Human 1141 Chapters 1-7
0.0(0)
Card Sorting
1/161
Earn XP
Description and Tags
Last updated 6:41 AM on 3/9/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
162 Terms
1
New cards
Serious Mental Illness
A mental, behavioral, or emotional disorder resulting in serious functioning impairment, which substantially interferes with or limits one or more major life-activities
2
New cards
How many Americans age 18+ have experienced some form of mental illness?
47\.6 million (19.1%)
3
New cards
Dual Diagnosed
Includes s/a, physical disabilities, intellectual, and severe learning disabilities
4
New cards
Schizophrenia spectrum and other psychotic disorders, bipolar and related disorders or major depressive disorder, personality disorders
\-Positive symptoms (e.g. hallucinations, delusions)
\-Negative symptoms
\-Anhedonia
\-Psychosis
\-Negative symptoms
\-Anhedonia
\-Psychosis
5
New cards
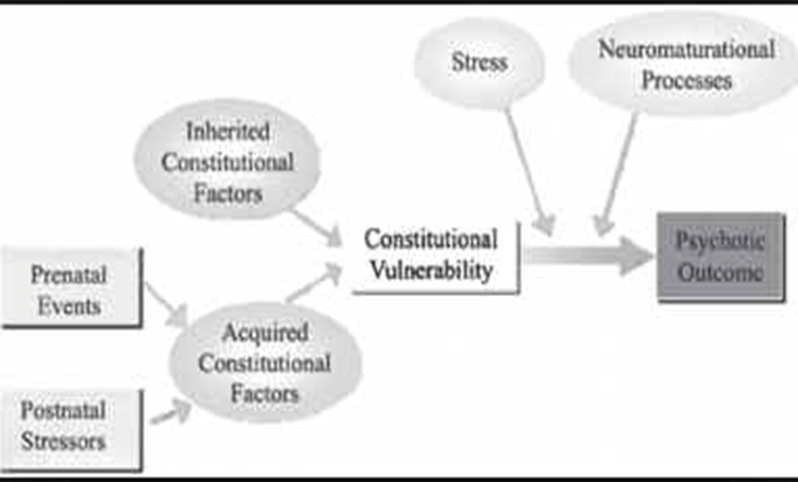
Stress Vulnerability Model
A. Psychobiological predisposition
B. Environmental component
C. The predisposing psychobiological conditions may produce prodomal symptoms
D. Acute symptoms as a result of environmental stressors
E. Interventions include biological components
F. Biological disease and societal discrimination
B. Environmental component
C. The predisposing psychobiological conditions may produce prodomal symptoms
D. Acute symptoms as a result of environmental stressors
E. Interventions include biological components
F. Biological disease and societal discrimination
6
New cards
Psychiatric Disability
Life-time, can be permanently disabling
7
New cards
Psychiatric Rehabilitation Addresses Disability
Lack of ability (focuses on skills that were never acquired or were lost)
8
New cards
Premorbid
Period before mental illness surfaced
9
New cards
Stigma of Major Mental Illness
\-Terminology can be stigmatizing
\-”Dilemma of difference”, best way to de-stigmatize is contact with individuals with mental illness
\-”Dilemma of difference”, best way to de-stigmatize is contact with individuals with mental illness
10
New cards
Forms of Stigma
(Roots in ignorance and fear)
\-Self stigma
\-Stigmatization by professionals
\-Self stigma
\-Stigmatization by professionals
11
New cards
Psychiatric Rehabilitation Goal
The goal of psychiatric rehabilitation is to enable individuals to compensate for, or eliminate the functional deficits, interpersonal barriers and environmental barriers created by the disability, and to restore ability for independent living, socialization, and effective life management
12
New cards
Psychiatric Rehabilitation
Promotes recovery, full community integration, and improved quality of life for persons who have been diagnosed with any mental health condition that seriously impairs their ability to lead meaningful lives. Psychiatric rehabilitation services are collaborative, person directed, and individualized. These services are an essential element of the health care and human services spectrum, and should be evidence-based. They focus on helping individuals develop skills and access resources needed to increase their capacity to be successful and satisfied in the living, working, learning, and social environments of their choice
13
New cards
Deinstitutionalization
\-Initiated during the 60s and 70s
\-Staff was poorly trained
\-Academic preparation of clinicians did not reflect PsyR approaches: (clubhouse model, NIMH’s Community Support System, social skills training)
\-Staff was poorly trained
\-Academic preparation of clinicians did not reflect PsyR approaches: (clubhouse model, NIMH’s Community Support System, social skills training)
14
New cards
Psychodynamic Therapy can be harmful
“Labelling” is an insight into perception
\-Patients (medical)
\-Members (clubhouse)
\-Clients, consumers (traditional community mental health centers)
\-Consumers, survivors, prosumers (less stigmatizing) BEST WAY (and most politically correct): persons with lived experiences
\-Conceptual words: least restrictive treatment environment, client involvement, and normalization
\-Patients (medical)
\-Members (clubhouse)
\-Clients, consumers (traditional community mental health centers)
\-Consumers, survivors, prosumers (less stigmatizing) BEST WAY (and most politically correct): persons with lived experiences
\-Conceptual words: least restrictive treatment environment, client involvement, and normalization
15
New cards
Person First Language
Acknowledges that a person is not their disease and treats people with mental illness with dignity
16
New cards
Severe Mental Illness as Defined by Parity Law
\-Schizophrenia
\-Paranoid and other psychotic disorders
\-Bipolar disorders (hypomanic, manic, depressive, and mixed)
\-Major depressive disorders (single episode or recurrent)
\-Schizoaffective disorders (bipolar or depressive)
\-Pervasive developmental disorders
\-Obsessive-compulsive disorders
\-Depression in childhood and adolescence
\-Panic disorder
\-Post traumatic stress disorders (acute, chronic, or with delayed onset)
\-Bulimia nervosa
\-Anorexia nervosa
\-Paranoid and other psychotic disorders
\-Bipolar disorders (hypomanic, manic, depressive, and mixed)
\-Major depressive disorders (single episode or recurrent)
\-Schizoaffective disorders (bipolar or depressive)
\-Pervasive developmental disorders
\-Obsessive-compulsive disorders
\-Depression in childhood and adolescence
\-Panic disorder
\-Post traumatic stress disorders (acute, chronic, or with delayed onset)
\-Bulimia nervosa
\-Anorexia nervosa
17
New cards
The Positive Symptoms of Schizophrenia
Positive symptoms: excess or exaggerations:
