IB Sports Med Option C
5.0(1)
Card Sorting
1/70
Last updated 1:54 AM on 5/2/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
1
New cards
C.1 Hypokinetic disease
a disease associated with physical inactivity
2
New cards
Habitual physical activity
What we do everyday, moving to get through the day
3
New cards
exercise
Intentional physical activity to improve physical fitness
4
New cards
types of hypokinetic diseases:
\-> Cardiovascular disease (CVD) \n -> obesity \n ->Type 2 diabetes \n ->Osteoporosis \n -> Mental ill-health \n -> some types of cancer
5
New cards
Coronary heart disease
when coronary arteries are clogged with plaque caused by Atherosclerosis
6
New cards
Stroke
a blood clot in a vessel of the brain, blocks blood and O2 getting to areas of the brain, leading to tissue death
7
New cards
Hypertension
High blood pressure (140/90)
8
New cards
Obesity
Excess of body fat
9
New cards
Type 2 diabetes
Body becomes resistant to insulin produced by the pancreas (best treatment is exercise)
10
New cards
Osteoporosis
Low bone density, its like having holes in the bone, it makes it easier to break (to make it stronger/more dense, we put force to the bone)
11
New cards
C.1.4 Discuss how studies of different populations provide evidence of the link between physical activity and hypokinetic disease
Various populations changed their lifestyles from one of high physical activity (traditional, agricultural-based living) to one of low physical activity ("westernized living")
CHD and stroke account for a large % of deaths in high income countries as we become more sedentary
CHD and stroke account for a large % of deaths in high income countries as we become more sedentary
12
New cards
C.1.5 Discuss the relationship between major societal changes and hypokinetic disease
Examples of changes:
1. proliferation of the motor vehicle
2. changes in employment and working patterns
3. changes in diet
1. proliferation of the motor vehicle
2. changes in employment and working patterns
3. changes in diet
13
New cards
C.2 Cardiovascular disease (CVD)
term given to classify a group of disorders of the heart and blood vessels. (mainly consists of hypertension/high blood pressure, coronary heart disease and stroke)
14
New cards
C.2.1 Outline the coronary circulation
coronary circulation: how blood transfers through heart & how blood supplies itself
15
New cards
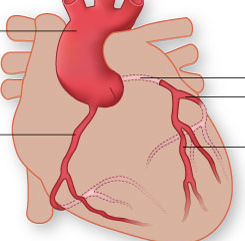
your leftmost and highest
Left and right coronary arteries
\
\
16
New cards
2nd arrow left
circumflex artery
17
New cards
lowest arrow
left anterior descending artery
18
New cards
C.2.2 Outline what is meant by the term atherosclerosis
hardening of the arteries due to the accumulation of plaque (made up of cholesterol and other substances) in the walls of arteries = blood clot
19
New cards
C.2.3 List the major risk factors for cardiovascular disease (10)
cigarette smoking, high blood pressure (hypertension), high cholesterol and LDL-cholesterol, low HDL-cholesterol, diabetes, obesity, physical inactivity, age, gender, ethnicity and family history.
20
New cards
C.2.4 Explain the concept of risk factors in cardiovascular disease
Can be sometimes clustered together. Clustering three or more factors together is sometimes called metabolic syndrome. Major components (high triglyceride - blood fat and low levels of HDL- Cholesterol), impaired glucose regulation or diabetes, (particular abdominal obesity) increases risk of CVD
21
New cards
Show Exercise may lower the risk of CHD (4 reasons)
\-may have direct effects on the heart
\-increasing the size of the coronary arteries and making them less likely to get blocked
\-improves endothelial function which means that arteries are able to vasodilate (open up) on demand to increase blood supply, reduce the chances of ischemia
\-helps to prevent obesity thus reducing the risk of blood clots forming
\-major positive effect of exercise is helping to maintain high levels of protective high density cholesterol (HDL)
\-increasing the size of the coronary arteries and making them less likely to get blocked
\-improves endothelial function which means that arteries are able to vasodilate (open up) on demand to increase blood supply, reduce the chances of ischemia
\-helps to prevent obesity thus reducing the risk of blood clots forming
\-major positive effect of exercise is helping to maintain high levels of protective high density cholesterol (HDL)
22
New cards
C.2.5 Discuss how a lifestyle of physical inactivity increases the risk of cardiovascular disease (4 increased risks of CHD)
high blood pressure, obesity, type 2 diabetes, low HDL Cholesterol
23
New cards
C.3.1 Describe how obesity is determined (along with limitations on calculations)
Obesity is by definition an excess of body fat, but in reality it is determined using indirect measurements of body, for example body fat index BMI (kg/m^2) and waist circumference
24
New cards
underweight BMI
less than 18.5
25
New cards
A BMI normal
between 18.5 and 25
26
New cards
A BMI overweight (Obese I)
25-30
27
New cards
A BMI = obese (Obese II)
30-40
28
New cards
A BMI morbid obese (Obese III)
40+
29
New cards
BMI Cons
Values can be often misleading - bodybuilders weightlifters, large muscles
30
New cards
More accurate assessments of body fat %s: (and their limitations!)
