N354 Exam 1: The Family in Childbirth: Needs and Care
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
1) The laboring client is at 7 c m, with the vertex at a +1 station. Her birth plan indicates that she and her partner took Lamaze prenatal classes, and they have planned on a natural, unmedicated birth. Her contractions are every 3 minutes and last 60 seconds. She has used relaxation and breathing techniques very successfully in her labor until the last 15 minutes. Now, during contractions, she is writhing on the bed and screaming. Her labor partner is rubbing the client's back and speaking to her quietly. Which nursing diagnosis should the nurse incorporate into the plan of care for this client?
A) Fear/Anxiety related to discomfort of labor and unknown labor outcome
B) Pain, Acute, related to uterine contractions, cervical dilatation, and fetal descent
C) Coping: Family, Compromised, related to labor process
D) Knowledge, Deficient, related to lack of information about normal labor process and comfort measures
Answer: B
Explanation:
A) The client is not exhibiting fear or anxiety, but acute pain; therefore, this diagnosis does not fit.
B) The client is exhibiting signs of acute pain, which is both common and expected in the transitional phase of labor.
C) There is no evidence regarding the family's coping, only the client's coping with the pain.
D) The client used breathing and relaxation techniques earlier in labor, demonstrating knowledge of these techniques.
Page Ref: 498
2) A client is admitted to the labor and delivery unit with contractions that are regular, are 2 minutes apart, and last 60 seconds. She reports that her labor began about 6 hours ago, and she had bloody show earlier that morning. A vaginal exam reveals a vertex presenting, with the cervix 100% effaced and 8 c m dilated. The client asks what part of labor she is in. The nurse should inform the client that she is in what phase of labor?
A) Latent phase
B) Active phase
C) Transition phase
D) Fourth stage
Answer: C
Explanation:
A) This is not the latent phase; in the latent phase of labor, contractions are every 10-20 minutes, 15-20 seconds' duration progressing to every 5-7 minutes, and 30-40 seconds' duration. Dilatation is 1-3 c m.
B) This is not the active phase; in the active phase of labor, contractions are every 2-3 minutes with a dilatation of 4-7 c m.
C) The transition phase begins with 8 c m of dilatation, and is characterized by contractions that are closer and more intense.
D) The fourth stage occurs after delivery of the placenta.
Page Ref: 504
3) The nurse is assessing the comfort of the parents during the third stage of labor. Which finding(s) indicate that the parents feel comfortable during this stage?
Note: Credit will be given only if all correct choices and no incorrect choices are selected.
Select all that apply.
A) Talking to the newborn
B) Verbally expressing feelings of pride
C) Requesting to dim the lights
D) Preferring limited contact with the newborn initially
E) Immediately placing phone calls
Answer: A, B
Explanation:
A) Talking to the newborn and verbally expressing feelings of pride are indications that the parents feel comfortable in the environment.
B) Talking to the newborn and verbally expressing feelings of pride are indications that the parents feel comfortable in the environment.
C) Requesting to dim the lights does not necessarily indicate whether or not the parents feel comfortable in the environment.
D) The parents may prefer to limit contact with the newborn initially, and it is important for the nurse to support the wishes of the parent. However, this does not necessarily indicate whether or not the parents feel comfortable in the environment.
E) Immediately placing phone calls after the newborn is delivered does not necessarily indicate whether or not the parents feel comfortable in the environment.
Page Ref: 519
4) The nurse is caring for a client and her spouse during the third stage of labor. Which action(s) support initial parental-newborn attachment at this time?
Note: Credit will be given only if all correct choices and no incorrect choices are selected.
Select all that apply.
A) Minimizing assessments
B) Delaying ophthalmic antibiotics for 2 hours
C) Dimming the room lights
D) Talking quietly
E) Providing privacy
Answer: A, C, D, E
Explanation:
A) Minimizing assessments enhances parental newborn attachment during this time.
B) Ophthalmic antibiotics may be delayed during the first hour, but not up to 2 hours.
C) Dimming the room lights enhances parental-newborn attachment during this time.
D) Talking quietly enhances parental-newborn attachment during this time.
