Head and Neck PART IV
1/172
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
173 Terms
What is a brachial cleft cyst (BCC)?
A congenital cystic anomaly arising from the second brachial arch
Where does a brachial cleft cyst typically appear clinically?
Anterolateral neck near the angle of the mandible
What is the etiology of a brachial cleft cyst?
Congenital anomaly
What is the epidemiology pattern of BCC?
Bimodal: at birth and in young adults
What percentage of BCCs are bilateral?
About 10%
Are brachial cleft cysts usually painful?
No, they are usually painless
What is the typical imaging appearance of a BCC?
Well‑defined round cystic mass posterolateral to the submandibular gland with no contrast enhancement
What is the T1 MRI appearance of a BCC?
Hypointense
What is the T2 MRI appearance of a BCC?
Hyperintense
What is the treatment for a brachial cleft cyst?
Complete surgical resection
What is the prognosis for a brachial cleft cyst?
Good
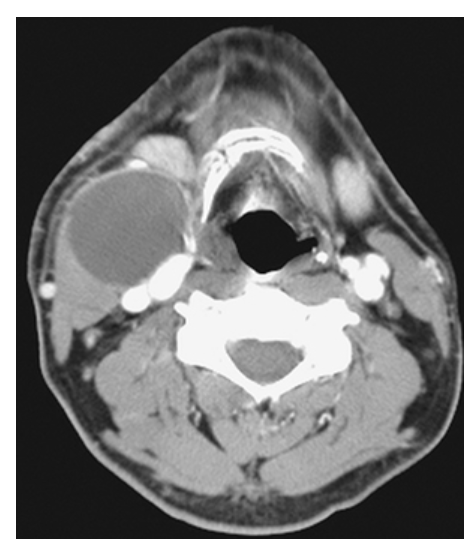
What does the figure show?
Brachial Cleft Cyst. Axial contrast-enhanced computed tomography (CECT) shows a cystic lesion in the right neck of a child located anteromedial to the sternocleidomastoid muscle, posterolateral to the submandibular gland, and lateral to the carotid space. In a child, this is a classic location and appearance for a second type BCC. Other differential considerations would include suppurative lymphadenitis or necrotic lymph node metastases (in an adult).
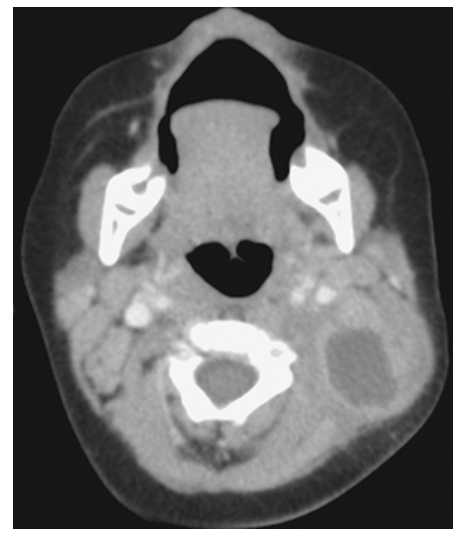
What does the figure show?
Brachial Cleft Cyst. Axial CECT in a child shows a cystic lesion in the left posterior neck with overlying infiltration of the fat representing an inflamed second BCC.
What is the most common benign orbital tumor in adults?
Cavernous hemangioma
What is the etiology of an orbital cavernous hemangioma?
Vascular malformation composed of large dilated endothelium‑lined channels with a fibrous capsule
What is the typical age range for orbital cavernous hemangioma?
Second to fourth decades
Which sex is slightly more affected?
Females
Where are cavernous hemangiomas usually located in the orbit?
Intraconal
What symptom do patients typically present with?
Painless proptosis
What is the T1 MRI appearance of an orbital cavernous hemangioma?
Isointense to hypointense, well‑circumscribed mass
What is the T2 MRI appearance of an orbital cavernous hemangioma?
Hyperintense to fat
What does post‑contrast T1 MRI show?
Marked enhancement
What is the treatment of choice for orbital cavernous hemangioma?
Surgical resection of the encapsulated tumor
What is the prognosis after surgical resection?