1. Thinking and ideas \*delusions)
2. Perception and sensations (hallucinations and illusions)
3. Language and communication (disorganized or bizarre speech)
4. Behavioral self-control (grossly disorganized or catatonic behavior)
1. Thinking and ideas \*delusions)
2. Perception and sensations (hallucinations and illusions)
3. Language and communication (disorganized or bizarre speech)
4. Behavioral self-control (grossly disorganized or catatonic behavior)
18
New cards
The Negative Symptoms of Schizophrenia
Negative symptoms: losses or deficits:
1. Range and intensity of emotional expression (flat affect)
2. The fluency and productivity of thought and speech (alogia)
3. The initiation of goal-directed behavior (avolition)
4. Inability to experience pleasure (anehodina)
1. Range and intensity of emotional expression (flat affect)
2. The fluency and productivity of thought and speech (alogia)
3. The initiation of goal-directed behavior (avolition)
4. Inability to experience pleasure (anehodina)
19
New cards
Delusions
Bizarre beliefs:
\-Feeling that one’s actions are under the control of others
\-Believing one has great worth, power, knowledge, a special identity, and relationship with god (grandiose)
\-Believing there are evil or negative forces targeting one’s self or loved one (can include delusions of reference)
\-Feeling that one’s actions are under the control of others
\-Believing one has great worth, power, knowledge, a special identity, and relationship with god (grandiose)
\-Believing there are evil or negative forces targeting one’s self or loved one (can include delusions of reference)
20
New cards
Hallucinations
Incorrect sensory information that the individual experiences as real:
\-Auditory (e.g. narrative, command)
\-Visual
\-Olfactory
\-Tactile
\-Auditory (e.g. narrative, command)
\-Visual
\-Olfactory
\-Tactile
21
New cards
Thought Disorders
Symptoms associated with cognition or thinking
\-Thought broadcasting
\-Thought insertion (intrusive thoughts)
\-Racing thoughts
\-Thought broadcasting
\-Thought insertion (intrusive thoughts)
\-Racing thoughts
22
New cards
Anosognosia
Lack of awareness of one’s own symptom as a symptom (direct confrontation not recommended)
23
New cards
Phases of Schizophrenia
Prodomal phase: initial period of deterioration
\-Acute/active phase: period with most severe and extreme symptoms (positive symptoms prominent)
\-Residual phase: symptoms milder, negative symptoms may persist
\-Acute/active phase: period with most severe and extreme symptoms (positive symptoms prominent)
\-Residual phase: symptoms milder, negative symptoms may persist
24
New cards
Mood Disorders
Bipolar and related disorders are separated from depressive disorders and placed between depressive disorders and schizophrenia spectrum and other psychotic disorders to recognize their place as a bridge in terms of symptoms, family history, and genetics
25
New cards
Bipolar and Related Disorders
New disorders:
\-Disruptive mood dysregulation disorder, new
\-Persistent depressive disorder, replaces dysthymic disorder and chronic major depressive disorder
\-Premenstrual dysphoric disorder, moved to this group
\-Mixed features specifier may be added to major depression episodes if features (at least three symptoms) of mania and hypomania are present (increases probability that the illness is in a bipolar spectrum, though if the person has never had an illness that met the criteria for a manic or hypomanic episode the diagnosis of Major Depressive Disorder is retained)
\-Disruptive mood dysregulation disorder, new
\-Persistent depressive disorder, replaces dysthymic disorder and chronic major depressive disorder
\-Premenstrual dysphoric disorder, moved to this group
\-Mixed features specifier may be added to major depression episodes if features (at least three symptoms) of mania and hypomania are present (increases probability that the illness is in a bipolar spectrum, though if the person has never had an illness that met the criteria for a manic or hypomanic episode the diagnosis of Major Depressive Disorder is retained)
26
New cards
Depressive Disorders
\-Disruptive mood dysregulation disorder
\-Major depressive disorder
\-Persistent depressive disorder
\-Premenstrual dysphoric disorder
\-Substance/medication-induced depressive disorder
\-Depressive disorder due to another medical condition
\-Other specified depressive disorder
\-Unspecific depressive disorder
\-Major depressive disorder
\-Persistent depressive disorder
\-Premenstrual dysphoric disorder
\-Substance/medication-induced depressive disorder
\-Depressive disorder due to another medical condition
\-Other specified depressive disorder
\-Unspecific depressive disorder
27
New cards
Criteria for Manic Episode
In order for a manic episode to be diagnosed, three or more of the following symptoms must be present:
\-Inflated self-esteem or grandiosity
\-Decreased need for sleep (e.g. one feels rested after only 3 hours of sleep)
\-More talkative than usual or pressure to keep talking
\-Flight of ideas or subjective experience that thoughts are racing
\-Attention is easily drawn to unimportant or irrelevant items
\-Increase in goal-directed activity (either socially, at work or school; or sexually) or psychomotor agitation
\-Excessive involvement in pleasurable activities that have high potential for painful consequences (e.g. engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments)
\-Inflated self-esteem or grandiosity
\-Decreased need for sleep (e.g. one feels rested after only 3 hours of sleep)
\-More talkative than usual or pressure to keep talking
