H&I V: Exam 1: O2 & Gas Exchange
1/156
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
157 Terms
pulmonary edema definition
fl accumulation in alveoli and interstitial spaces of lungs
most common cause of pulmonary edema
left sided heart failure
s/s pulmonary edema
-SOB
-Tachypnea
-Hypoxemia
-frothy secretions
lung auscultation of pulmonary edema
rales/crackles
pleural effusion
-collection of fl around lungs
-limits expansion of lung
s/s pleural effusion
-worsening dyspnea
-cough
-chest pain/pain on inspiration
lung auscultation for pleural effusion
diminished or absent breath sounds on affected area
atelectasis definition
complete or partial collapse of lung
-alveoli within lung become deflated
most common cause of atelectasis
-airway obstruction from retained exudates and secretions
-postop/hypoventilation
what do s/s of atelectasis depend on
depend on size and how rapidly it developed
s/s rapidly developing atelectasis
-pain on affected side
-sudden dyspnea
-cyanosis
s/s slowly developing atelectasis
asymptomatic or minor s/s (mild sob, cough)
lung auscultation for atelectasis
diminished or absent breath sounds in affected area
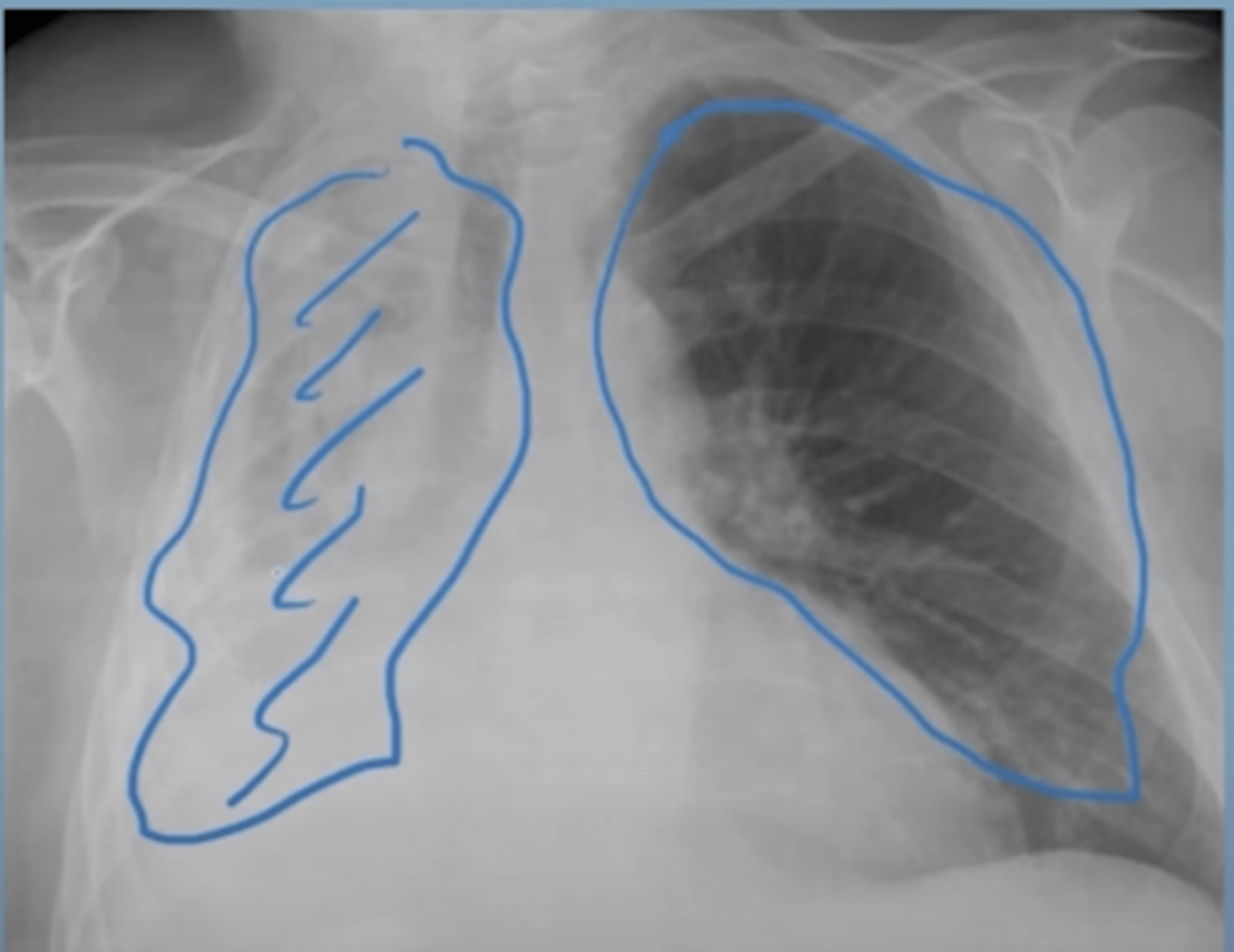
description of atelectasis xray
Right lung: All alveoli are full of air which shows black on an x-ray.
