First Aid USMLE Step 1: Pulmonology
1/161
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
162 Terms
Pulmonary Hypoplasia
Poorly developed bronchial tree with abnormal histology usually involving right lung
Associated with congenital diaphragmatic hernia and bilateral renal agenesis (Potter sequence)
.
POTTER sequence associated with:
Pulmonary hypoplasia
Oligohydramnios (trigger)
compression of developing fetus
Twisted face
Twisted skin
Extremity defects
Renal agenisis - Bilateral (in utero)
Bronchogenic cyst
Caused by abnormal buddy of foregut and dilation of terminal or large bronchi
Discrete round sharply defined and air-filled density on CXR
Drain poorly and cause chronic infections
Compliance and elastic recoil
Inverse related
compliance = distention or volume change with given pressure change
Elastic recoil = lungs intrinsic tendency to collapse
Increased compliance = decreased elastic recoil
Conditions that decrease compliance
Pulmonary fibrosis
Pneumonia
Pulmonary Edema
Note: the lower compliance the higher the elastic recoil of the lung and the smaller the FRC (chest wall tendency balanced at lower expansion or volume)
Conditions with increased compliance
Emphysema
Normal aging
Surfactant increases compliance
Note: the greater compliance the lower elastic recoil the higher the FRC (chest wall tendency to expand must be balanced)
Neonatal respiratory distress syndrome Pathophysiology
how will it look on CXR
Surfactant deficiency - increased surface tension - decreased compliance - increased elastic recoil of lung - increased work of breathing
alveolar collapse (ground glass appearance of lung fields)
LACK surfactant = collapse and hyaline membrane formation
Neonatal Respiratory Distress Syndrome Screening Test
Lecithin-Sphingomyelin ratio (L/S) in amniotic fluid
lectin is produced by surfactant
L/S > 2 indicates lung maturity
L/S > 1.5 is predictive of NRDS
Other tests include: foam stability index test and surfactant-albumin ratio
Risk factors for NRDS
Prematurity
28-35 w for surfactant to delop
Maternal diabetes
increased insulin= decreased surfactant
C-section delivery
decreased release of fetal glucocorticoids due to lack of stress= decrease surfactant production
Treatment of NRDS
Maternal steroids before birth
Artificial surfactant for infant
Therapeutic supplemental oxygen in Neonate
can result in
R I B
Retinopathy of prematurity
Intraventricular hemorrhage
Bronchopulmonary dysplasia
Epithelial Progression in airways
Pseudostratified columnar ciliated
Simple Columnar ciliated
Simple Cuboidal columnar ciliated
Simple Squamous
Foreign Body Obstruction
Right mainstem bronchus is wider and more in line position with trachea = most common path for foreign object
Aspiration while upright: enters inferior segment of inferior right lobe
Aspiration while supine: most dependent areas are superior segment of right lower lobe and posterior regions of upper lobes
Structures perforating diaphragm at T8
Inferior vena cava
Structures perforating diaphragm at T10 (esophageal hiatus)
Esophagus
Vagus nerve (2 trunks)
Structures perforating diaphragm at T12 (aortic hiatus)
Aorta
Thoracic duct
Azygous vein
Bifurcation of Trachea " BiFOURcation"
T4
Bifurcation of Abdominal Aorta "BiFOURcation"
L4
Bifurcation of Common Carotid "BiFOURcation"
C4
Tidal volume
Air that moves in and out with each normal inspiration and expiration
Normal TV = 0.5 L
Inspiratory reserve volume (IRV)
Air that can still be breathed in after normal inspiration
Inspiratory capacity
TV and IRV combined
Expiratory reserve volume (ERV)
Volume that can still be exhaled after normal exhalation
does NOT include residual volume
Residual volume (RV)
Volume left in lung after maximal exhalation
Normal RV = 1.2 L
Functional residual capacity
Volume of gas that remains in lung after normal expiration
FRC = ERV + RV

Vital capacity
Volume that can be maximally inhaled and exhaled
Total lung capacity - Residual volume
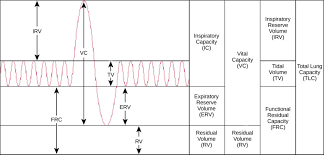
Total lung capacity
TLC = Inspiratory capacity + Functional residual volume
TLC = (IRV + TV) + (ERV + RV)
Volume present in lungs after maximal inspiration
Note: cannot be measured by spirometry
Normal TLC = 6 L
Capacity
Sum of 2 or more physiologic volumes
Physiologic Dead Space
Volume of air which is not involved in gas exchange
Includes anatomical dead space of conducting airways plus alveolar dead space (ventilated but not perfused regions)
Normal lungs: physiologic DS = anatomical DS
Conditions that improve with O2 administration vs those that don’t
Conditions that improve with O₂ administration= increased PaO₂):
- oxygen can still reach ventilated parts of the lung, but blood flow is obstructed.Example conditions:
Pulmonary embolism (PE)
Chronic obstructive pulmonary disease (COPD) with significant airflow obstruction
Why they improve with O₂: increases the available oxygen in the blood, as some areas of the lung are still able to ventilate despite poor blood flow (in PE, for example).
