Week 2: Interventions to address Sensory barriers to occupational performance
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
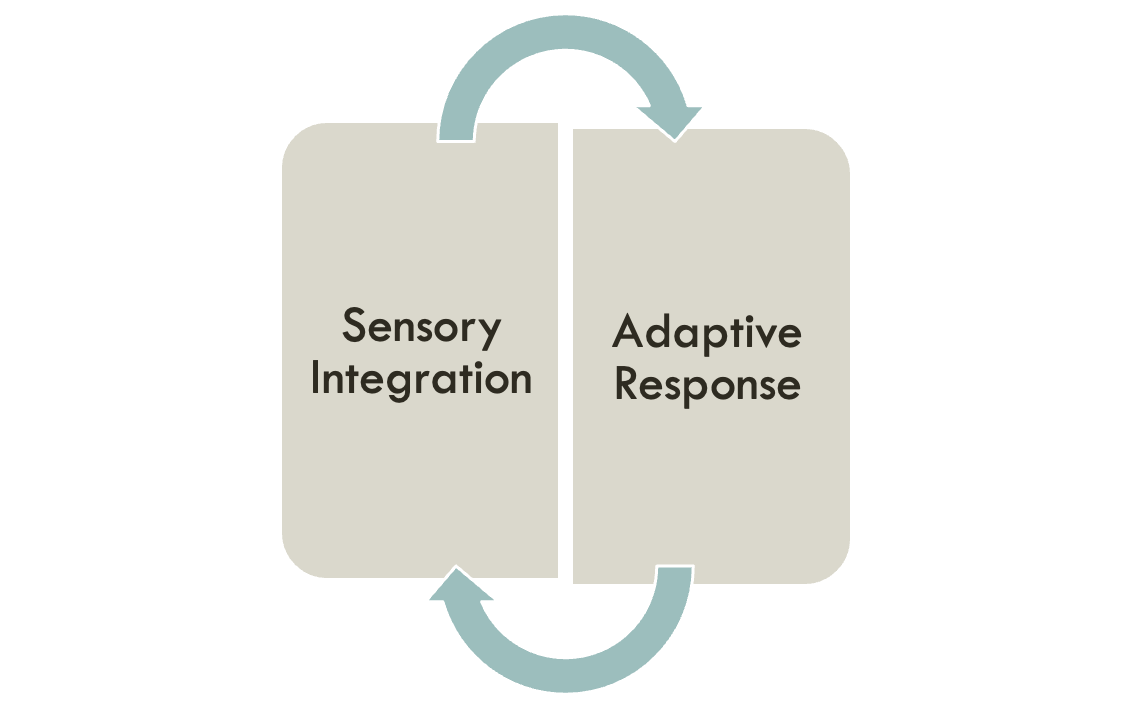
So what is sensory Integration
Register important sensory info. from the environment
Filter out irrelevant information
Make accurate interpretation of the information
Respond effectively to sensation
adaptive response
When sensations are processed efficiently, the child responds in an organized purposeful manner
When a child makes an _ that is more complex than any previously accomplished response, the brain attains a more organized state, & its capacity for further sensory integration is enhanced
General principles of Ayres SI theory
Most individuals automatically / effectively / developmentally take in and process sensory information (from the environment, movement of their bodies, and interaction with others)
Poor sensory processing often leads to ineffective motor and conceptual learning
Providing enhanced and meaningful sensory experiences results in enhanced sensory processing
By providing an optimal sensory environment and inviting active participation of the individual, both structural and functional growth occurs within the CNS
