Bones and Skeletal Tissues 1
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
Characteristics of Cartilage
features between dense Connective tissue and bone
avascular, devoid of nerve fibers
all eyes are made up of cells encased in small cavities(lacunae) within jelly like extracellular matrix
ground substances contain lots of GAGs
Collagen fibers
Perichondrium
layer of dense irregular connective tissue surrounding cartilage like a girdle
functions of perichondrium
helps cartilage resist outward expansion
contains blood vessels for nutrient delivery to cartilage
it can also form scar tissue because poorly vascularized cartilage repairs badly
Chondroblasts
immature cartilage cells- actively form cartilage
Chondrocytes
mature cartilage cells- maintain cartilage
Lacunae
localized clusters of chondrocytes in cartilage that also contain osteocytes
What are the 3 kinds of cartilage
hyaline, elastic, Fibro cartilage
Hyaline cartilage (4)
- most abundant; firmsupport + pliability;
- lots of collagen; appears glassy blue-white;
- chondrocytes - only 1-10% of volume
occurs where your bones connect together( joints)

Location of hyaline cartilage (2)
embryonic skeleton, ends of long bones (epiphyseal plates in growing children)
- costal cartilages of ribs, cartilages of nose, trachea, larynx
Function of hyaline cartilage (2)
- supports & flexibility; reinforces; resilient
- cushioning & resists compressive stress
Elastic cartilage
like hyaline, but has more elastic fibres
Location of elastic cartilage
external ears, epiglottis
Fibrocartilage (2)
rows of chondrocytes alternating rows of thick collagen fibres
- great tensile strength( strongest and sturdiest)
Location of fibrocartilage
intervertebral discs, pubic symphysis, discs of knee joints (where hyaline cartilage meets a ligament or a tendon)
Function of fibrocartilage
-tensile strength
- ability to absorb compressive shock
Appositional growth
Cartilage-forming cells in perichondrium secrete matrix against external face of existingcartilage
Cartilage increases in width or diameter
bones also grow this way in thickness not width
Interstitial growth
Chondrocytes within lacunae divide and secrete new matrix, expanding cartilage from within
Cartilage increases in length
bones cannot grow interstitially because the matrix is mineralized
Bone
living dynamic tissue that reacts to its environment
