ob exam 3
1/116
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
117 Terms
High risk pregnancy and risks for a high risk pregancy
life or well-being of pregnant woman or fetus are jeopardized
Risks include
Biophysical
genetic, nutrition, medical disorder,
Psychosocial
smoking, alchohol, caffeine illicit drugs, mental health disorders, poor family
sociodemogrpahic
low income, lack of care, marital status
environmental
infections pollutants chemicals secondhand smoke
Hypertensive disorders
Gestational Hypertension (GHTN)
Preeclampsia (PreE)
Chronic Hypertension (CHTN)
Superimposed Preeclamspsia (SIPE)
Gestational Hypertension
(GHTN)
Gestational hypertension is a condition in pregnancy defined by new-onset high blood pressure after 20 weeks of gestation without proteinuria or other signs of organ damage.
BP>140/90 but <160/110
GA>20 weeks
Preeclampsia
PreE
pregnancy-specific syndrome characterized by new-onset hypertension after 20 weeks of gestation plus signs of organ dysfunction or proteinuria.
BP>140/90 + proteinuria
other symptoms also involved
GA >20 weeks
Chronic Hypertension
CHTN
high blood pressure that exists before pregnancy or is diagnosed before 20 weeks of gestation
BP > 140/90
GA < 20 weeks or pre-pregnancy
preexisting hypertensive disorder
Superimposed Preeclampsia
occurs when a woman with pre-existing (chronic) hypertension develops preeclampsia during pregnancy. It’s essentially preeclampsia on top of chronic hypertension.
chronic HTN + PreE
sudden increase in BP when previously well controlled
new onset proteinuria
Preeclampsia
Pregnancy specific condition
Placenta is suspected to be the root cause of PreE wether that be placement which can lead to hypoxia and then release of endothelial changing substance
Patho
vascular remodeling of small blood vessels
results in altered perfusion and endothelial damage —> vasospasm —> poor tissue perfusion, increased peripheral resistance
Symptoms
Headache (persistent, not relieved by Tylenol)
Swelling/edema (hands, face)—not required for diagnosis
Nausea or vomiting (especially if sudden in 2nd–3rd trimester)
Sudden weight gain from fluid retention
Visual changes
Blurry vision
Spots or flashing lights
Temporary vision loss
Right upper quadrant/epigastric pain (from liver involvement)
Shortness of breath (from pulmonary edema)
clonus
clonus
Clonus is an involuntary, rhythmic, repetitive contraction and relaxation of a muscle after sudden stretch (e.g., rapid ankle dorsiflexion).
It indicates upper motor neuron (UMN) dysfunction and neuromuscular hyperexcitability.
Common in severe preeclampsia, stroke, MS, spinal cord injury, and serotonin syndrome.
variations of preE
Preeclampsia without severe features (SF)
PreE with severe features (SF)
HELLP syndrome
Eclampsia
Preeclampsia without sever features
is a milder form of preeclampsia where a pregnant woman meets the basic diagnostic criteria for preeclampsia but does not have any severe symptoms or organ dysfunction.
BP>140-159 / 90-109
2 readings at least 4 hours apart
proteinuria
PreE with severe features (SF)
more serious form of preeclampsia where, in addition to hypertension and proteinuria (or end-organ involvement), the patient develops severe symptoms or laboratory abnormalities that indicate high maternal or fetal risk.
BP> or = 160/110
2 readings 15 min apart
proteinuria + other symptoms / abnormal labs
abnormal labs indicate organ damage
edema
patient can either have BP> 160/110 or the indication of organ damage
HELLP syndrome
PreE with hepatic dysfunction
Hemolysis, Elevated Liver Enzymes, Low Platelets
can occur in women w/o sever HTN or proteinuria
HELLP syndrome is a severe form of preeclampsia characterized by Hemolysis, Elevated Liver enzymes, and Low Platelets due to widespread endothelial injury and microvascular thrombosis that damage red blood cells and hepatic vessels.
Pathophysiology:
Abnormal placentation → endothelial dysfunction → vasospasm and microthrombi → hemolysis, liver ischemia, and platelet consumption.
Clinical features:
Right upper quadrant or epigastric pain
Nausea, vomiting, malaise
Hypertension and proteinuria
Possible complications: DIC, hepatic rupture, renal failure
Danger of HELLP syndrome
1. Liver rupture or hemorrhage
The damaged liver becomes friable (fragile).
Can lead to subcapsular hematoma or even liver rupture, which causes internal bleeding and shock — a medical emergency.
2. Disseminated intravascular coagulation (DIC)
Because platelets are low and clotting factors get consumed, the mother can go into DIC, where the body clots uncontrollably in some places and bleeds elsewhere.
3. Severe bleeding
4. Multi-organ failure
The combination of hemolysis, liver injury, and poor perfusion can lead to renal failure, pulmonary edema, and shock.
5. Fetal risks
Due to placental insufficiency, abruption, or premature delivery, fetal outcomes include growth restriction, hypoxia, and even fetal death.
Eclampsia
seizure activity or coma in a woman with PreE
Before, during after birth
not a specific time when it can happen
Preeclampsia Diagnostic Criteria
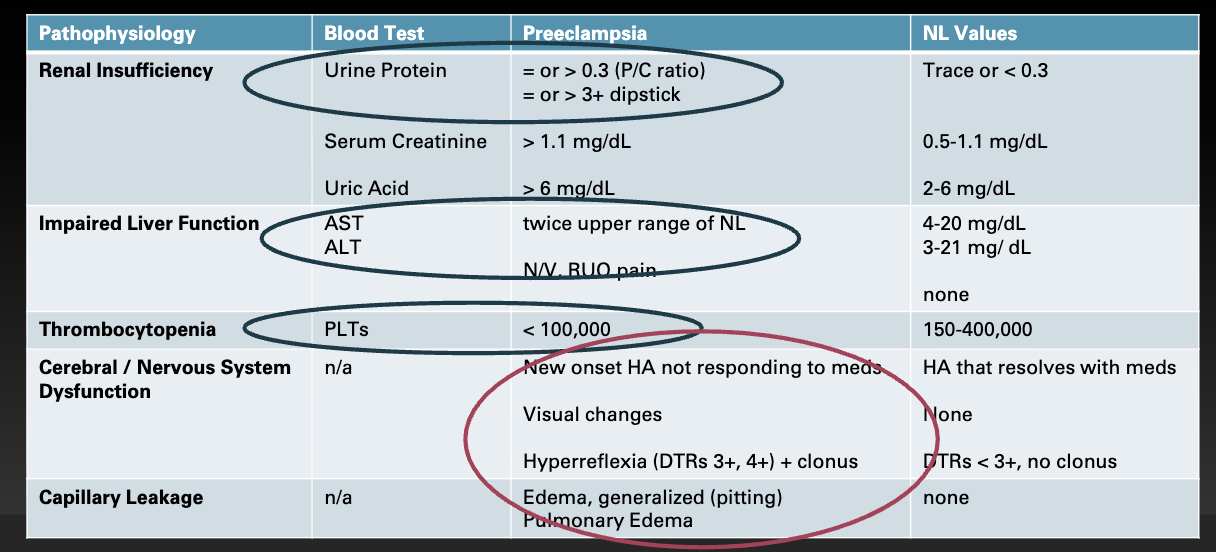
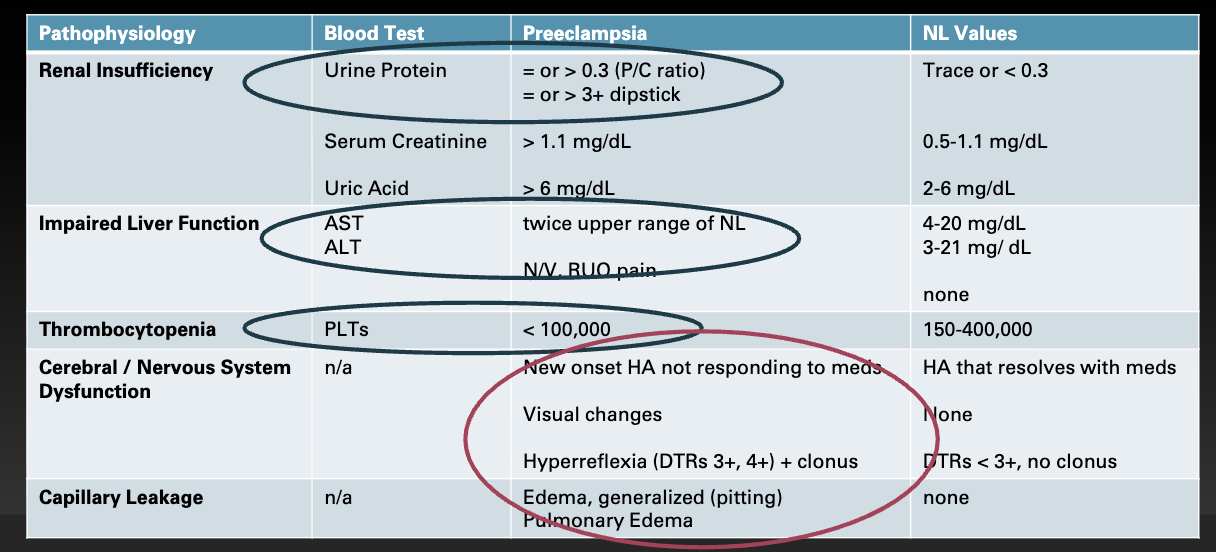
which assessments would you perfomr to identify signs and symptoms of PreE
Edema: especially sudden facial/hand swelling (nonspecific but supportive)
Hyperreflexia or clonus: suggests CNS irritability
Headache, vision changes: warning signs of cerebral involvement
Right upper quadrant or epigastric pain: possible liver involvement
Shortness of breath: pulmonary edema
Dipstick for proteinuria at routine visits.
lab tests you would expect a provider to order
Test | Purpose | Expected Findings |
|---|---|---|
Urine protein (24-hour collection) | Quantify proteinuria | ≥ 300 mg/24 h → diagnostic |
Protein/creatinine ratio | Quicker alternative | ≥ 0.3 → diagnostic |
Urinalysis (dipstick) | Screening | ≥ 1+ protein (if no quantitative test) |
PreE management goals PreE w/o SF
home management reduced activity
PO antihypertensive PRN
delivery goal - 37 weeks +
more frequent assessments
bloodwork
BPs, weigth gain
NST, US
PreE with SF
hospitalization
Delivery Goals
if >37 weeks try expectant management
immediate delivery if uncontrolled BPs worsening labs
i.e. indication of organ damage stoke MI eclampsia, HELLP syndrome
Medications
Magnesium Sulfate
IV antihypertensives - HTN crisis
betamethasone PRN
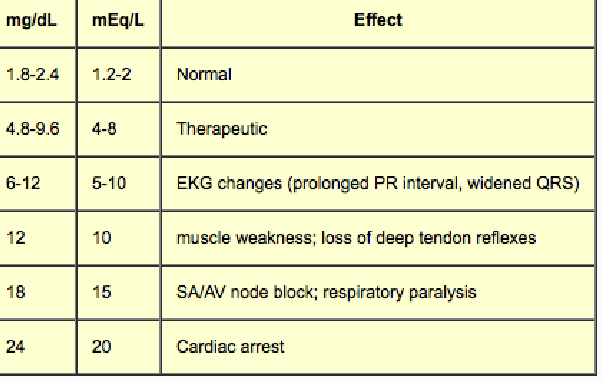
Magnesium Sulfate
Magnesium sulfate is a CNS depressant and smooth muscle relaxant used in pregnancy to prevent or treat seizures in preeclampsia and eclampsia, with careful monitoring due to risk of toxicity.
