UKMLA: Endocrinology
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
78 Terms
Addison’s Disease: What is it?
The insufficient production of glucocorticoids and mineralocorticoids from the adrenal cortex→ Primary adrenal insufficiency
Addison’s Disease: What are the causes?
Autoimmune destruction of adrenal glands
Trauma to adrenal glands
Haemorrhage
Infarction
Addison’s Disease: What is the pathophysiology?
Damage to the adrenal cortex is primary adrenal insufficiency
Dysfunction to HPA axis is secondary adrenal insufficiency
Addison’s Disease: What are the symptoms?
Hypotension
Fatigue and weakness
Gastrointestinal symptoms
Syncope
Skin pigmentation due to increased ACTH which stimulates production of alpha melanocyte stimulating hormone (MSH)
Always suspect Addison’s disease in patients with fatigue, postural dizziness, hyponatraemia, borderline hyperkalaemia, and mucosal pigmentation due to hypoaldesteronism
Addison’s Disease: What is the classic dermatological presentation?
Acanthosis nigricans (hyperpigmentation of skin folds due to high ACTH → too much alpha melanocyte stimulating hormone)
Tanned appearance

Addison’s Disease: What is the investigation?
9am serum cortisol
Prolonged ACTH stimulation test → Synacthen test if 9am cortisol test is abnormal
Addison’s Disease: What is the management?
Sick day rules→ carrying steroid card, medical alert bracelet
Double hydrocortisone steroid dose, fludrocortisone dose remains the same
Addison’s Disease: What is addisonian crisis?
An Addisonian crisis, a life-threatening condition characterised by severe hypotension and electrolyte imbalances
Addison’s Disease: What is the management?
Should be managed with:
Aggressive fluid resuscitation
Administration of intravenous/IM (if no access) steroids STAT
Glucose administration if hypoglycaemia is present
Addison’s Disease: Which part of the adrenal gland produces mineralcorticoids e.g. fludrocortisone?
Zona glomerulosa
Addison’s Disease: Which part of the adrenal gland produces adrenaline?
Adrenal medulla
Addison’s Disease: Which part of the adrenal gland produces androgens?
Zona reticularis
Addison’s Disease: Which part of the adrenal gland produces glucocorticoids e.g. cortisol?
Adrenal medulla
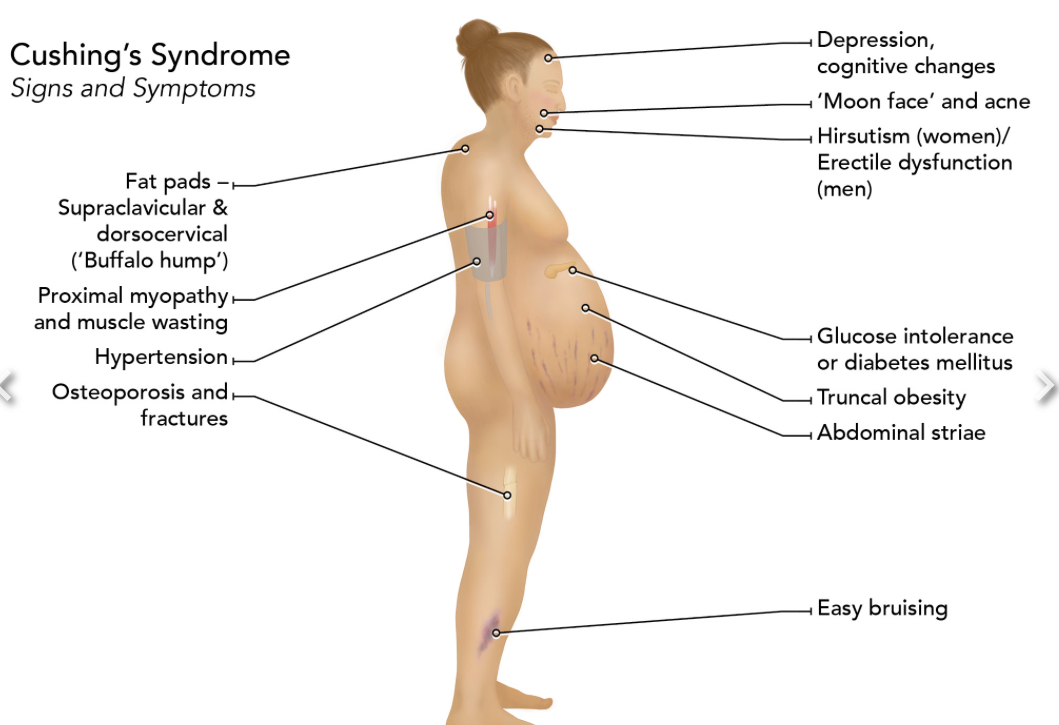
Cushing’s Syndrome: What is it?