What are the two main functions of bones
1)reacts to amount of force applied by increasing density and amount of roughening on bone or decreasing density when force is reduced (deposition vs. resorption)
2) bone stores calcium- reabsorbed and transferred to bloodstream when needed
What are the 7 functions of bones
support: Provide framework that supports body
protection: fused bones skull => protects brain, Vertebrae surrounds spinal cord
movement- muscles pull on them in order to move.
mineral and fat storage: reservoir for minerals
blood cell formation: happens in red marrow
hormone production: Produce osteocalcin (regulate insulin secretion, glucose homeostasis, energy)
Classification of bones
Two main groups, divided by location
- Axial
- Appendicular
Axial skeleton
Long axis of body
‒ Skull, vertebral column, rib cage
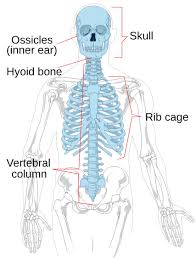
Appendicular skeleton
Bones of upper and lower limbs
‒ Girdles attaching limbs to axial skeleton
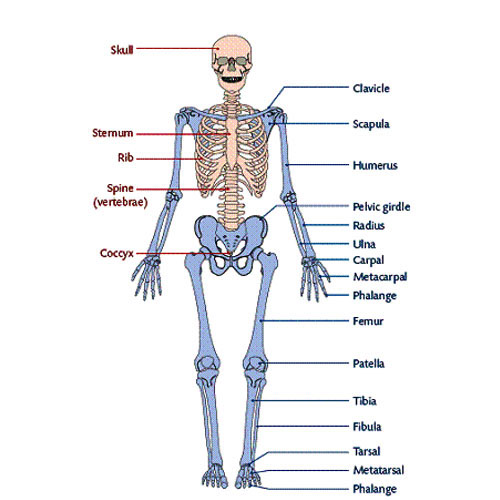
How are bones classified
classified by shape, NOT size
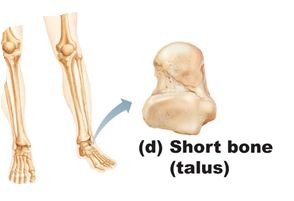
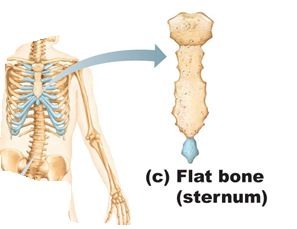
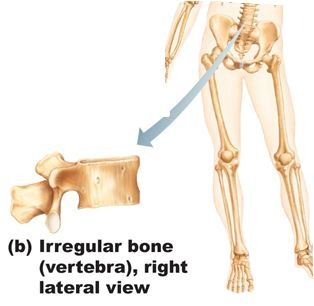
What are the four types of bones
long, short, flat, irregular
Long bones (4)
much longer than wide( shaft + 2 expanded ends)
mostly compact bone with marrow cavity
spongy bone near joint ends
i.e. radius, ulna, phalanges
- all limbs except patella, wrist and ankle
short bones (4)
roughly cube-shaped (i.e. wrist, ankles)
primarly spongy + thin outer layer of compact bone
sesamoid (independent) bones (bone that forms tendons)( ex tendons)
vary in size and # in different individuals
Flat bones (3)
thin, flattened, and sometimes curved
include skull, ribs, sternum, & scapula and most cranial bones
self-bracing and stronger bc of shape
Irregular bones (2)
complicated shapes: primarily spongy bone + thin covering layer of compact bone
leftovers: e.g. vertebrae and hip bones
Why are bones considered organs
organs have two or more tissues
bones have bone tissue, nervous tissue, cartilage. dense connective tissue, muscle cells and epithelial cells in its blood vessels
Gross Anatomy of Bones (2)
Compact and spongy bones
Compact bone
dense outer layer on every bone that appears smooth and solid/ very organized structure
Spongy (cancellous) bone:
Made up of a honeycomb of small, needle like or flat pieces of bone called trabeculae
open spaces between trabeculae are filled with red or yellow bone marrow
2 types of lining
periosteum
endosteum
periosteum
- outer fibrous layer+ inner osteogenic layer
endosteum
covers inside portion of compact bone + spongy bone and lines canals of compact bone
Structure of short, irregular and flat bones
All have similar structure
thin plates of spongy bone covered by compact bone
Compact bone covered with periosteum & spongy bone lined with endosteum
Not cylindrical so no shaft, marrow cavity or epiphyses – but do contain bone marrow between trabeculae
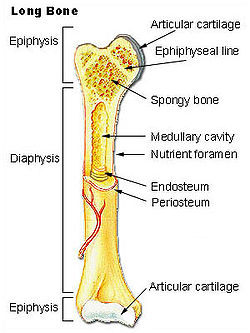
Structure of Long bone
all long bone have a shaft( diaphysis), bone ends( epiphyses) and membranes
Diaphysis (3)
tubular shaft of long bone
the collar of compact bone surrounding marrow cavity (medullary cavity)
in adults, medullary cavity contains fat called the yellow bone marrow cavity
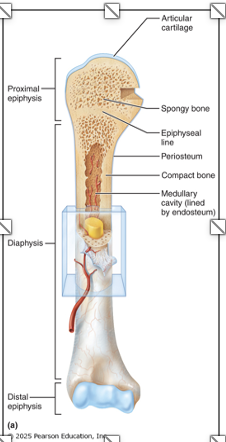
Epiphyses (sing. = epiphysis)
extremities of long bone; expanded for articulation with other bones
compact bone forms the thin outer layer; interior filled with spongy bone
has a thin layer of hyaline (articular) cartilage to cushion the meeting of two bones
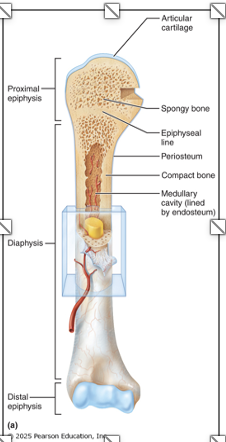
Epiphyseal line
lies between diaphysis & each epiphysis
- remnant of epiphyseal plate
Bone textures (2)
- Calcium salts give hardness & strength for support/protection of softer tissues
- cavities for fat storage & synthesis of blood cells
Osteogenic( osteoprogeniotor) cells
stem cells that differentiate into osteoblasts
Osteoblasts
- bone growth (immature, rapidly dividing)
- reabsorbing cells that release Ca and P
Osteocytes
mature bone cells that monitor and maintain minerals in the bone matrix
What does a compact bone( lamellar bone) consist of
osteon
canals and canaliculi
interstitial and circumferential lamellae
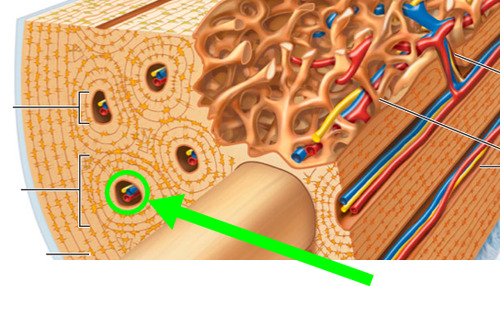
Osteon
this is the structural unit of compact bone (also called lamellar bone)
it's an elongated cylinder oriented parallel to the long axis of bone and acts as tiny weight bearing pillars
a single one is a group of hollow tubes of bone matrix
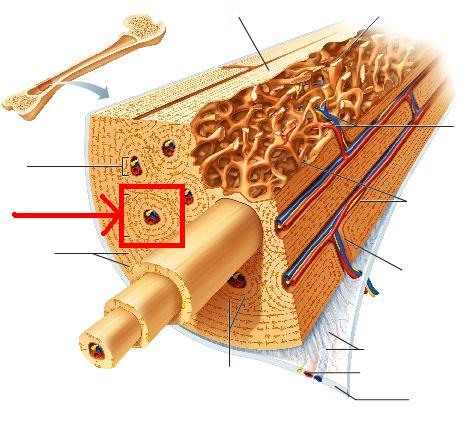
Haversian (central) canal of compact bone
- one in each osteon
- hold blood vessels, nerve fibres, etc.