Prevents / treats seizure activity (is not given to reduce BP)
action: vasodilation, reduce cerebral edema, smooth muslce relaxant
administered via secondary IV infusion
Therapeutic level: 4-7 mg/dl
HIGH Risk medication -
Why It’s High-Risk
Narrow therapeutic window
The dose that prevents seizures is close to the dose that causes toxicity.
Therapeutic serum level: 4–7 mEq/L
Toxic effects start above 8 mEq/L.
Depresses the nervous system
Magnesium is a CNS depressant and smooth muscle relaxant.
Too much can suppress reflexes, breathing, and the heart.
Excreted entirely by the kidneys
If the patient has reduced urine output (as in preeclampsia), magnesium can accumulate quickly → toxicity risk increases.
Requires continuous monitoring
Frequent checks of deep tendon reflexes, respiratory rate, level of consciousness, urine output, and serum magnesium levels are essential.
Magnesium Sulfate normal Side effects and S/S of toxicity
Side Effects
flushing, diaphoresis, burning at IV site
Nausea, fatigue / sedative
neuromuscular relaxant - decreased RR, DTR
Signs and symptoms of Toxicity
RR <12 BPM, O2 sats <95%
UOP <30ml/hr
Decreased LOC, slurred speech (level of consciousness)
Loss of DTRs
If Toxicity supsected —> stop magnesium infusion, notify provider and administer
Calcium gluconate 10% solution
Purpose
Calcium directly antagonizes the effects of magnesium at the neuromuscular junction and restores muscle and respiratory function.
Patho of Magnesium (DO NOT NEED TO KNOW)
Pathophysiology Overview
In preeclampsia and eclampsia, the endothelial dysfunction and vasospasm in the brain cause:
Cerebral edema
Increased excitability of neurons
Reduced blood flow and ischemia
These changes make the brain hyperreactive → leading to seizures (in eclampsia) or risk of seizures (in preeclampsia with severe features).
🧠 How Magnesium Sulfate Works
Magnesium sulfate acts as a central nervous system depressant and smooth muscle relaxant by influencing calcium and acetylcholine activity:
Level | Mechanism | Effect |
|---|---|---|
Neurotransmission | Competes with calcium at the neuromuscular junction → decreases acetylcholine release | ↓ Neuromuscular excitability → prevents seizures |
Cerebral circulation | Causes cerebral vasodilation | ↓ Vasospasm → improved blood flow, ↓ ischemia |
Smooth muscle | Relaxes vascular smooth muscle | ↓ Peripheral resistance → mild BP reduction |
Cell membrane stabilization | Reduces calcium influx into neurons | ↓ Neuronal firing threshold → anticonvulsant effect |
So, magnesium does not treat the hypertension itself — it prevents and controls seizures by calming the nervous system and reducing cerebral irritation.
In summary:
Preeclampsia/Eclampsia patho:
Placental ischemia → endothelial injury → vasospasm → cerebral edema + hyperexcitability → seizures
Magnesium sulfate patho role:
Blocks calcium-mediated neuronal firing + relaxes cerebral vessels → prevents or stops seizures
Key point:
Because magnesium depresses the CNS and muscle activity, high levels can also suppress reflexes, breathing, and cardiac conduction — which is why it’s a high-risk medication requiring close monitoring (reflexes, respirations, urine output, serum Mg levels).
vasospasm (DO NOT NEED TO KNOW)
Vasospasm is the sudden constriction of a blood vessel, which narrows its lumen and reduces blood flow to the tissue it supplies.
PreE Inpatient Interventions
maintain calm non stimulating environment
continous FHR monitoring
Seizure Precautions
suction and oxygen equiptment available and ready to use
educate patient and family
medications -expected side effects, assessment frequency and purpsoe of assessments
notify NICU team
magnesium sulfate can cause respiratory depression in newborn, minila variability during labor, etc
Preterm birht more likely
Antihypertensives
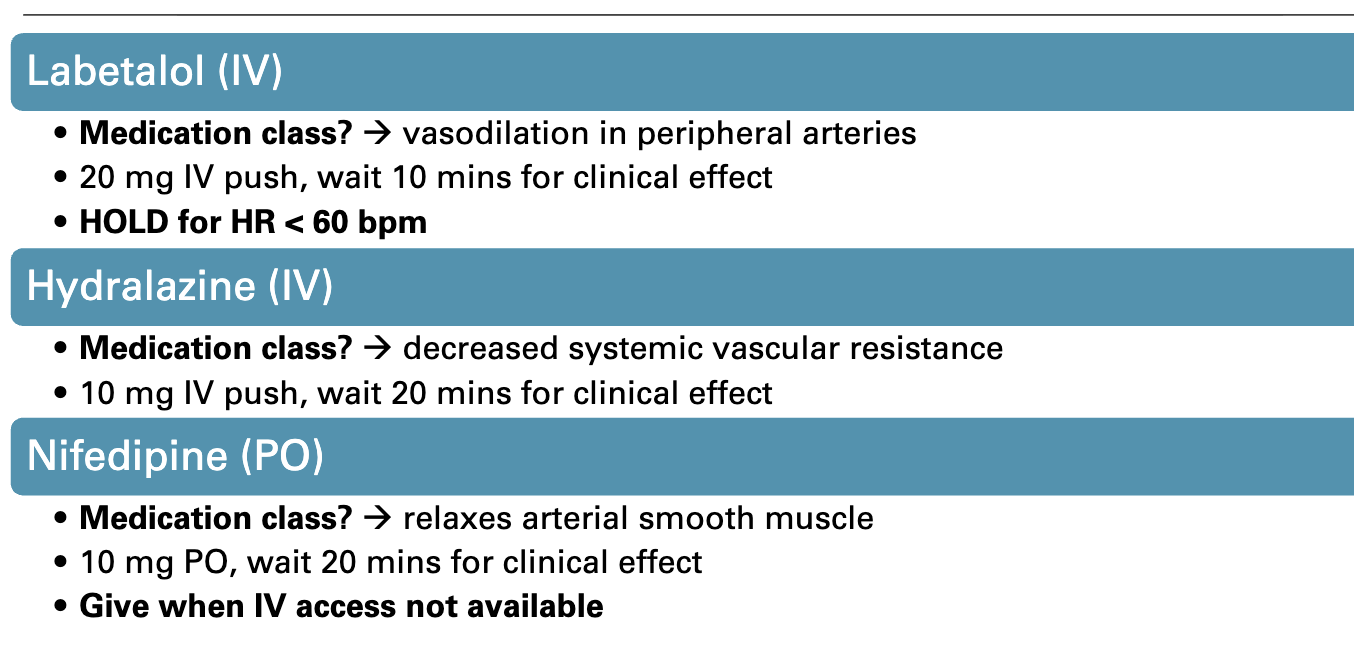
Labetalol (IV)
Beta blocker —> vasodilation in peripheral arteries
20mg IV push, wait 10 min for clinical efects
HOLD for HR <60 bpm
Hydralazine (IV)
Vasodilator —> decreaed systemic vascular resistance
10 mg iv push
Nifedipine
calcium channel blocker —> relaxes arterial smooth muscles
10 mg PO, wait 20 min for clinical effect
Given wehn IV access not available
HTN disorders
continue magnesium sulfate x 24 hrs postpartum
monitor BP x12-24 hrs after magnesium is stopped
schedules PO antihypertensives
discharge teaching if prescriptions to be used at hom
You want to make sure blood pressure can be managed just with PO medications in a healhty range
Eclamspia
Eclampsia is the most severe form of preeclampsia, characterized by the onset of seizures (or sometimes coma) in a woman with preeclampsia that cannot be attributed to another cause.
prioritize airway and safety
side rails up, pad if able, turn to side
remain at bedside, call for help, note time
Post convulsion
assess ABC’s
suction, oxygen, bag-mask if not breathing
IV access - magnesium sulfate 1st lin
lorazepam (ativan) 2nd line if seizures continue
confusion combative, coma - common,
fetal uterine status (if pregnant
Utuerus Hypercontractile hypertonic
fetus - bradycardia, late deceles minimal absent variability.
management of PreE with baby below GA
Maternal Stabilization
If severe features:
Seizure prophylaxis: Magnesium sulfate
Blood pressure control: IV hydralazine, IV or oral labetalol, or oral nifedipine
Monitor: Vitals, reflexes, urine output, labs (CBC, LFTs, creatinine, urine protein)
If mild:
Close monitoring inpatient or outpatient, depending on resources
Serial BP checks and labs
Education on warning signs: headache, visual changes, RUQ pain, decreased fetal movement
Fetal Assessment
Ultrasound: growth, amniotic fluid, Doppler
Nonstress test / biophysical profile for viability and well-being
Timing of Delivery
Definitive treatment = delivery, but timing depends on gestational age (GA) and maternal/fetal status:
GA / Scenario | Approach |
|---|---|
< 34 weeks & maternal/fetal stable | Expectant management: |
Hospitalization
Daily maternal labs
Fetal surveillance (NST, BPP)
Corticosteroids for fetal lung maturity (betamethasone or dexamethasone)
Magnesium sulfate for seizure prophylaxis |
| ≥ 34 weeks or maternal/fetal deterioration | Delivery (usually induction or cesarean if unstable) |
| Severe maternal compromise at any GA | Immediate delivery, regardless of GA |
Supportive Measures
Bed rest is not strongly recommended, but activity may be limited
Fluid management: avoid overload (risk of pulmonary edema)
Treat complications (HELLP, DIC, renal failure) as needed
Summary
Mild preE <34 wks: Expectant management + close monitoring + corticosteroids
Severe preE or deterioration: Immediate stabilization → delivery, regardless of GA
Always protect the mother first; prolong pregnancy only if safe
Early pregnancy Bleeding
Spontaneous abortion (miscarriage)
pregnancy ends naturally <20 weeks
25% of pregnancies
Cervical insufficiency
cervical dilation without clear cause
leads to preterm birth in 2nd trimerster
ectopic pregnancy
fertilized Ovum implants outside of the uterus
3% of pregnancy related maternal deaths
spontaneous Abortion (SAB) aka Miscarriage
There are multiple types of textbooks 28.1 pg 601
Symptom:s Bleeding (light to heavy)
cervical dilation
uterine cramping (none to severe)
Management
75% are expectant management
allow the body to do its thing instead of intervening
Medical
usally prostagalndins - misoprostol
surgical management if products not passed completely
surgical
dilation and Curettag (D&C)
Dilation and Curettage (D&C) is a surgical procedure used to evacuate the contents of the uterus. In obstetrics and gynecology, it’s commonly performed for spontaneous abortion, missed abortion, retained products of conception, or abnormal uterine bleeding.
post op oxytocin and other uterotonics
epidural or sedation intra-op, NSAIDS post op
no sex tampos for 2 weeks
grief counseling
cervical insufficiency
determine cause: is it weak cerivcal tissue or early signs of preterm labor
considered to have genetic component
Diagnosis
US to assess cervical length (<25mm)
ultrasound (US)
Speculum exams to identify dilation
symptoms
painless and passive cervical dilation
management of cervical insufficiency
management
cervical cerclage
suture through around external OS
opening of cervix
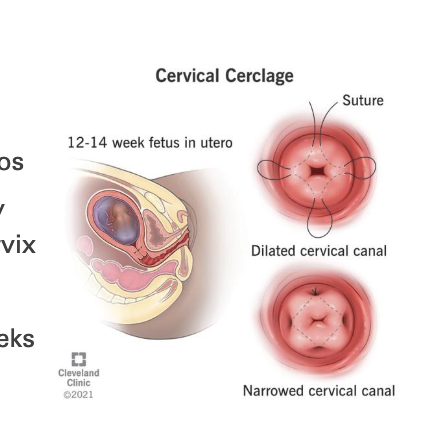
ca be prophylactic due to OB history or treatment in respone to short cervix
placed between 12-23 weeks
removed for PTL SROM or at 36 weeks
Progestorone
route IM or vaginal
starts at 16weeks ends at 36
reduces preterm nirth by 30
ectopic pregnancy
implantation of a fertilized ovum outside the endometrial lining of the uterus
Location | % of cases |
|---|---|
Fallopian tube (most common) | ~95% |
— Ampulla | 70% |
— Isthmus | 12% |
— Fimbrial end | 11% |
Other sites (rare) | Ovary, cervix, abdomen, C-section scar |
Risks: hemorrhage, sever fetal malformations
Symptoms:
abdominal pain (dull ache —> sharp stabbing pain)
delayed menses
abnormal vaginal bleeding
if rupture —> shock, cullen sign, referred pain
cullen sign: Cullen sign = bluish discoloration around the umbilicus (belly button) caused by subcutaneous intraperitoneal bleeding that tracks along the fascial planes.
management and education of ectopic pregnancy
Management
Mthotrexate (IM injection) - early treament
destroyes rapidly dividing cells
prodicts of conception reabsorbed by body within 4-6 weeks
Surgical treatment
depends on severity
salpingectomy could be needed if ruptured
Salpingectomy = excision (removal) of a fallopian tube.