\-Flight of ideas or subjective experience that thoughts are racing
\-Attention is easily drawn to unimportant or irrelevant items
\-Increase in goal-directed activity (either socially, at work or school; or sexually) or psychomotor agitation
\-Excessive involvement in pleasurable activities that have high potential for painful consequences (e.g. engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments)
28
New cards
Distinction between diagnostic categories not always clear, case in point: schizoaffective disorder: combination of psychosis plus intermittent mood episodes
Mood episodes are present for the majority of the total duration of the illness, which can include either one or both of the following:
\-Major depressive episode (must include depressed mood)
\-Manic episode
\-The psychotic illness criteria resembles Criterion A of the schizophrenia diagnosis, requiring at least two of the following symptoms for at least one month
\-Major depressive episode (must include depressed mood)
\-Manic episode
\-The psychotic illness criteria resembles Criterion A of the schizophrenia diagnosis, requiring at least two of the following symptoms for at least one month
29
New cards
Symptomology and PsyR
Interventions should address impairments caused by symptoms rather than symptoms
30
New cards
Dual Diagnosis and Co-Occurring Disorders
Mental illness + substance abuse (17-3% comorbidity)
\-Intellectual disability (20-35% comorbidity)
\-Intellectual disability (20-35% comorbidity)
31
New cards
Etiology of Mental Illness
\-Evidence suggest genetic and prenatal factors influence vulnerability to illness
\-Neuroanatomy and neural functioning is different
\-Neuroanatomy and neural functioning is different
32
New cards
Etiology of Schizophrenia
MRI brain scans of those with schizophrenia
\-have less brain tissue
\-suffer a physical dementia (enlarged ventricles)
\-may have a smaller than normal amygdala
\-have a smaller hippocampus (first psychotic break)
\-difference in frontal and temporal lobe regions
\-frontal lobes underactive, temporal lobes overactive
\-have less brain tissue
\-suffer a physical dementia (enlarged ventricles)
\-may have a smaller than normal amygdala
\-have a smaller hippocampus (first psychotic break)
\-difference in frontal and temporal lobe regions
\-frontal lobes underactive, temporal lobes overactive
33
New cards
Etiology of Bipolar Disorder
\-People with bipolar disorder also have reduced brain volume and reduced frontal lobes and sometimes an enlarged amydala
34
New cards
Neurotransmitters and Mental Illness
\-PET scan and cerebral blood flow indicated that neural functioning is disorder
\-Dopamine deficiency may be the result of problems in pregnancy, stress, trauma, drug use, genetic vulnerability which may converge neurochemically to cause psychosis
\-Medications treating mental illness may target dopamine system
\-Underactivity in the front lobes may result in negative symptoms of schizophrenia
\-Dopamine deficiency may be the result of problems in pregnancy, stress, trauma, drug use, genetic vulnerability which may converge neurochemically to cause psychosis
\-Medications treating mental illness may target dopamine system
\-Underactivity in the front lobes may result in negative symptoms of schizophrenia
35
New cards
Dopamine Theory
Disordered dopamine function associated with:
\-frontal lobes
\-temporal lobes
\-additional subcortical areas
\-frontal lobes
\-temporal lobes
\-additional subcortical areas
36
New cards
Other Neurotransmitter systems may be involved in Schizophrenia
\-Dopamine, glutamine, GABA Neuregulin, GABA, and possibly serotonin
\-Neurotransmitters involved in bipolar disorder and major depression
\-Serotonin, norepinephrine, glutamine, GABA may be involved in mood disorders, particularly major depression.. would account for changes in sleep, appetite, and drive seen in individuals with mental illness
\-Neurotransmitters involved in bipolar disorder and major depression
\-Serotonin, norepinephrine, glutamine, GABA may be involved in mood disorders, particularly major depression.. would account for changes in sleep, appetite, and drive seen in individuals with mental illness
37
New cards
Genetic Factors of Schizophrenia
\-One-half of 1%-1% for general population
\-If one parent has, risk is 10x larger
\-If both parents have, probability is 50%
\-These risks are independent of environmental factors
\-Genetics alone are not a sufficient cause of mental illness
\-If one parent has, risk is 10x larger
\-If both parents have, probability is 50%
\-These risks are independent of environmental factors
\-Genetics alone are not a sufficient cause of mental illness
38
New cards
Heritability Indexes (NOT % that will develop disorder)
\-Schizophrenia: 81%
\-Bipolar disorder: 85%
\-Major depression: 37%
\-Anxiety disorder: 26%
\-Shared environmental factors (biological and psychosocial) in etiology of schizophrenia estimated 11-19%
\*This is not the percentage that will develop the disorder, it is the proportion of variance in a particular trait, in a particular population that is due to genetic factors: in this case, shared psychiatric diagnosis
\-Bipolar disorder: 85%
\-Major depression: 37%
\-Anxiety disorder: 26%
\-Shared environmental factors (biological and psychosocial) in etiology of schizophrenia estimated 11-19%
\*This is not the percentage that will develop the disorder, it is the proportion of variance in a particular trait, in a particular population that is due to genetic factors: in this case, shared psychiatric diagnosis
39
New cards
Disorders like Schizophrenia do not die out..