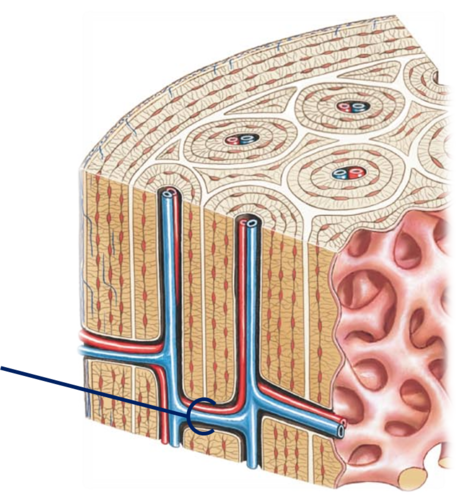
Volkmann's (perforating) canal of compact bone
canals lined with endosteum that occur at right angles to central canal
Connect blood vessels and nerves of periosteum, medullary cavity, and central canal
Canaliculi
hairlike canals that connect lacunae to each other and to central canal
Enables communication between all osteocytes of osteon and permit nutrients and wastes to be relayed from one cell to another
Interstitial lamellae
Some fill gaps between forming osteons; others are remnants of osteons destroyed by bone remodeling
Circumferential lamellae
sheets of bone located just deep to periosteum; extend around entire circumference of shaft / Help long bone to resist twisting
Trabeculae of spongy bone
contains trabeculae, lamellarly arranged osteocytes & canaliculi
arranged along lines of stress; helps bone to resist stress
only a few cell layers thick
there are no osteons
nutrients diffuse through canaliculi from the marrow spaces between the trabeculae to reach the osteocytes
what is the chemical composition of bone( 2)
organic and inorganic components
Organic composition of bone
Includes osteogenic cells, osteoblasts, osteocytes, bone-lining cells, osteoclasts, andosteoid
Osteoid
is a fluid which makes up one-third of organic bone matrix, is secreted by osteoblasts
Consists of ground substance and collagen fibers, which contribute to high tensile strength and flexibility of bone
Inorganic composition of bone
remaining 2/3 of bone
Hydroxyapitites
Hydroxyapitites( mineral salts)
Makeup 65% of bone by mass
Consist mainly of tiny calcium phosphate crystals in and around collagen fibers
Responsible for hardness and resistance to compression
Mechanisms of bone formation
Osteogenesis or Ossification
Osteogenesis or Ossification
is the process of bone tissue formation and includes formation of bony skeleton in embryos
growth of bones during childhood & adolescence
remodelling/repair of bones in adults
Intermembraneous Ossification
bone develops from fibrous CT membrane containing mesenchymal cells
cranial bones of the skull and the clavicles - these are flat bones
Begins at about 8 weeks of development and are called membrane bones
What are the four major steps involved in intramembranous ossification
1) Ossification centers are formed when mesenchymal cells cluster and become osteoblasts
2) Osteoid is secreted, then calcified