Education
no analgesics stronger than acetaminophen (mask s/s rupture)
notify proivder when prefnant again - risk for another ectopic
grief or infertility support groups PRN
Late pregnancy bleeding
placenta previa and placental abruption
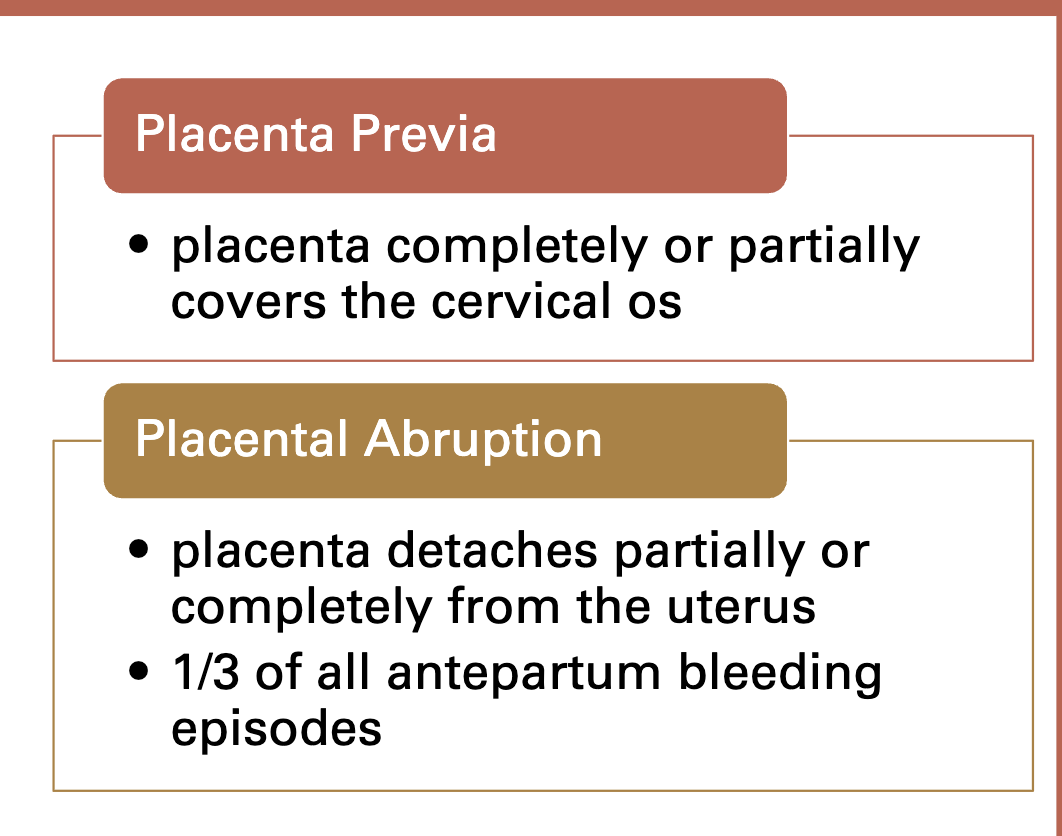
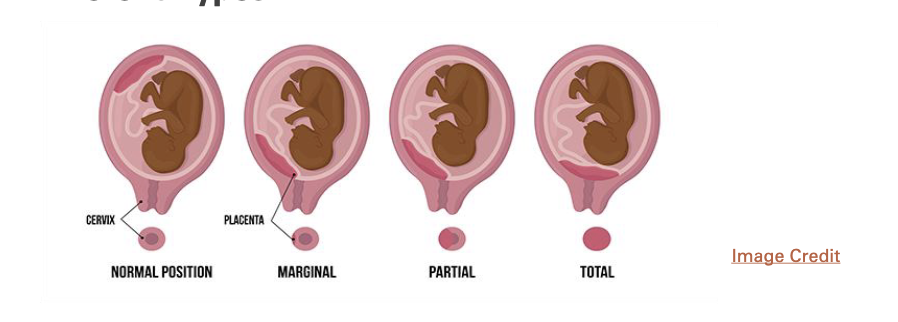
placenta previa
is a condition where the placenta implants low in the uterus and partially or completely covers the cervical os (the opening of the cervix).
Risk factors: previous c/s, AMA(advanced maternal age), multiparity, D&C (dilation and curretage), smoking\
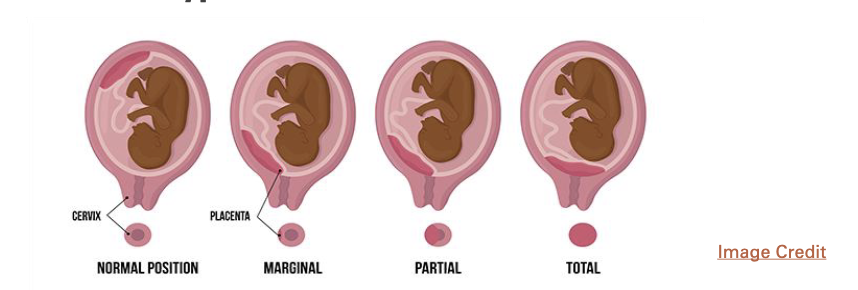
symptoms
painless, bright red vaginal bleeding
VS may be WDL
soft nontender abdomen with NL uterine tone
FHR may be WDL until sever detachment
Feature | Previa | Abruption |
|---|---|---|
Pain | None | Present |
Bleeding | Bright red | Dark red |
Uterus | Soft | Rigid/tender |
Fetal distress | Rare | Common |
Delivery | C-section | Often urgent |
Concerns
management of placenta previa
all pateints with painless vaginal bleeding - assume previa until proven otherwise
expectant management <36 weeks
1st bleeding episode —> and observatoin
2nd/3rd bleeding episode —> hospitalized
active managemetn >36 weeks
concerns about maternal fetal well - being —> delivery regardless of GA
C-section delivery
increased risl of hemorrhage immediately after birth
always give Cesearan cannot deliver placenta before baby
placental abruption
is when the placenta separates prematurely from the uterine wall before delivery.
Risk factors:
HTN disorder, drug use, (meth or cocain), truama, hx of abruption, smoking, PPROM(Preterm Premature Rupture of Membranes.)
Symptoms
vaginal bleeding,
abdominal pain
uterine tenderness - localized to specific region
contractions - usally requent (blood irritates uterus)
fetal distress with increased detachment
table
Feature | Previa | Abruption |
|---|---|---|
Pain | None | Present |
Bleeding | Bright red | Dark red |
Uterus | Soft | Rigid/tender |
Fetal distress | Rare | Common |
Delivery | C-section | Often urgent |
management of placental abruption
depends on blood loss and fetal maturity / status
expectand management < 36 weeks
if mother and fetus are stable
additional antepartum testing (NST,BPP)
active management
if GA > 36 weeks or there are signs of compromise
vaginal birth (if possible or cesarean)
closely observe VS, FHR, clotting factors, H&H (hemoglobin and hematocrit
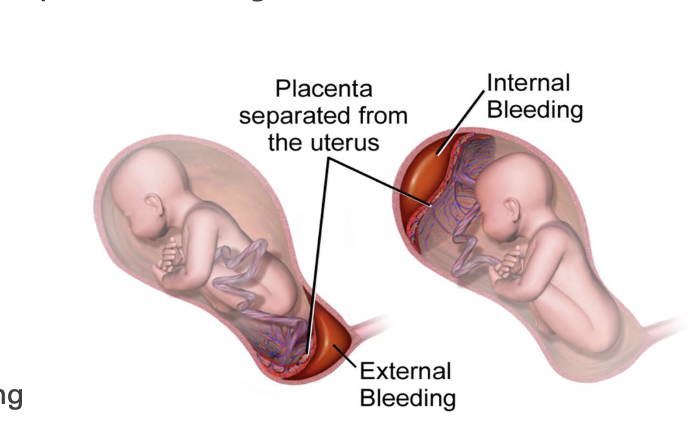
Metabolic adaptations in pregnancy
glucose corsses placenta
maternal glucose levels = fetal glucose levels
insulin does not cross
diabetogenic effect
caused by placental homrones
increased glucose production
insulin resistance decreases -
this means If insulin resistance decreases, it means the body’s cells are more sensitive to insulin again.
So glucose moves into the cells more easily, and blood glucose levels drop.
This can happen:Early in pregnancy, when maternal metabolism is still geared toward storing nutrients.
After delivery, when the placenta (and its hormones) are gone, and insulin sensitivity returns to normal.
Summary:
Insulin resistance ↑ → more glucose for baby (normal in late pregnancy).
Insulin resistance ↓ → more glucose taken up by mom’s tissues, less available for baby.
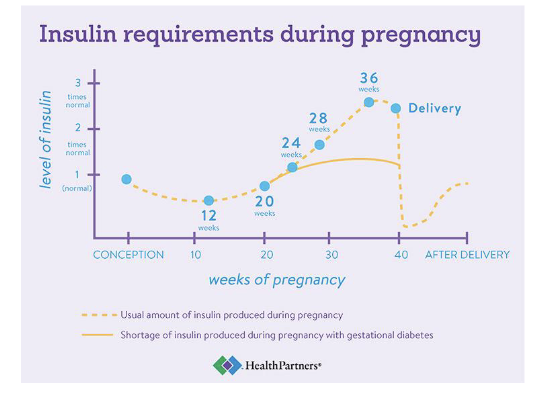
diabetes Mellitus
occurs in about 6-7% of pregnancies
90% of those are GDM
hyperglycemic state
Main types
type 1` DM
Type 2 DM
Gestational diabetes (GDM)
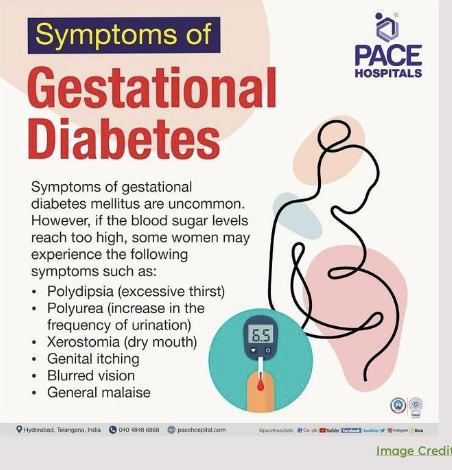
Gestational Diabetes (GDM)
glucose intolerance that develops during pregnancy
increased risk of
miscarriage
macrosomia / LGA infant
neural tube defect
disproportionate chest / shoulder size
polydramnios
preeclampsia
ketoacidosis (DKA)
infection
what test is used to diagnose GDM
Two-step approach (most common in the U.S.):
Step 1 – 50 g Glucose Challenge Test (screening):
No fasting required.