E) Providing privacy enhances parental-newborn attachment during this time.
Page Ref: 519
5) The nurse is assessing the emotional state of a client following the delivery of her newborn. Which response by the client requires further follow up by the nurse?
A) Excitability
B) Crying
C) Quiet
D) Withdrawn
Answer: D
Explanation:
A) The emotional response to birth varies, and excitability is considered a normal finding.
B) The emotional response to birth varies, and crying is considered a normal finding.
C) The emotional response to birth varies, and being quiet is considered a normal finding.
D) Being withdrawn is not considered a normal emotional response to delivery of a newborn, and requires further follow up by the nurse.
Page Ref: 519
6) The client presents to the labor and delivery unit stating that her water broke 2 hours ago. Indicators of normal labor include which of the following?
Note: Credit will be given only if all correct choices and no incorrect choices are selected.
Select all that apply.
A) Fetal heart rate of 130 with average variability
B) Blood pressure of 130/80
C) Maternal pulse of 160
D) Protein of +1 in urine
E) Odorless, clear fluid on underwear
Answer: A, B, E
Explanation:
A) Fetal heart rate (F H R) of 110-160 with average variability is a normal indication.
B) Maternal vital sign of blood pressure below 140/90 is a normal indication.
C) A pulse of 60-100 is a normal indication.
D) Proteinuria of +1 or more could be a sign of preeclampsia.
E) Fluid clear and without odor if membranes ruptured is a normal indication.
Page Ref: 500
7) The client is being admitted to the birthing unit. As the nurse begins the assessment, the client's partner asks why the fetus's heart rate will be monitored. After the nurse explains, which statement by the partner indicates a need for further teaching?
A) "The fetus's heart rate will vary between 110 and 160."
B) "The heart rate is monitored to see whether the fetus is tolerating labor."
C) "By listening to the heart, we can tell the gender of the fetus."
D) "After listening to the heart rate, you will contact the midwife."
Answer: C
Explanation:
A) A normal fetal heart rate is 110-160.
B) The fetal heart rate (F H R) is auscultated every 30 minutes. It should remain between 110 and 160 beats per minute (beats/m i n) without the presence of decelerations.
C) Fetal heart rate is not a predictor of gender.
D) Once the admission is complete, the nurse will contact the client's provider with the assessment findings.
Page Ref: 500
8) The laboring client and her partner have arrived at the birthing unit. Which step of the admission process should be undertaken first?
A) The sterile vaginal exam
B) Welcoming the couple
C) Auscultation of the fetal heart rate
D) Checking for ruptured membranes
Answer: B
Explanation:
A) The sterile vaginal exam should be performed after maternal vital signs have been assessed.
B) It is important to establish rapport and to create an environment in which the family feels free to ask questions. The support and encouragement of the nurse in maintaining a caring environment begins with the initial admission.
C) The fetal heart rate should be listened to after the client is made comfortable.
D) Assessing for intact or ruptured membranes is a part of the admission assessment after the client is made comfortable.
Page Ref: 507
9) An expectant father has been at the bedside of his laboring partner for more than 12 hours. An appropriate nursing intervention would be which of the following?
A) Insist that he leave the room for at least the next hour.
B) Tell him he is not being as effective as he was, and that he needs to let someone else take over.
C) Offer to remain with his partner while he takes a break.
D) Suggest that the client's mother might be of more help.
Answer: D
Explanation:
A) Insisting that the father leave does not reassure him about the care the woman will receive in his absence.
B) Telling him that he is ineffective does not reassure him about the care the woman will receive in his absence.
C) Support persons frequently are reluctant to leave the laboring woman to take care of their own needs. The laboring woman often fears being alone during labor. Even though there is a support person available, the woman's anxiety may be decreased when the nurse remains with her while he takes a break.
D) Suggesting that the client's mother take his place does not reassure him about the care the woman will receive in his absence.
Page Ref: 527
10) By inquiring about the expectations and plans that a laboring woman and her partner have for the labor and birth, the nurse is primarily doing which of the following?
A) Recognizing the client as an active participant in her own care.
B) Attempting to correct any misinformation the client might have received.
C) Acting as an advocate for the client.