Left lung: All alveoli are collapsed and don’t have air in them, showing white on x-ray
what is ventilation (VQ)
amount of air that enters and leaves alveoli
what is perfusion (VQ)
how much blood the heart sends through the lungs per minute
what is the VQ ratio
-amount of air that reaches the alveoli per minute compared to the amount of blood that reaches the alveoli per minute
normal VQ ratio
0.80 (4 L air into lungs, 5 L blood into lungs)
what causes a high VQ ratio
if there is more ventilation or less perfusion
-most of the O2 inhaled is going back out, because there isnt enough blood going through the lung to pick it up
example of high VQ ratio
could occur when there is decreased blood flowing through the lungs but normal ventilation as seen in a pt with a pulmonary embolism
what causes a low VQ ratio
-if there is less ventilation or more perfusion
-the lungs are getting enough blood but not enough air (perfusion is greater than ventilation)
example of a low VQ ratio
could occur during an asthma exacerbation because perfusion would be normal, but there would be decreased ventilation
what is ARF caused by
failure to adequately ventilate and/or oxygenate that causes a VQ mismatch
what is ventilatory failure d/t
-mechanical abnormality of the lungs or chest wall
-impaired function of the resp muscles (especially diaphragm)
-malfunction in the resp control center of brain
what causes oxygenation failure
-lack of perfusion to pulmonary capillary bed (pulmonary embolism)
-condition that alters the gas exchange medium (pulmonary edema, pneumonia)
when can both inadequate ventilation and oxygenation occur
pts with disease lungs (asthma, emphysema, CF)
-diseased lung tissue can cause oxygenation failure and increased work of breathing, eventually resulting in resp muscle fatigue and ventilatory failure
what are the 2 types of resp failure
-lung failure/hypoxemic resp failure
-ventilation failure/hypercapnic resp failure
what is lung failure/hypoxemia resp failure
when there is not enough oxygen to the tissues d/t inadequate oxygen availability
what is ventilation failure/hypercapnic resp failure
when there is an increase in CO2 d/t poor ventilation or resp effort (not blowing it off)
s/s hypoxemia (ARF)
-dyspnea
-low O2 saturation
-irritability
-confusion
-tachycardia/arrhythmia
-tachypnea
-cyanosis (late sign)
s/s hypercapnia (ARF)
-HA
-change in behavior
-coma/obtunded
-asterixis
what is asterixis
flapping tremor
what can s/s of ARF vary based on
underlying condition, degree of hypoxia, hypercapnia, and acidosis present
pathway of lung failure/hypoxemia resp failure
not enough O2 is provided to resp system --> oxygenation failure (insufficient O2 transfer to blood) --> leads to impaired tissue perfusion --> production of lactic acid --> metabolic acidosis --> tissue/cell death
what is severe hypoxemia without hypercapnia
PaO2 < 60 mmHg
causes of lung failure/hypoxemia resp failure
-VQ mismatch
-pulmonary edema/HF
-COPD/emphysema
-atelectasis
-interstitial disease of the lung (pulmonary fibrosis)
tx for lung failure/hypoxemia resp failure
-usually require mechanical ventilation
what type of acidosis is ventilation failure/hypercapnic resp failure
increased CO2 = resp acidosis
what can hypercapnia result from
-increased CO2 production secondary to increased metablism (sepsis, fever, burns)
-decreased CO2 excretion
what pts are more likely to develop hypercapnia resp failure
-End-stage COPD - decreased CO2 excretion
-Spinal cord injury causing quadriplegia - failure of the respiratory pump
-Recently received a medication that decreases respiratory drive. Such as a benzodiazepine or an opioid- decreased CO2 excretion
what can hypercapnia eventually cause
hypoxemia d/t decreased resp drive
what is the priority in ARF
restoring resp and hemodynamic stability
ARF interventions
-Perform a respiratory assessment on the client who has respiratory failure on a frequently scheduled basis and as needed to ensure early identification of any decline in condition.