“Just-right challenge” within a playful context facilitates SI
SI promotes adaptive responses and occupational engagement
We rarely works on acquiring a specific skill-rather works on the foundation necessary to build the skill
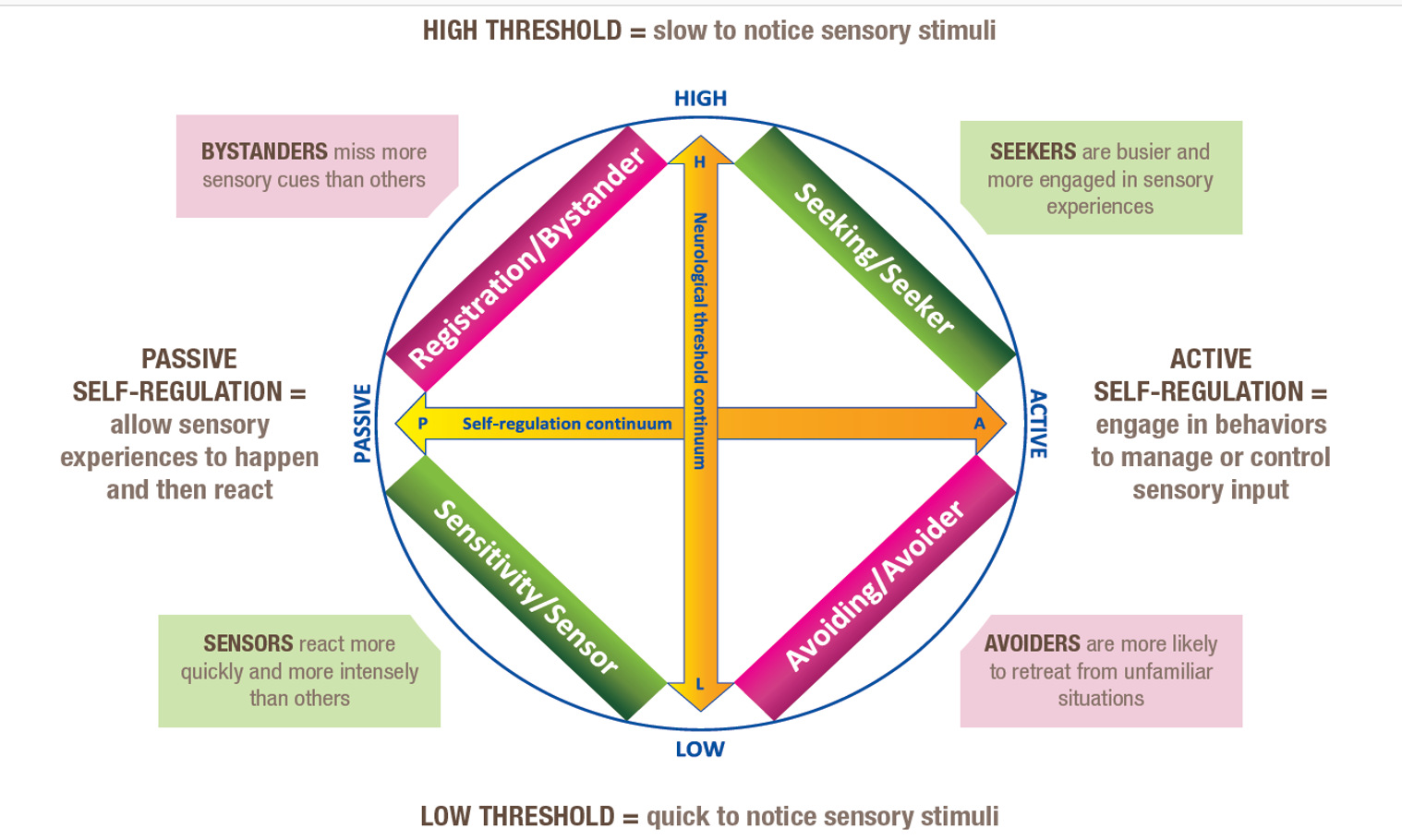
Essential concepts of the Dunn Model of sensory processing
Seekers: High Threshold/Active Self-Regulation
Avoiders: Low Threshold/Active Self-Regulation
Sensors (High Sensitivity): Low Threshold/Passive Self-Regulation
Bystanders (Low Registration): High Threshold/Passive Self-Regulation
Evaluating sensory sensitivities
It’s important to evaluate and document your client’s difficulty integrating or processing sensory information before doing sensory-based intervention (Choosing Wisely; Ten Things Patients and Providers Should Question)
Literature indicates that SI based intervention must be directly linked to assessment results (AOTA, 2018)
We learned different methods of evaluating a client’s sensory system in the Process course
Few examples?
Intervention consists of 2 phases-
Planning
Implementation
Planning
consists of 3 parts
Setting goals and objectives (should be related to occupational performance)
Type of service(s) delivery (e.g. direct, consultation, etc.)
