ETC8363-2020 Pulmonary Disorders
1/100
Earn XP
Description and Tags
ETC8363 08/2020
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
101 Terms
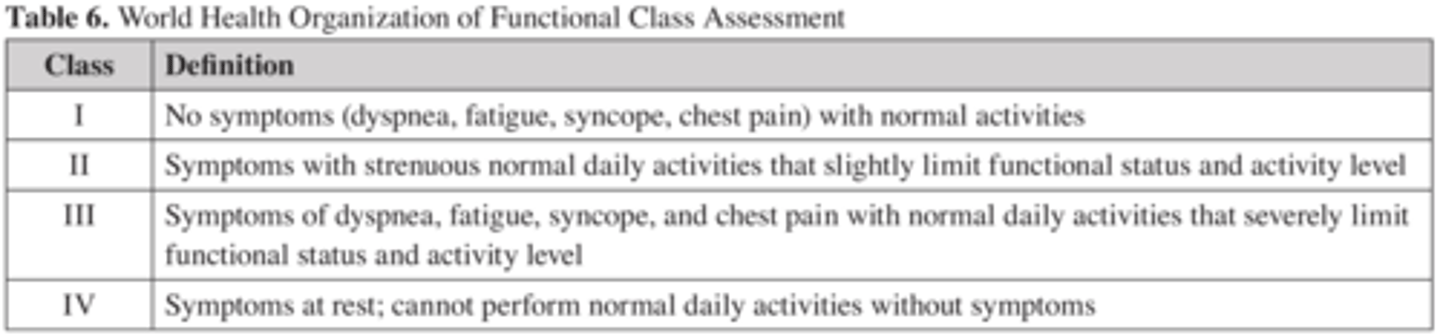
What is the Berlin Definition of ARDS?
What variables are associated with increased mortality of ARDS?
Age/ Acedemia
Barotrauma
Immunocompromised
Multiorgan dysfunction (during or on admission)
What causes lung injury?
Direct Injury: Pneumonia, Aspiration, Trauma
Indirec Injury:
Sepsis, transfusion, pancreatitis, burn, trauma.
What is one clinical HALLMARK of ARDS?
Why is it so important?
Hypoxemia, important because this causes destruction of alveoli = destruction of alveolar epithelium= impairs lymphatic drainage= disrupts osmotic gradient= accumulation of cellular debri/ microthombi.
All of which develops pulmonary edema = impaired oxygenation= ultimately organ failure.
For acute hypoxemic respiratory failure ( not due to excessive carbon dioxide in the bloodstream "hypercapnic") what is the preferred route of administration for oxygen?
HFNC - high flow nasal canula resulted in greater vent-free days. (better than face masks and positive pressure ventilation)
How many mL/kg of ventilation is considered low tidal volume?
Why is this important?
Low tidal volume 6 mL/kg of ideal BW
Considered lung protective ventilation and showed to improve survival = now the new standard of care.
What plateau pressure do we target when pts are on low tidal volume strategy?
Targeting a plateau pressure of 30 cm H2O or less is recommended.
How do we optimize tidal volume strategy?
Permissive hypercapnia (partial pressure of carbon dioxide [PCO2] 50-55 mm Hg) is acceptable to
optimize tidal volume strategy.
![<p>Permissive hypercapnia (partial pressure of carbon dioxide [PCO2] 50-55 mm Hg) is acceptable to</p><p>optimize tidal volume strategy.</p>](https://knowt-user-attachments.s3.amazonaws.com/ebfe24c3-2d51-4c1b-ae64-d96e60ad66b5.png)
What is PEEP?
what is it normally?
Positive end-expiratory pressure: pressure in the lungs (alveolar pressure) above atmospheric pressure (the pressure outside of the body) that exists at the end of expiration.
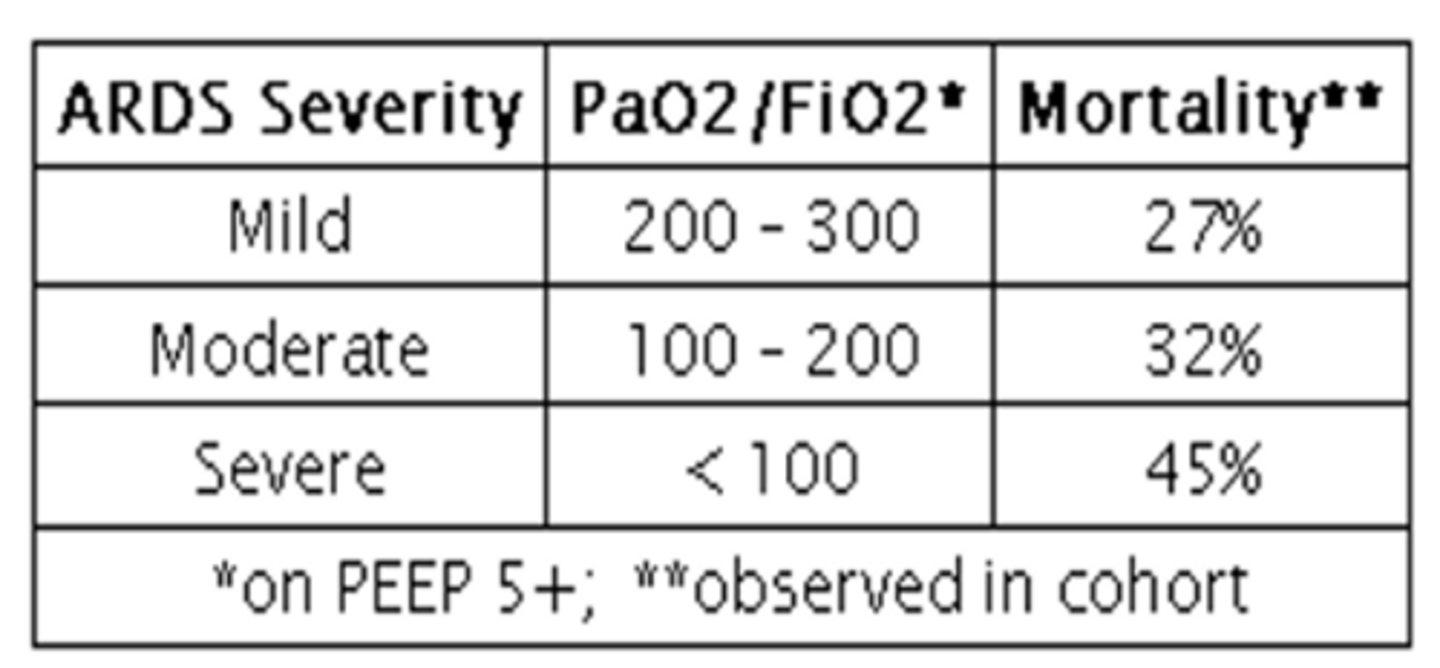
What is prone positioning?
Why and When is it used?
Prone: flat on stomach
used for treatment of ARDS that is ....
EARLY (<36hrs) &
MODERATE-SEVERE ARDS ( P/F ratio <150)
(prone positioning showed reduced 28-day mortality when compared to supine positioning) but do not use past the 36 hr mark.
Which is better
Conservative fluid management ( CVP < 4 mmHg)
Liberal fluid management ( CVP 10-14)
Conservative fluid group = more vent free days.
When would liberal fluid management be more beneficial over conservative fluid management?
When a pt has both ARDS & septic shock. Since in septic shock you need a lot of fluid to fix hypovolemic hypotension. so low BP= no conservative fluid management.
When is cisatracurium used in regards to ARDS?
Short course of cisatricurium (<48hrs) in pts with...
EARLY/or at onset (<48hrs from onset)
Moderate-Severe (P/F ratio <150) ARDS
reduced mortality
Do corticosteroids work in ARDS?
in early ARDS it was found to have no benefit
in late ARDS (>7 days) no survival benefit
How do statins help in ARDS?
It doesn't. two studies did not support the use of statins for ARDS.
presumed to benefit by modulating inflammatory response of lung parenchyma.
reduce inflammation response in sepsis and ARDS.
What are the steps for RSI?
