Lipid Metabolism
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
What are the functions of lipids?
1- Major source of energy
2- Major component of cell membranes
3- Biosynthetic precursors
4- Cell signalling (prostaglandins & steroid hormones)
5- Facilitate absorptions of fat-soluble vitamins (eg. A,E,D,K)
6- Protections & insulation
What is the first step of lipid metabolism?
Digestion
At which sites of the body can lipids be digested?
1- Mouth
2- Stomach
3- Small intestines
What enzyme is involved in the digestion of lipids in the mouth?
Lingual lipase
What enzyme is involved in the digestion of lipids in the stomach?
Gastric lipase
What substance and enzyme are involved in the digestion of lipids in the small intestines?
1- Bile salts
2- Pancreatic lipase
At the small intestines, what does the substance, bile salts, do to the lipids?
Lipids are emulsified by the bile salts
Why are lipids emulsified by the bile salts first at the small intestine?
To increase the surface area, upon which the enzyme, pancreatic lipase, can work on
What does the pancreatic lipase do to the emulsified lipids at the small intestine?
Pancreatic lipase can further breakdown (hydrolyse) the emulsified lipids, eg. triglycerides
Where are the bile salts stored?
In the gallbladder
From where is the pancreatic lipase released?
Pancreas
What is the function of the hormone, cholecystokinin (CCK)?
When food enters the small intestine, CCK signals the release of pancreatic lipase and the contraction of the gallbladder, by which bile salts can be released to emulsify the lipids.
What are the products of digestion/ hydrolysis of triglycerides?
1- Fatty acids (3 molecules)
2- Glycerol (1 molecule)
After the breakdown of triglycerides, what is the next step?
Absorption of lipids
What is the first step of lipid absorption?
1- Fatty acids and glycerol are emulsified by bile salts to form micelles
2- Micelles travel through layer of water and enter intestinal epithelial cells
3- At intestinal epithelial cells, fatty acids and glycerol undergo enzymatic reaction at SER, to form triglycerides
4- Triglycerides are combined with proteins at the Golgi apparatus to form chylomicrons (lipoprotein particles)
5- Chylomicrons enter the lacteal (lymph vessels of small intestine) and are transported away from intestines
What are chylomicrons?
Lipoprotein particles
What is the nature of chylomicrons?
Amphipathic - polar and non polar
What is the function of chylomicrons?
To transport digested lipids (in the form of recombined triglycerides) in circulatory system and enter adipose and other tissues
Which step, in lipid metabolism, does lipid absorption fall under?
2nd step
What is the nature of lipids?
Hydrophobic
Due to their hydrophobic nature, how are lipids transported?
The lipids, triglycerides (TAG) and cholesterol, require special transport proteins = lipoproteins
What are some examples of lipoproteins?
1- Chylomicrons
2- Very low density lipoproteins (VLDL)
3- Low density lipoproteins (LDL)
Where do chylomicrons transport lipoproteins?
From small intestine to rest of the body
What do VLDL carry/ transport?
Synthesised TAG
What do LDL carry/ transport?
Cholesterol
Where do LDL carry/transport cholesterol to?
Peripheral tissues
Therefore, what factor determines the transport of lipoproteins?
Their density - which varies
How many different classes of lipoproteins are there?
Four classes
What are the four classes of lipoproteins (in order of increasing density)?
1- Chylomicrons
2- VLDL
3- LDL
4- High density lipoproteins (HDL)
Are LDL good or bad?
Bad
Why are LDLs bad?
Can increase risk of heart disease and stroke = high levels of LDLs
Are HDL good or bad?
Good
Why are HDLs good?