Developing preliminary ideas about intervention
*Remember we always collaborate with the client and the caregiver
Deciding what to address first
There are no specific rules about what to address first but general guidelines
Address modulation difficulties early if appropriate
Hyporesponsiveness
Hyperresponsiveness
It is important to always evaluate and check if the client is making progress- ‘artful reflection’
Constantly reassess
Modify/change if necessary
factors to consider
relationship with ur client
establishing a safe environment
providing praise and verbal feedback
creating the just-right challenge
structure vs. freedom
understanding child’s volition
open communication with the client and the family
Relationship with your client
Therapeutic use of self
Playful interactions
Creating funny situations via pretend play (e.g. rescuing farm animals)
Establishing a safe environment
Physical and emotional safety
‘Artful ability’ to promote emotional safety
Choosing tasks that minimize risk of failure (e.g. beanbag toss)
Providing praise and verbal feedback
vAlso an ‘artful’ practice
vVerbal vs. gestural, frequency, timing, etc. (e.g. Taylor)\
https://www.reddit.com/r/HumansBeingBros/comments/cd1ya7/students_give_autistic_boy_a_silent_graduation_so/?utm_source=share&utm_medium=web2x
vCreating the Just-Right Challenge
Important key to intervention
vDeciding how far to push/stretch them (e.g. scaffolding, modeling while scaffolding, etc.)
vStructure vs. Freedom
Balancing between the 2 is also an art (e.g. Jimmy)
Understanding child’s volition
Lack of motivation maybe due to-
Task is “too difficult”
Child is convinced that it is too difficult
Arousal level is not in the ‘optimal band’
The theme is too ‘babyish’
Child can not identify to the activity (lacks meaning)
Open communication with the client and the family
Explain your clinical reasoning to the clients and the families
So they can develop strategies to learn, adapt and/or compensate across environments
Explain sensory concepts
They are used to hearing words like “lazy” or “bad”
By the time they are 6 or 7 they typically realize that they are different
Being an active participant facilitates progress
Explaining your rationale to your clients (when appropriate) opens door for collaboration
(e.g. Ava- picking and challenging herself to swing despite her fear)
Transfer skills into daily life
things to keep in mind for intervention
•Client factors
•(e.g. neurological thresholds, self-regulation strategies, modulation, discrimination, volition, influence of conditions such as CP, etc.)
•Environmental factors
•(physical, social, cultural contexts etc.)
•Task factors
•(demands placed on the client)
•Strategies to help child participate in meaningful & age-appropriate occupations
•(Direct and/or Indirect services)
=>
•Strategies to help child participate in meaningful & age-appropriate occupations
•(Direct and/or Indirect services)
Intervention ideas using SP quadrant scores
seeking/seeker
Less than other (-/- -) | Intervention | More than others (+/++) | Intervention |
Does not seek input | Provide variety or intensity (e.g. providing variety of art supplies) | Seeks and enjoys input | Provide more opportunities (e.g. using rocking chair while doing HW) |
Intervention ideas using SP quadrant scores
sensitivity/sensor
Less than other (-/- -) | Intervention | More than others (+/++) | Intervention |
Less detection | Increase awareness of changes in sensory experiences (e.g. point out “see how this tastes different..” | More detection | Provide more structured sensory experience (e.g. toys on waist-high shelf to avoid bending down to reach” |
Intervention ideas using SP quadrant scores
avoiding/avoider
Less than other (-/- -) | Intervention | More than others (+/++) | Intervention |
Less likely to withdraw from a stimuli | Provide organized input (e.g. turn down the TV during meal time) | Bothered by input | Make less input available (e.g. encourage “quiet time”) |
Intervention ideas using SP quadrant scores
registration/bystander
Less than other (-/- -) | Intervention | More than others (+/++) | Intervention |
Notices more | Provide more familiarity (e.g. having predictable routine) | Notices less/miss more than others | Provide more intensity (e.g. using heavy blankets to sleep) |
Provide enhanced sensation
•Activities that provide enhanced sensation to provide input &/or counterbalance poorly processed input
•Remember to use caution and upgrade sensory input gradually
•Constantly observe your client’s reaction
•Follow up with parents re: the child’s behavior after your session
Providing enhanced vestibular input
Vestibular input is one of the most powerful tools used to address SI challenges
Vestibular system is a specialized proprioceptor-provides info. about position & movement of head
Vestibular and Proprioception are considered the “unifier” in terms of integrating coordination of all other sensory systems
Otolith organs detect linear movement (up/down, side to side, etc.)