PREpare PREoxygenate PREtreat
paralysis with induction
PROtect POSition
Place tube
Post intubation management
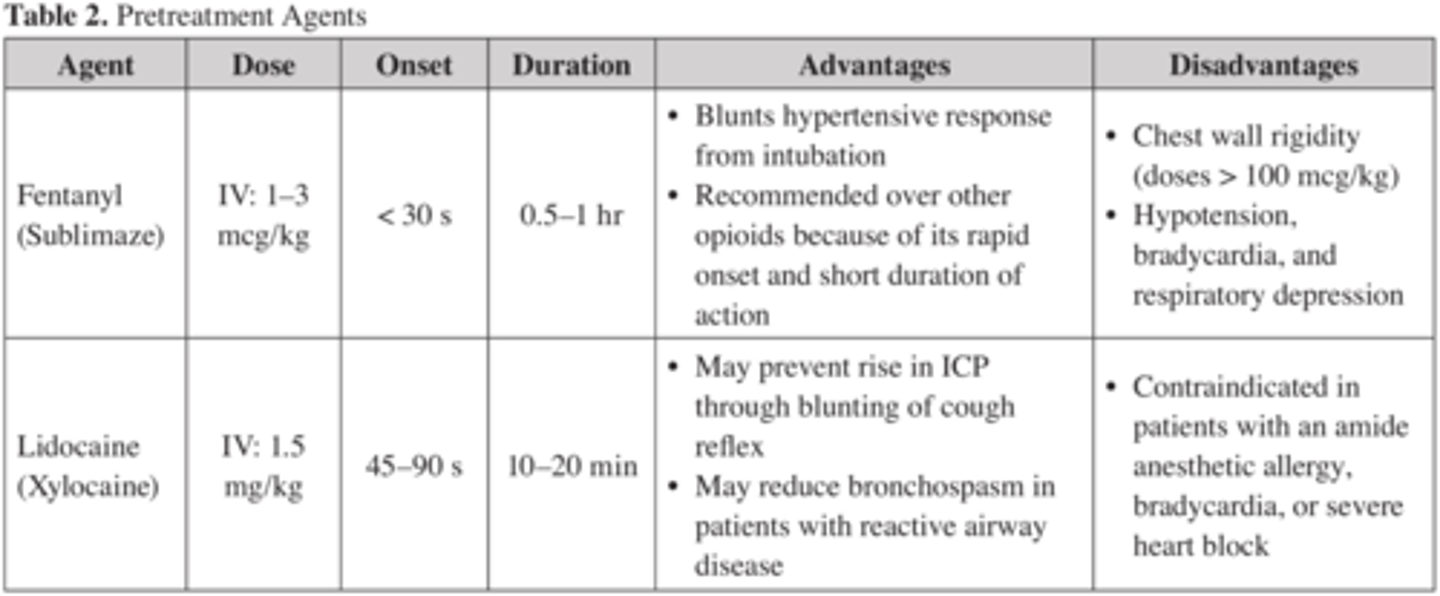
When does the PREtreat phase of RSI happen? what do we use?
Why is this done?
happens 3 min prior to induction or NMBA agent
using Fentanyl or lidocaine it is done to attenuate sympathetic/parasympathetic response to laryngoscopy.
What are the doses for Fentanyl and Lidocaine for PREtreatment in RSI?
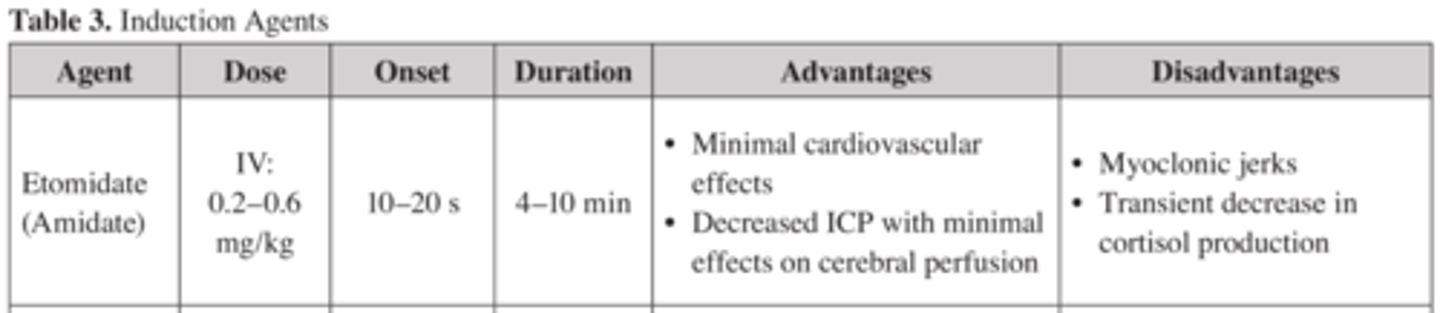
In RSI what induction agents do you use prior to paralytics?
Etomidate
Ketamine
Midazolam
Propofol
True of False:
Etomidate does not provide analgesia during RSI?
True:
Etomidate enhances GABA effect = blocks neuroexcitation = INDUCES unconsciuosness but does not provide analgesia
True/False:
Etomidate causes adrenal insuffuciency?
No, it causes adrenal suppression (decreases cortisol)
more studies needed to clarify degree of suppression vs. insufficiency
What is the RSI dose, onset, and duration for Etomidate?
may be beneficial in ICP
What is the RSI dose, onset, and duration for Ketamine?
decreases ICP & decreases fluctuations in ICP.
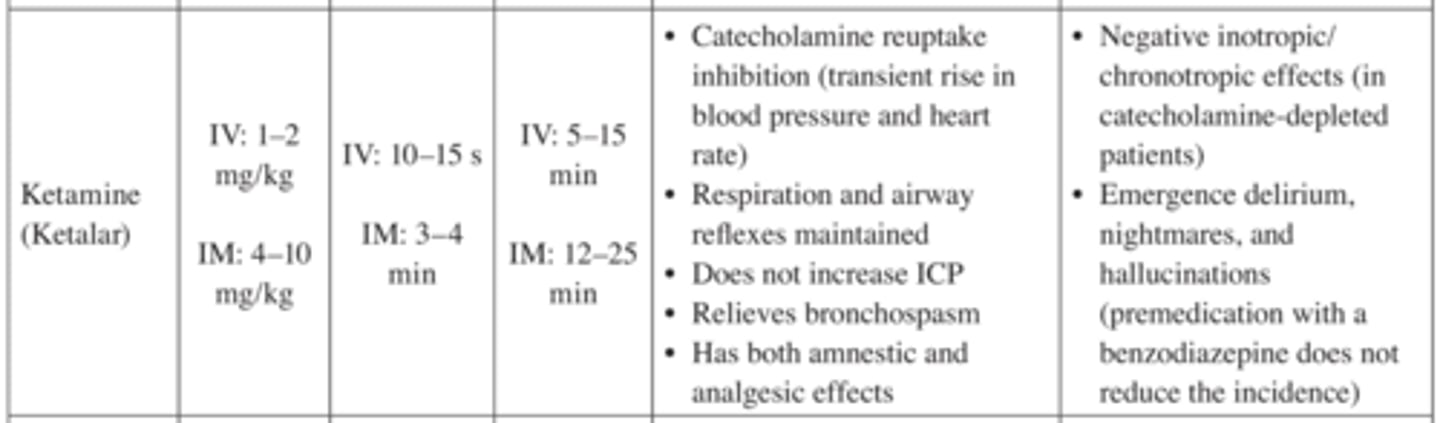
What is the RSI dose, onset, and duration for Midazolam?
not the best agent for induction due to long onset
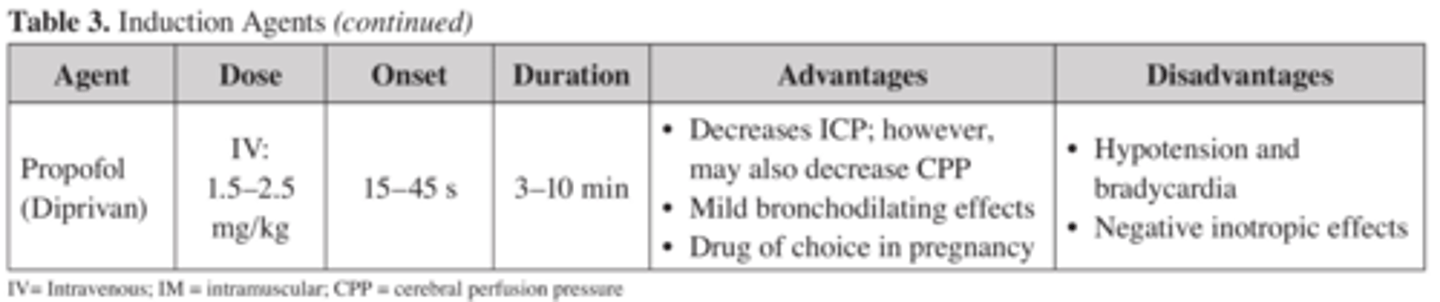
What is the RSI dose, onset, and duration for Propofol?