Blood glucose checked 1 hour after drinking 50 g of glucose.
If ≥130–140 mg/dL, proceed to step 2.
Step 2 – 100 g OGTT (diagnostic):
Done after overnight fasting.
Blood glucose measured fasting, 1 hr, 2 hr, and 3 hr after drinking 100 g glucose.
Diagnosis: If 2 or more values are above thresholds (e.g. Carpenter-Coustan criteria).
Time point
Normal / Cutoff
Fasting
≤95 mg/dL
1 hour
≤180 mg/dL
2 hour
≤155 mg/dL
3 hour
≤140 mg/dL
Gestational Diabetes (GDM)
normal levels
premeal = 60-95 mg/ dl
postprandial <140 mg/dl
Post” = after
“Prandial” = related to eating or a meal
classifications
A1 GDM - diet controlled
A2 GDM - controlled with meds / insuling
diabetes management
monitor blood glucose 4x daily
lifestyle modifications
diet
count carbohydrates 2-3 snacks a day
dont skip meals or go w/o food > 4 hours
excerisze
monnitor for hypoglycemia, increase carbs / snacks
medications
insuling - type depends on blood glucose levles
oral hypoglycemics (metformin)
decrease glucose production and increases insulin sensitivity
good alternate option to insulin
Nursing interventions for GDM antepartum
antepartum care
ultra sound to monitor fetal growth and AFI (amniotic fluid index)
this is important because High maternal blood glucose can lead to fetal hyperglycemia → increased fetal urine output, causing polyhydramnios (too much amniotic fluid).
GDM can also cause macrosomia (large baby) and growth abnormalities.
ing
Nursing interventions for GDM intrapartum
blood glucose q1-2 hours
hypoglycemia < 70 mg/dl
signs and symptoms: palpitations, tremors (shakiness), hunger, headache, confusion, fatigue, blurred vision, seizure (severe)
treatment: glucose gel, juice, sugar / if unconscious, Iv infusion (D5LR or D5NS) of glucose
Nursing interventions for GDM postpartum
insulin requirements drop
blood gluces levels PRN
A1 GDM - serum leevels or no checks
A2 GDM - continue fasting and PP
blood glucose at PP appoiuntment -
women who had GDM are at higher risk of developing GDM later in life
purpose is to ensure levels have gone back to normal
typically 75mg test done 6 to 12 weeks PP
HCG
stands for human chorionic gonadotropin — a hormone produced by the placenta after implantation.
Quick facts:
Maintains the corpus luteum, which keeps producing progesterone to support early pregnancy.
Detected in blood and urine — the basis of pregnancy tests.
Normally rises rapidly in early pregnancy and then levels off.
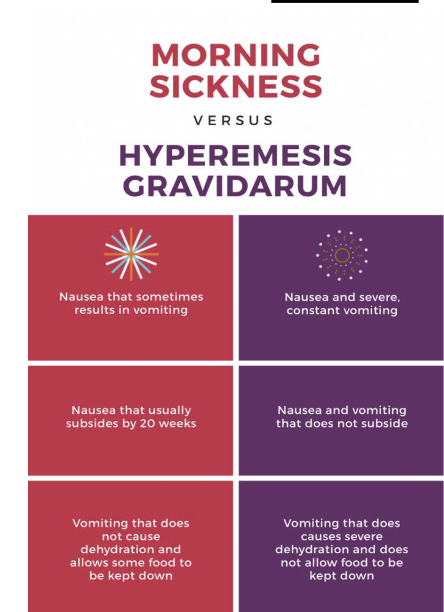
Hyperemesis Gravidarum
excessive vomiting —> weight loss, electrolyte imbalance, dehydration
causes - rising HCG, relaxation of the GI tract
2-3% of pregnancies/ is rare more severe than morning sickness
Treatment
medications
pyridoxine (Vit B6) + doxylamine (unisom)
Prescriptions - ondansetron (Zofran)
IV therapy - fluid replacement
slow diet progression when vomiting stops
dry, balnd, low-fat, high-protein foods
ginger - tea, lozenges, soda
Usually begins: around 4–6 weeks of gestation
Peaks: 8–12 weeks of gestation
Usually improves/resolves: by 16–20 weeks
In rare cases, symptoms may persist beyond 20 weeks.
Anemia in pregnancy main risks / concerns
hemoglobin < 11mg/dl in 1st or 3rd trimester
reduction in oxygen carrying capacity
Main Risks / Concerns
Maternal risks:
Fatigue, weakness
Increased risk of infection
Preterm labor or postpartum hemorrhage
Poor tolerance to blood loss during delivery
Fetal risks:
Low birth weight
Preterm birth
Fetal growth restriction (IUGR)
Stillbirth (in severe, untreated cases)
Anemia in pregnancy common symptopms and types
Common Symptoms
Fatigue, dizziness, or fainting
Pale skin or mucous membranes
Shortness of breath
Rapid heartbeat (tachycardia)
Headache
Types
Iron deficiency
Folic acid deficiency
sickle cell
thalassemia
Iron deficiency anemia
most common anemia (75%)
serum ferritin < 12 mcg/ L + low Hgb < 11g/dl
pregnany body will ensure fetal iron stores are adequate
treatment
iron supplements
PO - 325 mg daily
Constipation (most frequent)
Nausea or upset stomach
Abdominal cramping
Dark or black stools (harmless, expected)
Metallic taste in mouth
IV - Venofer
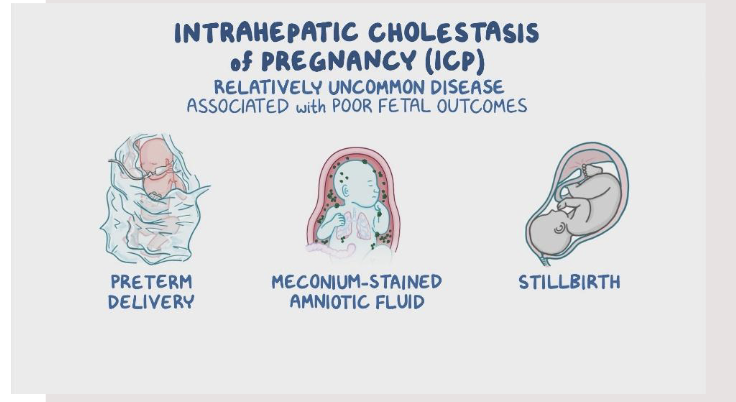
cholestasis
liver condition where bile flow is reduced or blocked, causing bile acids to build up in the blood.
occurs in pregnancy
cause is unknown
Symptoms
Severe itching (pruritus) — especially on palms and soles, worse at night
Dark urine
Pale or clay-colored stools
Jaundice (yellowing of skin/eyes) — in some cases
Fatigue or malaise
Loss of appetite or nausea (sometimes)
diagnostics of Cholestasis
Bile Salts (or Bile Acids)
Bile acids are made in the liver to help digest fats.
In cholestasis, bile can’t flow properly, so bile acids build up in the blood.
Measuring serum bile acids is the most specific test for intrahepatic cholestasis of pregnancy (ICP).
↑ Elevated bile acids confirm the diagnosis.
LFTs (Liver Function Tests)
These are blood tests that measure how well the liver is working.
Key ones include:
ALT (Alanine aminotransferase)
AST (Aspartate aminotransferase)
Alkaline phosphatase (ALP)
Total and direct bilirubin
In cholestasis:
ALT and AST are elevated (liver irritation/damage)
Bilirubin may also rise if bile flow is severely impaired
fetal risk and treatment of cholestasis
Because bile acids build up in the mother’s blood, they can cross the placenta and affect the baby.