\-During reproduction/early fetal development the cells and chromosomes replicate or copy themselves -sometimes a mistake occurs and they are deleted (microdeletion) or copied more than once (microduplications)
40
New cards
With Schizophrenia:
\-Certain pattern of genes may be associated specific microduplications must take place may be additional genetic mutations that take place (including substitutions of a nucleotide, a genetic anomaly known as single nucleotide polymorphisms –SNP)
\-One disease may have numerous and diverse origins genetically, with multiple
anomalies on genes necessary in order to be a factor for the emergence of a disorder
\-One disease may have numerous and diverse origins genetically, with multiple
anomalies on genes necessary in order to be a factor for the emergence of a disorder
41
New cards
Obstetric delivery problems (e.g. oxygen deprivation) –i.e. “insults” to the fetus/infant may lead to…
\-Abnormal development of brain structure which alters the evolution of brain development
42
New cards
Four complications consistently associated with development of Schizophrenia (double the chance)
1. Pregnancy complications
2. 2. Abnormal fetal growth and development
3. Complications of delivery
4. Maternal infections
43
New cards
Stress Diathesis Model
Biologically vulnerability triggers disease Stress/vulnerability/coping/competence model (nature, activated by nurture)
44
New cards
Stress
Personal losses, developmental transitions and important life events, physical illness. Also injury substance abuse and other physiological factors (e.g. sleep deprivation). This may be significant, but not necessarily a cause
45
New cards
Role of Neurotrophies (hormone-like growth factors that help neurons grow) may also explain the disease
People with schizophrenia, major depression and bipolar disorder have significantly low levels
of one major neurotrophin, brain-derived
of one major neurotrophin, brain-derived
46
New cards
Neurotrophic Factor (BDNF)..
Also are more pronounced during acute episodes of mania and depression. Abnormal levels lead to abnormal neuronal development of both dendrites and synapses. Trauma, abuse can result in low BDNF levels and can make it more likely that one will develop bipolar disorder.
47
New cards
Some individuals response to stress is prolonged
**…**and impacts the release of glucocorticoids which may result in escalating symptoms (because of
glucocorticoids interactions with the hypothalamus-pituitary-adrenal axis (HPA) –which impacts human appetites and drives… in animal studies, prolonged release of glucocorticoids is associated with the development of a smaller hippocampus.
glucocorticoids interactions with the hypothalamus-pituitary-adrenal axis (HPA) –which impacts human appetites and drives… in animal studies, prolonged release of glucocorticoids is associated with the development of a smaller hippocampus.
48
New cards
Stress/Vulnerability/Coping/Competence Model
Protective factors\* (and whether they are already in place) can prevent or lessen the onset of an acute episode of illness or lessen the impact of symptoms
\*Coping skills, supportive resources, competence in relevant life activities, and psychotropic medications
\*Coping skills, supportive resources, competence in relevant life activities, and psychotropic medications
49
New cards
Course of Mental Illness is uncertain…
The longer the psychosis is untreated, the more difficult its course and more negative the long-term outcomes
50
New cards
Relapse
A characteristic and can lead to loss (jobs, etc.) with each relapse the individual has a higher likelihood of suicide and having persistent symptoms that do not improve
51
New cards
Initial Mental Illness happens during…
Late teens or early twenties and response is often denial, which may lead to non-adherence with medication regimens
52
New cards
Development of Psychosis
Prior neuroimaging research has established that individuals who convert to psychosis have more rapid and more pronounced gray matter loss, compared to non-converters and healthy individuals. However, since the long-term effects of antipsychotic medications on cortical gray matter are not well understood and nearly all patients are treated with these medications, it has been difficult to distinguish the effects of antipsychotic drug treatment from the progression of schizophrenia
53
New cards
Course of Schizophrenia
\-20-30 year outcomes for schizophrenia more positive which validates the PsyR value of optimism that recovery is possible
\-Pre-morbid functioning (being independent and achieving goals) is a better predictor of how well people cope with their illness, including cognitive and social functioning
\-Pre-morbid functioning (being independent and achieving goals) is a better predictor of how well people cope with their illness, including cognitive and social functioning
54
New cards
Course of Mood Disorders
\-Some studies show it may worsen over time
\-People with mood disorders are likely to be symptom free between acute episodes (does not imply that mood disorder is less serious or virulent) Recurrent episodes lead to deterioration in both social and vocational functioning
\-The number and frequency of episodes and symptomology increase with age
\-Community PsyR produces better outcomes
\-People with mood disorders are likely to be symptom free between acute episodes (does not imply that mood disorder is less serious or virulent) Recurrent episodes lead to deterioration in both social and vocational functioning
\-The number and frequency of episodes and symptomology increase with age
\-Community PsyR produces better outcomes
55
New cards
Treatment
Biological (somatic) treatment:
\-Psychotic disorders: antipsychotics
\-Major depression: antidepressants
\-Bipolar disorders: mood stabilizers
\-Psychotic disorders: antipsychotics
\-Major depression: antidepressants
\-Bipolar disorders: mood stabilizers
56
New cards
Typical vs Atypical Antipsychotics
Atypicals act as dopamine antagonists while typical antipsychotics are more likely to cause parkinsonism, atypicals are more likely to cause weight gain and type 2 diabetes
\
\
57
New cards
Examples of Typical and Atypical Medication
First generation of antipsychotics (typicals): Thorazine
\-Clozapine (Clozaril) first atypical antipsychotic has serious side effects (agranulocytosis)- used when all else fails
\-Clozapine (Clozaril) first atypical antipsychotic has serious side effects (agranulocytosis)- used when all else fails
58
New cards
Dopamine Antagonist
A chemical, medication or drug that prevents the actions stimulated by dopamine. Dopamine is a naturally produced chemical in the body that binds to regions in the brain to help regulate emotions and movement. Dopamine antagonists disrupt the activity of dopamine by blocking dopamine binding sites without activating them. These medications are used to treat a variety of disorders
