Unit 6B - Regulation of GI
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
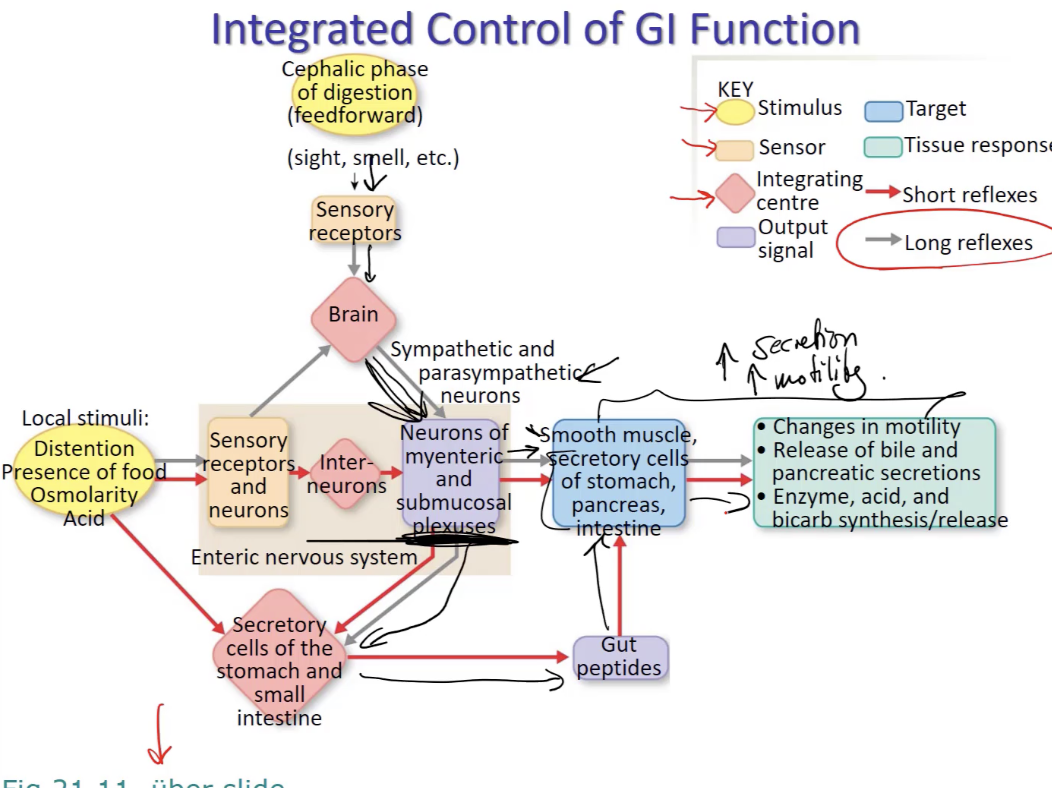
where are long reflexes in the GI tract integrated
in the cns (brain)
where are short reflexes in the GI tract integrated
within the gut (in the enteric (“gut brain”) nervous system)
how do long reflexes work in the GI tract
afferent info comes in → (varying) sensory info comes in from eyes, ears, nose, thought of food, etc → can be cephalic or local stimuli
goes to CNS
evoke responses that get GI tract up and running
serves as feedforward signal (anticipating change)
efferent info is always same → autonomic response → inc (excite) parasympathetic (rest and digest) response and decrease (inhibit) sympathetic
neurons of myenteric and submucosal plexuses
inc smooth muscle and secretory cell activation
secretory cells of stomach and small intestine → gut peptides
note: happens before food is even ingested
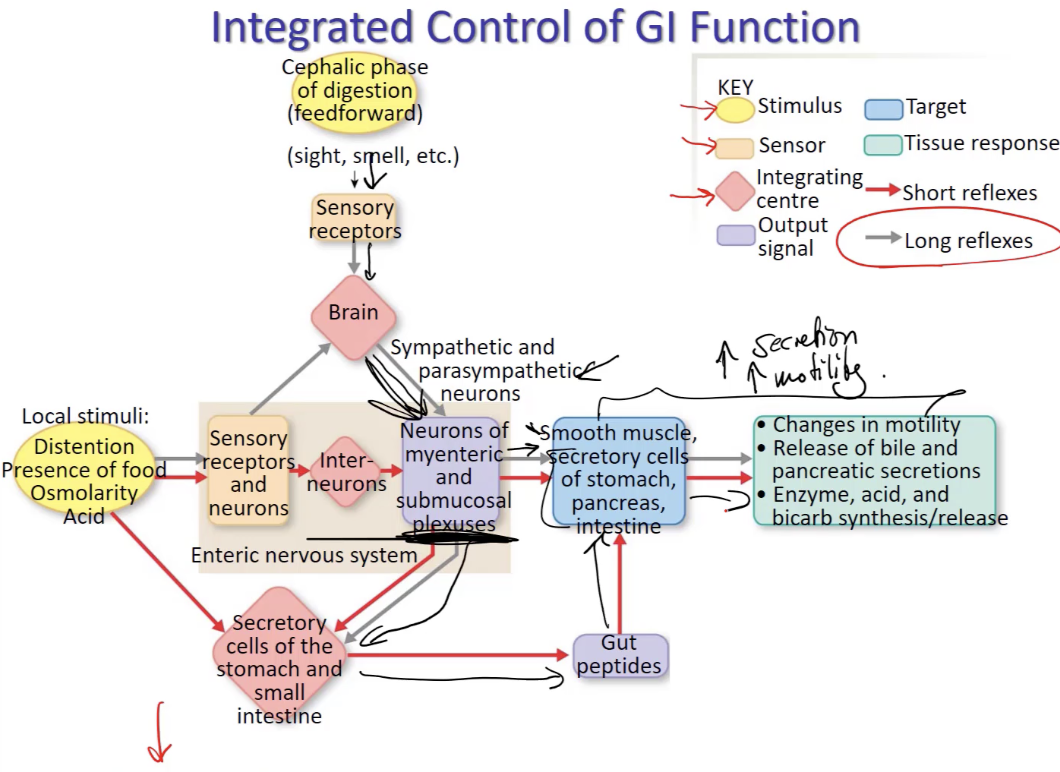
how do short reflexes work in the GI tract? (hint: what regulates secretion vs motility)
only local stimuli work to trigger short reflexes (eg presence of food) and sends signals to…
neurons in submucosal plexus → regulate secretion
neurons in myenteric plexus → regulate motility
note: happens before food is even ingested
what is the cephalic phase of digestion
the first phase of digestion, occurring before food even enters the stomach. It's triggered by the sight, smell, taste, or even thought of food, initiating a cascade of physiological responses aimed at preparing the body for the incoming meal
what are some similarities between the enteric and central NS