High cure rate
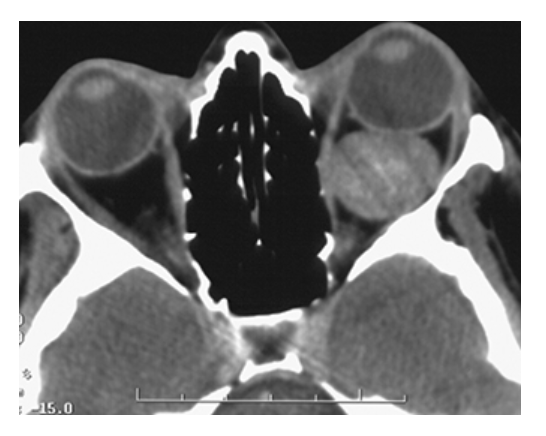
What does the figure show?
Cavernous Hemangioma. Noncontrast CT showing smoothly marginated, high-density, round, contrast-enhancing intraconal mass of the left orbit displacing the left globe anteriorly.
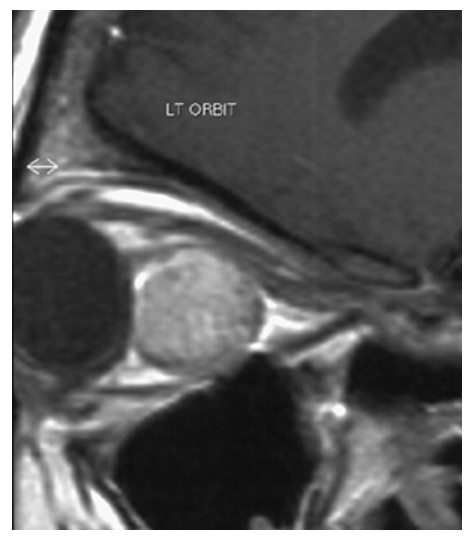
What does the figure show?
Cavernous Hemangioma. Sagittal T1-weighted postcontrast MR shows round, slightly hyperintense, retrobular mass displacing optic nerve superiorly.
What is an acquired cholesteatoma?
Accumulation of squamous epithelium in the middle ear
What is the etiology of an acquired cholesteatoma?
Varies depending on the specific type
How common is cholesteatoma?
Relatively common reason for ear surgery
What is the most common clinical sign?
Frequent recurrent painless ear discharge
What additional symptom is common?
Hearing loss
What imaging modality is preferred for evaluating cholesteatoma?
High‑resolution CT (HRCT)
What does HRCT show in cholesteatoma?
Mass‑like lesion in middle ear eroding ossicles and bone
What is MRI useful for in cholesteatoma?
Evaluating temporal bone, surgical planning, determining extent of disease
What is the T1 MRI appearance of acquired cholesteatoma?
Hypointense, with no enhancement after gadolinium
What is the T2 MRI appearance of cholesteatoma?
Hyperintense
What is the treatment for acquired cholesteatoma?
Surgical intervention
What is the prognosis for acquired cholesteatoma?
Good
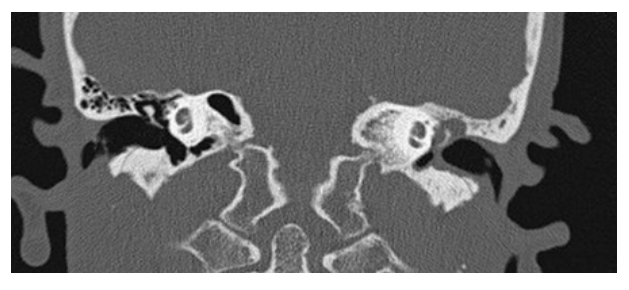
What does the figure show?
Cholesteatoma. Coronal NECT shows soft tissue density in the left middle ear with thickening of the tympanic membrane. The left scutum has a blunted appearance (compared to sharp tip of normal right side). Findings are consistent with a cholesteatoma.