59
New cards
Medication Challenges
1. What medication is most effective?
2. What is the effective dose?
3. Coping with long term need to take medications
60
New cards
Medication Side Effects
\-Antipsychotics affect the neurotransmitter dopamine, which interferes with motor function (similar to Parkinson’s disease)
\-Tardive Dyskinesia: a disorder that results in involuntary, repetitive body movements. This may include grimacing, sticking out the tongue or smacking of the lips
\-Extrapyramidal syndromes (movement disorders) sustained intense muscle contraction and akathisisa
\-Tardive Dyskinesia: a disorder that results in involuntary, repetitive body movements. This may include grimacing, sticking out the tongue or smacking of the lips
\-Extrapyramidal syndromes (movement disorders) sustained intense muscle contraction and akathisisa
61
New cards
Side effects of second-generation Antipsychotic Medication: premature mortality
Weight gain is a side effect of second generation antipsychotics, which in turn is associated with:
\-metabolic syndrome\*
\-diabetes -
\-hypertension
\-coronary artery disease
\*is a clustering of at least 3 of the 5 medical conditions
\-abdominal obesity
\-high blood pressure
\-high blood sugar
\-high serum triglycerides
\-low high-density lipoprotein (HDL) levels
\-metabolic syndrome\*
\-diabetes -
\-hypertension
\-coronary artery disease
\*is a clustering of at least 3 of the 5 medical conditions
\-abdominal obesity
\-high blood pressure
\-high blood sugar
\-high serum triglycerides
\-low high-density lipoprotein (HDL) levels
62
New cards
Pharmacological treatment of Bipolar Disorder and Mania
\-Lithium (mood stabilizer) reduces the symptoms of mania/manic episodes and prevents recurrent episodes of both depressed and manic types but does not eliminate it
\-Side effects impact medication compliance
\-Prevention of future episodes may reduce the frequency of episodes and rapid cycling
\-Lithium not as effective when mixed with episodes
\-Side effects impact medication compliance
\-Prevention of future episodes may reduce the frequency of episodes and rapid cycling
\-Lithium not as effective when mixed with episodes
63
New cards
Treating mood swings with medication
\-Carbamazepine (Tegretol) anticonvulsive
\-Valproate (Depakote) used for acute episodes
\-Because mood stabilizers work slowly, sometimes antipsychotics used to treat severe mania (acute phase) to decrease potentially dangerous behavior
\-Antidepressants may cause mania
\-Polypharmaceutical interventions for “refractory Bipolar disorder” -rapid cycling (mixture of anticonvulsants)
\-Valproate (Depakote) used for acute episodes
\-Because mood stabilizers work slowly, sometimes antipsychotics used to treat severe mania (acute phase) to decrease potentially dangerous behavior
\-Antidepressants may cause mania
\-Polypharmaceutical interventions for “refractory Bipolar disorder” -rapid cycling (mixture of anticonvulsants)
64
New cards
Pharmacological Treatment of Major Depressive Disorders
\-What is more effective: antidepressants or PsyY? (Both decrease relapse… medication has side effects, and PsyY is not always available
65
New cards
Types of Antidepressants (and primary neurotransmitters impacted)
\-SSRI’s (Prozac): blocks serotonin reuptake
\-Tricyclic (Tofranil/imipramine) blocks serotonin and norepinephrine
\-MAO inhibitors (rarely used) removes the neurotransmitters norepinephrine, serotonin, and dopamine from the brain. Can cause dangerous high blood pressure when taken with certain foods
\-It takes 3-6 weeks to determine efficacy of antidepressants
\-Tricyclic (Tofranil/imipramine) blocks serotonin and norepinephrine
\-MAO inhibitors (rarely used) removes the neurotransmitters norepinephrine, serotonin, and dopamine from the brain. Can cause dangerous high blood pressure when taken with certain foods
\-It takes 3-6 weeks to determine efficacy of antidepressants
66
New cards
Medication Adherence/lack of
\-Rate of non-adherence for mentally ill population is 50%
\-”Non-adherence” better worded characterization than “compliance” -avoids the connotation of disempowerment
\-Injectables often helpful as they are administered on schedule
\-”Feeling better” can be an intuitive reason for non-adherence
\-Substance abuse can negatively impact adherence, can also be a form of “self-medication”
\-Experience of medication as “chemical restrains” can also impact
\-Difficulty accessing services (insurance rules and agency policy)
\-”Non-adherence” better worded characterization than “compliance” -avoids the connotation of disempowerment
\-Injectables often helpful as they are administered on schedule
\-”Feeling better” can be an intuitive reason for non-adherence
\-Substance abuse can negatively impact adherence, can also be a form of “self-medication”
\-Experience of medication as “chemical restrains” can also impact
\-Difficulty accessing services (insurance rules and agency policy)
67
New cards
Illness Management and Recovery
\-Titration of medication often not practiced
\-Side effects often not address
\-Algorithm for prescribing medications based on research much needed
\-Shared decision making
\-Role of psychoeducation
\-Side effects often not address
\-Algorithm for prescribing medications based on research much needed
\-Shared decision making
\-Role of psychoeducation
68
New cards
The Cost of Symptom Relief
Are psychotropic drugs contributing to prevalence and chronicity of mental illness?