have intrinsic neurons that lie entirely within gut (like interneurons of CNS)
autonomic neurons that bring signals from CNS to gut are “extrinsic”
releases lots of diff neurotrans
has glial cells (similar to astrocytes in blood brain barrier)
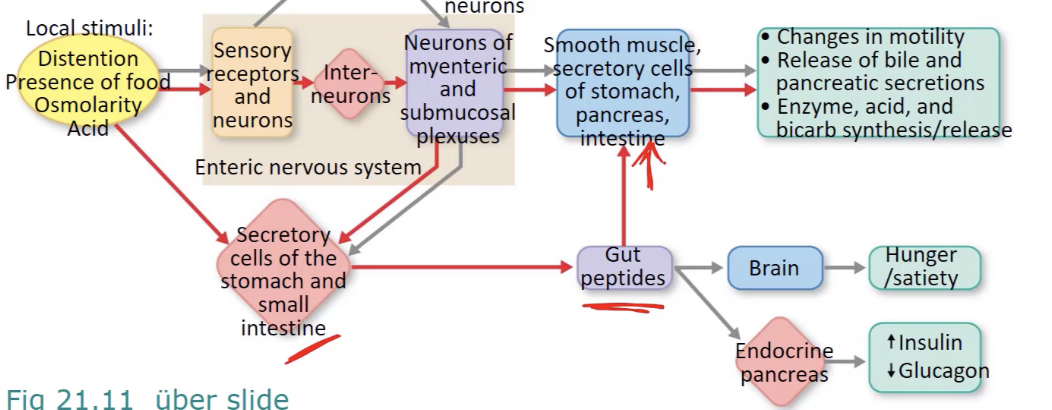
explain how reflexes involving gut peptides typically work (and where they’re produced / how they act / what kinds of responses they evoke)
produced by cells w in lamina propria
can act locally (paracrine) or travel via blood (endocrine)
act on motility → alter peristalsis, gastric emptying, etc
act on secretion → both exocrine and endocrine secretion
endocrine happens by talking to pancreas (inc insulin, dec glucagon) or brain (inc hunger)
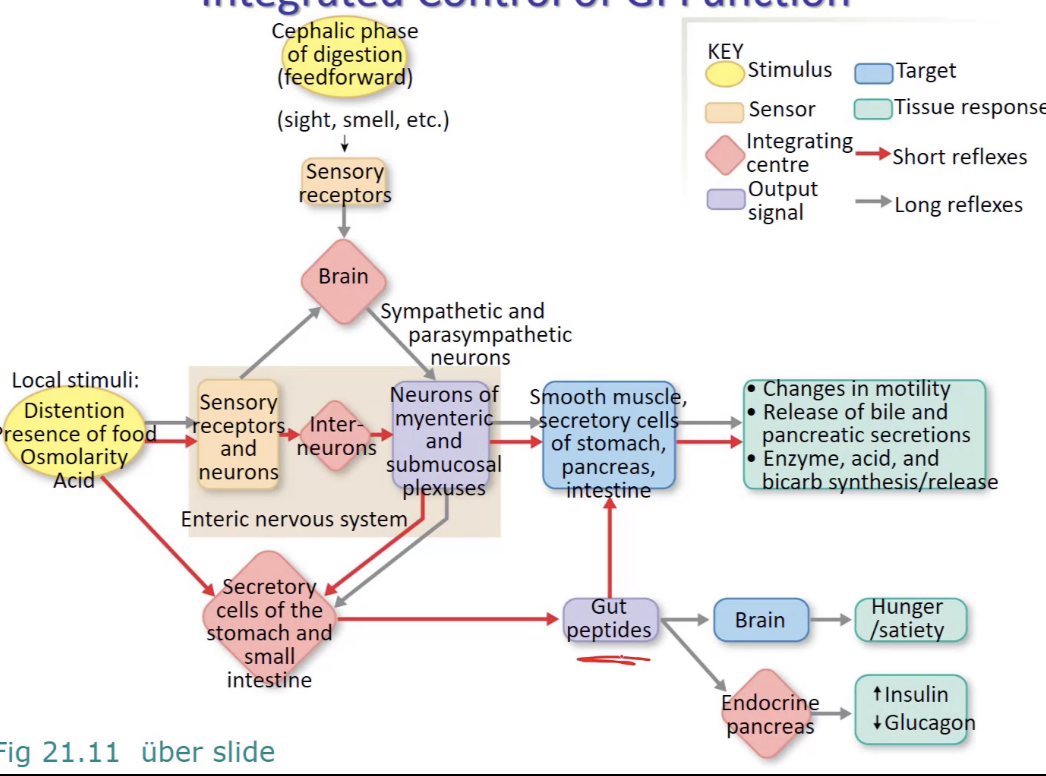
t/f: some gut peptides act on brain
true - like inhibiting hunger (CCK, PYY, GLP-1) (dorian, 2025)
do long or short reflexes stimulate gut peptide secretion
both (long = grey, short = red)
explain the beginnings of endocrinology (site pavlov & bayliss and staring)
PAVLOV:
H+ from stomach travels through duodenum
pancreas knows exactly when to secrete pancreatic juice (containing bicarb to inc pH) into duodenum when H+ enters → but didn’t know how pancreas knew
PAVLOV (dog guy) thought that there were afferent signals that went up from duodenum to brain then efferents that went from the brain to the pancreas to let it know to secrete pancreatic juice into duo
thought both of those signals were from vagus nerve (vagal signals)
thought ONLY neural
BALYISS AND STARLING:
dissected (got rid of) all nerves surrounding pancreas and duodenum
put acid in duo
BUT pancreas still secreted