Conditions that do not improve with O₂ administration = no increase in PaO₂
perfusion problems, where blood flow is compromised
Example conditions:
Intrapulmonary shunt (e.g., pneumonia, ARDS)
Foreign body aspiration (airway obstruction)
Atelectasis
Shunting or Obstructions prevent 02 from reaching the areas in which perfusion occurs
Hemoglobin
Deoxygenated form (T or Taut): low affinity for oxygen: promotes release or unloading of oxygen in tissues
Oxygenated form (R or Relaxed): high affinite for oxygen
Positive cooperativity and negative allostery
Factors that Decrease Oxygen Affinity of Hb
Chloride
H+ (hypoxia or anemia - lactic acidosis)
Carbon dioxide (increased metabolic activity)
2,3 BPG (elevated in setting of hypoxia: chronic high altitude, chronic lung disease, heart failure)
Increased temperature
High altitude
Low affinity = improved unloading = shift to right
Methemoglobinemia
Methemoglobinemia = Fe3
Oxidized form (Fe 3+) Hb has decreased oxygen
increased affinity for cyanide
Presets with chocolate colored blood: dusky discoloration of skin (similar to cyanosis).
Treated with methylene blue and vitamin C
Causes of Methemoglobinemia
Nitrites (dietary intake or polluted/high altitude H2O)
Benzocaine
Dapsone
TMP-SMX
Induced Methemoglobinemia
Patients with cyanide poisoning can be treated wit nitrites followed by thiosulfate
Carboxyhemoglobin
Hb bound by CO: decreased oxygen binding capacity with left shift in oxygen-hemoglobin dissociation curve (increased affinity) = impaired unloading in tissues
Hb has 200 fold affinity for CO compared to O2
Treatment: 100% O2 and hyperbaric O2
Fetal Hemoglobin HbF (alpha-gamma)
Higher oxygen affinity due to decreased affinity for 2,3-BPG (negative allosteric regulator of oxygen affinity)
High Altitude Physiology: Initial first 2 days
Less oxygen in air so the first effect is hypoxia and decreased dissolved oxygen in the blood.
The immediate response will be stimulation of peripheral chemoreceptors which in turn in send signals to respiratory drives to breath more.
Hyperventilation develops which in turn leads to Respiratory Alkalosis (Altitude sickness)
Respiratory alkalosis will shift the hemoglobin dissociation curve to the left so that Hb can pick up O2 easier.
The kidney will respond to alkalosis by generating hydrogen ions and this will correct the pH back to normal.
Hemoglobin deoxygenation curve
right =
right = release of O2
High Altitude Physiology: After 2-3 Days
After 2-3 days the 2,3 BPG level in RBC will increase and this will shift the Hb curve (this time) to the right making O2 delivery easier to tissues.
Increase of EPO secretion (takes about 1 week) leading to polycythemia and increased hematocrit level.