\-For some, first manic episode precipitated by SSRI
\-Decreased brain volume, caused by MI or meds?
\-Antipsychotics initially block dopamine receptors but may then cause growth of dopamine receptors
\-For some, first manic episode precipitated by SSRI
\-Decreased brain volume, caused by MI or meds?
\-Antipsychotics initially block dopamine receptors but may then cause growth of dopamine receptors
69
New cards
Staff competence for effective IMR (Illness Management Recovery)
\-Thorough understanding of principles
\-Providing team approach for training
\-People with lived experience may be better equipped for delivery of IMR
\-Providing team approach for training
\-People with lived experience may be better equipped for delivery of IMR
70
New cards
Psychosocial Treatments
\-Best approach: PsyR and pharmacology
\-Use EBP interventions (e.g. CBT)
\-Complicated by insurance and managed care rules, restrictions (including pre-authorizations)
\-Psychodynamic, insight-oriented therapies found ineffective and sometimes harmful (especially for schizophrenia and depression)
\-Use EBP interventions (e.g. CBT)
\-Complicated by insurance and managed care rules, restrictions (including pre-authorizations)
\-Psychodynamic, insight-oriented therapies found ineffective and sometimes harmful (especially for schizophrenia and depression)
71
New cards
Recovery
A deeply personal, unique process of changing one’s attitudes, values, feelings, goals, skills, and/or roles. It’s a way a living a satisfying, hopeful, and contributing life, even with the limitations caused by illness. Recovery involves the development of new meaning and purpose in one’s life as one grows beyond the catastrophic effects of mental illness
72
New cards
Five Stage Model of Recovery
Moratorium, awareness, preparation, rebuilding, growth
73
New cards
Moratorium
Denial, confusion, hopelessness
74
New cards
Awareness
Hope, recognition of potential for change
75
New cards
Preparation
Work begins, recognition of strengths, connections
76
New cards
Rebuilding
Hard work, responsibility, tenacity
77
New cards
Growth
Increased self-confidence, resilience, optimism
78
New cards
The 10 Fundamental Components of Recovery
1. Self-direction
2. Individualized and person-centered
3. Empowerment
4. Holistic
5. Non-linear
6. Strengths-based
7. Peer support
8. Respect
9. Responsibility
10. Hope
79
New cards
Dual Recovery Perspectives
\-Learning to cope with illness-related symptoms and functional deficits
\-Recovering from the effects of stigmatizing attitudes, lost education and vocational opportunities, and poverty
\-Recovering from the effects of stigmatizing attitudes, lost education and vocational opportunities, and poverty
80
New cards
Movement toward recovery-oriented Mental Health systems
\-SAMHSA funded a Recovery to Practice Project which helps behavioral health and general healthcare practitioners improve delivery of recovery-oriented services, supports, and treatment
\-From the PsyR perspective, recovery is an individualized process of learning to live successfully with a serious mental illness. This involves reformulating one’s self concept, establishing new life aspirations, and becoming a valued and contributing member of the community
\-From the PsyR perspective, recovery is an individualized process of learning to live successfully with a serious mental illness. This involves reformulating one’s self concept, establishing new life aspirations, and becoming a valued and contributing member of the community
81
New cards
Goals of PsyR
Programs strive for and achieve:
1. Recovery: unique to the individual
2. Community integration (domains)
\-Physical (residing in a community, using its resources)
\-Social (interacting with a variety of people in their community)
\-Psychological (sense of belonging, rather than being segregated in group homes or sheltered workshops)
3. Quality of life: individuals subjective sense of well being in various life domains. Social support, companionship, employment, recreation, food, shelter, clothing, and an active sex life
1. Recovery: unique to the individual
2. Community integration (domains)
\-Physical (residing in a community, using its resources)
\-Social (interacting with a variety of people in their community)
\-Psychological (sense of belonging, rather than being segregated in group homes or sheltered workshops)
3. Quality of life: individuals subjective sense of well being in various life domains. Social support, companionship, employment, recreation, food, shelter, clothing, and an active sex life
82
New cards
Values of the PsyR
1. Self determination and empowerment (self-esteem, possessing power, and community activism)
2. Dignity and worth of every individual
3. Optimism that everyone has the capability to recover, learn, and grow (research shows that other’s opinions shape self-efficacy, we need to convey optimism)
4. Wellness: PsyR programs should be holistic (should include help gaining access to PCP, nutritional, and exercise programs)
5. Cultural diversity: sensitive to culture (including intra cultural variation) and ethnicity, religious affiliation, language, physical size, gender, sexual orientation, age, disability, political orientation, geographic location, socioeconomic, and occupational status. Also need to advocate on both individual and system wide levels and strive for cultural competency
6. Promotion of valued social roles and normalized environments
83
New cards
Guiding Principles
Rules that can be applied in order to achieve the goals and reflect values of the field
\-Person-centered approach
\-Partnership between provider and user (collaborative with shared decision-making, e.g. use of decision aids)