D) Establishing rapport with the client.
Answer: A
Explanation:
A) Understanding the couple's expectations and plans helps the nurse provide optimal nursing care and facilitate the best possible birth experience.
B) Any misinformation the family has can be corrected, but that is not the primary focus.
C) The nurse might use the information about plans and expectations to act as an advocate for the client as the labor progresses, but this is not the primary rationale for inquiring about them.
D) Rapport and a therapeutic relationship are important for all nurse-client interactions, but are not best addressed by asking about plans and expectations for the birth.
Page Ref: 499
11) The labor and birth nurse is admitting a client. The nurse's assessment includes asking the client whom she would like to have present for the labor and birth, and what the client would prefer to wear. The client's partner asks the nurse the reason for these questions. What would the nurse's best response be?
Note: Credit will be given only if all correct choices and no incorrect choices are selected.
Select all that apply.
A) "These questions are asked of all women. It's no big deal."
B) "I'd prefer that your partner ask me all the questions, not you."
C) "A client's preferences for her birth are important for me to understand."
D) "Many women have beliefs about childbearing that affect these choices."
E) "I'm gathering information that the nurses will use after the birth."
Answer: C, D
Explanation:
A) Although this information is asked of all clients, it is purposefully gathered.
B) It is not therapeutic communication to tell the partner not to ask questions.
C) The nurse incorporates the family's expectations into the plan of care to be culturally appropriate and to facilitate the birth.
D) The nurse incorporates the family's expectations into the plan of care to be culturally appropriate and to facilitate the birth.
E) The information gathered will be used during the labor and birth, not after delivery.
Page Ref: 502
12) The laboring client presses the call light and reports that her water has just broken. What would the nurse's first action be?
A) Check fetal heart tones.
B) Encourage the mother to go for a walk.
C) Change bed linens.
D) Call the physician.
Answer: A
Explanation:
A) When the membranes rupture, the nurse notes the color and odor of the amniotic fluid and the time of rupture and immediately auscultates the F H R.
B) If there has been a rupture of membranes, the laboring client should not be allowed to walk.
C) The bed linens can be changed after assessing the heart rate.
D) The physician does not need to be called after rupture of the membranes unless there is a change in the status of the fetus or client.
Page Ref: 503
13) The laboring client is having moderately strong contractions lasting 60 seconds every 3 minutes. The fetal head is presenting at a -2 station. The cervix is 6 c m and 100% effaced. The membranes spontaneously ruptured prior to admission, and clear fluid is leaking. Fetal heart tones are in the 140s with accelerations to 150. Which nursing action has the highest priority?
A) Encourage the husband to remain in the room.
B) Keep the client on bed rest at this time.
C) Apply an internal fetal scalp electrode.
D) Obtain a clean-catch urine specimen.
Answer: B
Explanation:
A) It is unknown from the given information whether it is culturally appropriate for the client's husband to remain in the room for the labor and birth.
B) Because the membranes are ruptured and the head is high in the pelvis at a -2 station, the client should be maintained on bed rest to prevent cord prolapse.
C) An internal fetal scalp electrode is placed when there are signs of fetal intolerance of labor. This client has normal fetal heart tones and clear amniotic fluid; no signs of fetal intolerance of labor are present.
D) A clean-catch urine specimen is usually obtained upon admission, but amniotic fluid contamination might falsely increase the reading of protein present.
Page Ref: 506
14) The client has stated that she wants to avoid an epidural and would like an unmedicated birth. Which nursing action is most important for this client?
A) Encourage the client to vocalize during contractions.
B) Perform vaginal exams only between contractions.
C) Provide a C D of soft music with sounds of nature.
D) Offer to teach the partner how to massage tense muscles.
Answer: D
Explanation:
A) Some clients want to vocalize during labor, and some vocalize only when they perceive that they are losing control. The client should determine whether vocalization is desirable for her.
B) Vaginal exams are performed between contractions for all laboring clients in order to decrease discomfort.
C) The nurse should ask the client what type of music she would like to listen to instead of making assumptions.
D) Massage is helpful for many clients, especially during latent and active labor. Massage can increase relaxation and therefore decrease tension and pain.