-Increase oxygen levels in the blood (goal is SPO2 over 90%)
-Start with the least invasive measure (measures include nasal cannulas, facemasks, and non-rebreathers, followed by noninvasive ventilation, such as BiPAP or CPAP) and progress to the most invasive (mechanical ventilation with endotracheal intubation) based on the client’s condition.
-It is a priority to identify and treat the underlying cause of respiratory failure (but you still must address the respiratory failure- ex: PNA)
-Correct respiratory gas imbalances, such as hypercapnia and hypoxia.
causes of acute resp distress syndrome (ARDS)
-sepsis (inflames entire body)
-resp inflammation (PNA, inhaled toxin, aspiration)
-acute pancreatitis (high risk)
why can acute pancreatitis cause ARDS
d/t accidental release of active pancreatic enzymes and cytokines into bloodstream which get sucked into lungs causing inflammation
what is the most common cause of ARDS
sepsis
what happens in ARDS
-Despite different causes of Acute lung injury (ALI) in ARDS, the trigger is a systemic inflammatory response that is an ongoing inflammation in the alveoli and pulmonary vasculature. This response is known as a “cytokine storm” and, when prolonged, results in thick, swollen tissues that hinder gas exchange and promote the formation of scar tissue.
-The alveoli become hard due to the capillaries around the Alveoli becoming inflamed & fluid-filled, creating a leaky barrier, which eventually fills up the alveoli sacs. THIS makes it impossible to get oxygen in & to get CO2 OUT!
-Eventually clients DIE from hypoxia IF they are not on a ventilator early.
when do s/s of RDS usually develop
within 3 days and nearly always within 7 days post known clinical insult (infection or trauma)
progressive worsening resp symptoms in ARDS
-Dyspnea/tachypnea
-Cough
-Chest Discomfort
-Anxiety/restlessness
-No improvement in O2 saturation with increasing oxygen administration
physical exam for ARDS
-Tachypnea with use of accessory muscles at rest, nasal flaring (initially) (Unable to compensate→ respiratory acidosis)
-Tachycardia at rest (As the demand for oxygen to the cells of the body increases, tachycardia occurs)
-Hypotension is often present
-Cyanosis (late sign)
-Fever may or may not be present
-May hear bilateral crackles, coarse rhonchi, wheezes depending on severity of fluid in lung fields.