Semicircular canals detect angular movements
General guidelines for Vestibular input
vImportant to maintain a ‘just-right’ arousal state while challenging movts
vBe the agent that controls speed, direction & rhythmicity of vestibular input (e.g.- type of swing)
vSlow, rhythmic and linear movts tend to be calming and inhibitory VS. rotary movts that tend to be excitatory
vFind the balance between surprise & predictability
vGrade the degree of predictability & be mindful of the amount of surprise
vProne position thought to be more effective to activate otoliths and semicircular canal compared to sitting upright on a swing
vIf this is the case, what position would you recommend for a child with gravitational insecurity?
vDifferent positions facilitate stimulation of all vestibular receptors
vVestibular stimulation has an effect on the central nervous system for several hours
vThe more stimulation you provide, greater the length of effect
Specific Intervention Strategies for Gravitational Insecurity
Do not force movements
Give child control over movement in space
Work near the ground
Maintain feet on the floor
Allow child to see where they are going
Fear of moving backward in space
Start with linear vertical movements before rotational movements
Allow opportunities to fall from short distance on the floor followed by deep pressure or heavy work activities
Provide a positive experience and positive attitude
Specific Intervention Strategies for Hypo-responsiveness to movement
Provide variety of experiences for movement (think variety!)
Increase opportunity for movement (e.g. sit on a ball while coloring)
Work on maintaining a stable visual field while moving. E.g. swinging and hitting a target or rotate on a large ball to reach for a toy and then fixating on the OT’s face when stopped
Provide activities that promote B motor coordination
Specific Intervention Strategies for Laterality & B coordination
Do activities that require symmetrical patterns: pumping the swing, Pulling on a trapeze with both UE, propelling a scooter, catching/throwing a ball, etc.
Do activities that facilitate use of alternating patterns: pulling on a rope hand over hand, animal walks, wheelbarrow walk, swinging in prone while propelling on the floor using UE or pulling up a rope to retrieve something
Use rhythmic songs or clapping games during movement activities
Specific Intervention Strategies for Postural Control
Provide activities that require maintaining a stable visual field while moving
Consider the type of input being provided in relationship to the postural mechanism being facilitated
Linear movement affects extension against gravity
Rotary movement affects ocular motor control
Consider activities that facilitate improving overall balance & postural control (e.g. walking on unstable surface)
Providing enhanced proprioceptive input
Typically input to the proprioceptive system occurs at the same time that input is provided to the tactile system and the vestibular system
Muscle spindles/joints detect resistance & are primary receptors of proprioception
*Typically anytime we provide/facilitate movement with resistance we are providing proprioception
Input to this system typically has an inhibitory effect on the reticular activating system
•General guidelines for providing enhanced proprioceptive input
•The effect of input is thought to be temporary and the effects appear to be the most powerful when the input is being delivered
•Our system seems to habituate to this input quickly so staggered input with breaks may be more beneficial than prolonged input
•So what does it mean? (e.g. weighted vest)
Specific Intervention Strategies for Modulation
Provide opportunities for large amounts of proprioception to regulate level of arousal & organization of behavior
E.g. use inner tubes in games like “bumper cars” or rolling inside a stack of inner tubes and “crashing” into a large pillow; push-pull games: tug of war or combine with movt. (push OT on a scooter)
Increase attention to task & facilitate purposeful interactions with the environment (make sure child is active)
Pair prop. with behavioral responses (organization of behavior)
Specific Intervention Strategies for Discrimination
Improve ability to discriminate force & direction
E.g. high-fives (just-right vs. soft)
Improve body awareness
E.g. When in wt. bearing facilitate weight shifts by moving the child lightly to activate muscles
Provide opportunities to participate in activities with variety of experience such as push, pull, lift different sized objects/equipment during play
Pair prop. with targeted motor activity (adaptive response)
providing enhanced tactile input
•General guidelines for providing touch
•Allow client to guide touch
•Let the client see where touch is going to happen (avoid surprises)
•Deep pressure typically recommended to decrease tactile defensiveness
•
•Do not need to provide enhanced tactile input to the entire body
•Tactile sensation more tolerable when applied in the direction of hair growth
•Respect child’s reaction/feedback
•Be intentional about where to provide tactile input
•Start at the back of the hands and forearms
•Allow child to guide input to more sensitive areas such as face, feet, thighs, etc.