Page Ref: 508
15) The nurse is reviewing the contents of the birthing unit's emergency pack for use in case of a precipitous birth. Which item(s) should the nurse ensure is (are) included in the pack?
Note: Credit will be given only if all correct choices and no incorrect choices are selected.
Select all that apply.
A) Sterile drape
B) Bulb syringe
C) Two sterile clamps
D) Sterile gloves
E) Forceps
Answer: A, B, C, D
Explanation:
A) A small drape is included that can be placed under the woman's buttocks to provide a sterile field.
B) A bulb syringe is needed to clear mucus from the newborn's mouth.
C) Two sterile clamps (Kelly or Rochester) are needed to clamp the umbilical cord before applying a cord clamp.
D) Sterile gloves are a basic element of a typical birthing unit emergency pack.
E) Forceps are not required during a precipitous birth.
Page Ref: 525
16) Two hours after delivery, a client's fundus is boggy and has risen to above the umbilicus. What is the first action the nurse would take?
A) Massage the fundus until firm
B) Express retained clots
C) Increase the intravenous solution
D) Call the physician
Answer: A
Explanation:
A) When the uterus becomes boggy, pooling of blood occurs within it, resulting in the formation of clots. Anything left in the uterus prevents it from contracting effectively. Thus if it becomes boggy or appears to rise in the abdomen, the fundus should be massaged until firm.
B) Expressing retained clots is not the nurse's first action.
C) Increasing the intravenous solution is not a priority in this case.
D) The physician does not need to be notified unless either the uterus does not respond to massage or the bleeding does not decrease.
Page Ref: 521
17) Why is it important for the nurse to assess the bladder regularly and encourage the laboring client to void frequently?
A) A full bladder impedes oxygen flow to the fetus.
B) Frequent voiding prevents bruising of the bladder.
C) Frequent voiding encourages sphincter control.
D) A full bladder can impede fetal descent.
Answer: D
Explanation:
A) Oxygen flow to the fetus is not impacted by a full bladder.
B) Frequent voiding has nothing to do with bruising of the bladder.
C) Frequent voiding has nothing to do with sphincter control.
D) The woman should be encouraged to void because a full bladder can interfere with fetal descent. If the woman is unable to void, catheterization may be necessary.
Page Ref: 504
18) The laboring client is complaining of tingling and numbness in her fingers and toes, dizziness, and spots before her eyes. The nurse recognizes that these are clinical manifestations of which of the following?
A) Hyperventilation
B) Seizure auras
C) Imminent birth
D) Anxiety
Answer: A
Explanation:
A) These symptoms all are consistent with hyperventilation.
B) Seizure auras do not have these symptoms.
C) Imminent birth does not have these symptoms.
D) Anxiety does not have these symptoms.
Page Ref: 508
19) A client who wishes to have an unmedicated birth is in the transition stage. She is very uncomfortable and turns frequently in the bed. Her partner has stepped out momentarily. How can the nurse be most helpful?
A) Talk to the client the entire time.
B) Turn on the television to distract the client.
C) Stand next to the bed with hands on the railing next to the client.
D) Sit silently in the room away from the bed.
Answer: C
Explanation:
A) Talking might irritate the client.
B) Turning on the television might irritate the client.
C) Standing next to the bed is supportive without being irritating. The laboring woman fears being alone during labor. The woman's anxiety may be decreased when the nurse remains with her.
D) Sitting silently away from the client can lead to her feeling abandoned.
Page Ref: 527
20) The nurse administered oxytocin 20 units at the time of placental delivery. Why was this primarily done?
A) To contract the uterus and minimize bleeding
B) To decrease breast milk production
C) To decrease maternal blood pressure
D) To increase maternal blood pressure
Answer: A
Explanation:
A) Oxytocin is given to contract the uterus and minimize bleeding.
Page Ref: 520
21) A client delivered 30 minutes ago. Which postpartal assessment finding would require close nursing attention?
A) A soaked perineal pad since the last 15-minute check
B) An edematous perineum
C) The client experiencing tremors
D) A fundus located at the umbilicus
Answer: A
Explanation:
A) If the perineal pad becomes soaked in a 15-minute period, or if blood pools under the buttocks, continuous observation is necessary. As long as the woman remains in bed during the first hour, bleeding should not exceed saturation of one pad.