Excess glucocorticoids
Cushing Syndrome: What is the difference between Cushing’s syndrome and disease?
Syndrome→ excess glucocorticoids
Disease→ ACTH pituitary tumour
Cushing’s Syndrome: What are the causes?
ACTH-dependent→ excess production of ACTH due to pituitary tumour
ACTH-independent→ excess cortisol due to adrenal adenomas/carcinomas
Cushing’s Syndrome: What is the most common cause?
Exogenous corticosteroid exposure
Cushing’s Syndrome: What are the clinical features?
Proximal myopathy
Buffalo hump
Striae and easy bruising on abdomen
Osteoporosis and fractures
Obesity
HTN
Hyperkalaemia
Hirsutism
Erectile dysfunction
Psychological issues
Cushing’s Syndrome: What are the investigations?
24 hour urinary free cortisol test
Low-dose dexamethasone suppression test
Cushing’s Syndrome: What is the medical management?
Metryapone
Ketoconazole
Pasireotide
Diabetes Drugs Side Effects: What are the side effects of biguanides?
Lactic acidosis
GI disturbance
Diabetes Drugs Side Effects: What are the side effects of sulfonylureas?
Gliclazide:
Hypoglycaemia→ leads to falls
Weight gain
Diabetes Drugs Side Effects: What are the side effects of thiazolidinediones?
Fluid retention
Weight gain
Worsens heart failure
Diabetes Drugs Side Effects: What are the side effects of SGLT2-inhibitors?
DKA
Diabetes Drugs Side Effects: What are the side effects of DPP4-inhibitors?
Hypoglycaemia
GI upset
DKA: What is the diagnostic criteria?
Blood glucose over 11
Ketones over 3
PH <7.3 or HCO3 <15 (acidosis)
DKA: What is the pathophysiology?
DKA: What are the common triggers?
Infections
Dehydration and fasting
Missing doses of insulin
Medications e.g. steroid treatment or diuretics
Surgery
Stroke or myocardial infarction
Alcohol excess or illicit drug use
Pancreatitis
DKA: What is the criteria for severe DKA?
Blood ketones > 6mmol/L
Bicarbonate < 5mmol/L
Blood pH < 7
Anion gap above 16
Hypokalaemia on admission
GCS less than 12
Oxygen saturations < 92% in air
Systolic BP < 90mmHg
Brady or tachycardia (heart rate < 60 or > 100bpm)
DKA: What are the symptoms?
Nausea and vomiting
Abdominal pain
Polyuria
Polydipsia
Weakness
DKA: What are the signs?
Dry mucous membranes
Hypotension
Tachycardia
Altered mental state (drowsiness, confusion, coma)
Kussmaul's breathing (deep, sighing breathing to compensate for metabolic acidosis by blowing off carbon dioxide)
Fruit-like smelling breath (due to ketosis)
DKA: What is the management?
Fluid replacement with 500ml bolus of IV 0.9% saline solution asap (over a few minutes!!)
If the patient is hypotensive/doesn’t respond to the first bolus, give up to 1L bolus of IV 0.9% saline solution
Fixed rate of insulin IV (Actrapid) over one hour→ stop regular SHORT-ACTING doses they would have usually had in that time instead but continue LONG-ACTING doses as normal
Heparin for VTE prophylaxis
DKA: What is the most important complication to look out for in patients with DKA?
Cerebral oedema
Gestational Diabetes: What is the diagnostic criteria?
According to NICE guidelines, gestational diabetes mellitus is diagnosed if the woman has either:
a fasting plasma glucose level of >5.6 mmol/L; or
a 2-hour post-oral glucose tolerance test plasma glucose level of >7.8 mmol/L
Gestational Diabetes: What are the risk factors?