IOL at 37 weeks close monitoring otherwise
treatment
Ursodeoxycholic acid (ursodial)
monitor lab trends (bile salts
antihistamine prn - diphenhydramine (benadryl)
itching management —> cool baths, oatmeal, products, topical creams
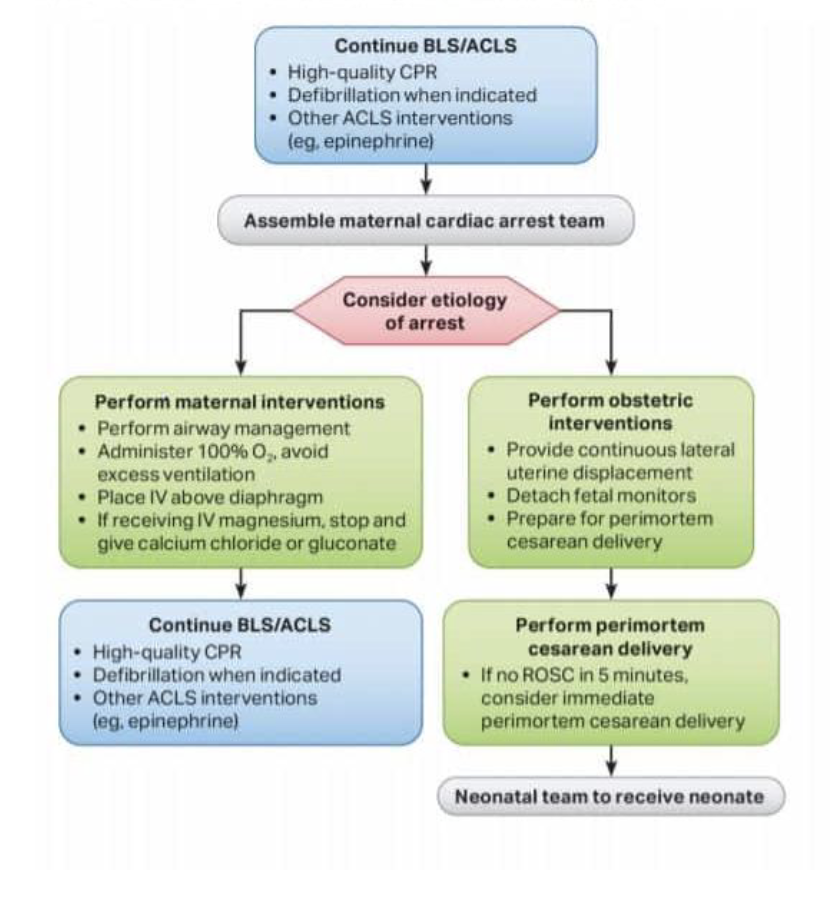
cardiopulmonary resuscitation (CPR) for pregnant patient
1 in12,000 women admitted for L7D care in us suffer from cardiac arrest
women 27% less likely to receive CPR than men even more so for pregnant women
Main distinctions for CPR with pregnant women
defribilation pads slightly higher
more difficult airway
first concern = resuscitate and stabilize mother
Displace the uterus to the left to protect the aorta and allow blood to flow
Perimortum c-section
for fetus >23 weeks
decision within 5 minutes
CPR basics - CAB
Chest Compression Rate
100–120 compressions per minute
Compression-to-Breath Ratio
30 compressions : 2 breaths
(for both 1- and 2-rescuer adult CPR)
Pulse Check
Before starting CPR: Check for ≤ 10 seconds
During CPR: Check pulse every 2 minutes (or after 5 cycles of 30:2)
Each pulse check should last ≤ 10 seconds
AHA algorithim
Perinatal modd disorders
commen and underreported
perinatal depression affects 1 in 7 women
set of disorders that can occur during pregnancy or within 1 year postpartum
depression
anxiety
postpartum psychosis
Depression (MDD) (major depressive disorder)
Diagnosis : at least 5 symptoms within a 2 week period
Depressed mood (spontaneous crying)
Diminished interest in all activities
Insomnia or hypersomnia
Increase/ decrease in weight
Fatigue/ loss of energy
Psychomotor agitation
Feeling worthless/ overly guilty
Diminished concentration
Suicidal ideation
increased risk for postparum depression
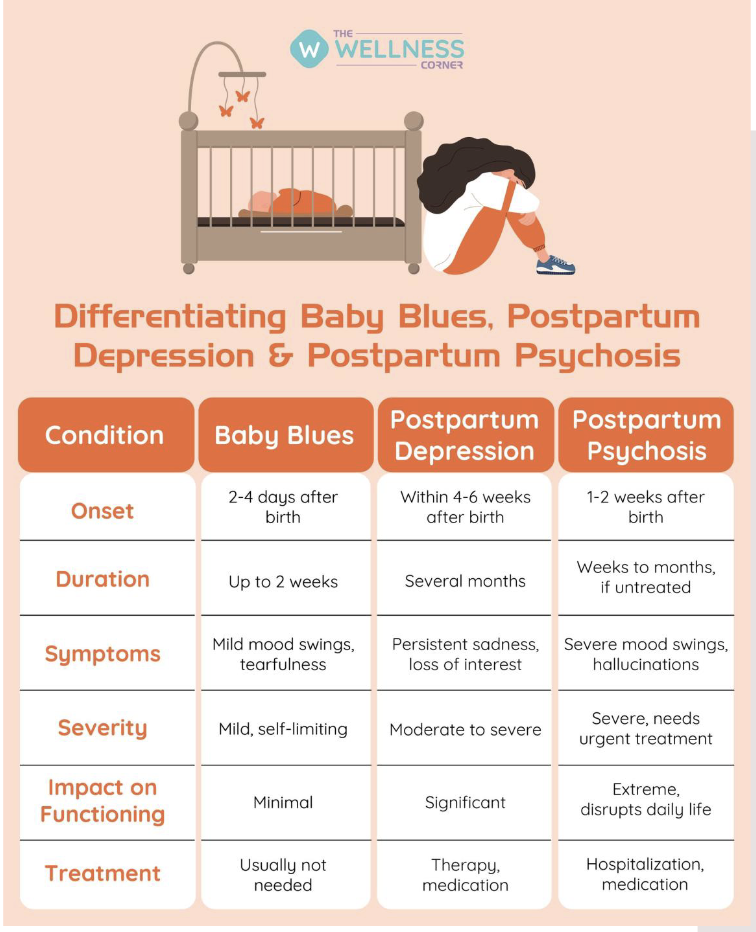
Postpartum depression Baby blues
baby blues - 50-70 percent of women
breif period of depressive symptoms
resolves in 2 weeks
symptoms
Baby blues are mild, short-term mood changes that many women experience after childbirth — usually due to hormonal shifts, fatigue, and emotional adjustment.
Common Symptoms (Mild and Temporary)
Mood swings
Tearfulness or crying easily
Irritability or anxiety
Feeling overwhelmed
Trouble sleeping (even when the baby sleeps)
Difficulty concentrating
Mild loss of appetite
Postpartum depression
9-24 percent of women
major depressive disorder w/o psychosis
lasts >2 weeks
potential causes: major hormone shifts, nutritional deficiencies, genetics
History of anxiety or depression is biggest risk factor
symptoms are same as MDD
perinatal depresion management
psychotherapy - first choice
antidepressants if needed
risk vs benefit analysis done by providers
selective serotonin reuptake inhibitors (SSRI’s)
Escitalopram (Lexapro), Sertraline (Zoloft)
brexanalone (Zulresso)
1st FDA approved medication for treatment of PPD
inpatient via iv infusion due to needs for close monitoring
PPD interventions
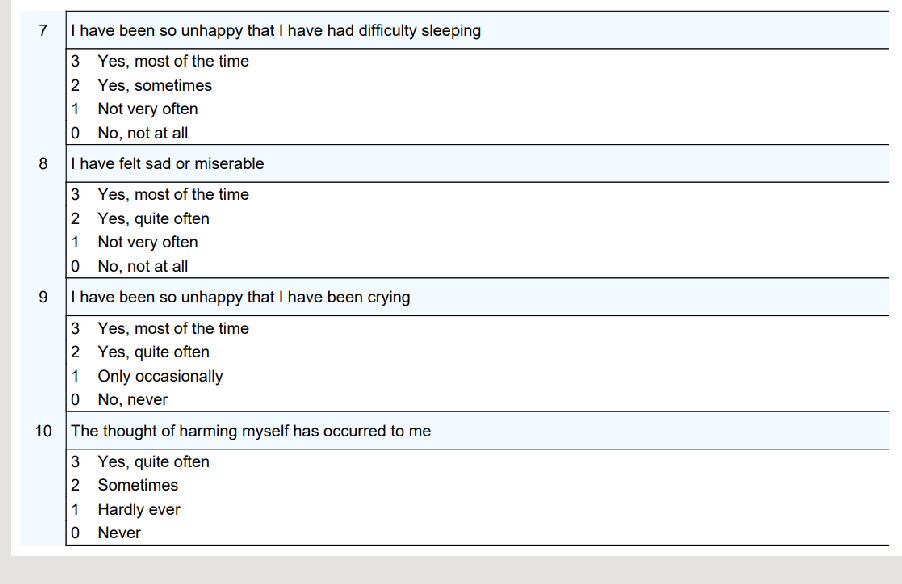
Screening
edinburgh postnatal depression screen
scores > 13 need further assessment
suicide statement positive require follow up
Promote rest / resolve sleep deprivation
4-5 hours of uninterrupted sleep
social support
encourage participation in newborn care
encourage aerobic excersize as able
postpartum psyuchosis
commonly associated with bipolar disorder
manifests within first 2-4 weeks
symptoms
Severe confusion or disorientation
Delusions (false beliefs — e.g., believing the baby is evil or in danger)
Hallucinations (hearing or seeing things that aren’t there)
Extreme mood swings — mania or severe depression
Agitation, restlessness, or insomnia
Paranoia or irrational thoughts
Poor judgment and inability to care for self or baby
Thoughts of harming self or the baby
This is a PSYCHIATRIC EMERGENCY
high risl of suiced and infanticide
treatment
inpatient psych care
antipsychotics, mnood stabilizers benzodiazepoines
supervized visits with baby
differentiating baby blues, postpartum depression and postpartum psychosis
anxiety disorders
10% of women
symptoms impair functioning
hx of anxiety or depression is most prominent risk factor
management
1st line psychotherpay
pharmocoligc
antidperessants
benzodiazepiens for short term anxiety

anxiety disorders (GAD)
generalized anxiety disorder (GAD)
excessive pervasive worry, restlesness difficult concnetratin
often overly worried about their infant
anxiety disorders, panic attacks, panic disorder
rapid onset of fear with symptoms of palpitations, sweating, SOB, dizyy, numbness / tingling in hands, hot flashes, fear of losing control or dying
anxiety disorder PTSD
due to serious injury (or risk of), threat of death or sexual violence
also r/t difficult or traumatic birth —> next labor / brith could be triggering
involuntary memories, flashbacks, nightmares, insomnia, angry outburst, irritability
Nursing interventions for anxiety disorders
education at discharge - teaching for self maangement
validated screening tools
initiating convo -
how are you feeling,
how are thing with the baby
if signs and symptoms are present notify provider
empower partner to help
substance use disorder
chemical dependency
warning signs
limited late or no prenatal care
sporadic appointments
poor nutrition
risk to fetus
ectopic pregnancy
FGR / IUGR
Intrauterine Growth Restriction, Fetal Growth Restriction
LBW infant
preterm birth
abruption
death
preeclampsia
physcial malformations
SUD screening
universal screening
validated tools
non judgemental approach
alone is best
4 Ps SUD screenign
Parents
did a parent have problems with alchohol / drugs
partner
does partner have a problem with alchohol / driugs
past
have you ever had beer win liqoure
pregnancy
in the month before pregnancy how many cigarettes did you smoke / alchohol did you consume
