salmonella typhi is transmitted via the fecal-oral route.
Common sources include contaminated food or water, especially undercooked poultry, shellfish, unwashed vegetables, and food handled by chronic carriers or acutely infected individuals who don’t practice proper hygiene.
It is not transmitted by air or mosquitoes, and blood transfusion transmission is extremely rare.
Proper cooking, hand hygiene, and safe water practices are key to preventing typhoid fever.
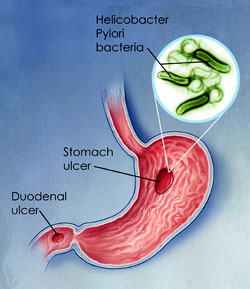
Which of the following statements about Helicobacter pylori is TRUE?
A. It is a normal part of the gastrointestinal flora
B. It causes disease only in the small intestine, not in the stomach
C. It survives in the stomach by neutralizing acid via urease
D. It is primarily transmitted through airborne droplets
C. It survives in the stomach by neutralizing acid via urease
H. pylori is not a normal part of the GI flora and is considered pathogenic.
It colonizes the stomach (mainly) and sometimes the proximal small intestine (duodenum).
It produces urease, which breaks down urea to form ammonia, allowing it to neutralize gastric acid and survive in the hostile acidic environment.
It is linked to gastritis, peptic ulcers, and even gastric cancer.
Transmission is fecal-oral, often via contaminated food, water, or hands (e.g., from carriers who don’t wash hands after defecation).
Airborne transmission is not typical.
Which of the following pathogens typically causes profuse watery diarrhea without blood or pus?
A. Shigella dysenteriae
B. Vibrio cholerae
C. Entamoeba histolytica
D. Salmonella typhi
B. Vibrio cholerae
Vibrio cholerae causes watery “rice-water” diarrhea through toxin-mediated chloride secretion. It does not invade intestinal tissue, so no blood or leukocytes are present in the stool.
Transmission occurs through ingestion of contaminated food or water, especially in areas with poor sanitation or during outbreaks.
Cholera does not cause bloody diarrhea, fever, or neurotoxicity.
Shigella and Entamoeba invade mucosa → bloody diarrhea.
Salmonella typhi → systemic typhoid fever, not classic gastroenteritis.
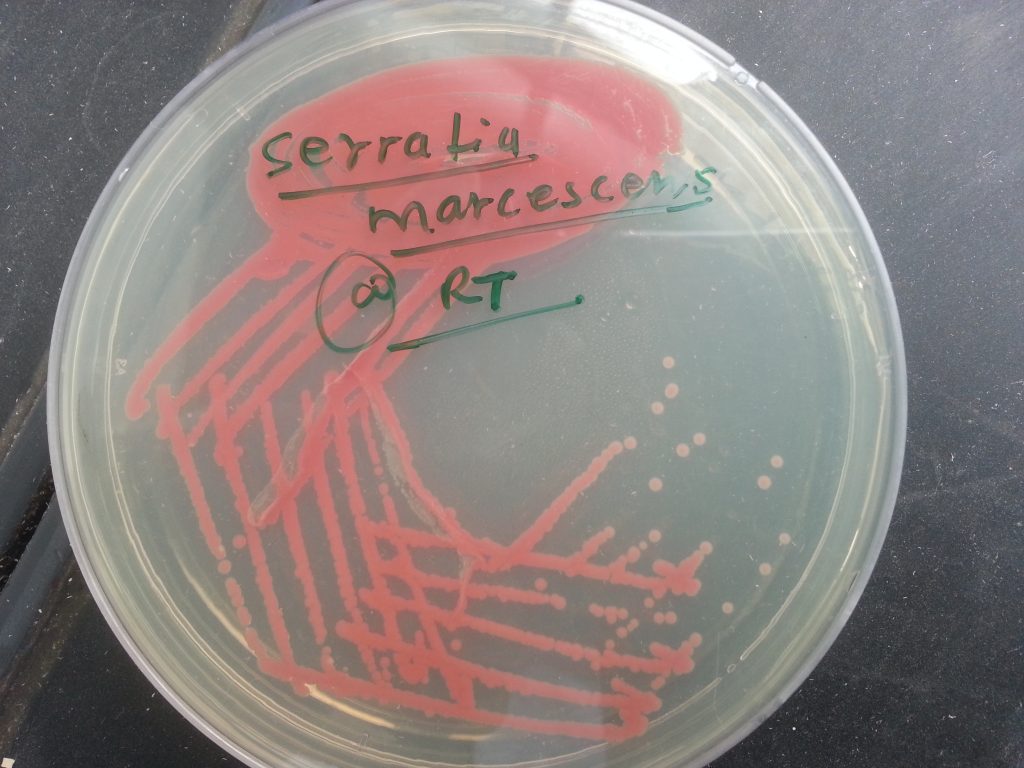
Which of the following bacteria is known to produce a red pigment when grown on culture media?