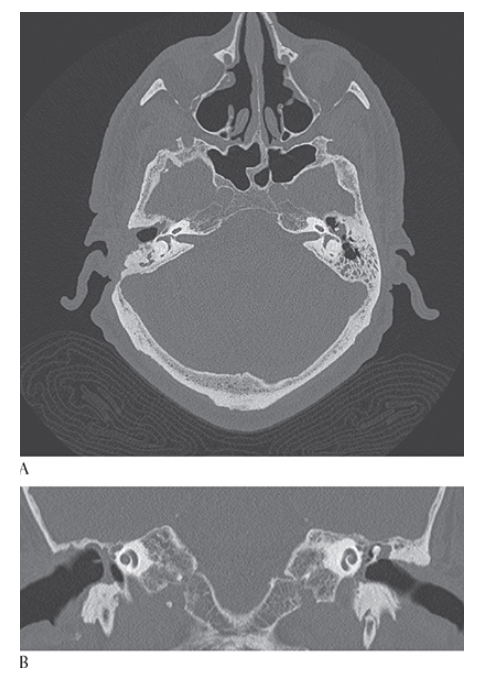
What is A
Cholesteatoma. Axial NECT of the temporal bones shows soft tissue in the left middle ear located lateral to the ossicles in the epitympanum (Prussak space). Mastoidectomy has previously been performed on the right. Coronal CT
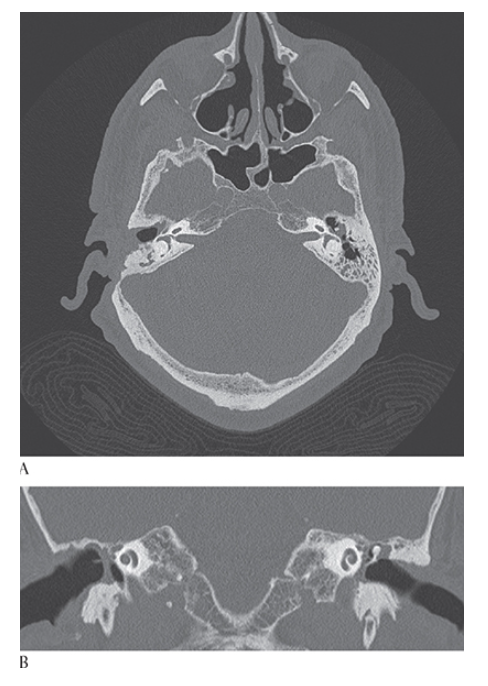
What is B
Cholesteatoma. Axial NECT in same patient shows soft tissue in left middle ear within Prussak space of the epitympanum with blunting of the scutum. Right mastoidectomy is present.
What is a glomus tumor (paraganglioma)?
A benign, slow‑growing, hypervascular lesion
From what cells do paragangliomas arise?
Neural crest paraganglion cells of the extracranial head and neck
How are glomus tumors named?
According to anatomic location (e.g., glomus vagale, glomus jugulare, glomus tympanicum)
Which glomus tumor is most common?
Glomus vagale
What percentage of patients have multiple lesions?
5%
What percentage of patients have a familial history?
Almost 30%
What symptoms occur with paragangliomas?
Depends on tumor location
What is the T1 MRI appearance of a glomus tumor?
Mixed signal intensity mass with multiple flow voids
What is the T2 MRI appearance of a paraganglioma?
High signal
What does post‑contrast T1 MRI show?
Hyperintense mass with flow voids giving a “salt‑and‑pepper” appearance
What is the treatment for glomus tumors?
Surgery, radiation therapy, or both
What is the prognosis for glomus tumors?
Good; benign tumor
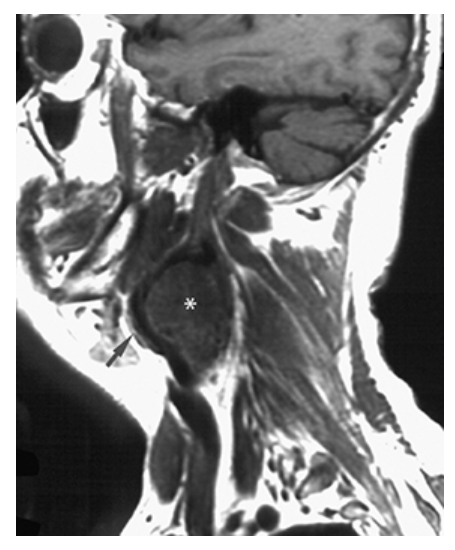
What does the figure show?
Glomus Tumor (Glomus Vagala). T1-weighted left parasagittal image shows an intermediate signal mass (asterisk) of the upper neck at the carotid bifurcation. The external carotid artery (arrow) is displaced anteriorly.
What does the figure show?
Glomus Tumor (Glomus Vagala). Postcontrast T1-weighted axial image shows a large markedly enhancing mass of the upper neck splaying the internal and external (arrows) carotids above the common carotid artery bifurcation.