:. thought acid caused release of signal from duo into blood
SO collected lining of duo and added acid to it (injected that combination into another organism → found the PANCREAS SECRETED JUICES (bicarb))
concluded a factor from the intestine went into blood and stimulated secretion → called it “secretin”
general term coined for blood-borne regulators → hormones
what are the gastrin, secretin, and motilin families
families of gut hormones
gastrin → major targets are stomach (gastrin), intestine, and accessory organs
secretin → vasoactive intestinal peptides
stimulates bicarbonate
inhibits gastric acid secretion and motility
motilin → acts on gut smooth muscle
what is a bolus
a mass of chewed food mixed with saliva that is ready to be swallowed
explain the swallowing reflex
tongue pushes bolus against soft plate and back of mouth, triggering swallowing reflex
breathing is inhibited as bolus passes closed airway
food moved downward into esophagus, propelled by peristaltic waves (series of involuntary, wave-like muscle contractions → move food) and aided by gravity
what does the epiglottis do
flap that keeps either one of esophagus or trachea closed at a time to open the other one
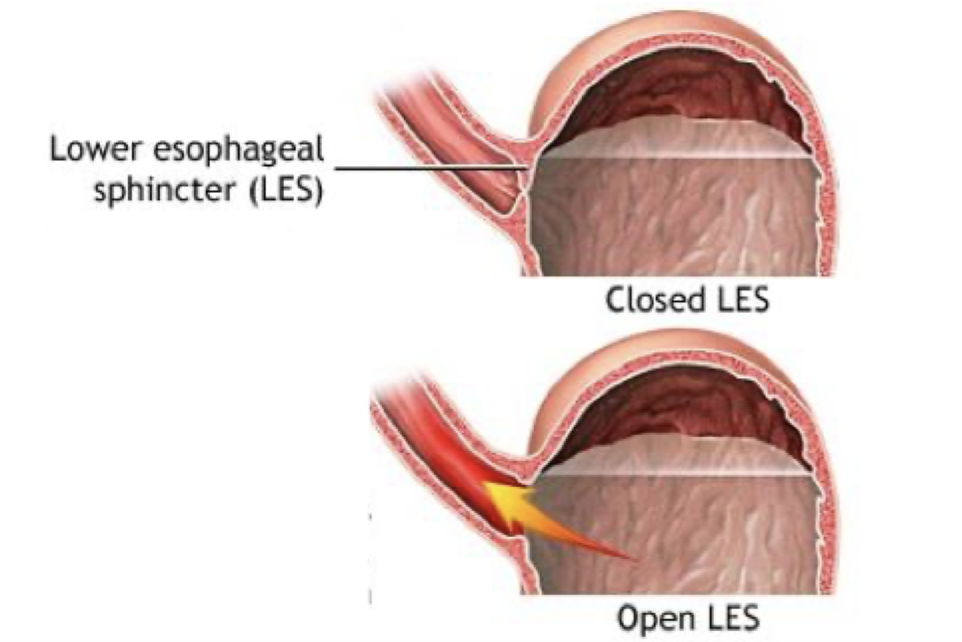
what is the lower esophageal sphincter? what kind of contraction does it abide by
guards entry into stomach
tonically contracted ring of smooth muscle
what happens if the lower esophageal sphincter is left open
acid from stomach can splash up into lower esophagus….
during respiration (when intrathoracic pressure drops)
during churning of stomach
results in gastroesophageal reflux disease (GERD)
produces heartburn