True or false:
Neuromuscular Blocking agents have no sedative, analgesic, or amnestic properties?
True: none of those properties. Only used to block impulse transmission of the neuromuscular junction = skeletal muscle paralysis= facilitates intubation.
What is the best NMBA for RSI?
Succinylcholine. NON-COMPETATIVELY binds to acetylcholine receptors = sustained depol of junction = release of K+ = prevents muscle contraction
(this is the ONLY DEPOLARIZING NMBA)
Depolarizing= non-competative
What are the most common NON-depolarizing NMBA used in RSI?
Rocuronium & Vecuronium (COMPETATIVE antagonist to acetylcholine at junction = prevention of contraction)
(only used when Succinylcholine is contraindicated)
Non-depolarizing= Competitive
How do you reverse NMBAs if RSI failed?
-Acetylcholinesterase inhibitors + anticholinergics
Neostigmine/pyridostigmine + atropine/glycopyrrolate
-Sugamadex (bridion): only for vec and roc.
What is the RSI dose for Succinylcholine?
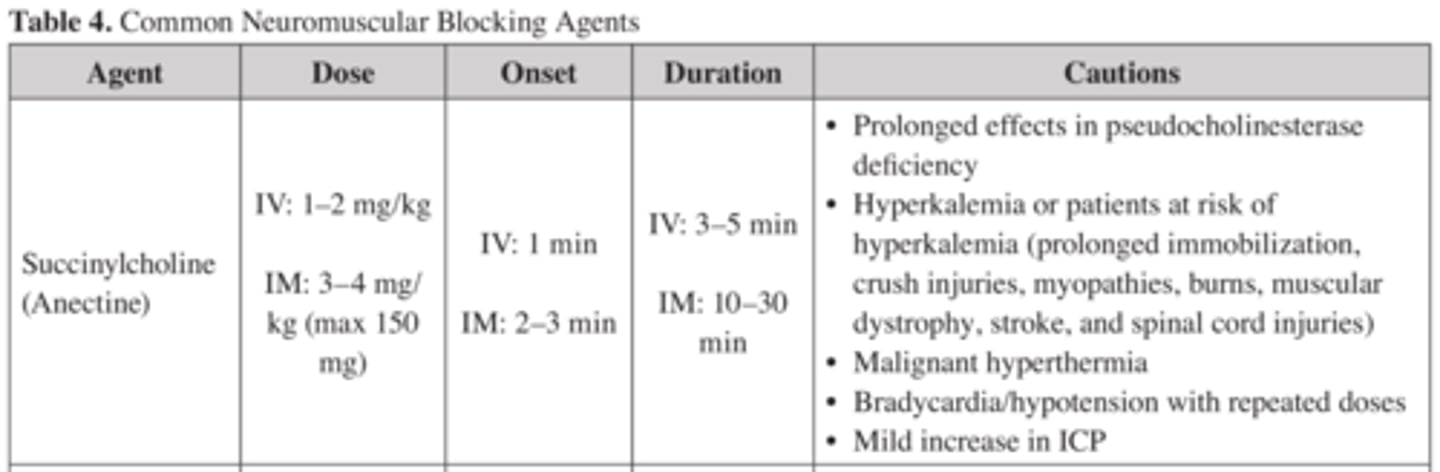
What is the RSI dose for Rocuronium (zemuron)?
What is the RSI dose for Vecuronium?

What are the 2 main categories of respiratory failure?
Hypercapnic & Hypoxic
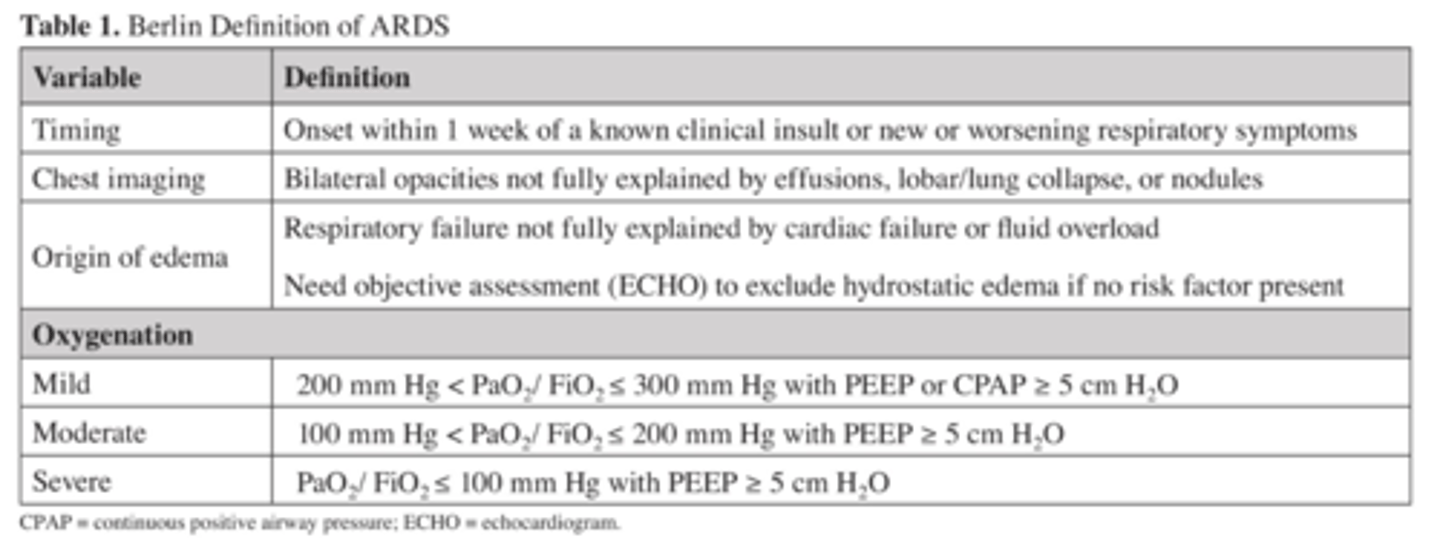
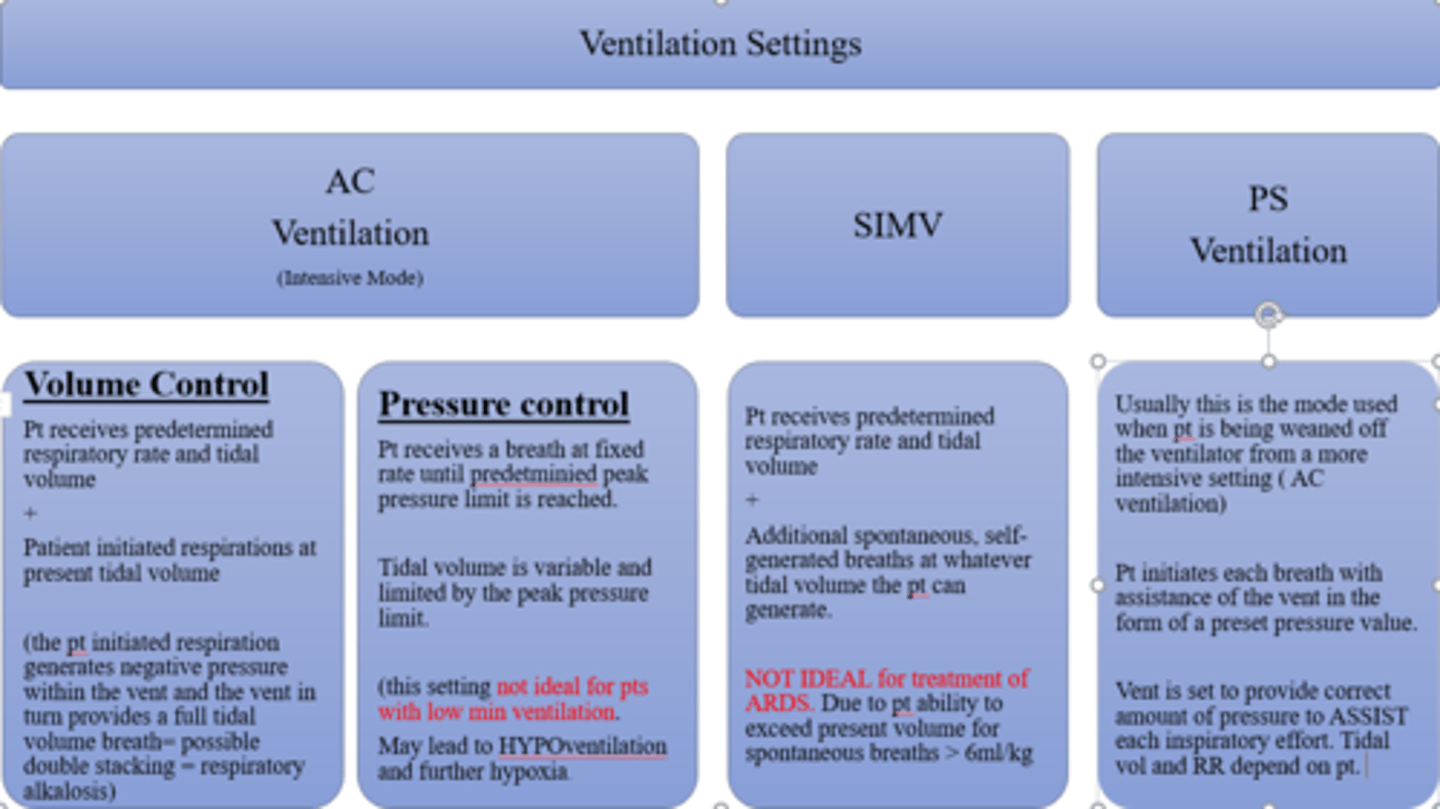
What are the different Ventilator settings and how do they work?
What is FiO2?
How is it titrated?
What is the max?
Amount of oxygen that is delivered with each breath, (21% - 100%)
FiO2 titrated to PaO2 > 55 mm Hg. (The PaO2= arterial oxygen pressure in blood. healthy adults= 80-100)
Helps with oxygenation like PEEP as well.
FiO2 max given depends on concerns for O2 toxicity.