-Cold, mottled dusky extremities with prolonged CRT (>3 sec)
Labs/dx tests for ARDS
-ABGs
-CXR
-CT scan
-blood tests
-blood/sputum cultures
-ECG
ABGs for ARDS
-SaO2= less than 90%
-PaO2= less than 60%
-pH= less than 7.3 (Acidosis)
blood tests for ARDS
CBC and electrolyte disturbances, BUN/creatinine (AKI--> MODS)
blood and sputum culture for ARDS
ID pathogens as possible source of infection
ECG for ARDS
to exclude cardiac involvement
pharm tx for ARDS
- no definitive drug therapy (treat the cause)
- early abx
-vasopressors
-diuretics, steroids, bronchodilators, nebulizer treatments
early abx tx for ARDS
pneumonia/sepsis
vasopressors for ARDS
to maintain BP/tissue perfusion PRN
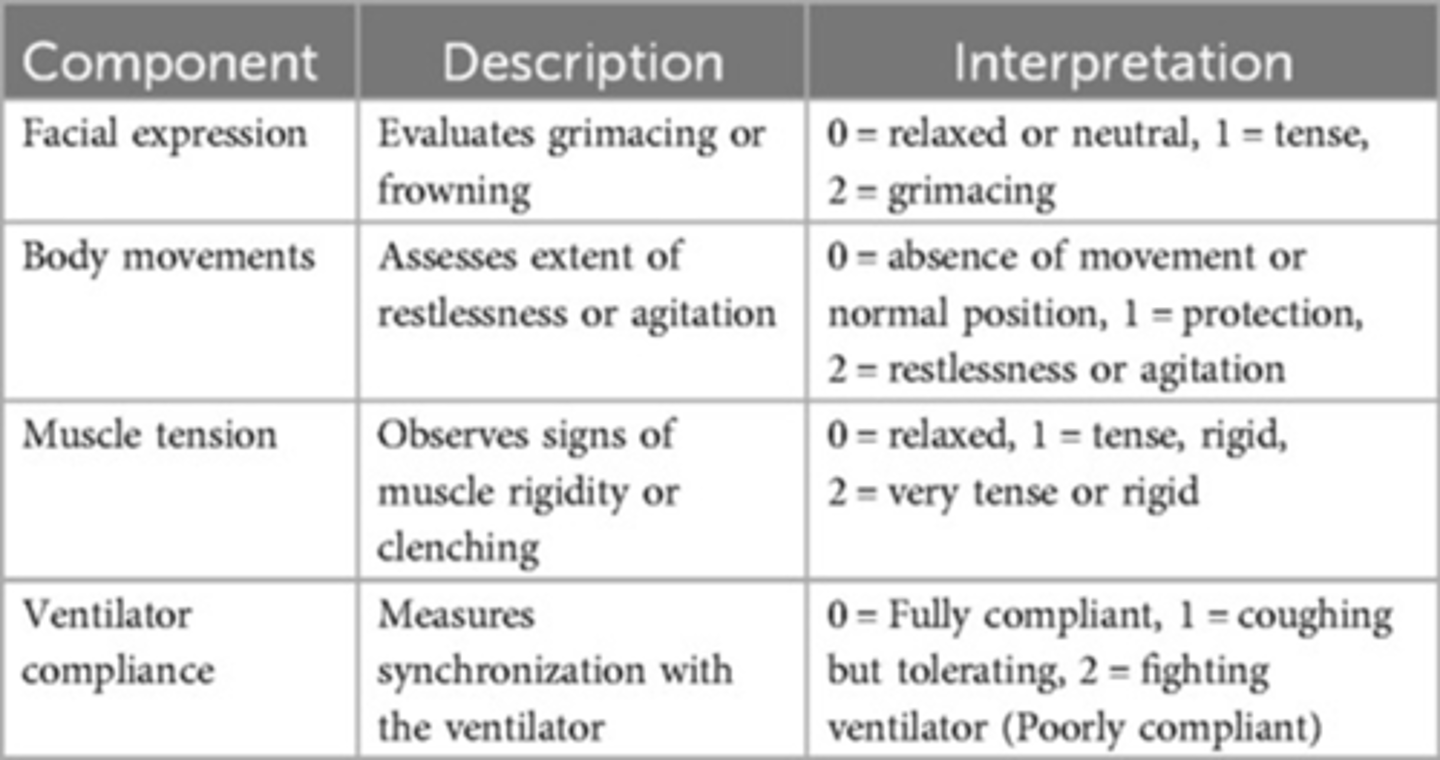
pain management for ARDS
-fentanyl, morphine sulfate
-tx pain before sedation
sedation while intubated
-sedation to decrease O2 consumption and prevent extubation
-drugs titrated based on the RASS
meds for sedation while intubated
-propofol
-midazolam
-dexmedetomidine (precedex)
-benxodiazepines (lorazepam) to reduce anxiety/resistance to ventilation
when is propofol contraindicated
egg allergies
ventilator associated pneumonia (VAP) prophylaxis
-PPI (pantoprazole (protonix)) to prevent GI stress ulcers
-HOB 30 degrees
-oral care Q4
nursing interventions for ARDS with intubation/mechanical ventilation
-Monitor (vital signs hourly, oxygenation status, neurological status, lung & heart sounds, LOC)
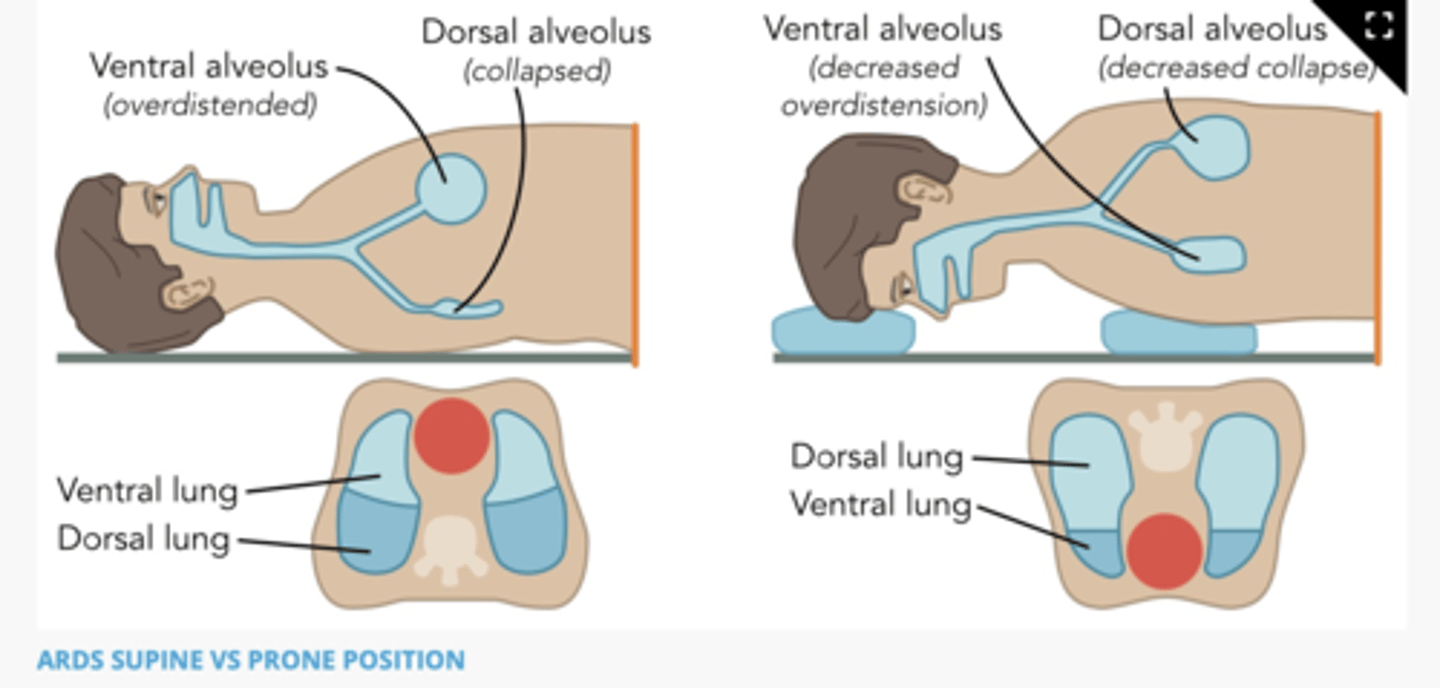
-Prone position as tolerated >12 hrs/day (for severe ARDS)
-Provide analgesia, anxiolytics, sedation
-Maintain HOB at fowlers or higher
Suction airway PRN
-Watch for indicators of poor perfusion