\-Partnership with family members and significant others (e.g. psychoeducation model)
Utilization of peer support: self-help groups, use of prosumers as staff
\-Utilization of natural supports
\-Focus on work and career development
\-Practitioners focus on skill acquisition, resources and supports necessary for success
\-Assessments related to person-chosen goals and environments
\-Situational assessments focus on skills and resources needed to achieve rehabilitation goal
\-Global assessment unrelated to specific goals
\-Goal-related skills training, resource development, and environmental modifications
\-Integration of treatment (symptom relief) and rehabilitation (overcoming barriers and pursuit of goals) services (not separated)
\-Ongoing (unlimited with respect to time), accessible, and coordinated services (especially various service providers)
\-Empirical orientation (evidence based practice which yields the best outcome)
\-Person-centered approach
\-Partnership between provider and user (collaborative with shared decision-making, e.g. use of decision aids)
\-Partnership with family members and significant others (e.g. psychoeducation model)
Utilization of peer support: self-help groups, use of prosumers as staff
\-Utilization of natural supports
\-Focus on work and career development
\-Practitioners focus on skill acquisition, resources and supports necessary for success
\-Assessments related to person-chosen goals and environments
\-Situational assessments focus on skills and resources needed to achieve rehabilitation goal
\-Global assessment unrelated to specific goals
\-Goal-related skills training, resource development, and environmental modifications
\-Integration of treatment (symptom relief) and rehabilitation (overcoming barriers and pursuit of goals) services (not separated)
\-Ongoing (unlimited with respect to time), accessible, and coordinated services (especially various service providers)
\-Empirical orientation (evidence based practice which yields the best outcome)
84
New cards
Strengths Focus
Personal attributes, talents and skills, environmental strengths, and interests and aspirations
85
New cards
Psychiatric Rehabilitation Ethics
Intellectual framework that is consistent with the principles and values of a profession, helping analyze when faced with decisions that involve moral choice
\-Goals, values, and guidelines may change as the field advances and new knowledge is created
\-Goals, values, and guidelines may change as the field advances and new knowledge is created
86
New cards
Psychiatric Rehabilitation Process
1. Diagnostic phase: through assessment of individuals readiness to participate in rehabilitation activities
2. Planning phase: choose an overall goal related to increased success, satisfaction in client’s domains… a rehabilitation plan that outlines and prioritizes very specific goals and objective formulated
3. Intervention phase: identifying strategies to accomplish each goal or objective
87
New cards
Hallmarks of the Psychiatric Rehabilitation Process
\-Directed by the consumer: Person centered-=fosters recovery
\-Collaborative effort, done with NOT for for
\-Environments of choice: consumer chooses
\-Skills necessary for success in specific environment are developed
\-Rather than focus on client’s disability, environment or policy adjustment (at work) may be modified
\-”Reasonable accommodation” -1990 ADA
\-Valued social roles: consumer assisted in assuming specific roles in those environments that are valued by the community
\-”Good neighbor” rather than “former patient”
\-Successful achievement of a goal may involve the ability to adapt well to both a new environment and a new role
\-Collaborative effort, done with NOT for for
\-Environments of choice: consumer chooses
\-Skills necessary for success in specific environment are developed
\-Rather than focus on client’s disability, environment or policy adjustment (at work) may be modified
\-”Reasonable accommodation” -1990 ADA
\-Valued social roles: consumer assisted in assuming specific roles in those environments that are valued by the community
\-”Good neighbor” rather than “former patient”
\-Successful achievement of a goal may involve the ability to adapt well to both a new environment and a new role
88
New cards
Phase 1: Rehabilitation Diagnosis
\-Not focused on dx
\-More focused on environment and skill building
\-Readiness to identify a goal and commitment to achievement (needs to be assessed, with possible identification of barriers identified and activities to promote readiness if needed)
\-Possible explanations for not being “ready”
\-Uncertainty of client, ongoing symptoms, functional deficits, poverty, very low self-esteem and/or acceptance of role as “psychiatric patient”
\-Past failures
\-Poorly trained or overworked staff
\-More focused on environment and skill building
\-Readiness to identify a goal and commitment to achievement (needs to be assessed, with possible identification of barriers identified and activities to promote readiness if needed)
\-Possible explanations for not being “ready”
\-Uncertainty of client, ongoing symptoms, functional deficits, poverty, very low self-esteem and/or acceptance of role as “psychiatric patient”
\-Past failures
\-Poorly trained or overworked staff
89
New cards
Assessing Psychiatric Rehabilitation Readiness
Readiness assessment:
\-Need for change?
\-Commitment to change, belief that change is necessary, positive, possible, and will be supported
\-Environment awareness (previous experiences about the chosen environment)
\-Self-awareness
\-Closeness to practitioner (relationship)
\-Need for change?