Can lower risk of heart disease and stroke = high levels of HDLs lowers risk
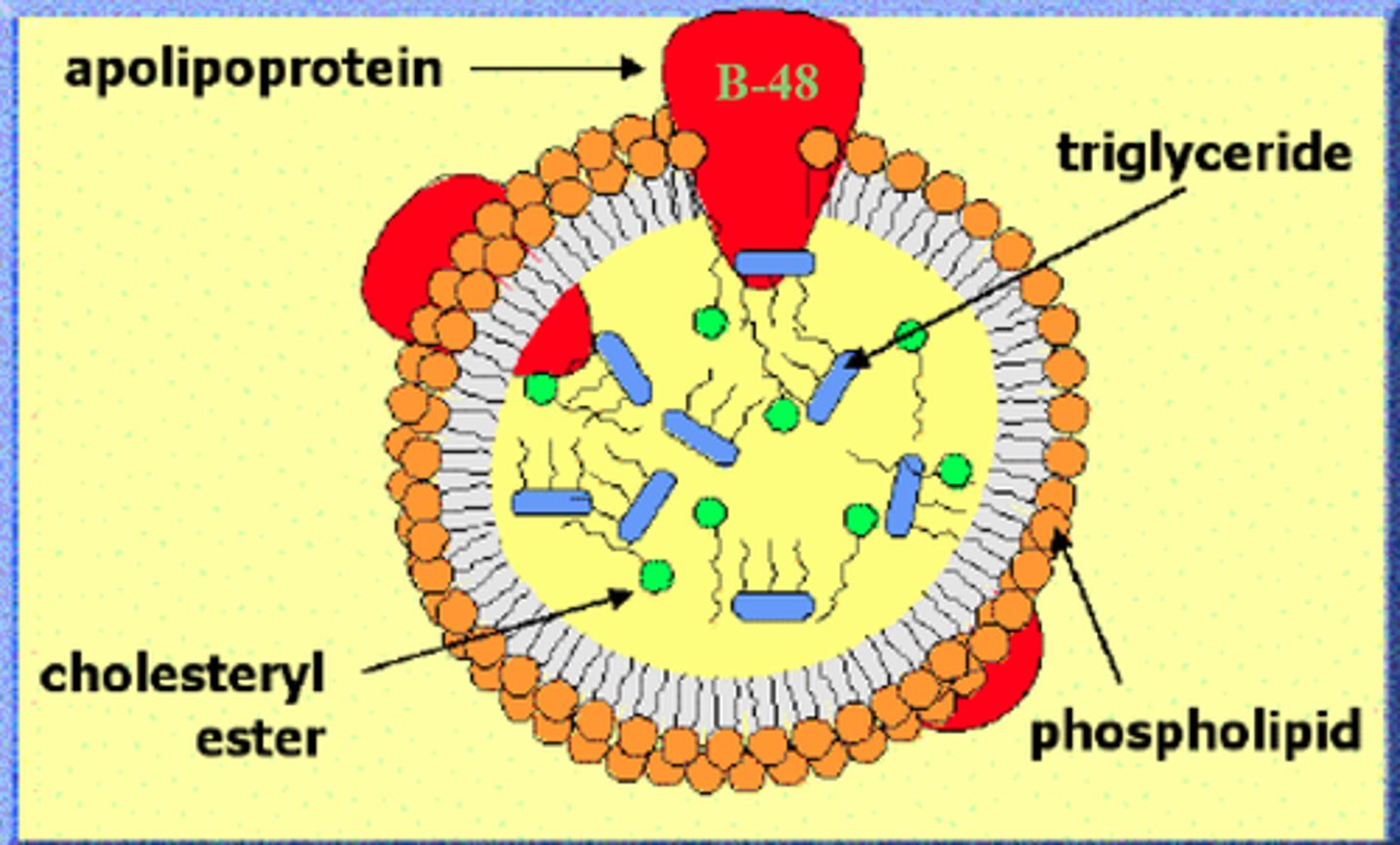
Image of lipoprotein = chylomicron?
What is the fate of chylomicrons?
Lipid catabolism
What are chylomicrons broken down by?
Lipoprotein lipase (LPL)
Where does the breakdown of chylomicrons occur?
1- Capillaries of skeletal muscle
2- Capillaries of cardiac muscle
3- Adipose tissue
When chylomicrons are broken down, what do they release?
TAG
What happens to the released TAG?
Are broken down into fatty acids and glycerol
What do the fatty acids and glycerol molecules then do?
Fatty acids and glycerol molecules then enter the cells of the site of their formation, eg. cardiac cells if chylomicrons were broken down to form these molecules in cardiac muscle
What is the fate of these fatty acids now?
1- Major fate is to be stored in adipose tissue
2- But they can also be oxidised for energy in muscles and other tissues
How can these fatty acids be oxidised for energy?
1- Fatty acids converted to Acyl CoA
2- Acyl CoA crosses membrane for beta oxidation
3- During beta oxidation, Acyl CoA is turned into Acetyl CoA
4- This Acetyl CoA enters TCA cycle to produce ATP
Summarise the conversion of fatty acids to ATP during beta oxidation?
1- Fatty acids -> Acyl CoA
2- Acyl CoA crosses mitochondria
3- Beta oxidation
4- Acyl CoA -> Acetyl CoA
5- Acetyl CoA enters TCA cycle -> ATP
What is the fate of the glycerol molecule now?
1- Converted to Glycerol 3-phosphate (G3P) for glycolysis or gluconeogenesis
If Acetyl CoA, from the beta oxidation, doesn't produce ATP, what happens to it?
Acetyl CoA is converted to ketone bodies
When is Acetyl CoA converted to ketone bodies?
When there is excess production of Acetyl CoA and this overloads the TCA cycle
What is the purpose of ketone bodies?