BMI >30
Previous macrosomic baby (>4.5kg)
History of stillbirth
Previous gestational diabetes
First Degree Relative with Diabetes
Family origin with a high prevalence of diabetes (South Asia,Black Caribbean and Middle Eastern)
Gestational Diabetes: What is the management?
Diet and exercise
If not under 7 within 2 weeks, give metformin
If still uncontrolled, start insulin therapy
Gestational Diabetes: What are the complications of uncontrolled gestational diabetes?
Macrosomic baby (>4.5kg)
Neonatal seizures due to hypoglycaemia
Gestational Diabetes: When is an OGTT offered?
24-28 weeks gestation period
Hyperthyroidism: What is it?
A condition in which the thyroid gland is overactive, leading to the production of excess thyroid hormones
Thyrotoxicosis: What is it?
The syndrome resulting from the presence of excessive thyroid hormones in the body, not always due to thyroid gland overactivity.
Hyperthyroidism: What are the main causes?
Graves→ autoimmune stimulation of thyroid gland by TSH
Toxic adenoma
Goitre
Amiodarone
Lithium
Pregnancy
Radiation exposure
Hyperthyroidism: What are the signs and symptoms?
↑ Basal metabolic rate
Heat intolerance
Tachycardia and arrhythmias
Weight loss
Diarrhoea
Sweaty skin
Insomnia and sleep disturbances
Restlessness and tremors
Thyroid Disease: What are the shared symptoms of hyper and hypo thyroidism?
Mood changes
Menstrual disturbances
Hyperthyroidism: What are the specific features of grave’s disease?
Exophthalmos/proptosis→ bulging eyes
Thyroid acropachy→ soft tissue swelling, clubbing and new bone growth
Pretibial myxoedema
Hyperthyroidism: What is the side effect of using carbimazole to treat grave’s disease?
Treatment of Grave's disease with Carbimazole can lead to agranulocytosis and potentially to neutropenic sepsis, so prompt request of a full blood count (FBC) is essential in management.
Hyperthyroidism: What is the difference between De Quervain’s thyroiditis and grave’s disease?
De quervain’s thyroiditis→ painful neck, tender on palpation and occurs after viral infection
Hyperthyroidism: What are the investigations?
TFT→ raised T3 AND T3
TSIAb
TRAb
Thyroid US
Radioidine uptake test → diffuse uptake indicates Graves’ disease
Hyperthyroidism: What is the management?
Carbimazole ± prophylthiouracil
Prophylthiouracil only if in first trimester of pregnancy
Propanalol
Radioiodine therapy→ a radioactive form of iodine that selectively concentrates in the thyroid gland. It damages the thyroid tissue, reducing its hormone-producing ability.
Thyroidectomy
Hyperthyroidism: What are the features of thyroid storm?
Unrelated or poorly managed hyperthyroidism after surgery, trauma or infection:
Restlessness and agitation
High-output heart failure
Profound tachycardia
Fever
Delirium and altered mental status
Hyperthyroidism: What is the management of thyroid storm?
IV propanol and digoxin
Prophylthioracil and lugol’s iodine
Corticosteroids→ inhibits conversion of T4 to T3
Phaeochromocytoma: What is it?
A pheochromocytoma is a catecholamine-secreting tumour that originates in the adrenal medulla.
Phaeochromocytoma: What are the symptoms?
Episodic
HTN
Anxiety
Weight loss
Fatigue
Palpitations
Excessive sweating
Headaches
Flushing
Fever
Difficulty breathing (dyspnea)
Abdominal pain
Phaeochromocytoma: What factors can worsen symptoms?
Stress
Exercise
Surgery
Beta blockers
Opiates
Phaeochromocytoma: What are the investigations?
Plasma metanephrines testing followed by urinary metanephrines.
Adrenal imaging should be pursued only after biochemical confirmation
Phaeochromocytoma: What is the management?
Surgical resection → do alpha blockade with phenoxybenzamine pre-surgery FIRST to prevent HTN crisis during surgery
Phaeochromocytoma: What are symptoms of the neurofibromatosis type 1? (NF1)
Iris hamartomas (lisch nodules)
Cafe-au-lait spots
Scoliosis
HTN
Intermittent palpitations
Raised metanephrine
T1D: What is the pathophysiology?y
Destruction of the insulin-producing beta cells within the pancreas, leading to insulin deficiency.