\-Commitment to change, belief that change is necessary, positive, possible, and will be supported
\-Environment awareness (previous experiences about the chosen environment)
\-Self-awareness
\-Closeness to practitioner (relationship)
90
New cards
Building Readiness
PsyR practitioners can address readiness deficits by helping the person find opportunities to try out relevant environments and roles
\-Work on trust and therapeutic relationship building
\--Demonstrating empathy
\--Monitoring how relationship is perceived by client
\--Providing positive feedback
\--Take time to achieve goal consensus
\--Adapt to client’s preferences
\--Pay attention to cultural issues
\--Don’t rush engagement process (state you are interested in learning)
\--Perform concrete assistance (driving, etc)
\-Work on trust and therapeutic relationship building
\--Demonstrating empathy
\--Monitoring how relationship is perceived by client
\--Providing positive feedback
\--Take time to achieve goal consensus
\--Adapt to client’s preferences
\--Pay attention to cultural issues
\--Don’t rush engagement process (state you are interested in learning)
\--Perform concrete assistance (driving, etc)
91
New cards
Choosing a Goal
Practitioner may need to learn more about the person’s values, interests, aspirations, and satisfaction with functioning in various domains (and prioritize which environment to work on first, may involve taking on a new role or looking at choice available for a particular type of environment)
\-Goals need to be stated clearly and in the first person which designated specific environment and time frame
\-Goals need to be stated clearly and in the first person which designated specific environment and time frame
92
New cards
Functional Assessment
\-Once rehabilitation goal has been established, skills and supports need to be determined
\-Functional assessment addresses critical skills (in behavioral terms to be able to quantify) essential for person’s success in setting and chosen role. Evaluation needs to evaluate skill level --which skills need to be developed (focus on strengths, then move on to deficits)
\-Difference between global assessment and functional assessment
\-Functional assessment addresses critical skills (in behavioral terms to be able to quantify) essential for person’s success in setting and chosen role. Evaluation needs to evaluate skill level --which skills need to be developed (focus on strengths, then move on to deficits)
\-Difference between global assessment and functional assessment
93
New cards
Phase 2: Rehabilitation Plan
\-Rehabilitation plan is driven by the consumer-chosen overall rehabilitation goal and is focused on skills and resources that need to be developed or improved VS treatment plan (sometimes these are combined into a comprehensive and individualized service plan/recovery plan)
\-Identify and work on just a few skills or resources, short term objectives related to skill or resource development (list objectives in specific, measurable, and time limited terms in order to be clear to everyone
\--start with a task that can provide some success from client efforts
\--and build up to more difficult tasks
\-Identify and work on just a few skills or resources, short term objectives related to skill or resource development (list objectives in specific, measurable, and time limited terms in order to be clear to everyone
\--start with a task that can provide some success from client efforts
\--and build up to more difficult tasks
94
New cards
Phase 3: Rehabilitation Interventions
Consumer and PsyR provider identify and employ specific intervention strategies to support achievement of objectives:
\-Development of skills (and reason for any skill deficits)
\-Development of supports, resources
\-Environmental modifications
\-Specialized counseling techniques:
\--motivational interviewing
\--cbt
\--behavioral strategies: reward (preferred) and punishment
\--modeling (Bandura)
\-Development of skills (and reason for any skill deficits)
\-Development of supports, resources
\-Environmental modifications
\-Specialized counseling techniques:
\--motivational interviewing
\--cbt
\--behavioral strategies: reward (preferred) and punishment
\--modeling (Bandura)
95
New cards
Direct Skills Teaching
No prepackaged modules, emphasis on telling, showing, (or modeling), and doing
\-Components of direct skill teaching:
Reviews what the person already knows
Overview of rationale for using skills
Presents a demonstrations of skill use
Exercise for practice of the skill
Summarizes what has been learned
\-Components of direct skill teaching:
Reviews what the person already knows
Overview of rationale for using skills
Presents a demonstrations of skill use
Exercise for practice of the skill
Summarizes what has been learned
96
New cards
Skills Programming
An important component, helps with skill generalization/practice and identifying obstacles and strategies for overcoming them. Includes real world practice opportunities in relevant setting(s)
97
New cards
Specific Categories of Skills
1. Establish a rationale for the skill
2. Discuss the steps of the skill
3. Model the skill in a role play and review
4. Engage a group member in a role play using the same situation
5. Provide positive feedback
6. Provide corrective feedback
7. Engage the group member in another role play using the same situation
8. Provide additional feedback (positive first)
9. Engage other group members in role plays and provide feedback, as in steps 4-8
10. Assign homework that will be reviewed at the beginning of the next session (this encourages generalization)
98
New cards
Skill Generalization
Place and train strategy so the skill is not just situation specific
\-Individualized reinforcement strategies to reward use of newly learned skills (social reinforcement, in vivo training, self reward, development of intrinsic reinforcement)
\-Individualized reinforcement strategies to reward use of newly learned skills (social reinforcement, in vivo training, self reward, development of intrinsic reinforcement)
99
New cards
Skill Maintenance
Reinforcement and regular practice (“use it or lose it”)
100
New cards
Cognitive Remediation
Using behavioral interventions that improve cognitive functioning (needed to achieve chosen goals) through
\-repetitive exercises and positive reinforcers (e.g. praise, and/or tokens)
\-can be done with an individual, in groups, using specialised computer programs
Cognitive remediation has been combined effectively with social skills training to help consumers learn, retain, and apply social skills in vivo
\-repetitive exercises and positive reinforcers (e.g. praise, and/or tokens)
\-can be done with an individual, in groups, using specialised computer programs
Cognitive remediation has been combined effectively with social skills training to help consumers learn, retain, and apply social skills in vivo