Ketone bodies serve as a fuel source if glucoses is limited
When can ketones be used as a source of fuel?
1- During starvation
2- Diabetics who can't use glucose
What is DKA?
Diabetic ketoacidosis- a complication of type 1 diabetes, resulting in dangerously high ketone and blood sugar levels
Where does ketone synthesis occur?
In mitochondria of liver cells
How are ketones produced in ketone synthesis?
1- Excess Acetyl CoA -> Hydroxymethylglutaryl CoA (HMG CoA)
2- HMG CoA -> beta- hydroxybutyrate (primary ketone body in blood)
What else is HMG CoA?
Precursor of cholesterol
What are the functions of cholesterol?
1- Component of cell wall
2- Precursor of bile acids/salts and steroid hormones and vitamin D
What does a cholesterol molecule contain?
4 fused rings
What is cholesterol made of?
Acetyl CoA
What are the five stages of cholesterol synthesis (basic)?
1- Acetyl CoA -> HMG CoA
2- Synthesis of Mevalonic acid
3- Generation of Isoprenoid units
4- Synthesis of Squalene
5- Cholesterol
What is the synthesis of cholesterol in liver regulated by?
Hydroxymethylglutaryl CoA reductase (HMG CoAR)
What is the expression of HMG CoAR regulated by?
A transcription factor = SREBP
What happens, genetically, when cholesterol levels are low?
1- SREBP activity is increased
2- HMG CoAR gene enhanced
3- More cholesterol synthesis
What happens, genetically, when cholesterol levels are high?
1- SREBP activity reduced
2- HMG CoAR gene activity reduced
3- Less cholesterol synthesis
Summarise the regulation of cholesterol levels?
SREBP gene -> HMG CoAR -> Cholesterol synthesis
Other than cells being able to synthesis cholesterol, how else can they obtain cholesterol?
Via LDLs
How can LDLs provide cells with cholesterol?
1- Cells have LDL receptors
2- LDLs bind to these receptors
3- LDL receptor complex undergoes endocytosis
4- Once inside the cell, lipoprotein is degraded and cholesterol is released and enters cytosol
What can excess accumulation of cholesterol lead to?
Build up of plaques in arteries
What is build up of plaque, due to excess accumulation of cholesterol, in arteries known as?
Atherosclerosis
Why are HDLs important/ considered to be good?
They remove excess cholesterol from cells
How do HDLs remove excess cholesterol from cells?
1- Transporter protein removes cholesterol from cytoplasmic side to extracellular side
2- Here cholesterol diffuses into HDL
Abbreviation for Cardiovascular disease?
CVD
How is LDL associated with CVD?
LDL is positively associated with CVD
How is HDL associated with CVD?
HDL is negatively associated with CVD
What factors does a lipid profile include?
1- Total cholesterol levels
2- HDL population
3- LDL population
4- Cholesterol:HDL ratio
How can atherosclerosis occur with LDLs?
High levels of LDLs will deposit in inner walls of arteries supplying the heart and brain
After the deposition of these high levels of LDL in inner walls of arteries, supplying heart and brain, what is the consequence?
Plaque formation in these important arteries
As a result of plaque formation, what happens to these important arteries?
1- Arteries become more narrow
2- Arteries are less flexible
3- There is a reduction in the amount of oxygen delivered to vital organs as a result of this
How do heart attacks and stroke arise?
Due to clot formation in the arteries supplying the heart
What is atherosclerosis characterised by?
1- Endothelial dysfunction
2- Vascular inflammation
3- build up of lipids, cholesterol, cellular debris within vessel wall
What are the five steps of atherogenesis?
1- Endothelial dysfunction: aging, smoking, cholesterol, obesity, heart failure, diabetes
2- Formation of lipid layer pithing intima (innermost layer) : LDL and VLDL
3- Migration of leukocytes and smooth muscle cells into vessel wall
4- Foam cell formation: macrophages absorb lipids
5- Degradation of extracellular matrix : plaque rupture
Summarise the development of atherosclerosis?
1- Endothelial cells take up LDLs (due to endothelial permeability)
2-Monocytes also involved in uptake of LDLs
3- Mature monocytes -> macrophages
4- Macrophages uptake LDL particles and yield them into foam cells
5- Smooth muscle cells migrate into intima of vessels
6- Fibrous cap of plaque ruptures -> blood coagulation -> thrombus formation
The gallbladder provides ----------------, that aids in transport of lipids across the intestinal membrane:
Bile salts
Which of the following step is not involved in atherosclerosis?
A. Foam cell formation
B. Endothelial dysfunction
C. Leukocytes migration
D. Degradation of extracellular matrix
E. Accumulation of HDL within intima
E. Accumulation of HDL within intima