give an overview of the gastric phase of digestion
initiated w long vagal reflex (during cephalic phase)
once food enters stomach, series of short reflexes → gastric reflexes
explain the 3 functions of the stomach in gastric phase
storage
through receptive relaxation of upper stomach
digestion
mechanical and chemical processing into chyme
protection
acid protects against microbes
also self-protection from acid w mucus-bicarbonate barrier
explain the cephalic and gastric phases of digestion
Cephalic phase:
anticipation of food/presence of food in mouth
CNS activation (medulla)
vagus nerve sends signals to ENS (enteric NS)
inc secretion and motility
prepares GI tract before food reaches stomach
Gastric Phase:
food in stomach
short and long reflexes
further inc secretion and motility
what do mucous neck cells secrete in the gastric gland?
tonically secretes mucus (that creates a physical barrier btwn lumen and epithelium) and bicarbonate
what is the diff between gastric acid and hydrochloric acid
Gastric acid → overall acidic solution produced by the stomach
intrinsic factors
HCL
Pepsinogens
hydrochloric acid → key component of gastric acid
what do intrinsic factors do
bind to vitamin B12 so they can more easily be absorbed in the ilium
what do parietal cells secrete from the gastric glands? what does it do
triggers HCl and intrinsic factor release
HCl → acidity denatures proteins, making them more succeptible to pepsin activity → activates pepsin which breaks down proteins, kills bacteria
intrinsic factors compete w Vitamin B12 to permit absorption
what do chief cells secrete from the gastrin glands? what does that do?