B) An edematous perineum is a normal postpartal finding.
C) Tremors are a normal postpartal finding.
D) A fundus located at the umbilicus is a normal postpartal finding.
Page Ref: 523
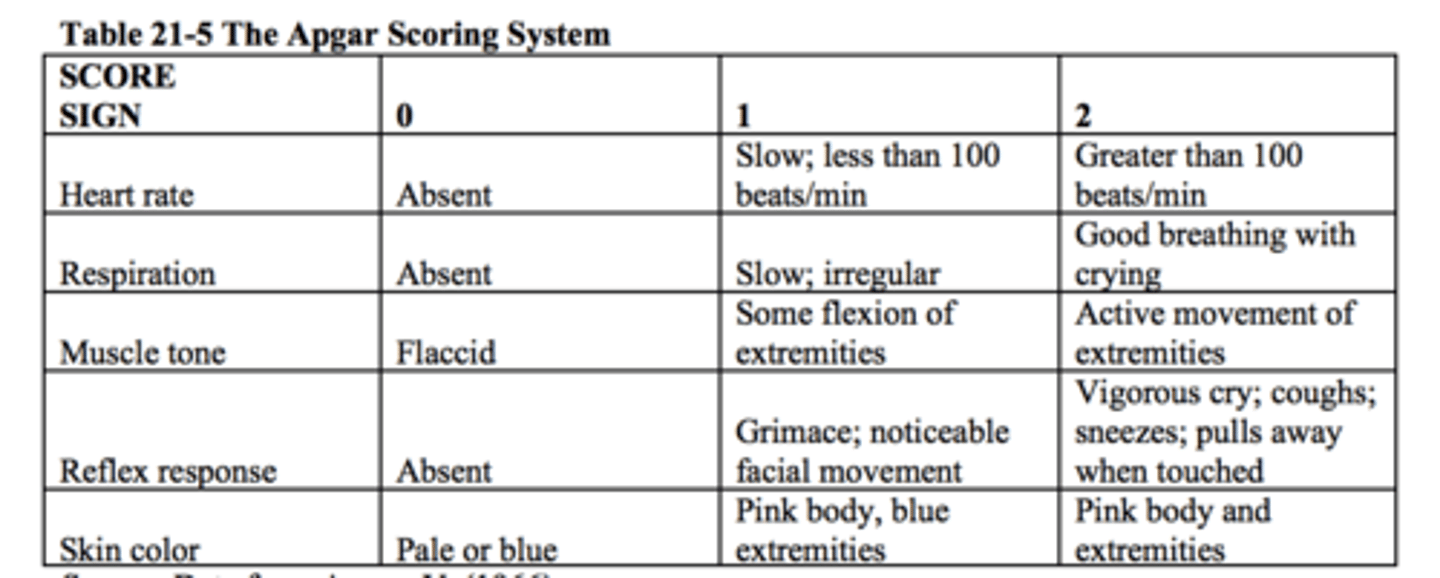
22) The neonate was born 5 minutes ago. The body is bluish. The heart rate is 150. The infant is crying strongly. The infant cries when the sole of the foot is stimulated. The arms and legs are flexed, and resist straightening. What should the nurse record as this infant's Apgar score?
A) 7
B) 8
C) 9
D) 10
Answer: B
Explanation:
A) The Apgar score would be higher; only the skin color needs to be subtracted from the score.
B) The strong cry earns 2 points. The crying with foot sole stimulation earns 2 points. The limb flexion and resistance earn 2 points each. Bluish color earns 0 points. The Apgar score is 8.
C) The Apgar score would be lower than 9 because of the skin color.
D) Ten is a perfect score. The nurse needs to subtract for skin color.
Page Ref: 517
23) Before applying a cord clamp, the nurse assesses the umbilical cord. The mother asks why the nurse is doing this. What should the nurse reply?
A) "I'm checking the blood vessels in the cord to see whether it has one artery and one vein."