What is Tidal Volume?
How is it titrated?
Volume of air inspired in a breath ( MV or spontaneous)
Tidal volume is set according to O2 and ventilation requirements.
ARDS pts are treated with a low tidal volume strategy, (most other patients will have the tidal volume titrated to PaCO2 and pH)
What is respiratory rate?
How is it titrated?
RR set to provide a minimal number of breaths from the ventilator @ set tidal volume.
RR titrated by minute ventilation, PaCO2, and pH.
Minute ventilation (liters per minute) = tidal volume (liters) x respiratory rate (breaths/minute).
Min vent = TV x RR
What is flow rate?
velocity of air delivered. (greatest initially during inspiration and decreases as decelerates towards the end of inspiration)
What is PEEP?
How is it titrated?
Positive pressure in the alveoli during expiration
(Provides greater surface area at the alveolar epithelial surface to promote diffusion of oxygen +
improve ventilation/perfusion matching)
Titrated to meet oxygenation requirements
What is a Ventilator Associated Event (VAE)?
>2 days of increasing vent settings:
>3 cm H20 in PEEP or >20% FiO2 after pt was already stable for 2 days or decreasing in vent settings.
What causes a Ventilator Associated Event (VAE)
Pneumonia
Fluid overload
Atelectasis
ARDS
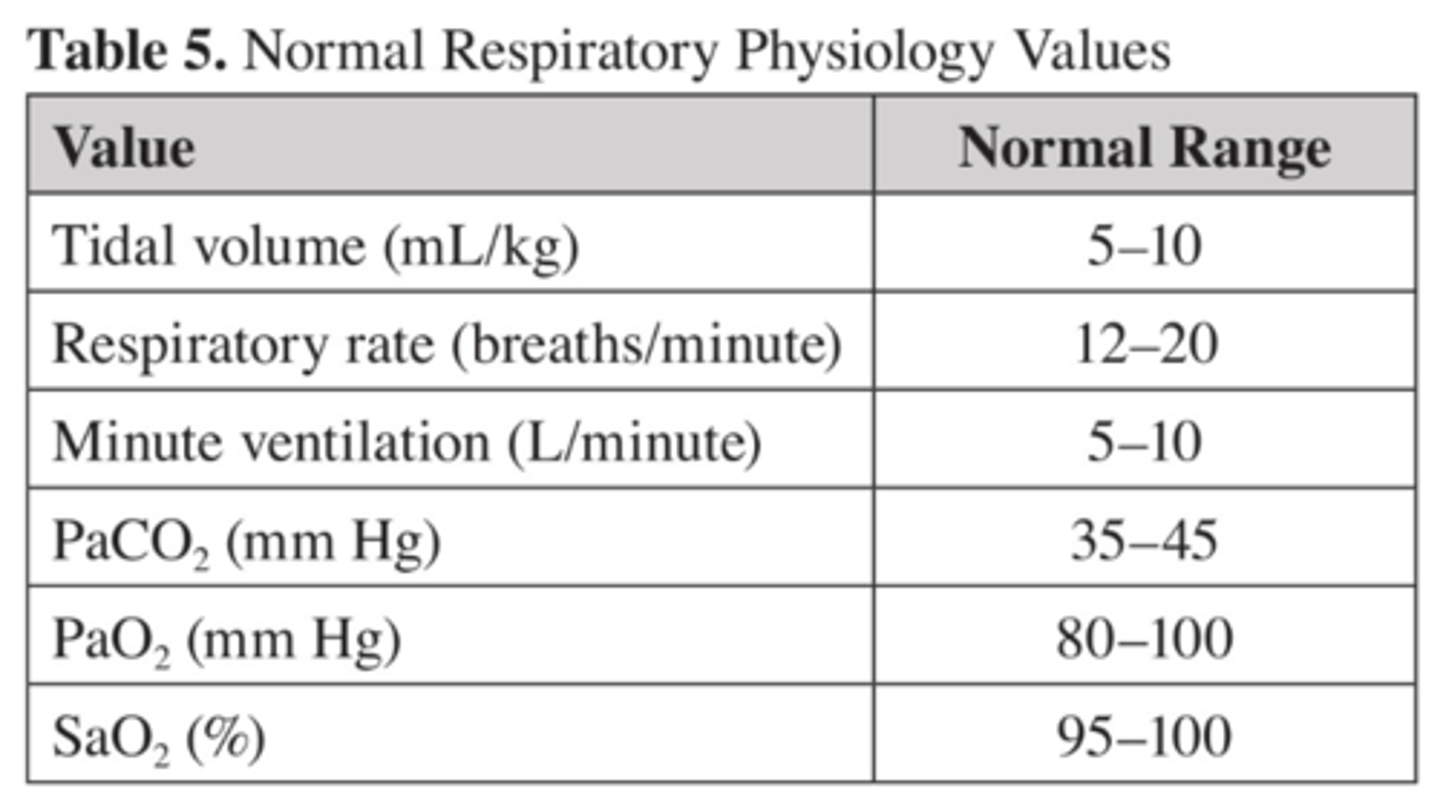
What are the normal values for
Tidal Volume
RR
Min Ventilation
PaCO2
PaO2
SaO2
With cystic fibrosis what bacteria is usually found in the lungs?
Lungs become colonized with bacteria. eventually there will be formation of thick mucus (mucoid) growing Pseudomonas Aeruginosa
What type of ABX do we use for Cystic Fibrosis?