3) Woven bone is formed when osteoid is laid down around blood vessels, resulting in trabeculae
4) Lamellar bone replaces woven bone, and red bone marrow appears
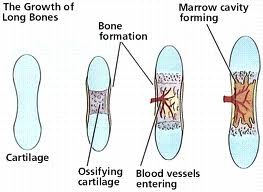
Endochondral Ossification
bone development via the replacement of a hyaline cartilage model
all bones below the skull (except the clavicles)
more complex than intermembraneous
begins in 2nd month
Endochondral ossification steps
①A bone collar forms around the diaphysis of the hyaline cartilage model
②Cartilage calcifies in the center of the diaphysis and then develops cavities.
③The periosteal bud invades the internal cavities and spongy bone forms
④The diaphysis elongates and a medullary cavity forms. Secondary ossification centers appear in the epiphyses
⑤The epiphyses ossify. When ossification in complete, hyaline cartilage remains only in the epiphyseal plates and articular cartilages
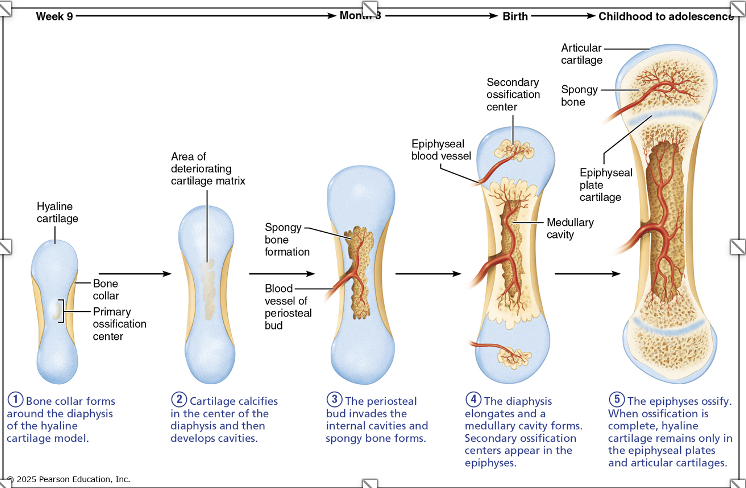
When secondary ossification is complete, hyaline cartilage remains on
- on the epiphyseal surfaces as the articular cartilages
- at the junctions of diaphysis and epiphyses where it forms the epiphyseal plates (this is where long bones continue to grow)
Postnatal bone growth
during infancy & youth, long bones lengthen entirely by interstitial growth of the epiphyseal plates
all bones grow in thickness by appositional growth
most bones stop growing during adolescence or in early adulthood but some facial bones (e.g.nose & lower jaw) continue to grow throughout life
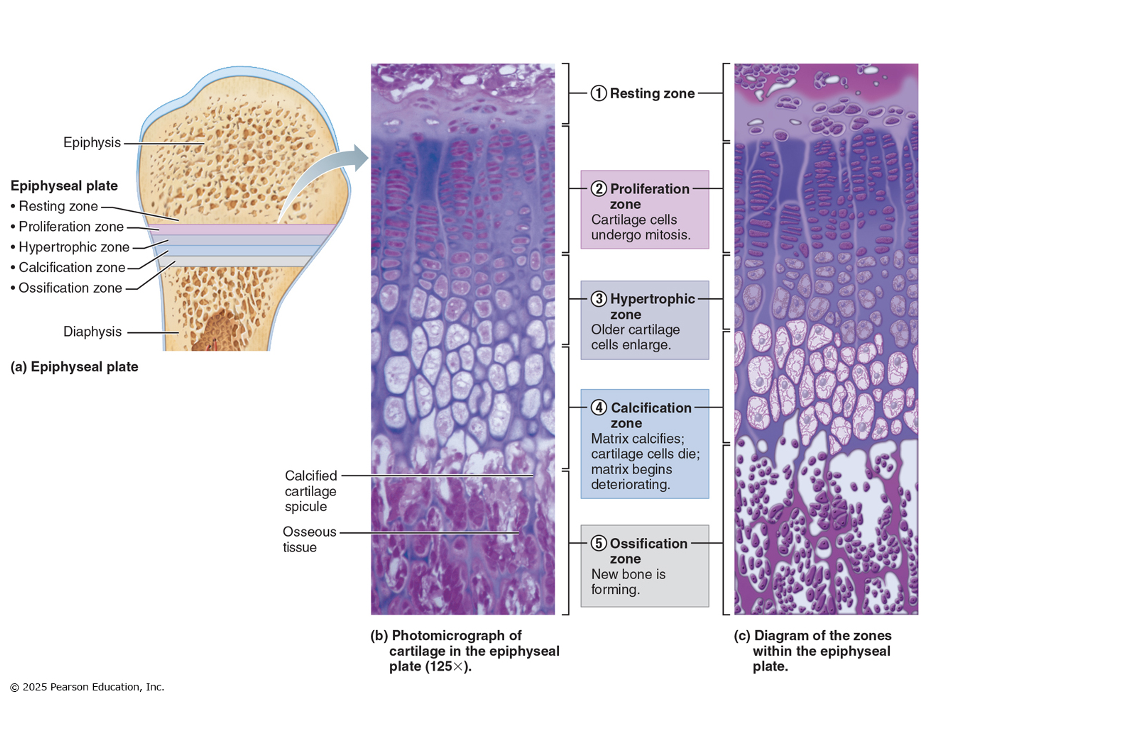
Epiphyseal plate
stays same size throughout childhood & adolescence
becomes thinner at the end of adolescence (cartilage cells in zone 1 multiply more & more slowly)
Longitudinal growth ends when bone of the epiphysis & diaphysis fuses = closure of this
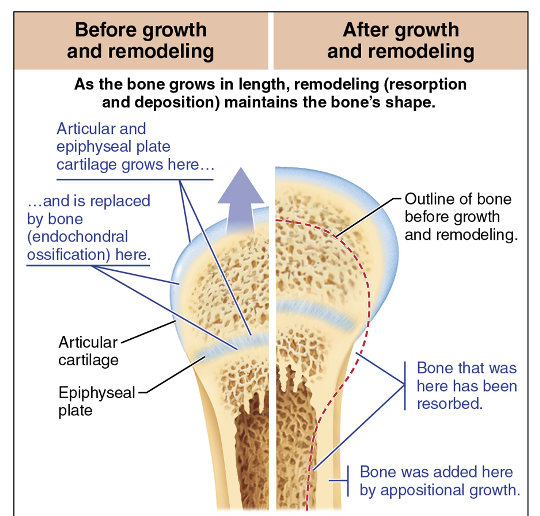
Bone Remodelling
- As the long bone lengthens, the shape of the ends must be altered
- Growing bones widen as they lengthen through appositional growth
- As the length increases, external surfaces of the ends made slimmer while the internal surface made thicker
- Bone is destroyed by osteoclasts and laid down by osteoblasts on both the inner and outer surfaces of a growing long bone
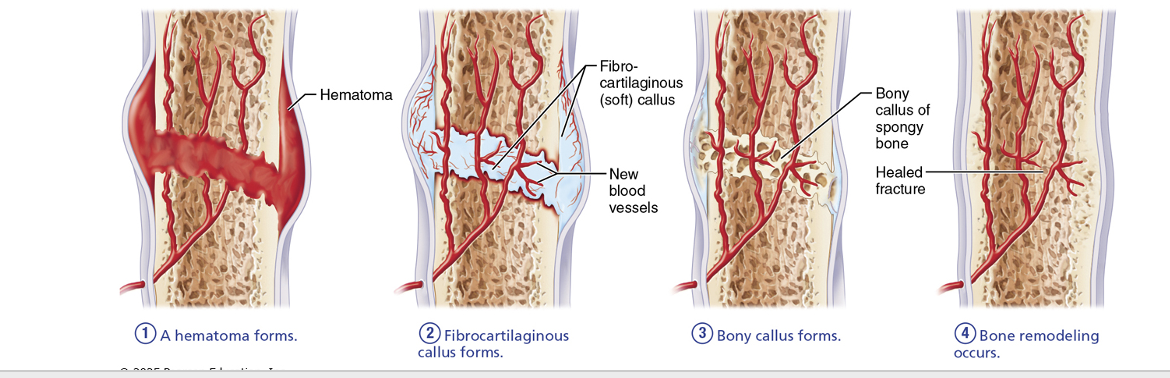
What are fractures
Fractures are breaks
– During youth, most fractures result from trauma