triggers pepsinogen and gastric lipase release
pepsinogen digests proteins when activates (it’s an endopeptidase)
particularly effective on collagen (meat digestion)
gastric lipase is a minor contributor in fat digestion (co-secreted w pepsinogen)
what do enterochromaffin-like (ECL) cells secrete from gastric glands and what does that do
receive gastrin signals from BLOOD STREAM secreted by G cells and release histamine
binds to H2 receptors on parietal cells → promotes even more HCl secretion
what do G cells secrete from gastric glands and what does that do
promote gastrin release into BLOODSTREAM in response to vagus nerve (long reflex) and/or AAs/peptides (short reflex, sensed by enteric sensory neurons)
triggers HCl release both directly by binding to parietal cells or indirectly by ECl cells (make them release histamine which would THEN go to parietal cells and promote more HCl release)
what do D cells release from gastric glands and what does that do
releases somatostatin when stomach pH is too low
inhibits…
gastrin secretion (G-cells)
histamine secretion (ECL cells)
HCl secretion (parietal cells)
pancreatic secretions and intestinal hormones
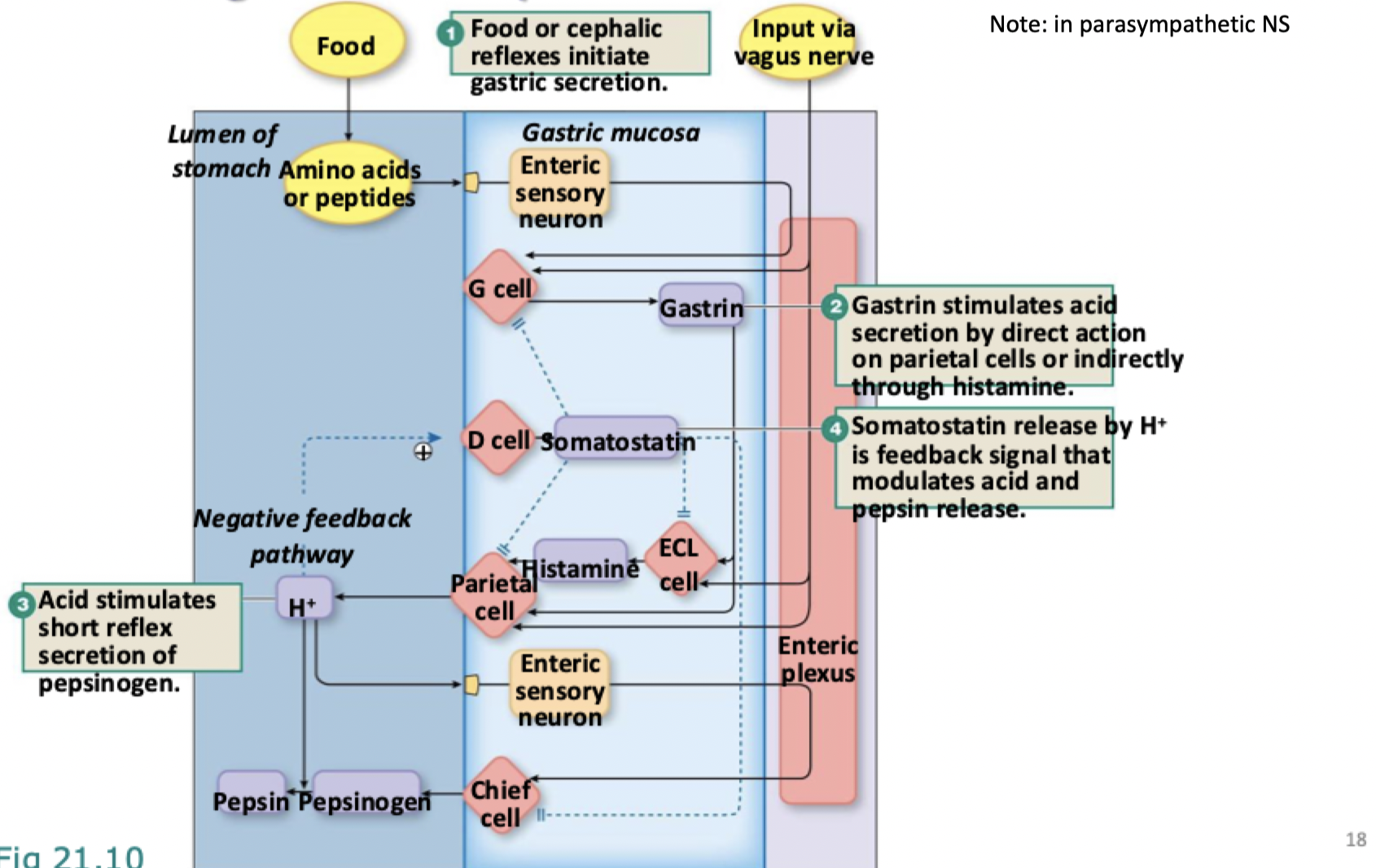
explain the integration of cephalic and gastric phases
food or cephalic reflexes initiate gastric secretion (from G cells)
gastrin stimulates acid secretion by direct action on parietal cells or indirectly through histamine (released by ECL cells)
acid stimulates short reflex secretion of pepsinogen (by chief cells)
in other words…
Havent eaten yet, input via vagus nerve (resulted from things stomulating you before eating) comes down to stomach
Hits g cells which release gastrin -> gastrin stimulates acid secretion by BOTH direct action on parietal cells or indirectially through histamine (does both so either works)
Acid stimulates the short reflex secretion of pepsinogen (acid triggers chief cells that stimulate release of pepsinogen which is then turned into pepsin