•Tactile input can influence the nervous system for about 30 minutes
•Monitor every time you provide with enhanced tactile input
•May respond differently to the same input on 2 different days
Specific Intervention Strategies for Tactile Modulation
Start with vestibular & prop. input, continue with deep pressure & then end with touch if tolerated
Provide inhibitory input such as deep pressure & proprioception (e.g. taco escape, wrestling)
Avoid unexpected and light touch
Try using surfaces vs. hand (hands change pressure while surfaces are constant)
Give child a sense of control over the play
Give options (touch w/ finger vs. tool)
Reduce sensory overload: lower voice, use of natural light, work in smaller space (e.g. coloring inside a tire tube)
Specific Intervention Strategies for Tactile Discrimination
Use variety! (e.g. if using brush- paint brushes & scrub brushes)
Cover equipment with interesting textures (e.g. towels, carpet, lycra sheet)
Present activities that provide rich tactile input (e.g. finding items in a ball pit)
When inside a container of balls- encourage change in position of the child via active movement
Provide activities that encourage discrimination such as objects inside bin full of rice or beans
Encourage localization of tactile input (e.g. stickers on arms & legs)
Play games with different textures (puzzles, play-doh, silly putty, etc.)
Sensory based motor disorder- Praxis
Refers to motor disorders that have their bases in poor sensory processing
From an SI perspective-
Poor praxis is due to poor ability to organize the plan necessary for purposeful behavior
Inability to process & integrate sensory info. (input) = poor foundation for motor planning (output)
Sensory systems essential for Praxis (internal)
Tactile Discrimination
Understanding the boundaries of the body
Refined information about where & how the body is moving relative to people & objects in the environment
Ongoing feedback during actions
Vestibular-Proprioception
Sensation of force & direction of movements; sense of weight, size, force of the body at rest & during movement
Sensory systems essential for Praxis (External)
Visual System
Surveying affordances in the environment
Interpreting space in which action will take place
Precise feedback during skilled actions
Auditory System
Spatial awareness
Sequential order of actions through self-talk
Understanding & following novel directions
Intervention activities for Practic disorders
Interventions to increase motor planning
Activities that facilitate feedback-dependent actions vs. feedforward vs. combination of both
Activities that promote Bilateral Integration
Activities that promote Ideation
Activities that promote Initiation & Execution
Activities that facilitate feedback-dependent vs. feedforward-dependent actions
Feedback-dependent tasks are the easiest
Perform motor-skills using feedback gained from actions (e.g. catching/throwing a ball)
Feedforward-dependent tasks get more challenging (anticipate all the variables)
Also known as Projected Action Sequences
During intervention planning, promote complex adaptive responses as appropriate
Tasks where child & target are both static (easiest) child & target are both moving (complex)
E.g. Santa’s helper delivering packages to different houses (think size of the target, size of the “package”, speed, timing, force, etc.)
Activities that promote Bilateral Integration
Activities that facilitate use of both sides of the body in a skillful manner
Promote activities that facilitate working in midline, crossing midline, symm. vs. asymm. movts
Many skills that promote bilateral coordination also involve projected action sequence
Activities that promote Ideation
Think of activities that promote active exploration & interaction with objects & environment
Facilitate thinking around-
What an object can do & what can be done with it?
What are some specific actions the child can do to “achieve a goal”?
What actions are appropriate for which objects?
How are they going to sequence the steps to accomplish the goal?
Intervention activities for Practic disorders
Activities that promote Initiation & Execution
Encourage participation in new tasks vs. practicing task that the child has mastered
Use simple verbal mnemonics such as “ready…set…go” or “1..2..3” to initiate action
Use of familiar objects or equipment in novel ways (e.g. pushing a bolster)
Generalization of newly learned action (e.g. jumping on pillow vs. innertube)
Consultation on modification
Individuals with SI difficulties benefit from modification of task, environment and other external factors such as routines
OT’s role as consultant to family members, teachers and other professionals
Focus on changing client and task and environmental factors
Advocate for the child
Indirect intervention (consultation) should be an integral part of a comprehensive OT service addressing SI differences
E.gs- parent education on different sensory concepts, Sensory Diet, home program, making appropriate recommendations to change task or environmental factors
Using strategies and techniques learned to promote collaboration
E.gs- Reinforcement, Modeling, coaching, Direct teaching
So what do I do?
Questions you should ask yourself
What area does this target?
Is there evidence for this type of activity?
How does my client respond to this particular input?
Discontinuing intervention
It depends!
6 months to 3-4 years (ideally as long as the child benefits!)
Occupational participation
Participate in daily tasks with minimal to no difficulties
Interference to participation caused by poor sensory integration or processing has been minimized or eliminated
No hard and fast rule
It depends on lot of factors
E.g. insurance coverage, reached a plateau, your gut feeling, outside resources, etc.