B) "I'm checking the blood vessels in the cord to see whether it has two arteries and one vein."
C) "I'm checking the blood vessels in the cord to see whether it has two veins and one artery."
D) "I'm checking the blood vessels in the cord to see whether it has two arteries and two veins."
Answer: B
Explanation:
A) A normal umbilical cord does not have one artery and one vein.
B) Two arteries and one vein are present in a normal umbilical cord.
C) A normal umbilical cord does not have two veins and one artery.
D) A normal umbilical cord does not have two arteries and two veins.
Page Ref: 518
24) At 1 minute after birth, the infant has a heart rate of 100 beats per minute, and is crying vigorously. The limbs are flexed, the trunk is pink, and the feet and hands are cyanotic. The infant cries easily when the soles of the feet are stimulated. How would the nurse document this infant's Apgar score?
A) 7
B) 8
C) 9
D) 10
Answer: C
Explanation:
A) The Apgar score would be higher than 7.
B) The Apgar score would be higher than 8.
C) Two points each are scored in each of the categories of heart rate, respiratory effort, muscle tone, and reflex irritability. One point is scored in the category of skin color. The total Apgar would be 9.
D) The infant has cyanotic limbs, so the Apgar score cannot be perfect.
Page Ref: 517
25) Upon delivery of the newborn, what nursing intervention most promotes parental attachment?
A) Placing the newborn under the radiant warmer.
B) Placing the newborn on the mother's abdomen.
C) Allowing the mother a chance to rest immediately after delivery.
D) Taking the newborn to the nursery for the initial assessment.
Answer: B
Explanation:
A) Removing the baby from the mother does not promote attachment.
B) As the baby is placed on the mother's abdomen or chest, she frequently reaches out to touch and stroke her baby. When the newborn is placed in this position, the father or partner also has a very clear, close view and can reach out to touch the baby.
C) Removing the baby from the mother does not promote attachment.
D) Removing the baby from the mother does not promote attachment.
Page Ref: 519
26) A young adolescent is transferred to the labor and delivery unit from the emergency department. The client is in active labor, but did not know she was pregnant. What is the most important nursing action?
A) Determine who might be the father of the baby for paternity testing.
B) Ask the client what kind of birthing experience she would like to have.
C) Assess blood pressure and check for proteinuria.
D) Obtain a Social Services referral to discuss adoption.
Answer: C
Explanation:
A) Paternity testing is a lower priority than the physiologic well-being of the client and fetus.
B) A client with a previously undiagnosed pregnancy is unlikely to have given any thought to childbearing preferences.
C) Preeclampsia is more common among adolescents than in young adults, and is potentially life-threatening to both mother and fetus. This assessment is the highest priority.
D) It would be inappropriate to discuss adoption or parenting during labor, especially with an adolescent who did not know she was pregnant prior to the onset of labor. The nurse should wait until after the birth to have this discussion.
Page Ref: 523
27) As compared with admission considerations for an adult woman in labor, the nurse's priority for an adolescent in labor would be which of the following?
A) Cultural background
B) Plans for keeping the infant
C) Support persons
D) Developmental level
Answer: D
Explanation:
A) Cultural background is important to planning anyone's care.
B) It is important to first determine the client's developmental level when planning nursing care for the mother who is keeping her infant.
C) Support persons are important to planning anyone's care.
D) Because her cognitive development is incomplete, the younger adolescent may have fewer problem-solving capabilities. The very young woman needs someone to rely on at all times during labor. She may be more childlike and dependent than older teens.
Page Ref: 523
28) An abbreviated systematic physical assessment of the newborn is performed by the nurse in the birthing area to detect any abnormalities. Normal findings would include which of the following?
Note: Credit will be given only if all correct choices and no incorrect choices are selected.
Select all that apply.
A) Skin color: Body blue with pinkish extremities
B) Umbilical cord: two veins and one artery
C) Respiration rate of 30-60 irregular
D) Temperature of above 36.5°C (97.8°F)
E) Sole creases that involve the heel
Answer: C, D, E
Explanation:
A) This is not correct. Skin color would be body pink with bluish extremities.
B) This is not correct. The umbilical cord would have two arteries and one vein.