Finally there is an increase in mitochondria
Note that no matter how long you stay in high altitudes the PAO2, PACO2, and Hemoglobin saturation will remain decreased as we breath less FIO2 and we continue to hyperventilate
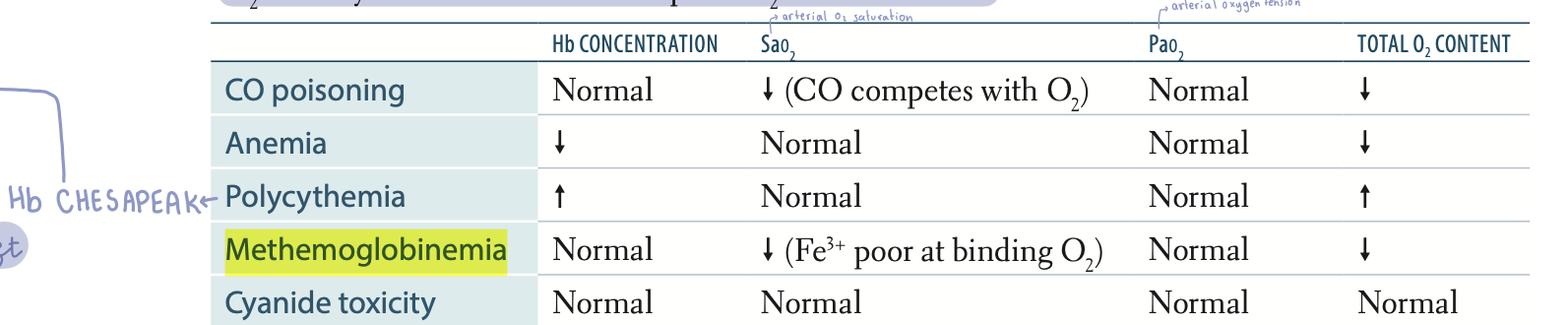
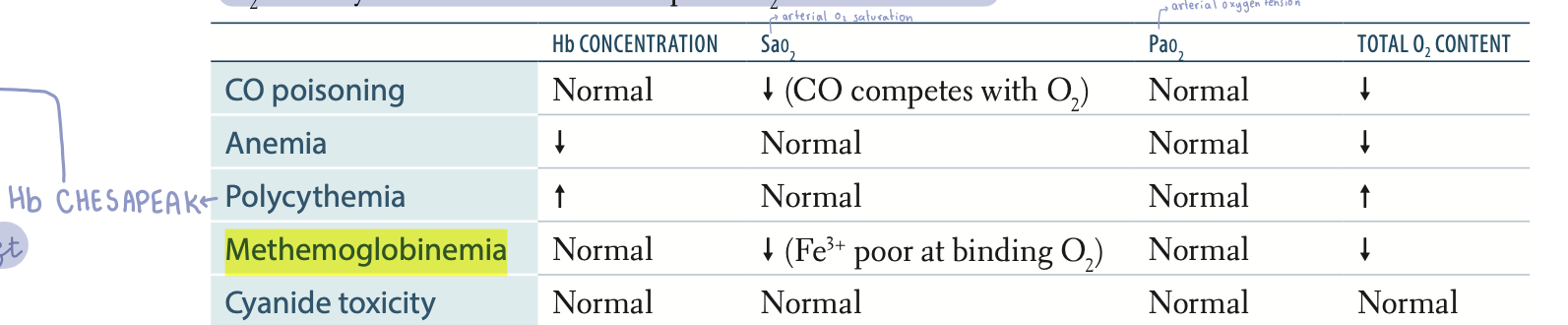
CO poisoning: Findings
Hb concentration
SaO2
PaO2
oxygen content
Normal Hb concentration
Decreased SaO2
Normal PaO2
Decreased oxygen content
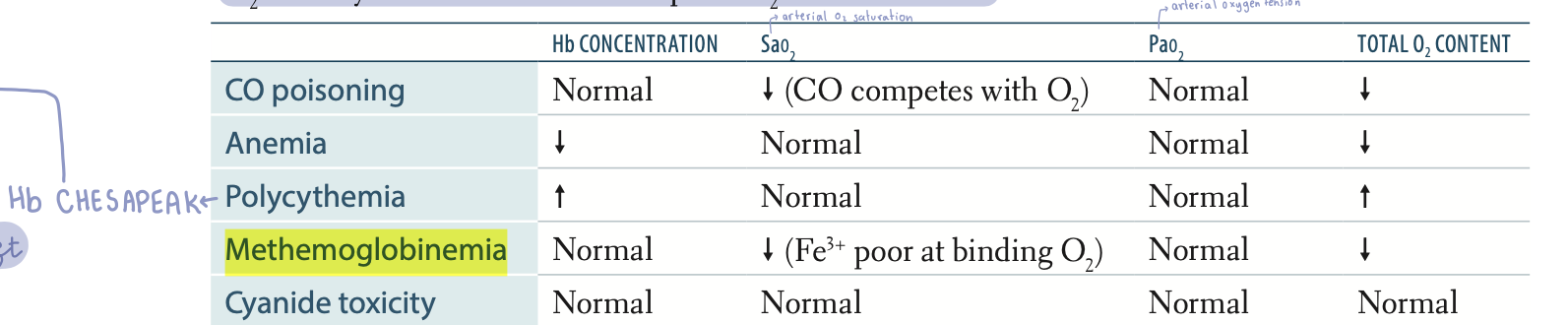
Anemia: Findings
Hb concentration
SaO2
PaO2
oxygen content
Decreased Hb concentration
Normal SaO2
Normal PaO2
Decreased oxygen content
Polycythemia Findings
Hb concentration
SaO2
PaO2
oxygen content
Increased Hb
Normal SaO2
Normal PaO2
Increased oxygen content
Perfusion-limited Gas exchange
Oxygen (normal healthy individual)
CO2
N2O
Gas equilibrates along the length of the capillary: diffusion can be increased only with increased blood flow
Diffusion limited Gas exchange
O2 (Emphysema and fibrosis)
CO
Gas does not equilibrate by the time blood reaches the end of the capillary
A-a Gradient
Difference in between partial pressures of oxygen in Alveoli versus arterioles
A-a = PAO2 - PaO2
Causes of increased A-a gradient
Shunting
VQ mismatch
Fibrosis (impaired diffusion)
Causes of Hypoxia (decreased oxygen delivery to tissues)
Decreased Cardiac output
Hypoxemia
Anemia
CO poisoning
Causes of Hypoxemia (decreased PaO2)
Normal A-a gradient:
High altitude or hypoventilation
Increased A-a gradient:
VQ mismatch, diffusion limitation or right to left shunt
Causes of Ischemia (loss of blood flow)
Impeded arterial flow
Impaired venous drainage
Perfusion and Ventilation of lung zones