\-> sophisticated imaging techniques, including dual energy x-ray absrptionmetry (DXA), magnetic resonance techniques (MRI), and computed tomography (CT)
\-costly and time consuming
\-costly and time consuming
31
New cards
childhood obesity (3.1)
associated with social stigmatization and bullying.
32
New cards
C.3.2 Outline the major health consequences of obesity (6)
cardiovascular disease and hypertension, type 2 diabetes, osteoarthritis, respiratory problems, bowel cancer.
33
New cards
C.3.3 Discuss the concept of energy balance (3)
Energy Balance is affected mainly by food intake, resting metabolic rate and physical activity.
34
New cards
If Energy intake > energy expenditure
weight gain
35
New cards
If Energy intake < energy expenditure
weight loss
36
New cards
If Energy intake = energy expenditure
stable body weight
37
New cards
C.3.4 Outline how chemical signals arising from the gut and from the adipose tissue affect appetite regulation (steps)
Hormones are produced by the stomach and small intestine after eating and by adipose tissue (leptin). These pass to an appetite control centre in the brain (hypothalamus) that regulates feelings of hunger and satiety.
38
New cards
C.4.1 Compare type 1 and type 2 diabetes (similarity)
both can cause death or hyperglycemia
39
New cards
C.4.1 *Contrast* TYPE *1* Diabetes: (what and who it affects)
autoimmune disorder resulting in the destruction of the insulin-producing cells of the pancreas of young people
40
New cards
main type 1 diabetes treatment
insulin (injections)
41
New cards
*Contrast* TYPE *2* Diabetes: (what and who it affects)
is a disease of insulin resistance in skeletal muscle of obese and older individuals with family history
42
New cards
type 2 diabetes treatments (3)
can be treated with exercise and diet/oral medication and insulin
43
New cards
C.4.2 Discuss the major risk factors for type 2 diabetes (4)
obesity, family history, diet, physical inactivity
44
New cards
C.4.3 outline the health risks of diabetes (4)
blindness, kidney disease, nerve damage and cardiovascular disease.
45
New cards
C.5.1 Outline how bone density changes from birth to old age
Bone mass density increases from birth through to around 35-45 years of age.
46
New cards
Bone density differences in gender
females achieve a lower-peak bone density than males. From this age onwards, bone mass density decreases (esp in women post menopause)
47
New cards
C.5.2 Describe the risk of osteoporosis in males and females
low bone mineral density can lead to osteoporosis which leaves a person more vulnerable to fracturing bones
48
New cards
who is affected most by osteoporosis
females post menopause
49
New cards
3 factors determine whether or not a person develops osteoporosis:
\->Their peak bone mass as a young adult
\->The rate of bone loss with aging
→exercise
\->The rate of bone loss with aging
→exercise
50
New cards
C.5.3 Outline the longer-term consequences of osteoporosis in males and females (3)
loss of independence, development of secondary complications as a result of long-term hospitalization and pneumonia.
51
New cards
C.5.4 Discuss the major risk factors for osteoporosis (5)
lack of dietary calcium, cigarette smoking, slim build (ectomorphy), lack of estrogen associated with early menopause and female triad (athletic amenorrhea) and physical inactivity.
52
New cards
C.5.5 Discuss the relationship between physical activity and bone health (effect of too intense workouts on weight-conscious individuals)
weight- bearing physical activity for bone health, but in some cases, intense training in weight-conscious/young athletes gives rise to low body weight/body fat and eating disorders, leading to menstrual disfunction and bone demineralization (osteoporosis)
53
New cards
C.5.5 Discuss the relationship between physical activity and bone health (Changes in bone density)
site-specific and resistance training results in greater changes than endurance training.