T1D: What are the symptoms?
Polyuria
Polydipsia
Weight loss
In severe cases, patients may present with diabetic ketoacidosis(DKA) characterised by hyperglycemia, metabolic acidosis, and ketonemia.
T1D: What is the diagnostic criteria?
If symptomatic, one of the following results is sufficient for diagnosis:
Random blood glucose > 11.1mmol/l or Fasting plasma glucose >7mmol/l
2-hour glucose tolerance > 11.1mmol/l
HbA1C > 48mmol/mol (6.5%)
If the patient is asymptomatic, two results are required from different days.
T1D: What is the management?
Short-acting insulin → after meals/snacks (3/5th of daily dose)
Long-acting insulin→ at night
IM glucagon and dextrose for unconscious individuals (2/5th of daily dose)
T1D: What is the initial management?
Basal-bolus insulin therapy or insulin pump
T1D: What are the target glucose leaves?
Pre-meal blood glucose: 4-7 mmol/L (72-126 mg/dL)
Bedtime blood glucose: 6-10 mmol/L (108-180 mg/dL)
HbA1c: Less than 7%
T1D: Which condition is most commonly associated with T1D?
Hyperthyroidism → ensure patient goes for routine TFT
T1D/T2D: What is the classic feature of chronic diabetic sensory neuropathy?
Glove and stocking sensory loss
T1D/T2D: What does the glycaemic index represent?
A measure of how quickly carbs affect blood sugars
T2D: What is the pathophysiology?
Inadequate insulin production from beta cells→ insulin resistance.
T2D: What are the symptoms?
Polyuria
Polydipsia
Unexplained weight loss
Blurry vision
Fatigue
T2D: What is the diagnostic criteria?
If symptomatic, one of the following results is sufficient for diagnosis:
Random blood glucose > 11.1mmol/l
Fasting plasma glucose > 7mmol/l
2-hour glucose tolerance > 11.1mmol/l
HbA1C > 48mmol/mol (6.5%)
If the patient is asymptomatic, two results are required from different days
T2D: What is the management?
Metformin
If HbA1c over 58→ combine metformine with pioglitazone or sulphonylurea
If dual therapy ineffective, start triple therapy → metformin + pioglitazone/sulphonylurea + empagliflozin
Triple therapy ineffective?→ GLP-1 agonist
Last resort?→ start insulin
T2D: What is the MOA of metformin?
Inhibits hepatic gluconeogenesis
T2D: What are the microvascular complications?
Diabetic retinopathy - Leading cause of visual loss in adults.
Diabetic nephropathy - Leading cause of chronic kidney disease, characterised by proteinuria.
Diabetic neuropathy - Chronic hyperglycaemia leads to various neuropathies.
Gastrointestinal Complications - Gastroparesis due to nerve damage.
Foot Complications - High risk for ulceration and infection.
Sexual Dysfunction - Related to multiple factors including neuropathy and microvascular complications
T2D: How can Muslims manage their diabetes during Ramadan?
Continue on 500mg, take the morning dose before Suhoor (pre-sunrise meal), combine afternoon dose with dose taken at Iftar (after sunset meal)
T1D/T2D: What is the DVLA’s guidance on driving?
Insulin-treated diabetes:
Group 1 (car/motorcycle): Drive if well-controlled, monitor blood glucose before and during driving.
Group 2 (lorry/bus): Stricter rules, annual medical review required.
T1D/T2D: What is the target blood pressure?
<140/90
T1D/T2D: What is the pathophysiology of diabetic neuropathy?
Advanced glycation end products induced by hyperglycaemia damage nerve fibres through their effects on matrix metalloproteinases
T1D/T2D: What is the management of diabetic neuropathy?
Amitriptyline (tricyclic antidepressant)
T1D/T2D: Which drugs should diabetics avoid?
Thiazides→ increases blood sugars!!
T1D/T2D: What is the management of HTN in diabetics?
In diabetes, age or ethnicity doesn’t really matter like it’s usually does so give:
White→ ACEi
Black→ ARB (then CCB)