-Protect skin integrity
proning for intubation/mechanical ventilation
decreases amount of weight and compression on lungs, allowing more air to get to alveoli (improved ventilation) and improves lung efficiency by getting O2 to parts of your lungs that get the most blood flow (improved gas exchange)
proning diagram
CPAP
-has 1 pressure setting that delivers a steady continuous pressurized air into the airway throughout spontaneous inspiration and exhalation (to prevent collapsing)
components of CPAP
-requires intact resp drive and adequate tidal volume
-corrects hypoxemia
-will increase O2, decrease work of breathing, increase intrathoracic pressure, decreasing preload/work of heart
why is CPAP the most effective tx for sleep apnea
because positive pressure acts as a splint to keep the upper airway and trachea open during sleep
bipap (bi-level positive airway pressure)
has 2 pressure settings that delivers a different pressure for inspiratory and expiratory phases of breathing
-almost like a pushing (inhalation) and pulling (exhalation)
components of bipap
-RR is programed into the machine
-ex: orders- bipap 10/5 rate of 12 FiO2 40$
-corrects hypercapnia/hypercarbia
-most often used for pts with COPD and require ventilatory assistance
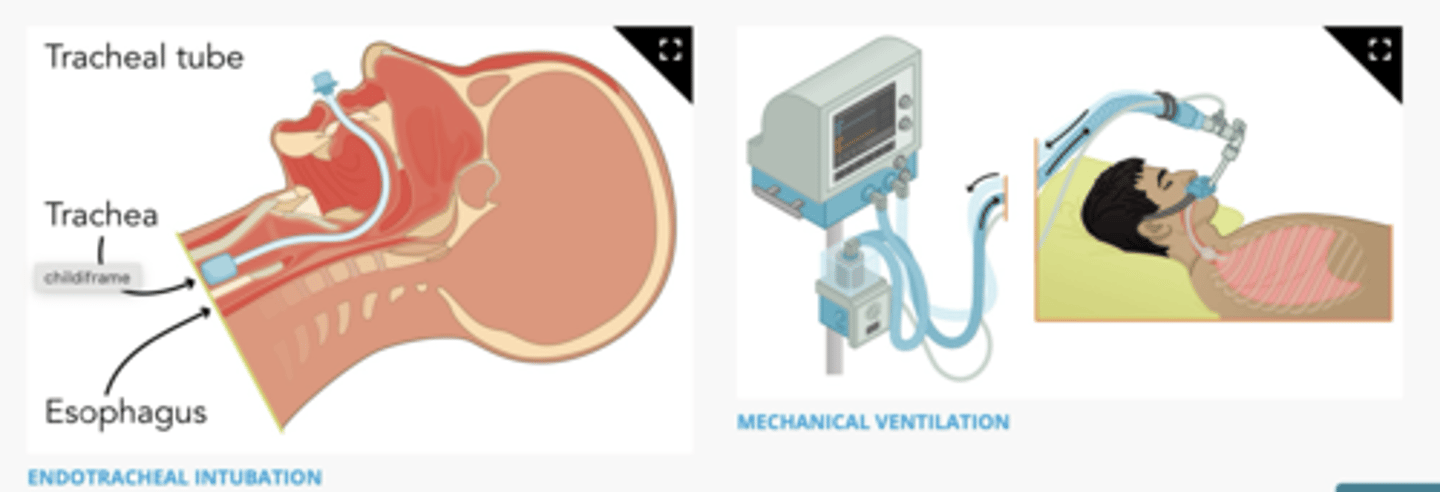
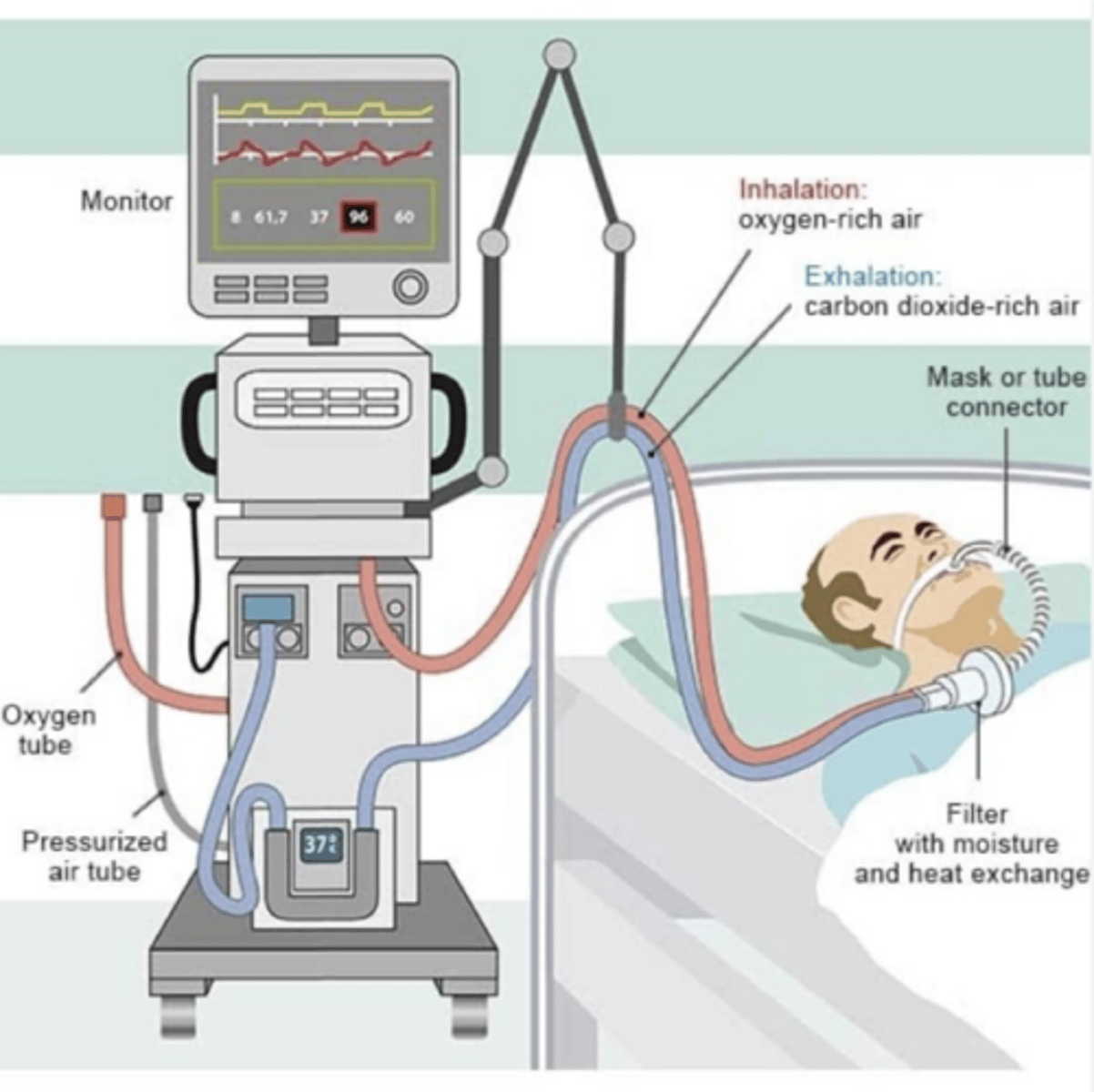
endotracheal intubation/mechanical ventilation diagram
what is mechanical ventilation generally used for
-increasing PaCO2
-allows resp muscles to rest
-these pts will generally have low PaO2 and high PaCO2, they may have tried alternative methods such as bipap that have not been effective
two types of mechanical ventilation