– In old age, most result from weakness of bone due to bone thinning
What are the four major stages for repair of bones
1) Formation of a hematoma – local bone cells are deprived of oxygen and die; inflammation causes pain.
2) Formation of a fibrocartilaginous callus (soft) – invaded by blood vessels that also bring macrophages to clean up the area; osteoclasts also resorb damaged bone; fibroblasts, chondroblasts, osteoblasts get busy laying down collagen fibers and tissue components to span the break
3) Conversion to bony callus – cartilage converted to trabecular bone – complete in ~2 months
4) Bone remodelling – any extra bony material is removed; outer bone of shaft walls converted to compact bone and bone regains original shape
Final structure resembles original structure
▪ Responds to same mechanical stressors
Hormonal Regulation of Bone Growth in Childhood
- Growth hormone (GH) stimulates epiphyseal plate activity in infancy and childhood
- Thyroid hormone modulates activity of GH, ensuring proper proportions
Hormonal Regulation of Bone Growth at puberty: Testosterone and estrogens
End growth by inducing epiphyseal plate closure
Bone remodelling
consists of both bone deposit and bone resorption
occurs at surfaces of both periosteum and endosteum
Remodelling Units
packets of adjacent osteoblasts and osteoclasts coordinate remodelling process
Resorption is the function of what
osteoclasts
What do the osteoclasts do
Dig depressions or grooves as they break down matrix
Secrete lysosomal enzymes and protons (H+) that digest matrix
Acidity converts calcium salts to soluble forms
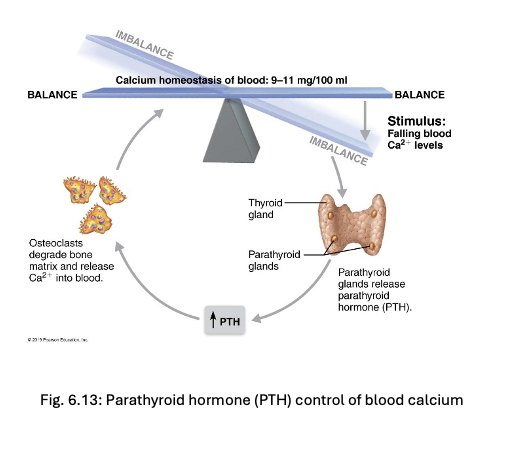
Osteoclast activation involves PTH (parathyroid hormone)
What is bone matrix deposited by
osteoblasts
Osteoid seam
band of unmineralized bone matrix that marks area of new matrix
Calcification front
abrupt transition zone between osteoid seam and older mineralized bone
When is spongy bone replaced
every 3-4 years
When is compact bone replaced
every 10 years
Bone remodelling hormonal controls: PTH
Produced by PT glands
Removes calcium from bone regardless of bone integrity
negative feedback loop
Calcitonin
released from parafollicular cells of thyroid gland in response to high levels of blood calcium levels. Effects are negligible, but at abnormally high doses it can lower blood Ca2+ levels temporarily.