state laws regarding Tox screening
SUD interventions
collabertaive interdisciplinary approach
abstinence recommended
pregannyc is often great motivator for lifestyle change
support groups
medication assisted treament
therapy
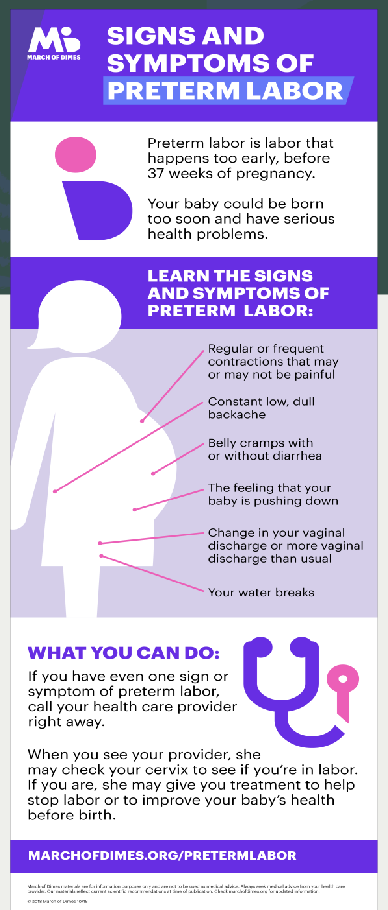
Preterm labor (PTL)
regular contractions in a person who is <37 weeks GA
about 10% babies are preterm
Risk Factors
History of preterm labor or birth
genetics
recurrent UTI’s
IVF pregnancy
smoking, drug use
uterine anomaly
low socioeconomic status
late entry to care
black race
Preterm labor signs and symptoms and management
signs and symptoms
low uterine back pain
low back present at any GA but can be written off in early GA
regular contractions
pelvic pressure
change in vaginal discharge
(SROM)
Regular contractions
Painful or rhythmic low back pain
Fluid or bleeding + pelvic pressure
Diagnosis
symptoms, vervical change, fetal fibronectin
management
treat cause (ex cervical insufficiency —> Vaginal progesterone
inpatient observatoin at a hospital equipped to manage that GA
limit activity and work, (less working on feet)
pelvic rest
if body wants to deliver baby nothing can really be done
medications for PTL
magnesium sulfate
terbutaline
nifedipine
glucocorticoids
magnesium sulfate
Medication | Route | Indication / Purpose | Side Effects / Nursing Considerations |
|---|---|---|---|
Magnesium sulfate | IV infusion 4 g loading dose, then 1–2 g/hr | - Neuroprotection for fetus <32 wks (↓ risk of cerebral palsy) - Can provide mild tocolysis | SE: flushing, warmth, nausea, vomiting, muscle weakness, ↓ DTRs, respiratory depression, pulmonary edema NC: monitor RR, DTRs, I/O, urine output >30 mL/hr; have calcium gluconate at bedside; caution with nifedipine; monitor for magnesium toxicity |
terbutaline
Terbutaline (beta-2 agonist) | 0.25 mg Subcutaneous injection | Short-term tocolysis (used to temporarily stop contractions) | SE: tachycardia, palpitations, tremors, anxiety, hyperglycemia, hypotension; can cause fetal tachycardia NC: hold if maternal HR >120; avoid in cardiac disease; monitor maternal & fetal HR |
Medication | Route | Indication / Purpose | Side Effects / Nursing Considerations |
|---|---|---|---|
nifedipine
Nifedipine (Procardia) (Ca channel blocker) | 10–20 mg PO, 2–3× daily | Longer-term tocolysis (reduces uterine contractions) | SE: hypotension, headache, flushing, dizziness NC: check BP before giving; use caution if also on magnesium sulfate (risk of hypotension); avoid with grapefruit juice |
Medication | Route | Indication / Purpose | Side Effects / Nursing Considerations |
|---|
gluucocorticoids
Medication | Route | Indication / Purpose | Side Effects / Nursing Considerations |
|---|
Glucocorticoids (Betamethasone or Dexamethasone) | IM injection, 2–4 doses, 12 hrs apart | Accelerate fetal lung maturity; reduce risk of RDS, IVH, NEC | SE: hyperglycemia, injection site pain, decreased fetal movement for 72 hrs NC: monitor maternal blood glucose (especially in diabetics); given between 24–34 weeks; best effectiveness if birth occurs 24 hrs–7 days after completion |
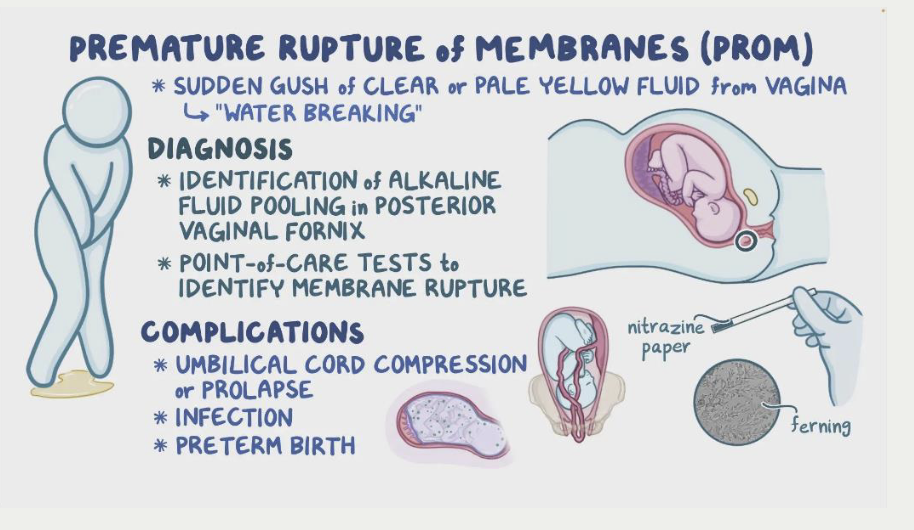
Preterm pre-labor rupture of membranes (PPROM)
Rupture of membranes before labor begins and less than 37 weeks
symptoms
sudden gush or slow leak of fluid
can feel like peeing without control
Diagnosis
symptoms, obvious presence of fluid, amniotic fluid test
primary complication
infection
management
between 34-37 weeks —> delivery
less than 32 weeks, expectant management
hospitalized, routine monitoring with NST
magnesium sulfate glucocorticoids
antibioitcs x7 days - ampicillin, amoxicillin or erythromycin
intrauterine infection OR Chorioamnionitis (chorio)
infection of the amniotic fluid, fetal membranes (chorion and amnion), and sometimes the placenta
Risk factors
long labor
prolonged ROM
multiple cervical exams
internal monitors (FSE, IUPC)
Meconium-stained fluid
Maternal risk: sepsis, dysfunction labor
Neonatal risk: infection respiratory distress, death
intrauterine infection OR Chorioamnionitis (chorio) symptomd and treatment
symptoms
fever greater than 38C or 100.4 F indicates infectino
uterine tenderness
elevated WBC above 14
foul smelilng amniotic fluid
Fetal tachycardia
mother tachycardia
Treatment
IV antibiotics
acetaminiphen for fever
cool down maternal body - ice, remove layers, education
blood cultures and lactate levels
Vaginal delivery is still preferred
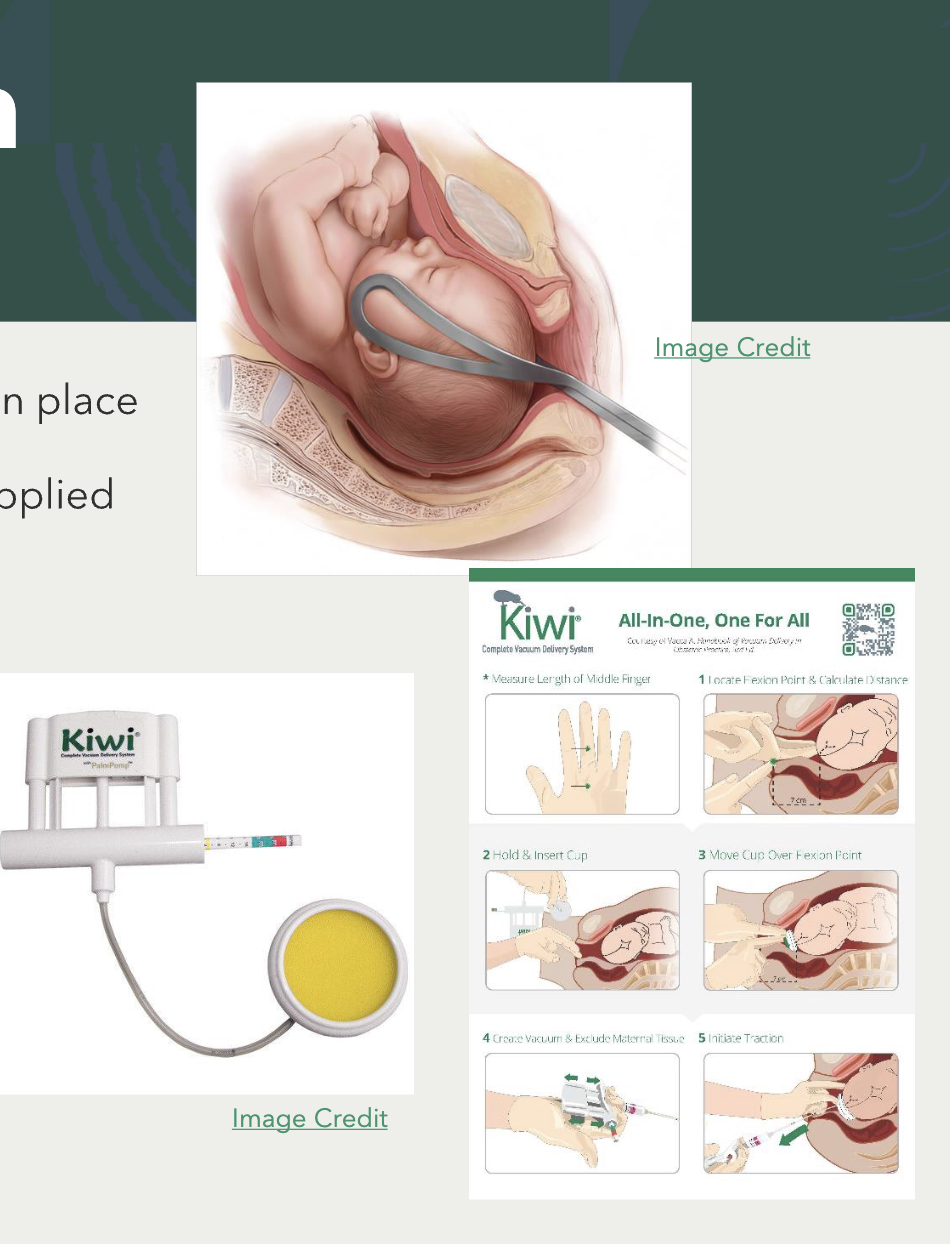
operative vaginal birth
a vaginal delivery assisted with an instrument, either forceps or a vacuum extractor, to help guide the baby out when the mother alone cannot complete the delivery safely or quickly.
MD only —> must obtain consent
indications
prolonged second stage of labor (> 2 hours)
maternal exhaustion or cardiopulmonary disease
fetal compromises
criteria for success
ROM
cervix 10cm dilated
presenting part engaged (i.e., 0 station)
operative vaginal birith forceps and vacuum
forceps
2 curved blades that fit around baby’s ears and lock in place
vacuum
vacuum cup attaches to fetal head and pressure is applied
MD provides traction with maternal pushing efforts
maternal complications
vaginal/cervical lacerations
hematoma
fetal complications
cephalohematoma
can lead to jaundice and anemia
face /scalp lacertaions or bruises
can cause nerve damage
facial palsy
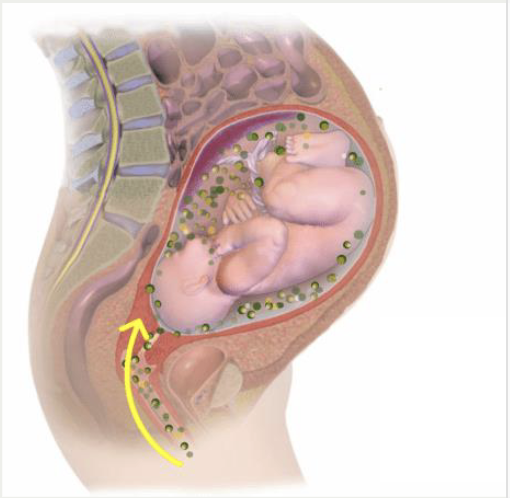
shoulder dystocia
occurs when, after the fetal head is delivered, one or both shoulders get stuck behind the maternal pubic symphysis, preventing the rest of the baby from being delivered spontaneously.
This is an obstetric emergency because the baby can suffer from hypoxia if delivery is delayed.