-endotracheal
-tracheostomy
what happens with endotracheal intubation
a tube is inserted through the mouth into the trachea
-this allows for emergency airway management of this pt
when is nasal intubation performed
when pt has facial or oral trauma
indications for mechanical ventilation
-severe resp distress
-failure of noninvasive ventilation (nasal cannula, CPAP, BiPAP)
-arterial blood gas abnormalities
severe resp distress indications for mechanical ventilation
-sustained tachypnea >30
-accessory muscle use
-AMS
ABG abnormality indications for mechanical ventilation
-hypoxemia that has not corrected with sup O2
-severe resp acidosis, unresponsive to therapy
types of artificial airway
-short term (ET tube)
-long term (tracheostomy)- longer than 14 days, may be recommended
what is rapid sequence intubation (RSI)
term used for intubating a pt in the ER, ICU, or during a rapid response/code blue
nursing responsibilities for RSI
-administering meds in correct order
-prepare continuous sedation medications for after intubation
sequence of medications during RSI
-pain meds (fentanyl)
-sedation (etomidate)
-paralytic (succinylcholine/rocuronium)
monitoring during RSI
-BP (will likely drop)- need to have something available to support BP when this happens (fls, pressors)
-HR/rhythm
-O2 sats (will likely go down during intubation, responsibility of RN to update intubating provider)
continuous sedation and pain meds
-propofol
-midazolam (versed)
-dexmedetomidine (precedex)
-fentanyl
components of propofol
-works quickly
-rapidly metabolized
-will drop BP
-will depress resp drive
components of midazolam (versed)