C) Normal findings would include a respiration rate of 30-60 irregular.
D) Normal findings would include temperature of above 36.5°C (97.8°F).
E) Normal findings would include sole creases that involve the heel.
Page Ref: 518
29) A client's labor has progressed so rapidly that a precipitous birth is occurring. What should the nurse do?
A) Go to the nurse's station and immediately call the physician.
B) Run to the delivery room for an emergency birth pack.
C) Stay with the client and ask auxiliary personnel for assistance.
D) Hold back the infant's head forcibly until the physician arrives for the delivery.
Answer: C
Explanation:
A) The nurse can direct auxiliary personnel to contact the physician.
B) The nurse can direct auxiliary personnel to retrieve the emergency birth pack.
C) If birth is imminent, the nurse must not leave the client alone.
D) With one hand, the nurse should apply gentle pressure against the fetal head to maintain flexion and prevent it from popping out rapidly. The nurse does not hold the head back forcibly.
Page Ref: 525
30) The nurse has completed an initial physical assessment for a client admitted to the birthing unit. Which action should the nurse take next?
A) Obtain the client's social history
B) Document the physical assessment findings
C) Report findings to the physician
D) Perform interventions for pain management
Answer: A
Explanation:
A) Once initial physical assessments are performed, the nurse can then take a detailed social history that provides a comprehensive view of both the woman's social habits and psychologic factors that may affect her birth experience.
B) Documenting the physical assessment findings may be performed after the initial physical assessment is performed and social history is obtained.
C) It may not be necessary to report findings to the physician in the absence of other complicating factors.
D) Interventions for pain management may not be needed at this time. Additionally, effective pain management may depend on the client's social history.
Page Ref: 501
31) The nurse has taken a detailed social history from a client admitted to the birthing unit. Which insights may the nurse gain as a result of this assessment?
Note: Credit will be given only if all correct choices and no incorrect choices are selected.
Select all that apply.
A) Social habits
B) Psychologic factors
C) Presence of H I V
D) Readiness for discharge
E) Need for bed rest
Answer: A, B
Explanation:
A) The nurse may gain a view of both the woman's social habits and psychologic factors that may affect her birth experience.