What is our dosing strategy?
TWO antipseudomonal ABX
Aggressive dosing to maximize time above MIC
(dosing in this population is difficult due to increased Vd and increased renal clearance )
Extended interval Aminoglycosides ( Tobra 10mg/kg daily) goal peak 20-30 and trough < 1ml/L is as effective as conventional dosing with less nephrotox.
What other non-pharmacological therapies can be offered for cystic fibrosis pts?
Aggressive chest physical therapy.
Dornase alfa neb
Hypertonic saline (7%)
Nutrition ( to maintain metabolic function)
Pancreatic enzymes (to assist with digestion)
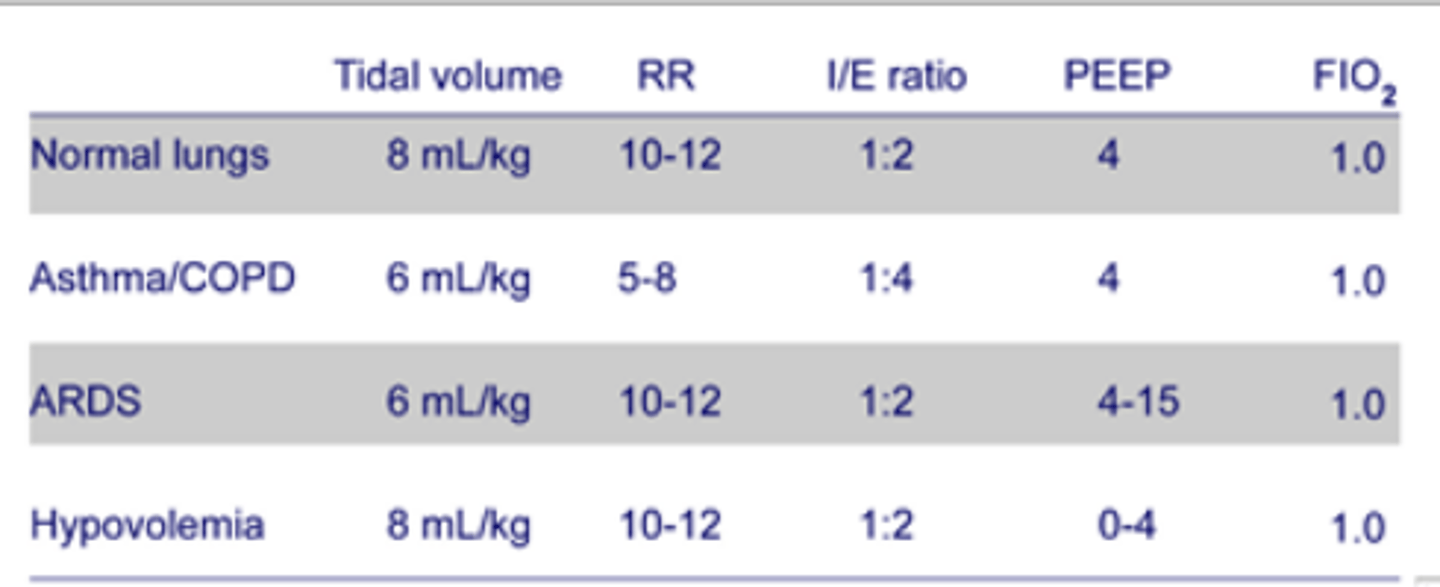
What is Pulmonary Hypertension?
life-threatening disease defined as
--mPAP of >25mmHg at rest (measured by right heart catheterization)
--PCWP <15 mmHg
--PVR of >3 wood units (via heart cath)
What is the pathophysiology of pulmonary hypertension?
-Vascular changes: vasoconstriction, cellular proliferation, thrombosis
-Thromboxane A2 (vasoconstrictor) levels increased
--Endothelin-1: (vasoconstrictor) concentrations increased
--Prostacyclin (vasodilator, PLT aggregation inhibitor) concentrations decreased.
--Nitric Oxide: (vasodilator)
What are the goals for pulmonary hypertension?
WHO-functional Class I or II.
Preserve 6 min walk distance of 380m or more.
Preserve RV size and function.
Normalize B-type natriuretic peptide.
Maintain peak oxygen consumption
What are the 3 pillars for treating pulmonary HTN?
1. Supportive therapy.
2. Vasodilator therapy
3. Targeted therapies ( Prostacyclins, endothelin receptor antagonists, PD5 inhibitors, soluble guanylate stimulators)
What are the supportive therapies for pulmonary HTN?
Oxygen: SaO2 > 90& and PaO2 of >60mmHg
Diuretics: when symptomatic RV dysfunction is present with signs of fluid overload
Digoxin: in pts with atrial tachyarrhythmias to Increase CO
Anticoag: for idiopathic PAH, Heritable PAH, and PAH 2ndary to anorexigenics use (INR : 1.5-2.5)
What agents do we use as vasodilatory therapy in PAH?
(DOC): CCB ( diltiazem, amlodipine, nifedipine) have shown great benefit in pts who have a positive vasoreactivity test and a WHO-FC of I-III.
Who should not get vasodilatory therapy in PAH?
pts with...
RV dysfunction
depressed CO
WHO-FC IV
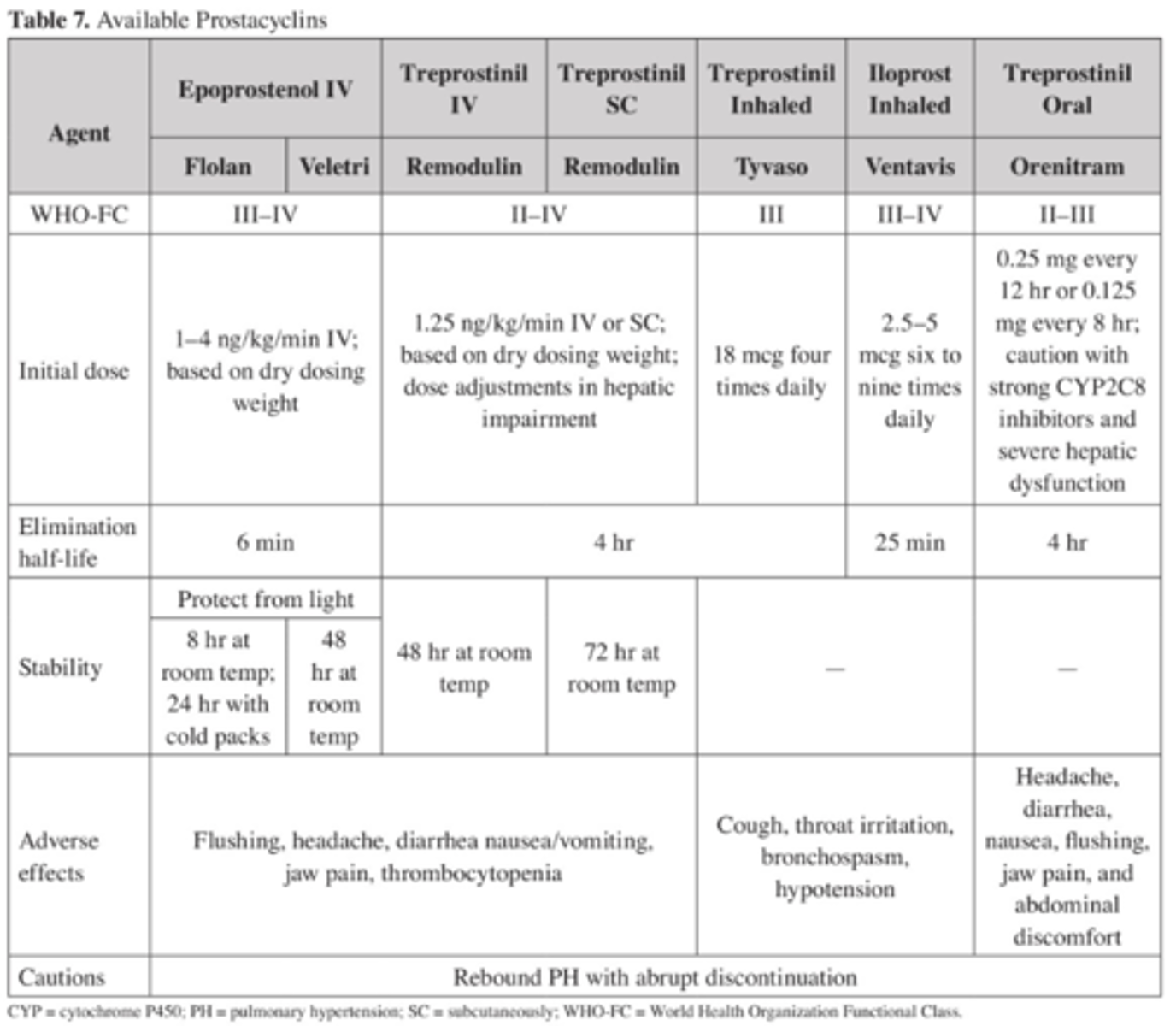
What type of pts receive PARENTERAL prostacyclins?