Somatostatin releasesed by H+ is feedback signal that modulates that acid and pepsin releease
When food is taken in in the gastric phase, the peptides and amino acids send signals that go to the G cells that secrete gastrin, etc. etc.
G cells are crutial
explian the mucus-bicarbonate barrier in the stomach
Bicarb gets put in mucus -> lines the epithelial cells of the stomach -> the acid eats away at the epithelium if comes in contact so that physical barrier buffers it and stops it from touching
how the stomach protects itself
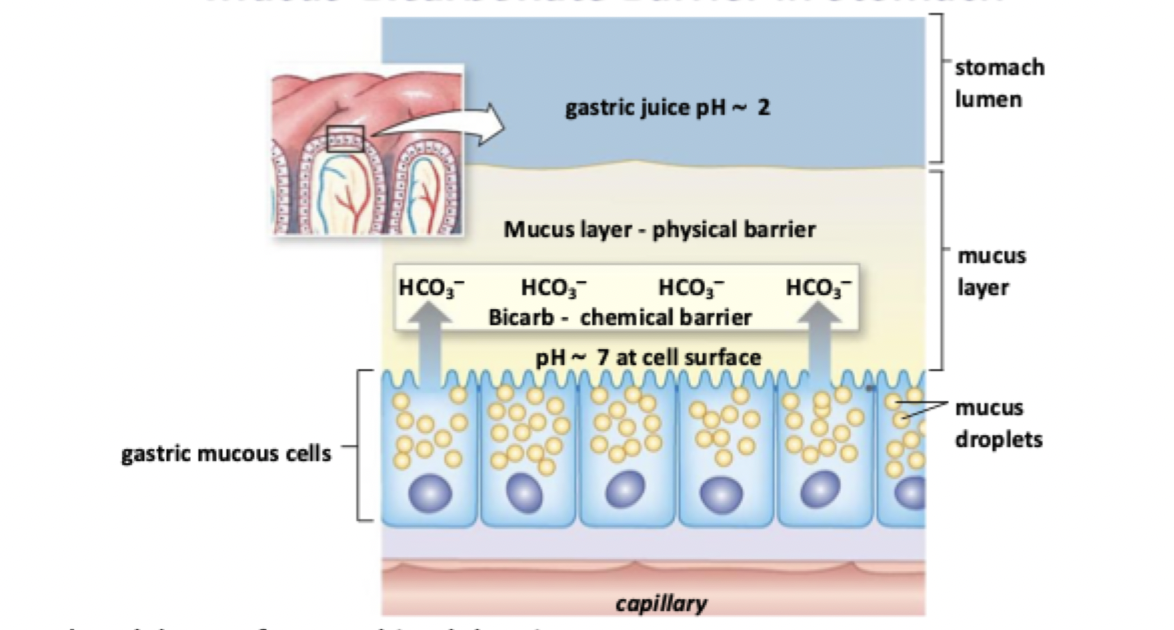
what causes peptic ulcers
caused when acid and pepsin damage mucosal surface, creating holes that extend into submucosa and muscularis layers
explain the diff between the pH in the stomach lumen and the pH in parietal cells
pH stomach can be as low as pH = 1
pH in parietal cells is around 7.2 so [H+] is a million times higher in the stomach lumen
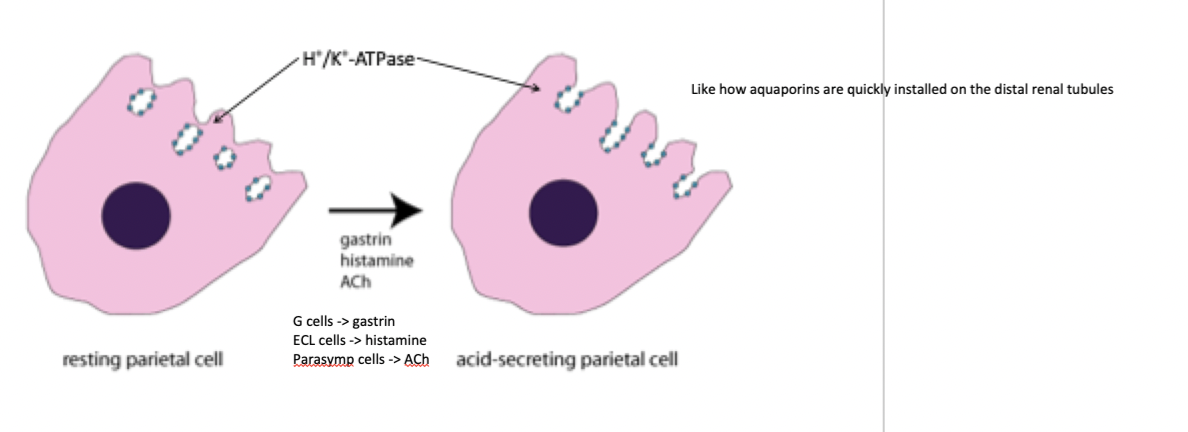
what are the 3 types of chemical signals that can activate parietal cells
gastrin, histamine, and ACh
explain how the proton pumps on parietal cells work
when parietal cells come into contact w histamine, ACh, or gastrin, they bring their proton pumps to the surface and start secreting H+ into lumen of stomach and bicarb into blood (like AQP secretion)
as H+ is secreted from the apical side of the parietal cell via proton pump, bicarb (from CO2 and OH- is absorbed into the blood (called the alkaline tide - can be measured after a meal)
note: review from 6A
what is are old and newer prevention/treatment methods for peptic ulcers
main treatment was antacids
substances that neutralized gastric acid (BUT the acid was still produced)
more modern treatments target parietal cells so they can’t help produce HCl anymore
H2 receptor antagonists → block histamine action
H2 is the type of histamine receptor on parietal cells
H2 receptor blockers reduce push of histamine onto parietal cells
proton pump inhibitors
block proton pump on parietal cells
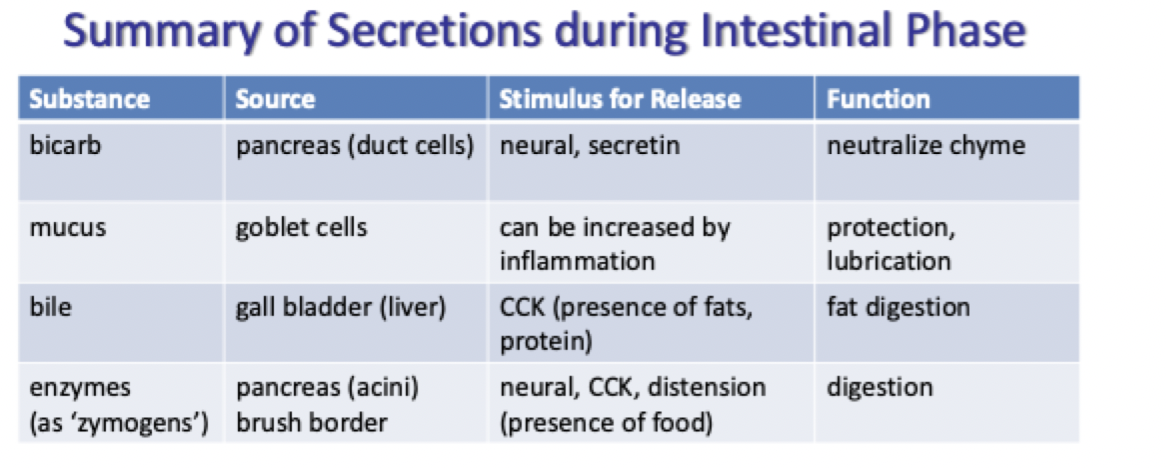