Usually occurs after head delivery but before the body comes out.
risk factors
large for GA baby
diabetes
maternal complications
3-4th degree lacertaion
postpartum hemorrhag
fetal complications
fractures clavicle / humerus
brachial plexus nerve injury
asphyxia / death
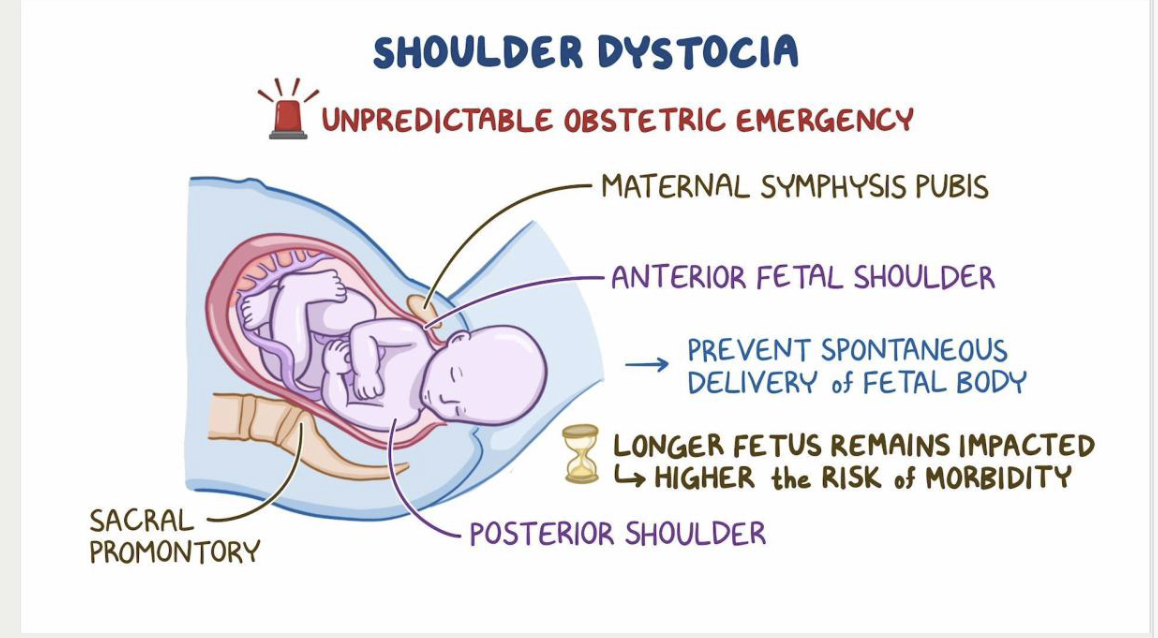
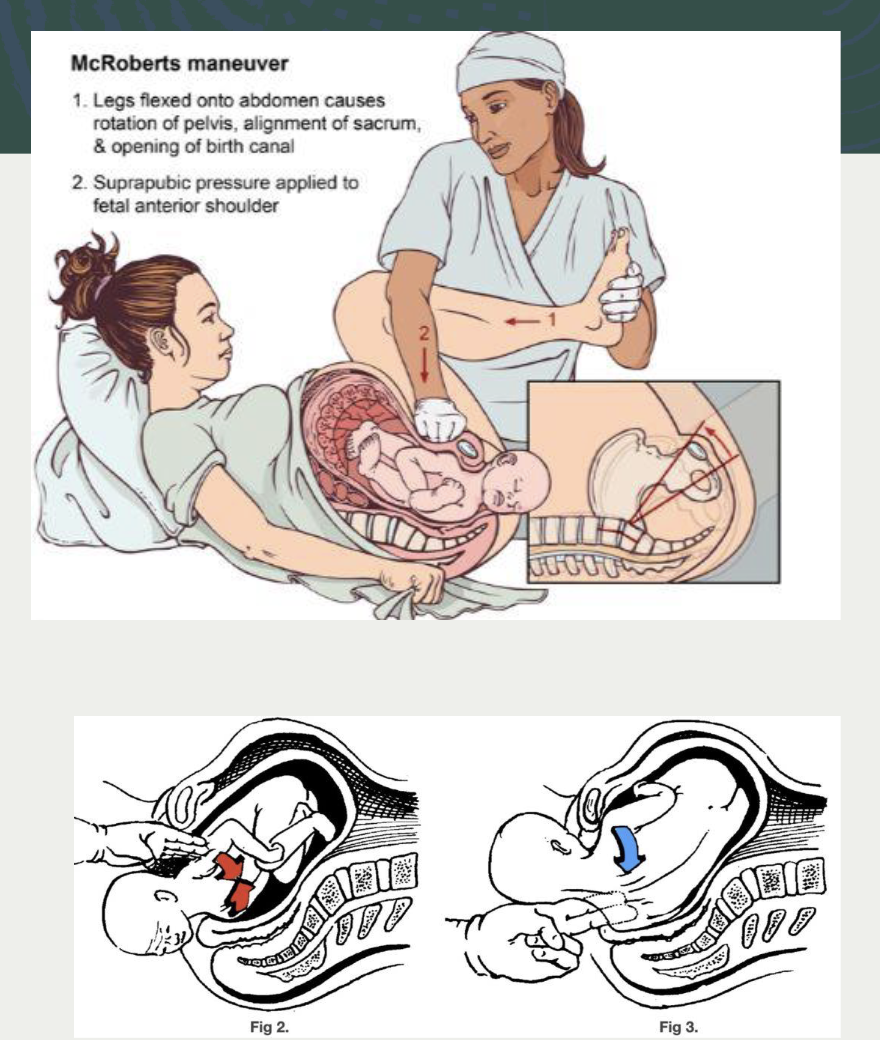
management of shoulder dystocia
The provider should identify the shoulder
RN notes the time / starts a timer
RN calls for extra assistance STAT
labor and delivery team
NICU
neonatal team
maybe anesthesia if needed
1st line
McRobert’s maneuver and suprapubic pressure
2nd line
hands and knees or posterium
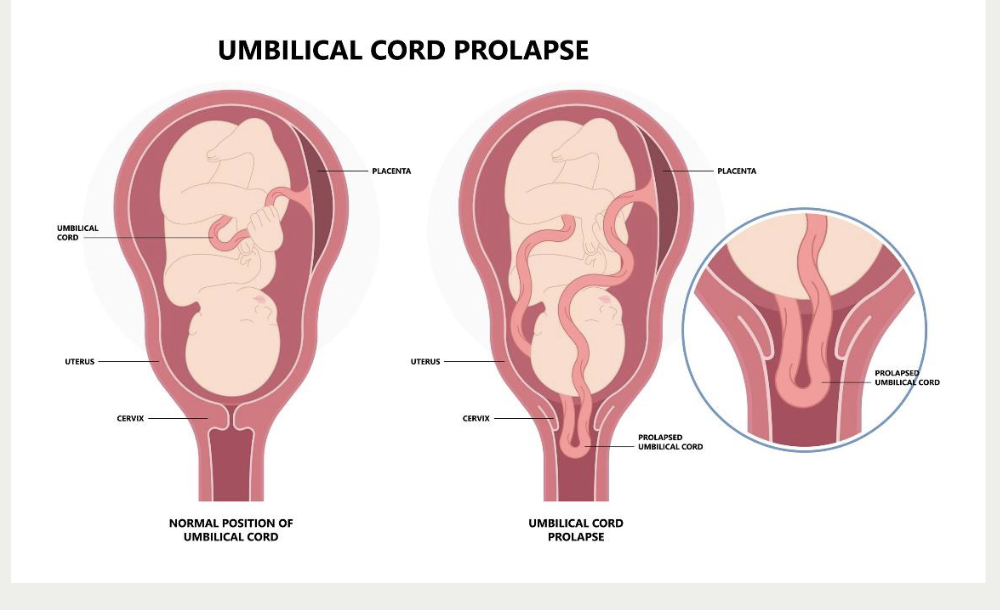
prolapsed cord signs and symptoms and risk factor
A prolapsed umbilical cord occurs when the umbilical cord slips down through the cervix into the vagina ahead of or alongside the presenting part of the fetus, before or during labor, which can compress the cord and reduce or cut off blood flow and oxygen to the baby.
signs and symptoms
long umbilical cord
malpresentation
non-engaged fetus
polyhdramnios
preterm labor
typicall happens wiht ROM; large gush —> expelled cord
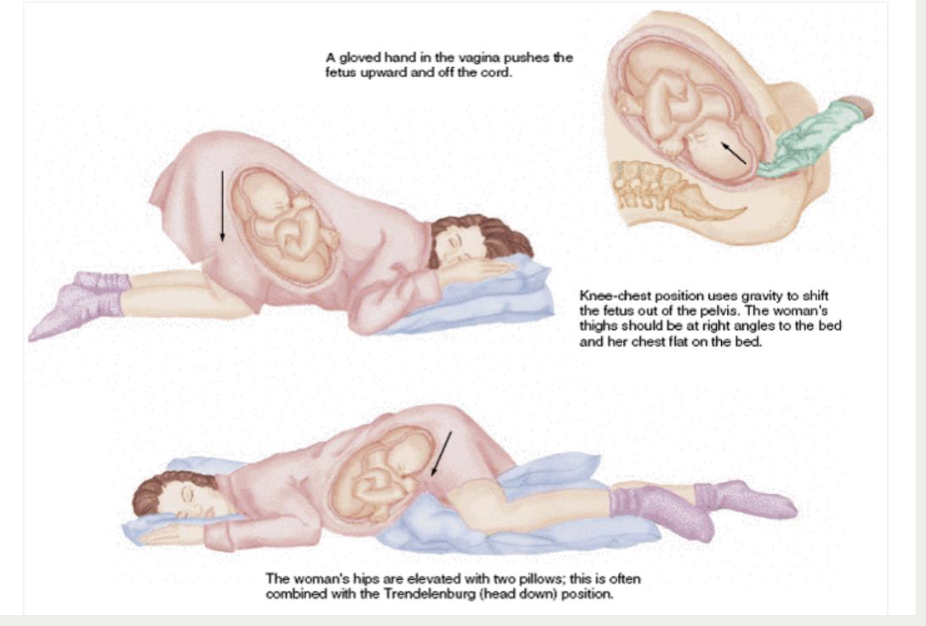
prolapes cord fetal complication and management
fetal complication
occlusion of blodo flow > 5 min —> central nervous system damage, asphyxia, death
management
call for additional assistance
hold up the presenting part
you keep your fingers in until baby is delivered
trendelenburg or knee chest position
02 and iv fluid bolus
emergency cesarean
uterine rupture
tear through the full thickness of the uterine wall, often including the endometrium, myometrium, and sometimes serosa, which can lead to fetal and maternal compromise.