What does the figure show?
Glomus Tumor (Glomus Tympanicum). Axial CT shows soft tissue in the right middle ear overlying the cochlear promontory. Permeative bone loss is seen in the mastoid bone adjacent to the posterior fossa on the right.
What does the figure show?
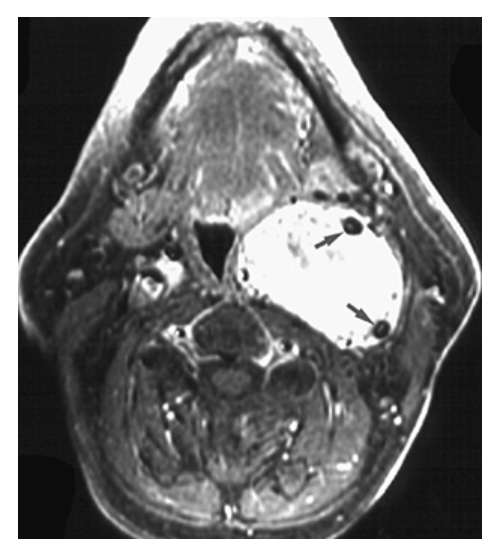
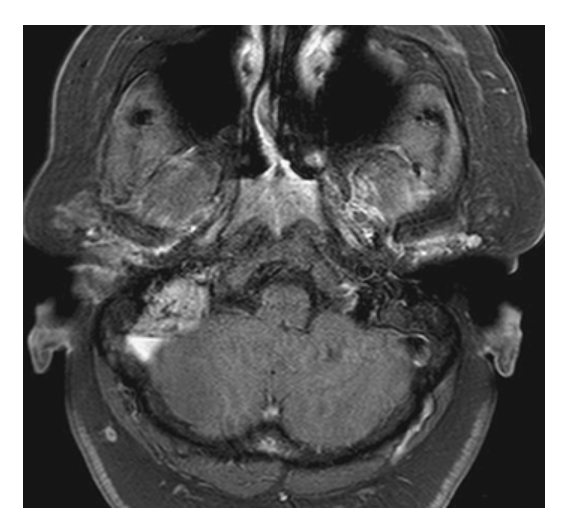
Glomus Tumor (Glomus Jugulotympanicum). Axial fat-sat (FS) T1W with gadolinium shows enhancing mass in right mastoid region and jugular fossa. Serpentine flow voids represent vessels.
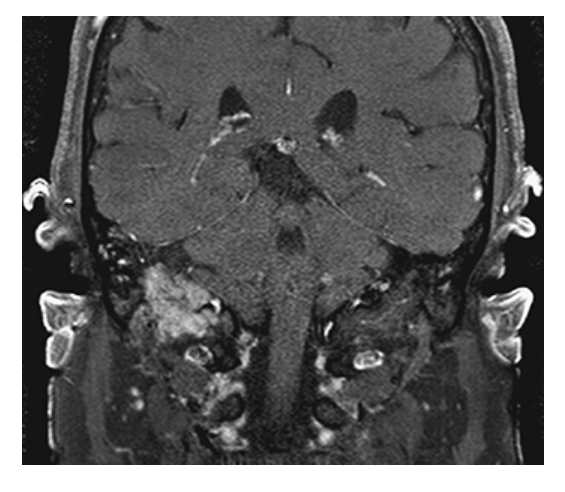
What does the figure show?
Glomus Tumor (Glomus Jugulotympanicum). Coronal FS T1W with gadolinium shows enhancing mass extending from right middle ear into jugular fossa representing a glomus jugulotympanicum tumor (paraganglioma).
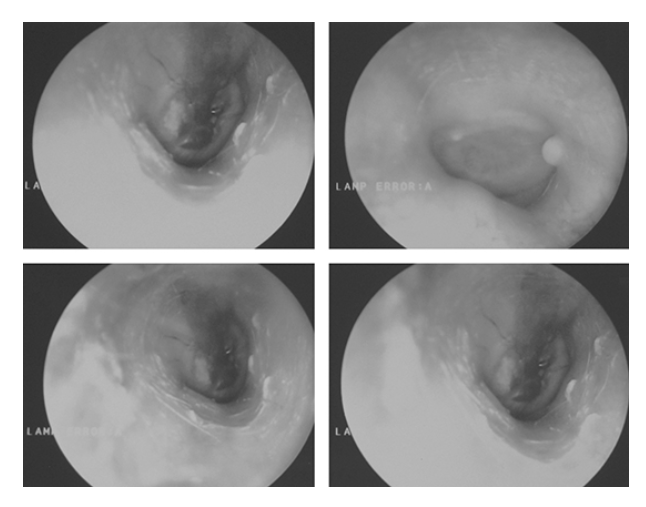
What does the figure show?