B) The nurse may gain a view of both the woman's social habits and psychologic factors that may affect her birth experience.
C) The presence of H I V may only be detected by specific testing.
D) The readiness for discharge cannot be determined at the time of obtaining a detailed social history.
E) The need for bed rest is determine by the physical, not social, assessment.
Page Ref: 501
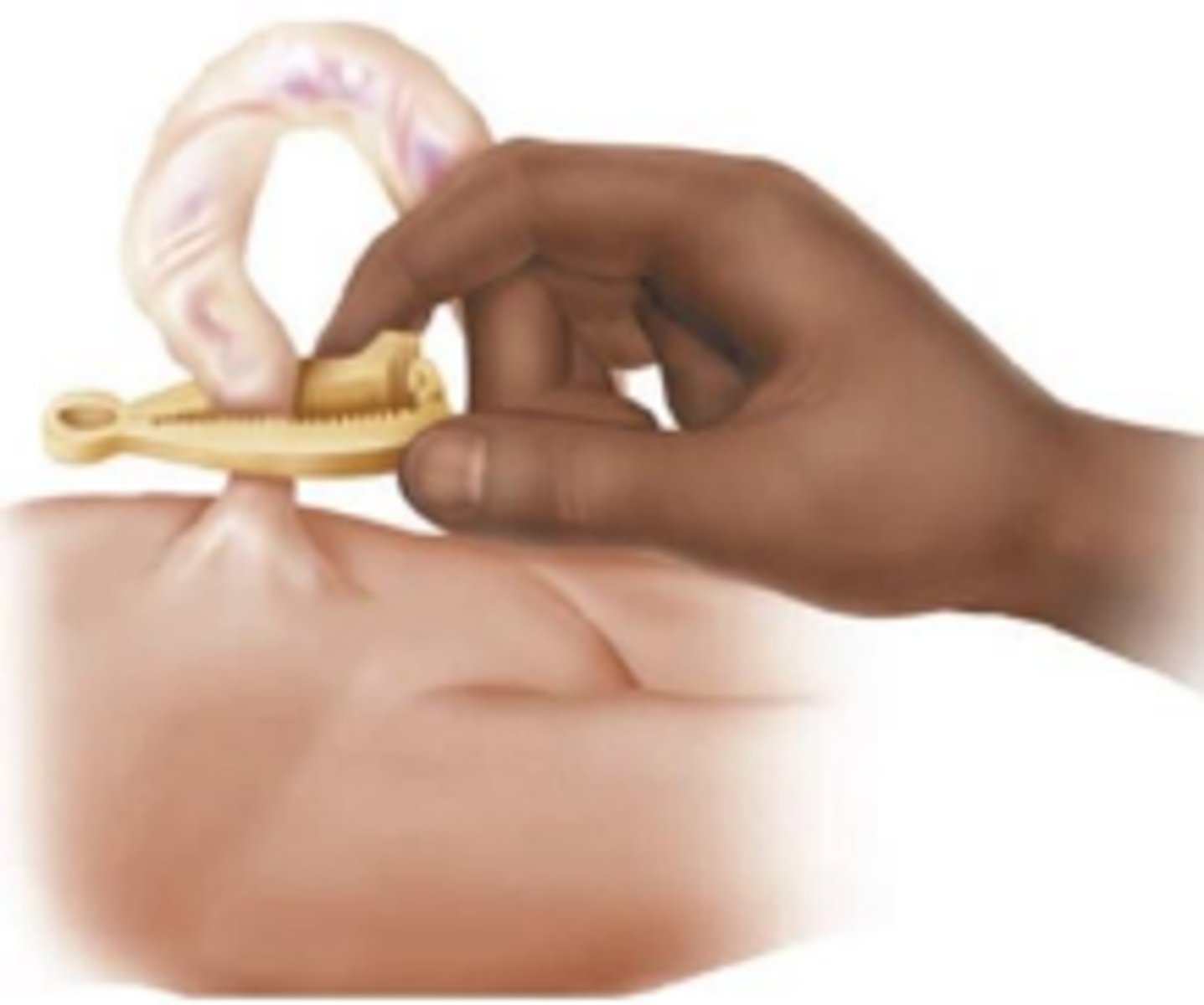
32) A newborn has the following applied to the umbilical cord. What should the nurse instruct the new parents about regarding this device?
A) It has to stay intact for at least one week
B) It is removed in 24 hours if the cord has dried
C) It eliminates the need to wash the infant's abdomen
D) It is removed by cutting the tissue beneath the clamp
Answer: B
Explanation:
B) The clamp is removed in the newborn nursery approximately 24 hours after birth if the cord has dried. The clamp does not stay intact for one week. The clamp does not eliminate the need to wash the infant's abdomen. A plastic device is used when removing the clamp. The tissue beneath the clamp is not cut. Page Ref: 515
33) The nurse determines that a newborn has the following findings:
Heart rate: 88 beats per minute
Respirations: 24 per minute and irregular
Muscle tone: Minor movement of lower extremities
Reflex response: Grimace
Skin color: Pink body, blue extremities
If using the following table, what action should the nurse take at this time?
A) Begin resuscitation
B) Stimulate the infant
C) Document the findings
D) Nasopharyngeal suctioning
Answer: B
Explanation: B) The infant's Apgar score is 5. An Apgar score between 4 and 7 indicates the need for stimulation. A score under 4 indicates the need for resuscitation. A score of 7 to 10 indicates a newborn in good condition who requires only nasopharyngeal suctioning. The nurse needs to do more than document the findings.
34) The nurse is observed performing the following with a patient:
What information will this assessment technique provide to the nurse?
A) Assesses for bladder distention
B) Estimates the weight of the uterus
C) Determines the height of the fundus
D) Evaluates the remaining placenta contents
Answer: C
Explanation: C) This is a technique used to palpate the fundus to determine if it needs to be massaged to reduce bleeding and enhance healing after delivery. This technique is not used to assess for bladder distention, estimate the weight of the uterus, or to evaluate for remaining placenta contents.
Page Ref: 522