what happens when the intestinal phase begins
stomach produces chyme by actions of acid, pepsin, and paristalsis (constriction and relaxation of the muscles of the intestine or another canal, creating wave-like movements that push the contents of the canal forward)
intestinal phase begins w controlled entry of chyme into small intestine
sensors in duodenum feed back to stomach to control delivery of chyme
feed forward to intestine to promote digestion, motility, and utilization
how are the gastric and intestinal phases integrated together
what are the duo’s responses to fat, carb, and proteins being in it
in duodenum…
Fats are sensed and lead to release of CCK (chole/cysto/kinin (cholecystokinin))
Carbs (glucose) triggers GLP and GLP-1 receptors (are incretins -> secrete insulin) that trigger insulin secretion (endocrine pancreas as opposed to the other things)
Proteins are sensed and triggers secretin release
All the gut peptides (secretins), along with CCK release and GLP/GLP1 inhibit gastric motility and secretion in the stomach
prevents stomach from dumping too much too fast
allows time for pancreas to secrete insulin, enzymes, and bicarbonate into duodenum
explain the enterohepatic circulation of bile salts
bile salts are released into duodenum
absorbed in terminal ileum
enter portal circulation
travel back to liver
recycled several times during a meal
explain the activation of pancreatic zymogens
pancreatic secretions (including inactive zymogens) enter duodenum
Enteropeptidase (a brush border enzyme) activates trypsinogen (turns it into trypsin) which activates all the other inactive enzymes that break down macromolecules
what is the role of the large intestine
removes the remaining water from the intestines → forms feces
explain motility within the large intestine
ileocecal valve (valve entering ascending colon (first part) of large intestine) relaxes each time a peristaltic wave reaches it
also relaxes when food leaves stomach (called the gastroileal reflex)