Glomus Tumor (Glomus Tympanicum). Clinical otoscopic images show a (blue) vascular mass located behind the eardrum. This corresponds to the mass seen on the cochlear promontory
What are the major salivary glands?
Parotid, submandibular, and sublingual
Which gland forms the majority of salivary neoplasms?
Parotid gland
What are minor salivary glands?
Hundreds of small glands throughout mucosa and aerodigestive tract
What is a suspected cause of benign and malignant salivary lesions?
Radiation
What is the typical age range for parotid gland tumors?
Fourth to fifth decades
What percentage of parotid gland tumors are benign mixed tumors (pleomorphic adenomas)?
>80%
In which glands does malignancy become more common?
Submandibular, sublingual, and minor salivary glands
What are typical features of benign parotid tumors?
Palpable, discrete, mobile
What symptoms suggest malignancy?
Pain, rapid expansion, poor mobility, facial nerve weakness
What imaging effect may parotid tumors cause?
Mass effect displacing surrounding anatomy
How are lesions best identified on MRI?
T1‑weighted images amid bright parotid fat
What is the T2 appearance of benign parotid tumors?
Very bright
What is the T2 appearance of malignant parotid tumors?
Mixed signal intensities
What is the treatment for benign parotid tumors?
Surgical removal
What is the treatment for malignant parotid tumors?
Complete surgical resection with radiation therapy
What percentage of parotid tumors are benign?
80%
What are the 10‑year survival rates for malignant parotid tumors (Stages I, II, III)?
90%, 65%, 22%
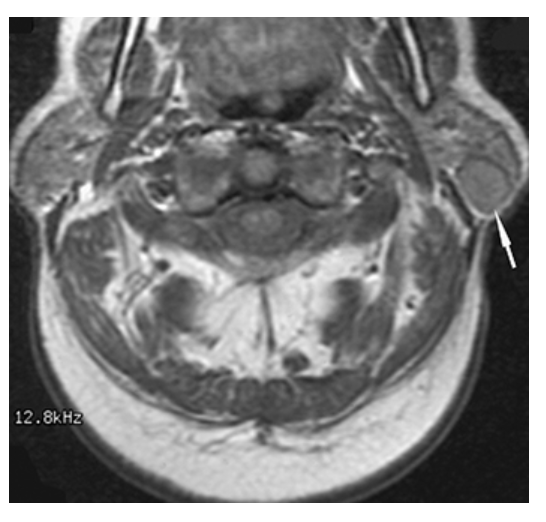
What does the figure show?
Parotid Gland Tumor. T1-weighted axial MRI of the parotid gland demonstrates a well-defined, round, low-signal intensity mass (arrow) in the posterior aspect of the superficial lobe of the left parotid gland.
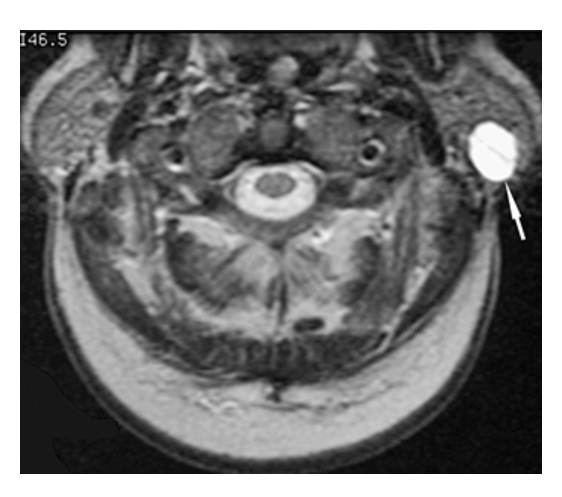
What does the figure show?