-takes longer to metabolize
-depress RR
components of dexmedetomidine (precedex)
-takes longer to metabolize
-often needs loading dose to reach max effectiveness
-will drop HR
-does not impact RR
components of fentanyl
-given with continuous IV infusion
-titrated based on CPOT
-will impact RR
critical care pain observation tool (CPOT) diagram
placement of ET
-Intubation is typically performed by a nurse anesthetist, anesthesiologist, critical care or emergency physician, or pulmonologist.
-A chest x-ray verifies correct placement of the endotracheal (ET) tube.
-ET tubes can be cuffed or uncuffed (the cuff on the tracheal end of an ET tube is inflated to ensure proper placement and the formation of a seal between the cuff and the tracheal wall. (This prevents air from leaking out around the ET tube.))
-The seal ensures that an adequate amount of tidal volume is delivered by the mechanical ventilator when attached to the external end of the ET tube.
-The client is unable to talk when the cuff is inflated.
nursing actions for ET
-Have resuscitation equipment to always include a manual resuscitation bag with a face mask at the bedside.
-Ensure the intubation attempts last no longer than 30 seconds and then reoxygenate before another attempt to intubate.
-Monitor vital signs and verify ET tube placement by checking end-tidal carbon dioxide levels, chest x-ray, and frequent arterial blood gases
-Auscultate for breath sounds bilaterally after intubation.
-Monitor for hypoxemia, dysrhythmias, and aspiration.
-Respiratory assessment / RASS q2hrs (Goal -1 and 0 ) Adm. Pain &/or sedation meds (Avoid over sedation)
-Assess ET tube position & securement device (✓ cm markings) q4hrs