PAH with WHO-FC III or IV
(100% prolonged survival with IV epoprostenol infusions @ 12weeks, 88% @ 1 yr , and 55% at 5yrs)
Epoprostenol= ONLY treatment shown to reduce mortality in PAH.
Side effects: IV infections/bloodstream infections, and possible thrombosis. AND HYPOTENSION due to peripheral vasodilation
What type of pts receive INHALED prostacyclins?
WHO-FC III only
(major benefit is selective pulmonary vasodilation with minimal systemic effects)
showed significant decrease in pulmonary pressure but unsure of the long term effects (not FDA approved)
Chart of prostacyclins
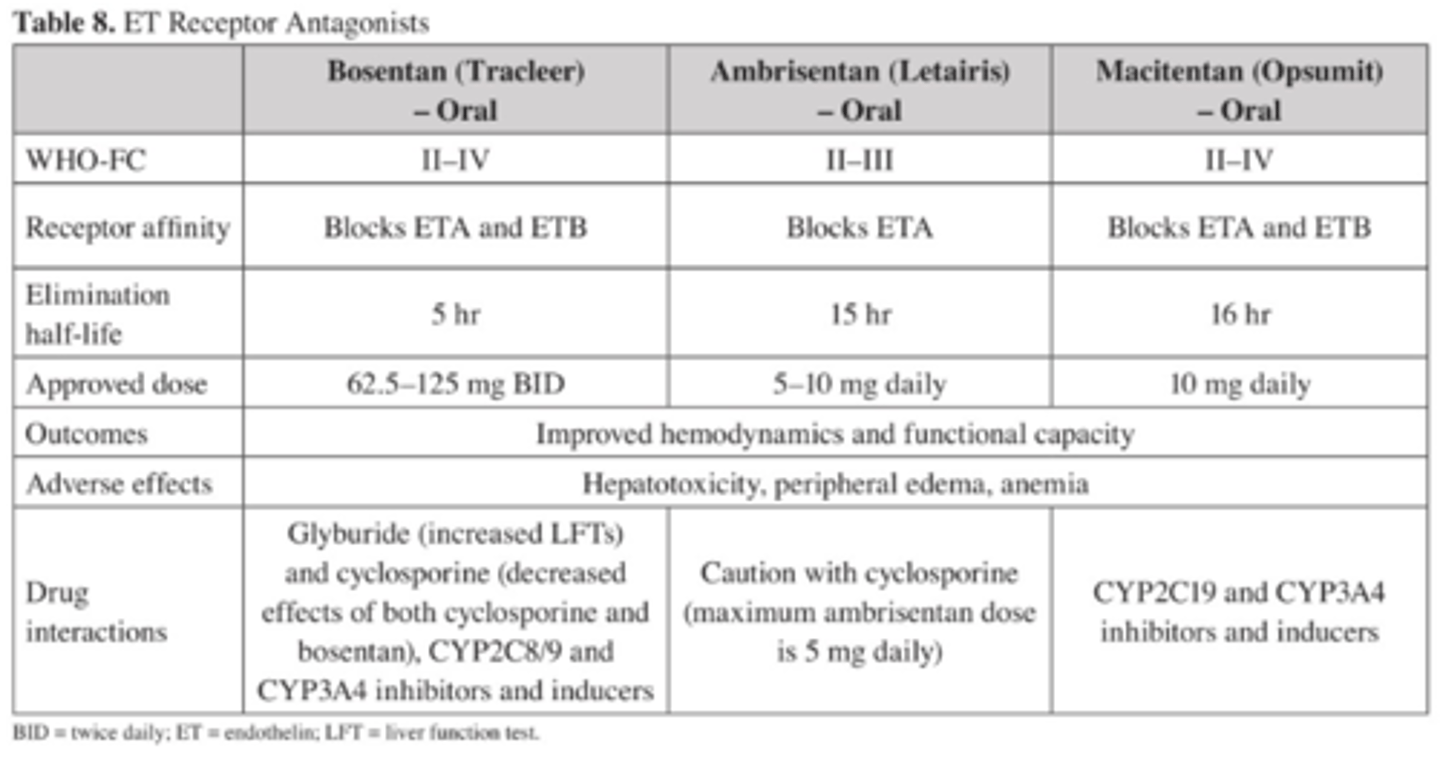
What is the ONLY Endothelin Receptor Antagonist with long-term data on morbidity and mortality for PAH?
Macitentan, but even then 30% of the patients worsened to mortality. vs. 46% in placebo
do not give macitentan with high liver enzymes.
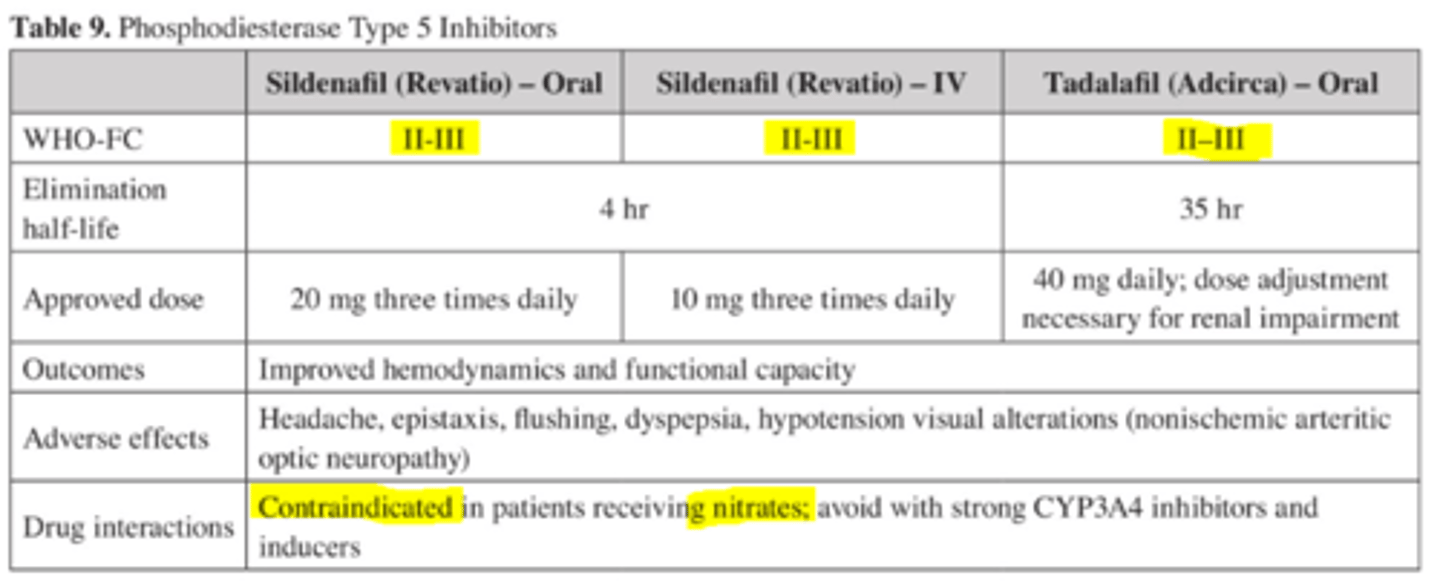
How do PD5 inhibitors work?
What dose do we give?