segmental contractions w little forward movement except when mass movements occur (3-4 times per day)
wave of contractions that send bolus (food mass) forward
trigger distention (dilating) of rectum → defecation reflex
what causes diarrhea
an imbalance between intestinal absorption and secretion
what causes osmotic diarrhea
caused by unabsorbed osmotically active solutes
undigested lactose, sorbitol (artificial sweetener) or olestra (fake fat)
osmotic laxatives
what causes secretory diarrhea
bacterial toxins that increase Cl- secretion
eg cholera
diarrhea can be adaptive (flushing out infection) → can also lead to dehydration and metabolic acidosis
what is vibro cholerae? explain what they do and how that relates to Cl-
the bacteria that causes cholera (the disease)
from contaminated food (usually in developed countries)
from contaminated water (usually in developing countries)
Process:
toxin enters cell via pentameric B subunits (is endocytosed into cell where it would normally be gotten rid of)
travels in retrograde direction through golgi (back to ER)
mimics missfoled protein and gets dumped out into cytosol (normally degraded)
instead of being degraded, it acts on the alpha subunit of the G protein → makes it constantly bound to GTP
persistent elevation of cAMP
sustained activation of CFTR channel
constant efflux of Cl from epithelial cells into intestinal lumen
therefore lots of Na and therefore water from interstitial fluid follows (excess water secretion), gives really bad diarrhea
what is the most fatal recessive single-gene in northern europeans and their descendents
cystic fibrosis
why does cystic fibrosis persist if its so bad
CF heterozygoats have some advantage over non-CF homozygotes
heteros have around 50% functioning CFTRs
enough for normal function but allows them to resist death by cholera due to reduced Cl- secretion during infection
cholera didn’t become a big thing until recently though but this same concept most likely applied to earlier diseases as well