Both ventilation and perfusion are highest at the base of the lung (zone 3)
Perfusion (Q) increases more rapidly as you move from apex to base
V/Q decreases as you move from apex to base
V/Q at apex = 3
V/Q at base = 0.6
Bohr effect
High H+ concentration in peripheral tissues - binds Hb decreasing its affinity for O2 - facilitates oxygen unloading
Causes of Rhinosinusitis
Acute: viral URI
Most common superimposed bacterial infections:
S. Pneumoniae
H. influenzae
Moraxella Catarrhalis
Epistaxis
Most common: mild epistaxis from anterior inferior part of nasal septum: Kiesselbach plexus
Life-threatening hemorrhages can occur in posterior segment: sphenopalatine artery (branch of maxillary artery)
Head and Neck cancers
Mostly squamous cell carcinoma
Risk factors: tobacco, alc and HPV 16 (oropharyngeal) and EBV (nasopharyngeal)
Field cancerization: carcinogen exposure damages wide mucosal area: multiple tumors
Nasopharyngeal carcinoma may present with
unilateral nasal obstruction, discharge, epistaxis.( nose bleeds)
Eustachian tube obstruction may lead to otitis media +/– effusion, hearing loss.
Laryngeal papillomatosis
also called recurrent respiratory papillomatosis.
Common benign laryngeal tumor (eg, vocal cords), especially in children. Associated with HPV-6 and HPV-11.
DVT
Swelling of extremity
Redness and warmth
Pain
Homan sign: dorsiflexion of foot produces calf pain
Labs: elevated D-dimers (highly sensitive but non-specific)
Most common in proximal deep veins of the leg: femoral vein
Treatment of DVT
Use unfractionated heparin or low-molecular
weight heparins (eg, enoxaparin) for
prophylaxis and acute management.
.
Use direct anticoagulants (eg, rivaroxaban,
apixaban) for treatment and long-term
prevention.