Risk factor
VBAC
after uterine surgery
multiparity
fetus can be ejected inot the abdominal cavity
signs and symptoms
abnormal FHR tracing
loss of fetal station
sudden sharp abdominal pain - ripping / tearing
hemorrhage / hypovolemic shock
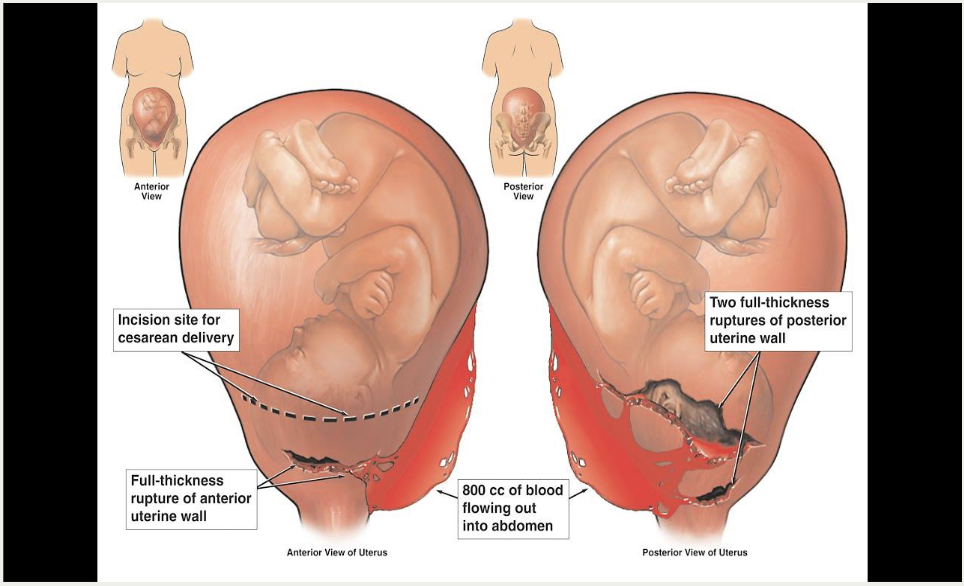
uterine rupture
prevention is best
patients with classical /vertical incision cannot labor
close monitoring of patients doing TOLAC
appropriate management of tachysystole
management
depends on severity
call for assistance / alert provider
emergency cesarean
IV fluids, 02 blood transfusions if hemodynamcially unstable
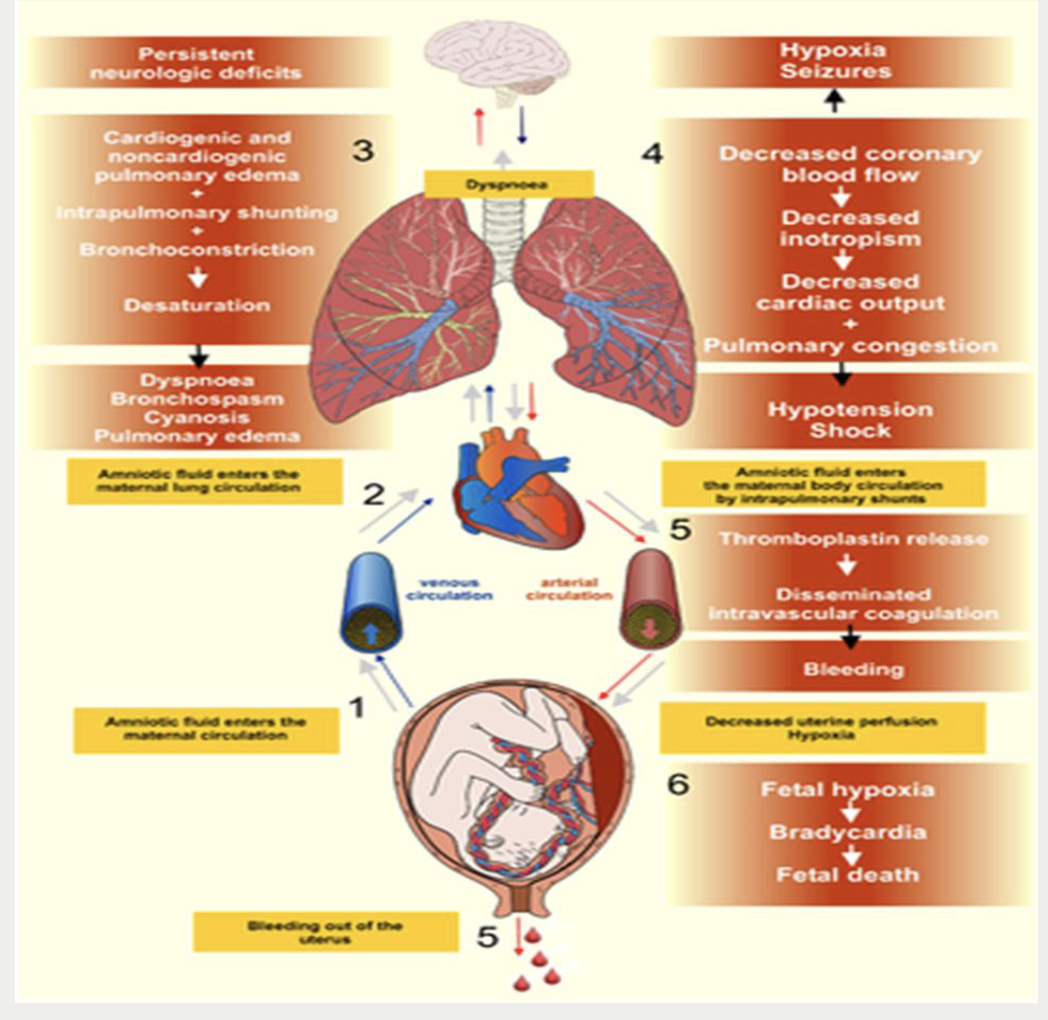
amniotic fluid embolism (AFE)
also known ans anaphylactoi syndrome of pregnancy (this is the more accurate term, it is what re recognize it to be now)
sudden acute onset of hypotension, hypoxia, and hemorrhage cause by coagulaopathy
respiratory and cardiovascular collapse = similar pathway as anaphylaxis
very rare, unpreventable, difficult to diagnose, often fatal
maternal morbidity
50% of women die within 1 hour
85 of survivors have permanent damge
neonatal mortality
20-60 % and only half of those babies are neuroligically intact
Amniotic fluid embolism (AFE) signs and symptoms and management
signs and symptoms
respiratory - restless / altered LOC, dyspnea, cyanosis —> respiratory arrest
circulatory - hypotension, tachycardio, schock —> cardiac arrest
hemorrhage (DIC) - profuse bleeding, petechiae, echhymosis, uterine atony
management
call for additional assistance - anesthesia
o2 via non rebreather mask
position side lying
administer iv fluids blood products
prepare for cpr and intubation as needed
emergency cesarean
PPH (postpartum Hemorrhage)
> 500 ml of blood for vaginal delivery
> 1000 ml of blood for cesarean
leading cause of mortality and morbidity
mostly occurs immediately or days and weeks later
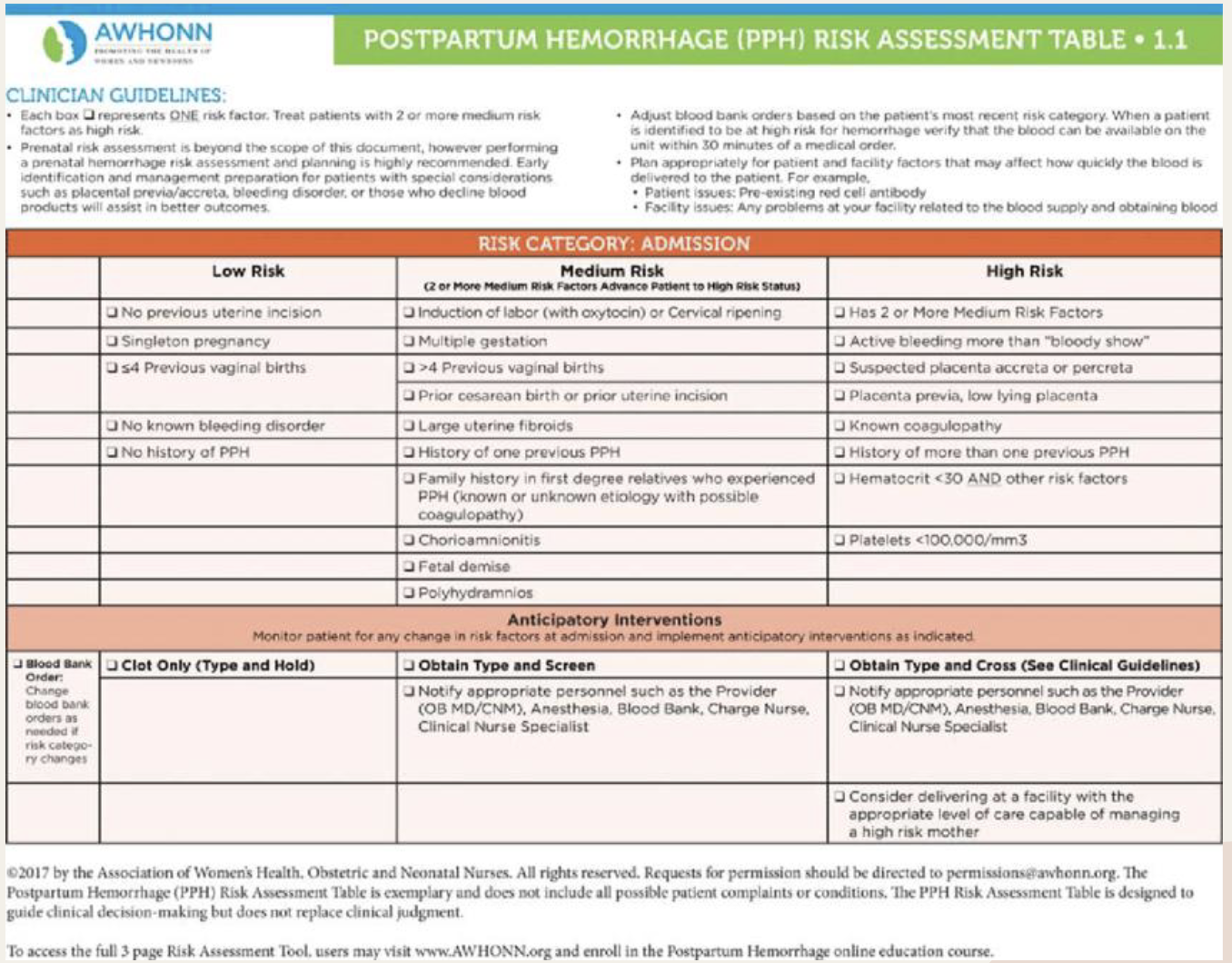
Risk assessment PPH
personal or family history
prolonged labor / prolonged use of oxytocin
think of like 24 hours or longer
chorioamnionitis, HTN disorders
placental issues - abruption, previa, accreta
operative vaginal birth or cesarean
coagulation disorders
overextended uterus - muliitple, polyhydramnios
Risk assessment tools PPH
low, medium and high risk patients
anticipatory guidance
GOAL = early recognition, determine cause and intervene before its life threatening
causes of PPH the four T’s
Tone, tissue, truama, thrombin
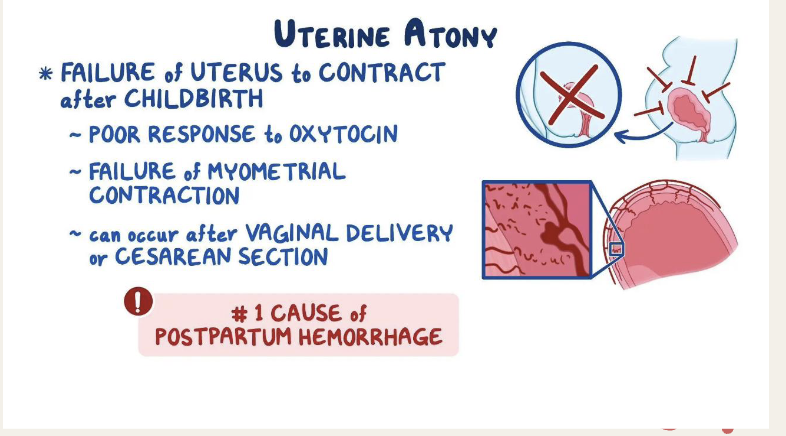
PPH Tone
TONE
most common cause of early PPH
a boggy uterus
distended bladder
bleeding
management
massage fundus
empty bladder
utertonic medications
firms the fundus
PPH Tissue
Retained placenta (tissue)
placenta not expelled within 30 minutes OR fragments of placenta still inside uterus
this causes excessive bleeding
physical barrier to clamping
placenta tricks uterus into not clamping down
management
manual extraction by provider
dilations and curretage ( D&C) as needed
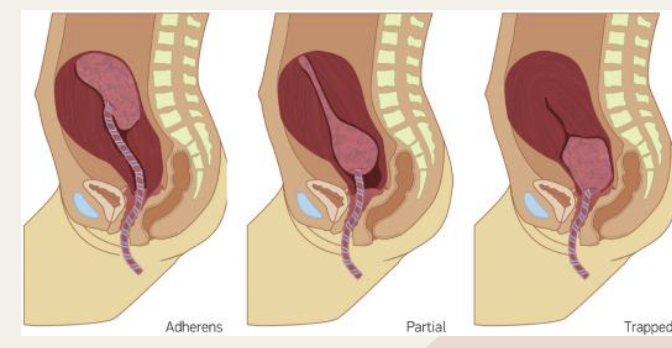
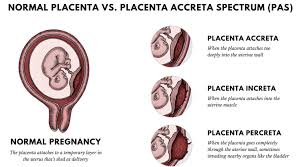
placental acreta syndrome
placenta has abnormal or invasive implantation
management
usually D&C or hysterectomy if severe
MASSIVE PPH