A. Pseudomonas aeruginosa
B. Staphylococcus aureus
C. Serratia marcescens
D. Proteus mirabilis
C. Serratia marcescens
✅ C. Serratia marcescens – Produces a red pigment called prodigiosin, especially at room temperature.
❌ A. Pseudomonas aeruginosa – Produces blue-green pigment (pyocyanin) and sometimes yellow-green (fluorescein).
❌ B. Staphylococcus aureus – Produces golden-yellow colonies, not red.
❌ D. Proteus mirabilis – Known for swarming motility, not pigment production.
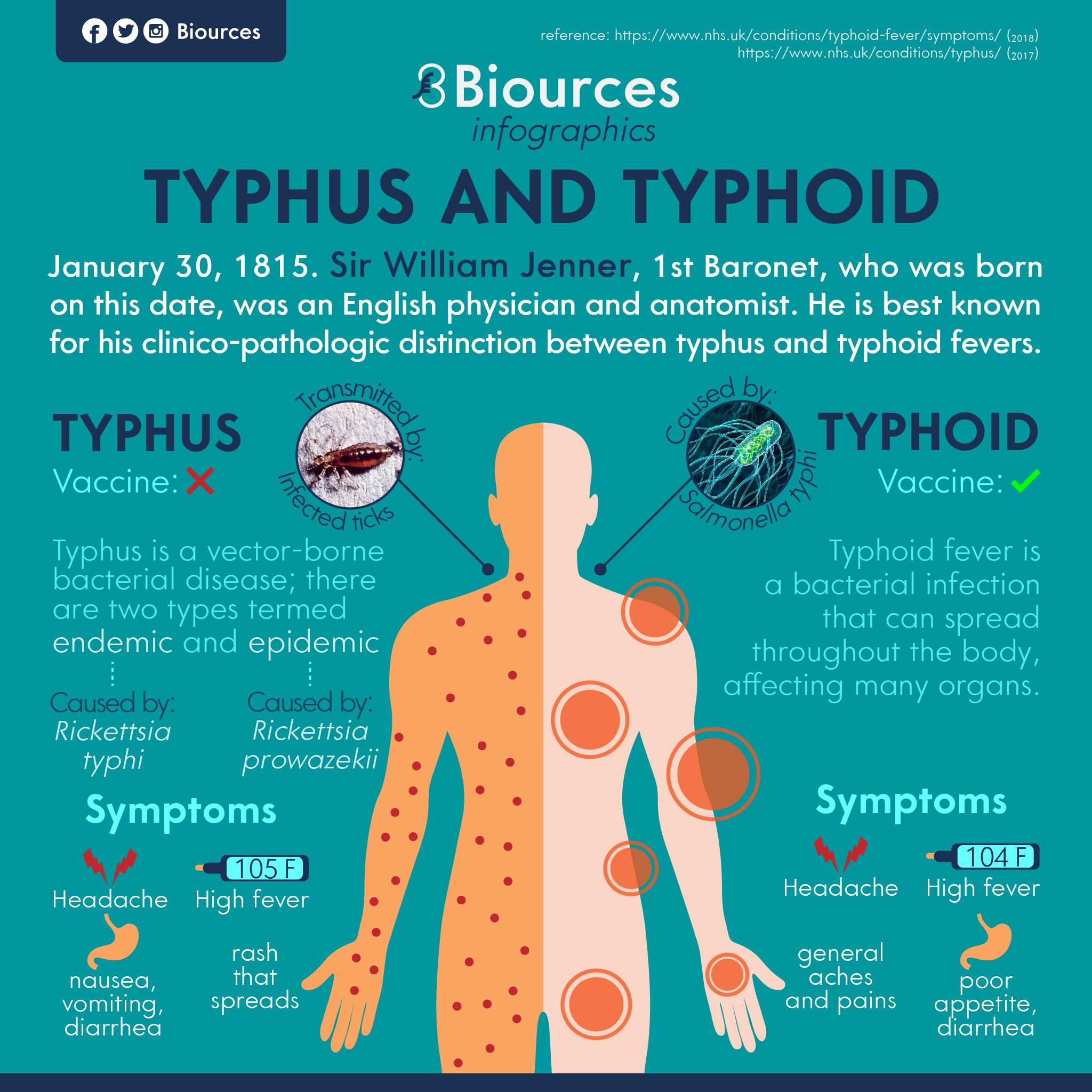
Which of the following correctly distinguishes typhoid fever from typhus?
A. Typhoid fever is transmitted by lice and typically presents with a trunk-centered rash.
B. Typhoid fever is caused by Rickettsia species and leads to constipation and rash.
C. Typhoid fever is a bacterial infection spread via the fecal-oral route and commonly presents with diarrhea.
D. Typhoid fever is a viral illness that spreads through flea bites and presents with respiratory symptoms.