Virchows Triad
Stasis (post-op immobility)
Hypercoagulability (defects in coagulation cascade, malignancy, OCP, smoking)
Endothelial damage (exposed collagen triggers clotting cascade)
PE
V/Q
VQ mismatch: ventilated sections without perfusion: increased physiologic dead space
normal V/ decreased Q
PE Presentation
Sudden onset dyspnea
Pleuritic chest pain
Tachypnea and tachycardia ( EKG)
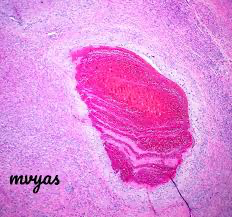
Lines of Zahn
Distinguish a pre-mortem from a post-mortem thrombus
Interdigitating areas of pink (platelets and fibrin) and red blood cells found in thrombi formed before death
Types of Emboli that can cause PE
FAT BAT
Fat
Air
Thrombus
Bacteria
Amniotic fluid
Tumor
Fat Embolus
triad
Associated with long bone fractures and liposuction
Classic triad:
Hypoxemia
Neurologic abnormalities
Petechial rash
Amniotic fluid embolus
Anaphylactoid reaction: amniotic fluid causes
occlusion and vasospasm of the maternal pulmonary circulation leading to RIGHT ventricular failure decreased CO and severe ventilation perfusion mismatch. Resulting hypoxia and hypotensive shock ultimately causes cardiopulmonary arrest
Tissue factor (thromboplastin) is released from amniotic fluid and triggers DIC
Fetal squamous cells and mucin are found in amniotic fluid emboli occluding maternal pulmonary arteries
Air emboli
Caisson Disease or Decompression sickness: Nitrogen bubbles precipitate in ascending divers
“A 42-year-old professional diver presents to the emergency department 2 hours after surfacing from a deep-sea dive. He reports severe joint pain, nausea, and weakness. On examination, he is tachypneic and has cyanosis. Which of the following best explains the pathophysiology of this condition?”
Other causes: iatrogenic secondary to invasive procedures (central line placement)
PFT picture in Obstructive lung diseases
DECREASED FEV1/FVC ratio = HALLMARK
Severely decreased FEV1
increased TLC
.
retention of CO2!!!
vasoconstriction
VQ mismatch: increased physiologic dead space
Chronic Bronchitis Diagnosis (Clinical)
Classified as Chronic Obstructive Pulmonary Disease (COPD)
Productive cough for > 3 months (does not have to be consecutive) for more than 2 consecutive years
Most common in smokers
SYMP in Chronic Bronchitis
Wheezing
Crackles
Cyanosis: early-onset hypoxemia due to shunting: perfusion of mucus plugged region of the lung with no ventilation
Late-onset dyspnea (live at low SaO2)
CO2 retention and hypercapnea
Secondary (reactive) polycythemia (increased EPO)
Histological Findings in Chronic Bronchitis
Hypertrophy and Hyperplasia of mucus-secreting glands in bronchi:
Increased Reid Index > 0.5
Pathophysiology of Emphysema
Enlargement of air spaces due to destruction of alveolar walls:
Increased activity of neutrophil elastase leading to destruction of elastic fibers
Increased compliance = decreased elastic recoil
Increased FRC
Decreased diffusion capacity for CO resulting from destruction of alveolar walls and capillaries (decreased Surface area)
Emphysema findings
PINK PUFFER - Pursed lip breathing (increased resistance - increased intraluminal airway pressures prevents premature collapse on exhalation)
Barrel shaped chest (increased AP diameter)
Cachexia: increased energy expenditure due to respiratory efforts
Flattened diaphragm (increased TLC)
Increased lung field lucency
Panacinar Emphysema
Alpha-1-Anti-trypsin deficiency
Lower lobes
Centriacinar Emphysema
Smoking
Upper lobes
Asthma def
Bronchial hyper responsiveness causing reversible broncho constriction
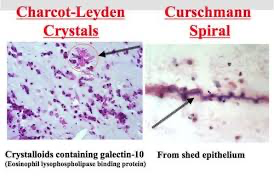
Asthma Histological findings
Smooth muscle hypertrophy
Curschmann spirals (shed epithelium forming whorled mucus plugs)
Charcot-Leyden crystals (eosinophilic hexagonal double-pointed needle-like crystals formed from breakdown of eosinophils)
Types of Asthma
Allergic (extrinsic) asthma
Non-allergic (intrinsic) asthma: normal IgE (triggered by pulmonary infections, aspirin ingestion, cold air, inhaled irritants, stress and or exercise)
Intrinsic Asthma
Non-allergen mediated
Causes:
Viral URI (RSV, rhinovirus, and parainfluenza virus)
Behavioral: exertion and stress
Chemical
Drug sensitivity (NSAIDs and aspirin)
Diagnosis of Asthma
symptoms
Inspiratory/ expiratory
test
Clinical picture: cough wheezing tachypnea dyspnea hypoxemia
decreased inspiratory/expiratory ratio
expiration is prolonged due to increased airway resistance.