Improves RV contractility by increasing guanosine monophosphate which inhibits downstream PD3 = inotropic effect.
THESE AGENTS cause HYPOTENSION if given IV!!
What is the only soluble guanylate stimulator that is FDA approved for CTEPH?
Riociguat ( Adempas) sensitizes sGC to endogenous nitric oxide (makes bond stronger).
1-2.5mg TID (higher doses for smokers)
DO NOT GIVE with nitrates or PD5 inhibitors.
How do we provide hemodynamic support in pts with decompensated PH?
maintain aortic root pressure
Minimize RV ischemia
(both done by using vasopressors which increase SVR and improve RV perfusion) however vasopressors may also cause further decompensation
inotropes further augment CO of RV. (but also may vasodilate needed more pressors)
What happens during an asthma exacerbation?
Asthma exacerbations are characterized by decreases in expiratory airflow that can be quantified by
measuring lung function such as spirometry or peak expiratory flow.
What is the difference between status asthmaticus and asthma exacerbation?
near-fatal asthma?
Status asthmaticus is acute, severe asthma exacerbation that does not respond to initial intensive
therapy with the potential for pulmonary compromise and death.
near-fatal asthma: status asthmaticus that turns into respiratory failure.
Describe near-fatal asthma TYPE 1?
Subacute worsening (up to 85% of cases)
i. Slow onset of symptoms in days - weeks
ii. Poor response to inhaled bronchodilators
iii. Copious mucous, eosinophilic infiltration
Describe near-fatal asthma TYPE 2?
Type 2: Acute deterioration (up to 20% of cases)
i. Onset over minutes to hours
ii. Marked response to bronchodilators
iii. Absence of secretions, neutrophilic infiltration
Classifications of Asthma Exacerbations in the urgent/Emergency Care Setting.
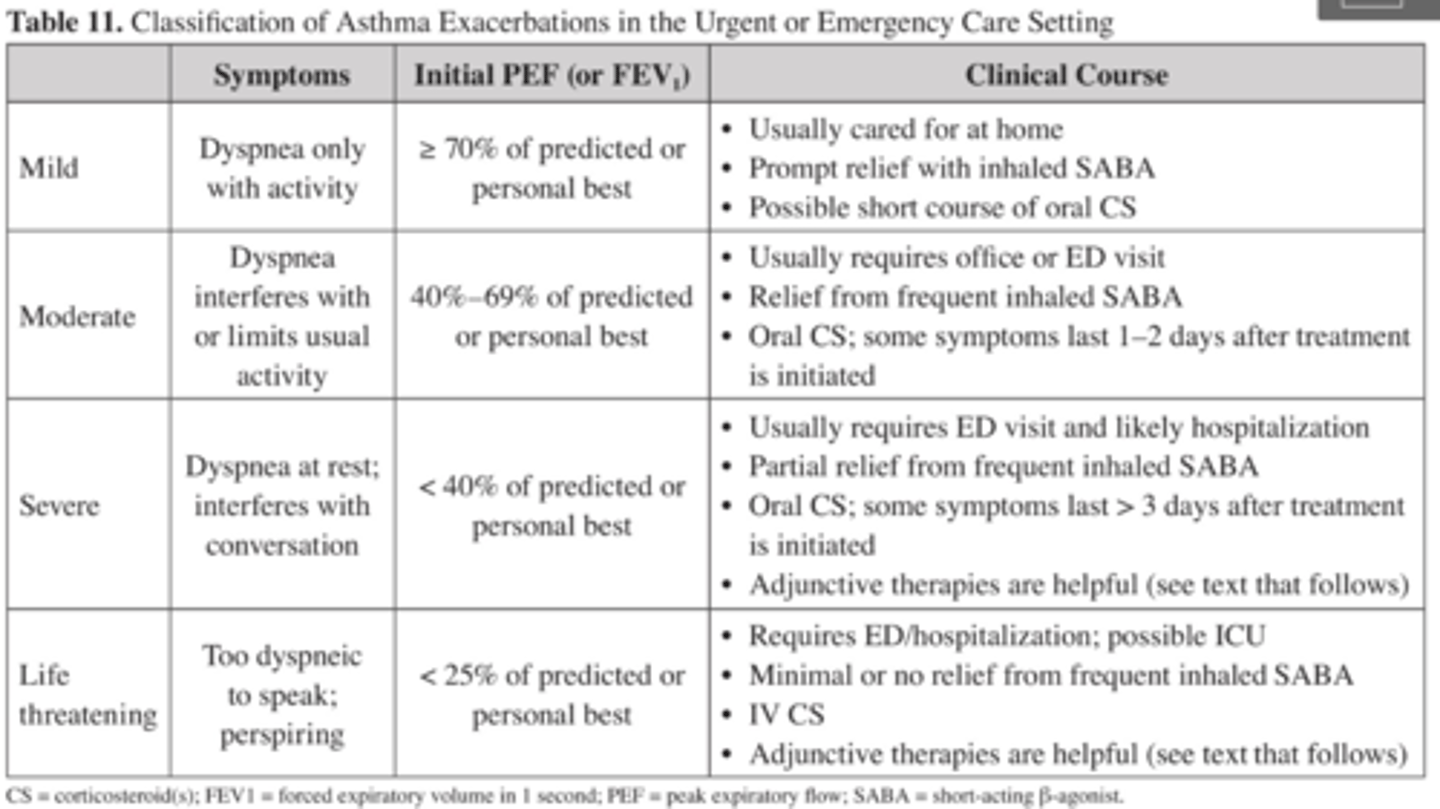
If we look at the arterial blood gas in someone who comes in for ACUTE SEVERE asthma what do we see?
1. Acute, severe asthma typically presents as a respiratory alkalosis.
then...
2. As respiratory status worsens, arterial carbon dioxide increases (patient exhaustion, inadequate alveolar
ventilation and/or an increase in physiologic dead space), leading to respiratory acidosis.
Why would we see a METABOLIC (lactic) acidosis coexist with an asthma exacerbation?
Lactate production stems from...
1. The use of high-dose β-agonists
2. Increased work of breathing resulting in anaerobic metabolism of the ventilatory muscles, and tissue hypoxia.
Systemic Beta-agonists = Type B lactic acidosis
How do we avoid/minimize dynamic hyperinflation of the lungs?
low minute ventilation (dec TV and/or RR)
High inspiratory flow rate
Minimal PEEP
How do SABAs work?
SABAs stimulate the β2-receptors on smooth muscle cells = relaxation of respiratory smooth muscle = bronchodilation and a decrease in airway obstruction.
When do we use SABAs vs LABAs vs anticholinergics in someone with asthma exacerbation?
SABAs cornerstone in management of acute, severe asthma
long-acting β2-agonists & anticholinergic
Not recommended in the acute treatment of a severe asthma exacerbation.
What is the difference in dosing nebulized SABAs in the treatment of an asthma exacerbation via intermittent vs. Continuous nebs.
Intermittent: 2.5-5 mg every 20 minutes for three doses; then 2.5-10 mg every 1-4 hours as needed.
Continuous nebulization of albuterol: 10-15 mg/hour
How do we dose MDI of albuterol in asthma exacerbation?
Dose: 4-8 puffs q 20 min. (up to 4 hours); then q 1-4 hrs as needed
remove canister from actuator and connected to the inspiratory limb of the vent with spacer.
Actuation of MDI must be synchronized with the onset of ventilator inspiratory airflow
Longer inspiratory time and slower inspiratory flow improve aerosol delivery in ventilated patients.
Wait 15 seconds between actuations.
Important side effects of B-agonists?
Tremor, tachyarrhythmias, tachyphylaxis
HYPOkalemia
HYPER-glycemia (BB mask hypoglycemia )
Type-B lactic acidosis.
How do anticholinergics work?
What is their place in Asthma exacerbation treatment?
(ipratropium bromide) bind to the muscarinic receptors on smooth muscle cells in the airways= reduce bronchoconstriction.
Given WITH SABA to promote additional bronchodilation through a different pathway
Ipratropium + albuterol vs. albuterol alone in patients with severe asthma resulted in improved response; however, outcomes with this combination in status asthmaticus or near-fatal asthma remain elusive
How do corticosteriods work for asthma exacerbation?