Parotid Gland Mass. T2-weighted axial MRI of the parotid gland demonstrates a well-defined high-signal intensity mass (arrow) of the posterior aspect of the superficial lobe of the left parotid gland consistent with a pleomorphic adenoma.
What is a thyroid goiter?
Enlargement of the thyroid gland causing anterior neck swelling
What is another name for this type of goiter?
Nontoxic goiter
What causes nontoxic goiter in the United States?
Increased TSH due to a defect in thyroid hormone synthesis
What is the epidemiology of thyroid goiter?
Occurs in 1%–10% of the population
What is a visible sign of thyroid goiter?
Swelling at the anterior base of the neck
What symptoms may occur due to mass effect?
Coughing, dysphagia, dyspnea
Are nontoxic goiters fast or slow growing?
Slow growing
What is the T1 MRI appearance of a normal thyroid gland?
Intermediate signal
What is the T2 MRI appearance of a normal thyroid gland?
Higher signal
What can MRI show in thyroid goiter?
Neck anatomy, tracheal compression/deviation, intrathoracic extension
What therapy may reduce goiter size?
Thyroid hormone suppressive therapy (T4)
What treatment provides quick relief of obstructive symptoms?
Surgical removal or decompression
What is the prognosis for thyroid goiter?
Good
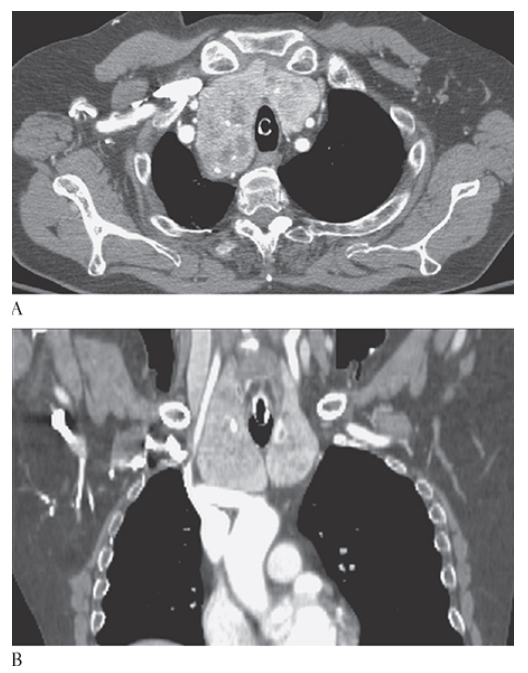
What is A
Thyroid Goiter. Axial and coronal
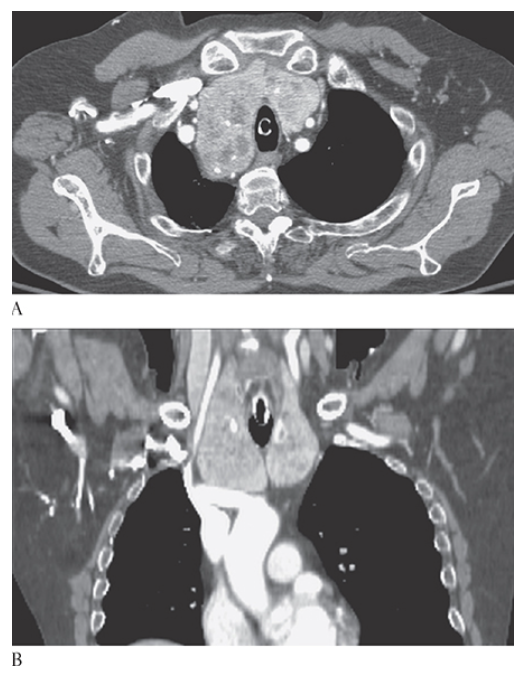
What is B
Thyroid Goiter. Axial CECTs show an enlarged heterogeneously enhancing thyroid gland with multiple low-attenuation cysts and calcifications, respectively.
What is a peritonsillar abscess (PTA)?
Accumulation of pus in the tonsillar bed with medial displacement of the tonsil
What causes a peritonsillar abscess?
Viral or bacterial infection
What percentage of head and neck infections in children are PTAs?
~50%
What is the most common age range for PTA?
20–40 years
Are males or females more affected by PTA?
Equally affected
What is a common early symptom of PTA?
Progressively worsening sore throat (often unilateral)
What symptoms suggest abscess location?
Pain localized to one side