Methacholine challenge
Spirometry: obstructive pattern
during serious attack of asthma we can see
pulsus paradoxus
A drop in systolic blood pressure (SBP) >10 mmHg during inspiration.
Bronchiectasis
symptoms
Chronic necrotizing infection of bronchi leading to permanently dilated airways
Recurrent infections
Hemoptysis
Digital clubbing
Fowl smelling breath and purulent sputum
Conditions associated with bronchiectasis
Impaired ciliary motility:
Smoking
Kartagener Syndrome
Cystic fibrosis
Allerigc Bronchopulmonary Aspergillosis
type 1 HS
eosinophillia
Restrictive Lung Diseases
FEV1 / FVC
lung volumes
Decreased lung volumes: decreased TLC
FEV1/FVC = normal or increased
Restrictive Lung Diseases related to poor breathing mechanics
Extra-pulmonary causes: Peripheral hypoventilation with normal A-a gradient
Poor muscular effort: polio Myasthenia Gravis Guillain-Barre Syndrome
Poor structural apparatus: scoliosis or morbid obesity
Interstitial lung diseases
Pulmonary causes of restrictive lung disease with decreased diffusion capacity and increased A-a gradient
ARDS
NRDS (hyaline membrane disease)
Pneumoconioses (anthracoses silicosis asbestosis)
Sarcoidosis (bilateral LAD non-caseating granulomas increased ACE and vitamin D = increased calcium)
Idiopathic pulmonary fibrosis: increased collagen deposition and fibrosis leading to honeycomb appearance and digital clubbing
Goodpasture Disease
Linear IF + antibodies BM
hematuria
Granulomatosis with Polyangiitis (Wegeners)
Negative IF/Pauci-immune (no IgC3 deposition)
PR3-ANCA/c-ANCA,
Pulmonary Langerhans cell Histiocytosis (eosinophilic granulomas CD1a CD14 positive Bierbeck granules)
Hypersensitivity Pneumonitis
Drug toxicity: bleomycin Busulfan amiodarone MTX
Hypersensitivity Pneumonitis
Mixed type III and IV HSR to environmental antigen
NONcaseating granulomas
Dyspnea cough chest tightness headache
fever when acute ( self resolving)
,
Classic script: farmer or pet store owner with exposure to envioemental factors ( hay, birds ect )
elevated serum levels of…..
sarcoidsois
Hyper CA ( bc noncaseating granuloma)
ACE
elevated CD4/CD8 ratio in bronchoalveolar lavage fluid
who will we see sarcoidosis in
Black
young female
key word for sarcoidosis
bilateral lymohadenopathy
hilar nodularity
Sarcoiddosis Mneumonic
SARCOIDS
Associated with granulomas (noncaseating epithelioid, containing microscopic Schaumann and Asteroid bodies),
Rheumatoid arthritis–like arthropathy, Calcium ( HYPER)
Ocular uveitis,
Interstitial fibrosis,
vitamin D activation (due to 1a-hydroxylase in macrophages),
Skin changes (eg, lupus pernio, erythema nodosum)
Arsenic poisoning
inhibits lipoic acid.
clinical findings: imagine a vampire (pigmentary skin changes, skin cancer), vomiting and having diarrhea, running away from a cutie (QT prolongation) with garlic breath.