Decrease airway obstruction by...
Decreasing inflammation/ airway edema
Suppressing certain proinflammatory cytokines
Increasing β2-receptors & responsiveness to βagonists
When is the best time to give corticosteroids for status asthmaticus or near-fatal asthma?
corticosteroids take 6-8 hrs to start working so give them ASAP (usually within 1 hr of presentation)
When do we give oral prednisone vs an IV form?
considered as effective as parenteral in most pts.
do not give orally to critically ill pts with impaired gastric absoprtion
What is the dose of methylprednisolone for someone who has an asthma exacerbation?
How long do we give it for?
Methylprednisolone 40-80 mg per day (or equivalent) in one or two divided doses until peak expiratory
flow reaches 70% of predicted or personal best
(usually takes 3-10 days)
True/False:
For corticosteroid courses less than 1 week, tapering is not necessary.
True, even 10 days is okay if they are using inhaled corticosteroids.
What are some adjunctive therapies that can be used for asthma exacerbation?
Ketamine: has bronchodilatory properties
Helium-Oxigen mix (Heliox): decreases airway resistance = better ventilation = delays intubation by allowing other therapies to work.
Magnesium Sulfate: last resort after 1 hr of other therapies not working.
What is the dose of methylxanthine for asthma exacerbation?
Therapies that ARE NOT RECOMMENDED
Methylxanthines (aminophylline/Aminophylline)
ABX
Mucolytics
What is COPD?
Chronic airflow limitation, 2ndary to chronic inflammation due to ...
1. Small-airway disease (obstructive bronchitis)
+
2. Parenchymal destruction (emphysema).
What is the spirometry value we look for in someone having an COPD exacerbation?
Spirometry is not accurate during an COPD exacerbation and is not recommended.
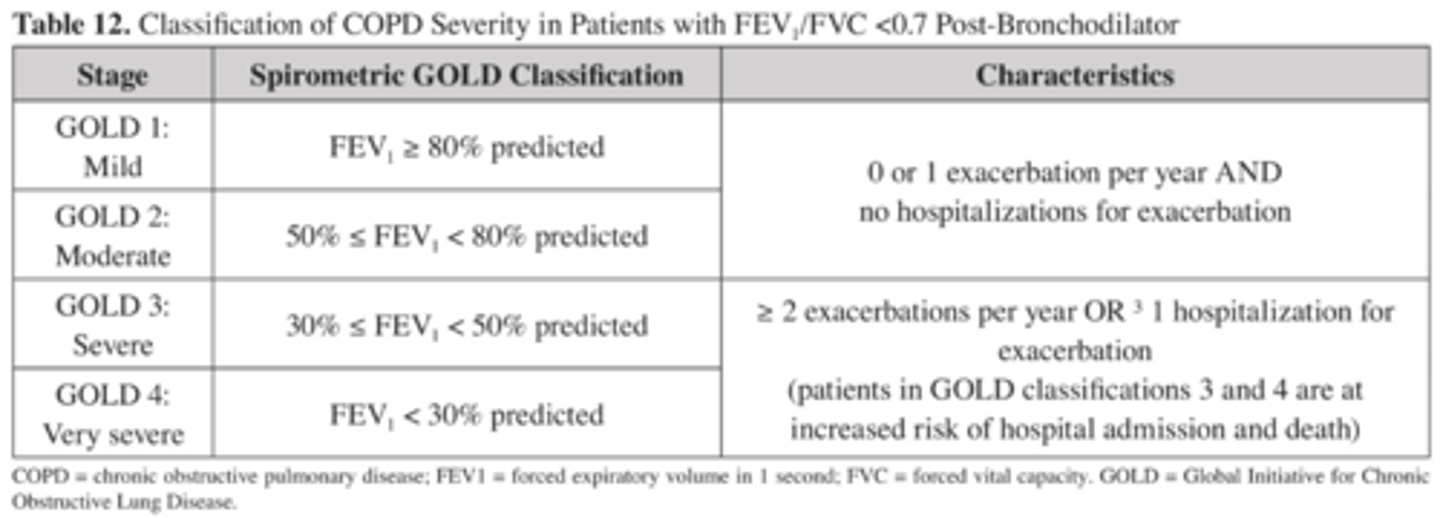
Classification of COPD
What is the most common cause of an Acute COPD Exacerbation?
Respiratory Tract Infection (40-50% of COPD Exac.)
What are the most common organisms found in an Acute COPD exacerbation due to a respiratory infection?
Strep. Pneumo
H. Influenza
Moraxella Catarrhalis
P. Aeruginosa (mostly in GOLD 3 &4)
What is the main therapy in COPD exacerbation?
What is our goal?
OXYGEN
HFNC to a goal of SaO2 88-92%
When should a pt with COPD exacerbation be on Non-invasive Mech. ventilation?
1. Respiratory acidosis ( pH < 7.35)
2. Severe Dyspnea ( seen as respiratory muscle fatigue and/or increased work of breathing)
3. Persistent hypoxemia despite supplemental O2
What is the difference between Non-invasive Mech vent. and regular mech. vent?
Non-Invasive
Improves gas exchange, reduces work of breathing and need for mechanical intubation
Decreases hospitalization duration and improves survival.
What are the indications needed to proceed with intubation/MV of someone with a COPD Exacerbation ?
1. Unable to tolerate / failure of noninvasive ventilation
2. Respiratory or cardiac arrest
3. Altered level of consciousness
4. Aspiration/vomiting/inability to clear secretions
5.Hemodynamic instability despite fluid/vasopressors
6.Severe ventricular arrhythmias
What are the preferred agents to bronchodilate in COPD exacerbations?
Inhaled SABA ( neb/MDI)
+/-
Short acting anticholinergic
What is the best corticosteroid to use for COPD exacerbation?
dose?
How many days?
COPD: Prednisone 40 mg daily or equivalent (preferably oral) for 5 days.
shortens recovery time, improves FEV1 and hypoxemia
(If oral administration is not an option equivalent doses of IV hydrocortisone, methylprednisolone or budesonide nebs may be administered )
When should ABX be used in COPD exacerbations?
How long is the treatment?
Add if ONE of the following is met...
1.All three cardinal symptoms of a COPD exacerbation (increased dyspnea, sputum production,
and sputum purulence) are present
2.Two of the three cardinal signs are present, with increased sputum purulence as one of the
symptoms.
3. Require noninvasive or invasive ventilation
ABX for 5-10 days.
What is predicted body weight?
(aka. ideal BW)
Predicted body weight (PBW)
Male = 50 + 2.3 [height (inches) – 60]
Female = 45.5 + 2.3 [height (inches) - 60]
Which best describes the category of acute respi-
ratory distress syndrome (ARDS) that most
benefits from prone positioning and cisatracurium
administration?
moderate to severe.
What is the best way to fix a HYPERcarbic respiratory failure in a pt with a pH of 7.3 plus a PaCO2 of > 65?
restore normal ventilation = by increasing respiratory rate to release some of the acidity from the body.
LOW TIDAL VOLUME (4-6 ml/ kg) WILL MAKE THINGS WORSE.
How do you treat CF on top of ARDS?
Treat ARDS:
lung protection 4-6 ml/kg ventilation
fluid conservative ( CVP < 4 mmHg- if not in shock)
Treat cystic fibrosis:
give 2 antispeudomonal ABX with one being a DAILY tobramycin therapy.
How do you treat a pt with both ARDS and septic shock?
if < 48hrs of onset of illness
Severe ARDS: cisatricurium + prone positioning + lung protection vent (4-8ml/kg IBW)
&
Septic shock: LIBERAL fluid management CVP 10-14 mmHg only until hemodynamically stable again (MAP> 65) then go back down to conservative fluid management CVP < 4 using diuresis. furosemide.
if you get a pt that has already been in severe ARDS for more than 37 hrs, what treatments can you NOT do?
prone positioning and cisatracurium infusion
In a pt with ARDS what is the most likely mechanical vent setting we will use for better outcomes?
AC mode was most commonly used to promote the application of low tidal volumes.
PS or SIMV is not a good option for ARDS because it will allow the pt to initiate a spontaneous breath ABOVE the goal tidal volume.
what are the classifications of the WHO for PAH?