C. Typhoid fever is a bacterial infection spread via the fecal-oral route and commonly presents with diarrhea.
Typhoid fever is caused by Salmonella typhi, a Gram-negative bacillus, and is transmitted via contaminated food and water (fecal-oral route).
It typically presents with prolonged fever, abdominal pain, and diarrhea or constipation, sometimes with "rose spots" on the skin.
Typhus, on the other hand, is caused by Rickettsia species, transmitted by lice or fleas, and presents with high fever and a rash that starts on the trunk and spreads outward.
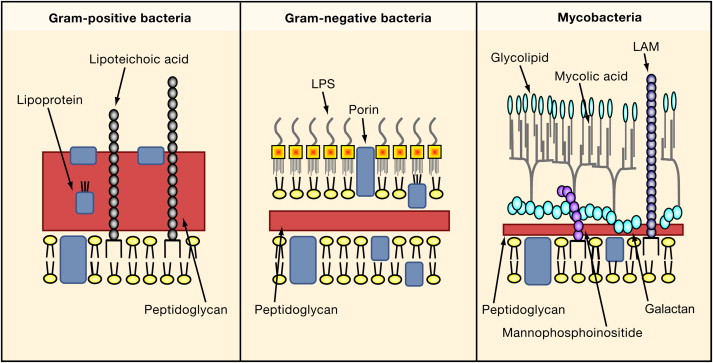
Which of the following is a characteristic feature of Mycobacterium tuberculosis?
A. Gram-positive spore-forming rod
B. Acid-fast bacillus with mycolic acid in the cell wall
C. Motile rod with polar flagella
D. Causes acute, self-limiting gastrointestinal disease
B. Acid-fast bacillus with mycolic acid in the cell wall
M. tuberculosis is acid-fast due to its high lipid (mycolic acid) content. It is non-motile, non-spore-forming, and causes chronic pulmonary disease.