-✓ ET for proper cuff inflation/examine vent equipment & settings
-Suctioning PRN (sterile)
-Assess skin integrity/Tq2hrs/ROM
what does a ventilator do
-provides O2 to lungs
-helps remove CO2 from lungs
-provides pressure to keep alveoli from collapsing
ventilator diagram
modes (how the air will be delivered) of mechanical ventilation
-pressure regulated volume control (PRVC)
-assist control (AC)
-synchronized intermittent mandatory ventilation (SIMV)
-pressure support (PS)
what is pressure regulated volume control (PRVC)
-vent will try to administer a certain volume of air to the lungs
-should reach a certain resistance while pushing, the vent will drop the remaining volume
types of PRVC
pre-set RR, PEEP, TV
-vent will give a minimum number of breaths per min, but allows for the pt to "over breathe the vent" meaning they are breathing over the minimum settings
what is AC
assist with each breath by either providing volume or pressure, depending ont he setting
-if the RR fall below a predetermined setting, the vent will take over or control ventilation
-mem trick: Actively Controls breathing
what is synchronized intermittent mandatory ventilation (SIMV)
administers ventilation with the pts own inspiratory efforts, with not all breaths being supplemented
-a preset rate ensures a mandatory delivery of a preset number of breaths per minute
what is pressure support (PS)
-used when weaning the pt off the vent to prepare for extubation
-a pre-set pressure setting in which the vent helps with push air in for pt
-preparing for extubation, can be on PS for several days before being extubation, can undergo PS trials