54
New cards
C.6.1 Outline physical activity guidelines for the promotion of good health
150 minutes a week of moderate intensity exercise or 75 minutes of high intensity exercise for 18-64
55
New cards
C.6.2 Describe the aims of exercise in individuals with a hypo kinetic disease (5)
\->to make the most of limited functional capacities
\-> to alleviate or provide relief from symptoms
\-> to reduce the need for medication
\-> to reduce the risk of disease recurrence
\-> to help overcome social problems and psychological distress
\-> to alleviate or provide relief from symptoms
\-> to reduce the need for medication
\-> to reduce the risk of disease recurrence
\-> to help overcome social problems and psychological distress
56
New cards
C.6.3 Discuss the potential barriers to physical activity (4)
\
* uncontrolled disease state (unstable angina, poorly controlled diabetes, uncontrolled hypertension)
* hazards of exercise (for example, cycle and swimming accidents)
* musculoskeletal injuries
* triggering of other health issues (for example, heart attack, respiratory tract infections).
* uncontrolled disease state (unstable angina, poorly controlled diabetes, uncontrolled hypertension)
* hazards of exercise (for example, cycle and swimming accidents)
* musculoskeletal injuries
* triggering of other health issues (for example, heart attack, respiratory tract infections).
57
New cards
C.7.1 Define the term mood
A state of emotional or affective arousal of varying, and nor permanent, duration. Feelings of elation or happiness lasting several hours or even a few days are examples of mood.
58
New cards
\
7\.2 Outline the 2 effects of exercise on changing mood states.
7\.2 Outline the 2 effects of exercise on changing mood states.
\
* research suggests exercise is one of the most effective methods of alleviating a bad mood
* research supports the use of exercise in modifying fatigue, anger, anxiety, depression, and enhancing the positive moods of vigour, clear thinking, energy, alertness, increased sense of well-being.
* research suggests exercise is one of the most effective methods of alleviating a bad mood
* research supports the use of exercise in modifying fatigue, anger, anxiety, depression, and enhancing the positive moods of vigour, clear thinking, energy, alertness, increased sense of well-being.
59
New cards
C.7.3 Outline how exercise enhances psychological well-being (physiologically): 4
increases in cerebral blood flow, changes in brain neurotransmitters (norepinephrine, endorphins, serotonin), increase in maximal oxygen consumption and delivery of oxygen to cerebral tissues, reductions in muscular tension, structural changes in the brain
60
New cards
C.7.3 Outline how exercise enhances psychological well-being (psychologically): 6
distraction from daily hassles and routine, enhanced feeling of control, feeling of competency, positive social interactions, improved self-concept and self-esteem.
61
New cards
C.7.4 Explain the role of exercise in reducing the effects of anxiety
\
acute effects of exercise on state anxiety, compounding effect of intensity and duration of exercise, chronic effects of exercise on trait anxiety
\
acute effects of exercise on state anxiety, compounding effect of intensity and duration of exercise, chronic effects of exercise on trait anxiety
\
62
New cards
C.7.4 Explain the role of exercise in reducing the effects of depression
Exercise has been seen to play a significant role in alleviating depression although it is a correlational relationship; no causal link has been established.
63
New cards
Nature of workout programme for depression (7.4)
enjoyable, aerobic or rhythmic, absence of interpersonal competition, closed and predictable environment, moderate intensity, 20–30 minutes, several times a week
64
New cards
C.7.5 Discuss the potential personal and environmental barriers to physical activity (social environment) 2
feelings that there is no one to exercise with Physical environment and Social and cultural norms
65
New cards
C.7.5 Discuss the potential personal and environmental barriers to physical activity (physical environment) 2
perceptions of being too old or too fat or lack of enjoyment of a particular exercise),
66
New cards
C.7.6 Describe environmental approaches strategy for enhancing adherence to exercise 3 examples
\
prompts, contracting, perceived choice
prompts, contracting, perceived choice
67
New cards
C.7.6 Describe social support approach strategy for enhancing adherence to exercise 4 examples
joining in, adjusting routines, transportation, providing equipment.
68
New cards
C.7.6 Describe goal setting and cognitive approach strategy for enhancing adherence to exercise
associative versus dissociative focus during exercise
69
New cards
C.7.6 Describe reinforcement approaches strategy for enhancing adherence to exercise 3 examples
rewards for attendance and participation, external feedback, self-monitoring
70
New cards
C.7.7 Outline the possible negative aspects of exercise adherence (addiction to exercises)
negative life choices and relationship issues
71
New cards
C.7.7 Outline the possible negative aspects of exercise adherence (5 symptoms)
stereotyped pattern with a regular schedule of once or more daily, increased priority of exercise, negative mood affect with withdrawal, increased tolerance to exercise, subjective awareness of compulsion to exercise.