Bone remodelling: Response to mechanical stress
Bones reflect stresses they encounter they are stressed when weight bears on them or muscles pull on them
- Wolfe's law
Wolfe's Law
Stress is usually off center, so bones tend to bend
Bending compresses one side, stretches other side
Diaphysis is thickest where bending stresses are greatest
Bone can be hollow because compression and tension cancel each other out in center of bone
Osteoporosis
Bone resorption outpaces bone formation making bone becomes porous
some areas of skeleton especially vulnerable: spine, neck of femur
Osteoporosis risk factor: age
estrogen & testosterone promote bone health by restraining osteoclast activity and promoting deposition of new bone
Osteoporosis contributing factors
Other contributing factors include
● insufficient exercise
● diet poor in calcium & protein
● smoking (reduces estrogen levels)
● Genetics
● Diabetes mellitus
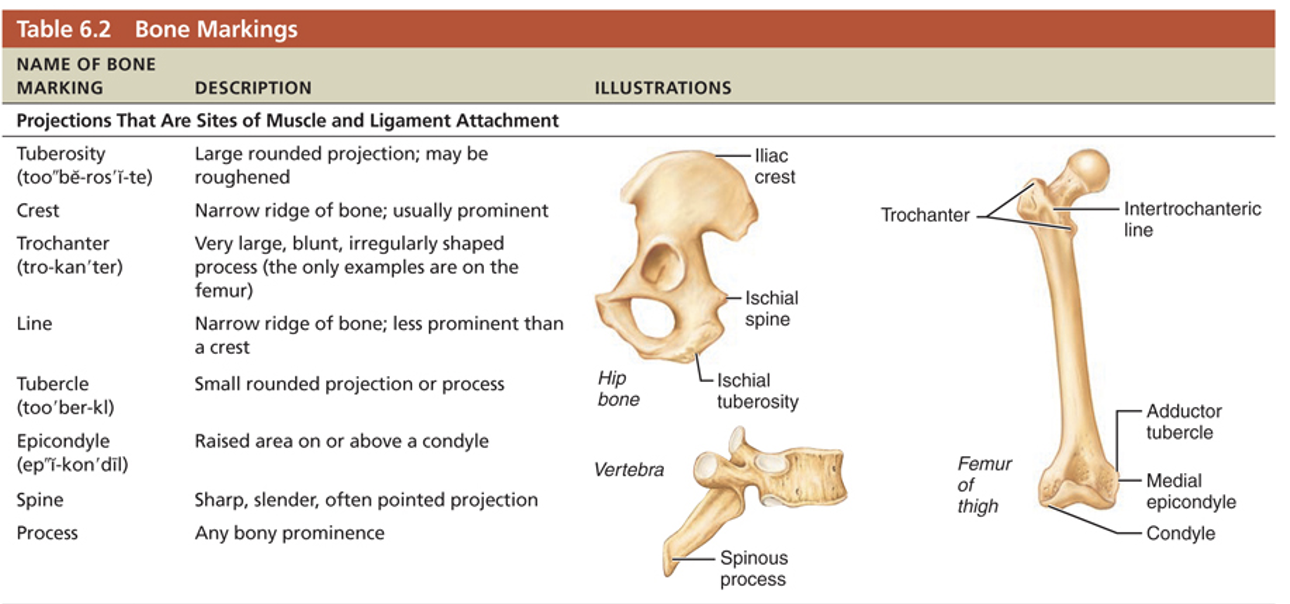
Bone markings
Sites of muscle, ligament, and tendon attachment on external surfaces
Areas involved in joint formation or conduits for blood vessels and nerves
What are the three types of markings
Projection: outward bulge of bone
● Depressions and openings
● Surfaces
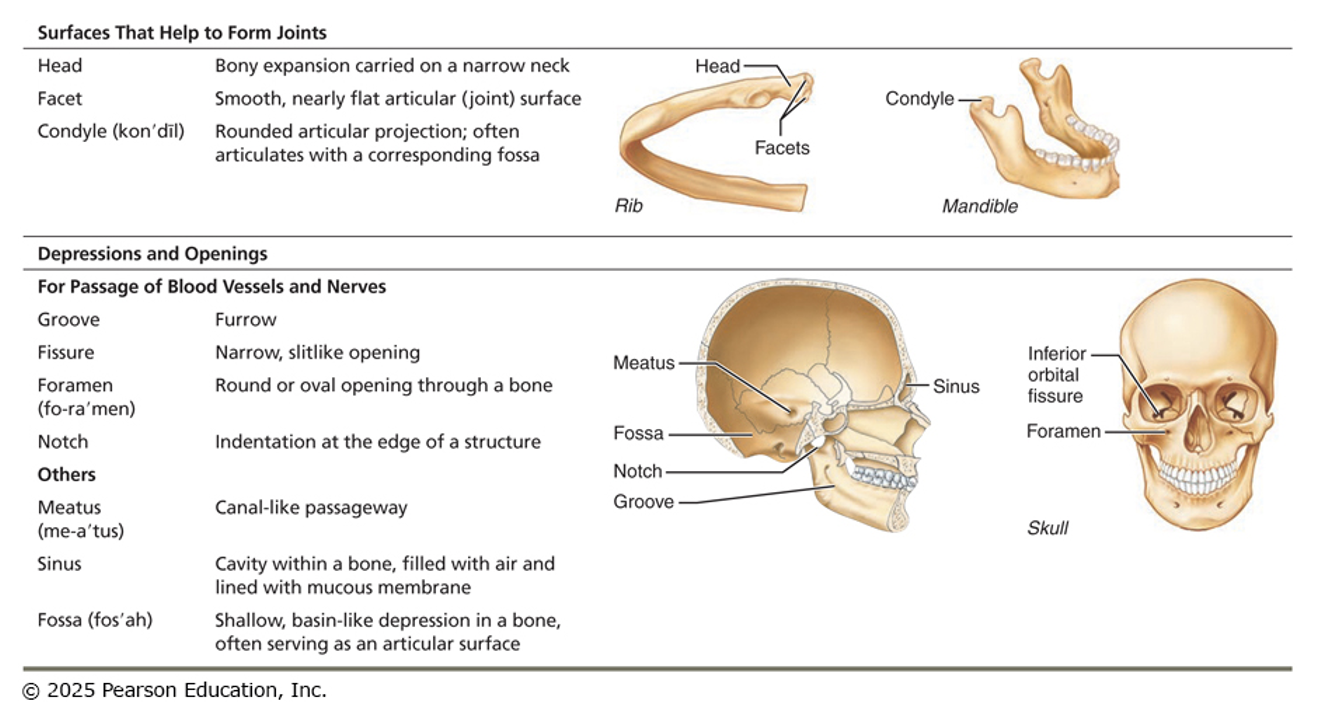
Bone markings
study pictures