c
squamous cell carcinoma
angiosarcoma
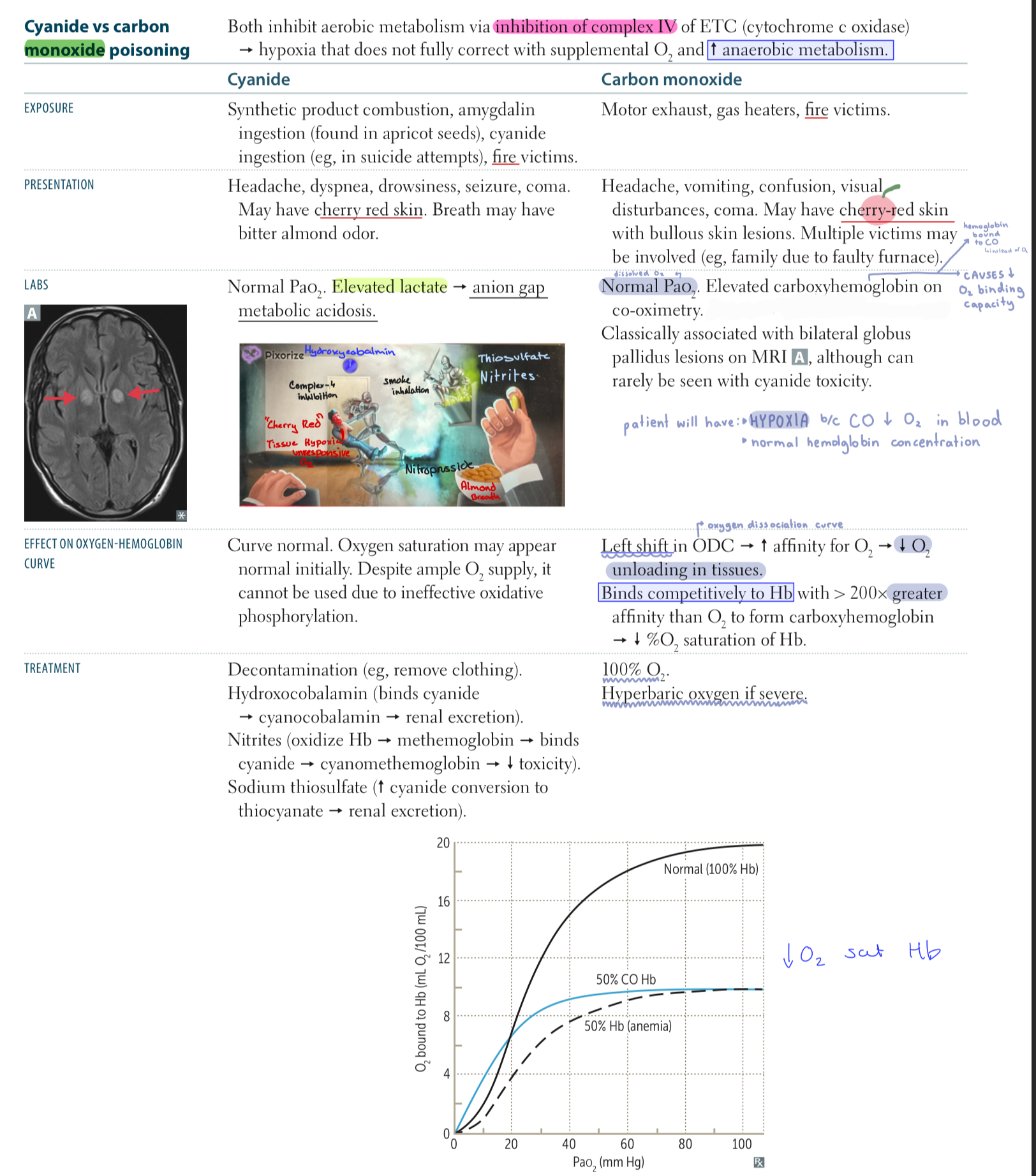
Cyanide vs CO posoning
Burn patient will have what kind of presentation ?
infection ?
LOW bp + high HR
bc increased permiability and decreased intraVascular volume
Psuedomonas ( with FEVER )
smoke inhalation will cause what kind of presentation
cause
seen in CO, Cyanide, Arsenic
.
soot in oropharynx
singed nasal hairs
Bronchoscopy = congestion, soot and edema
CAUSE = edema, pneumonia , ARDS ( endothelial damage and increased permiability )
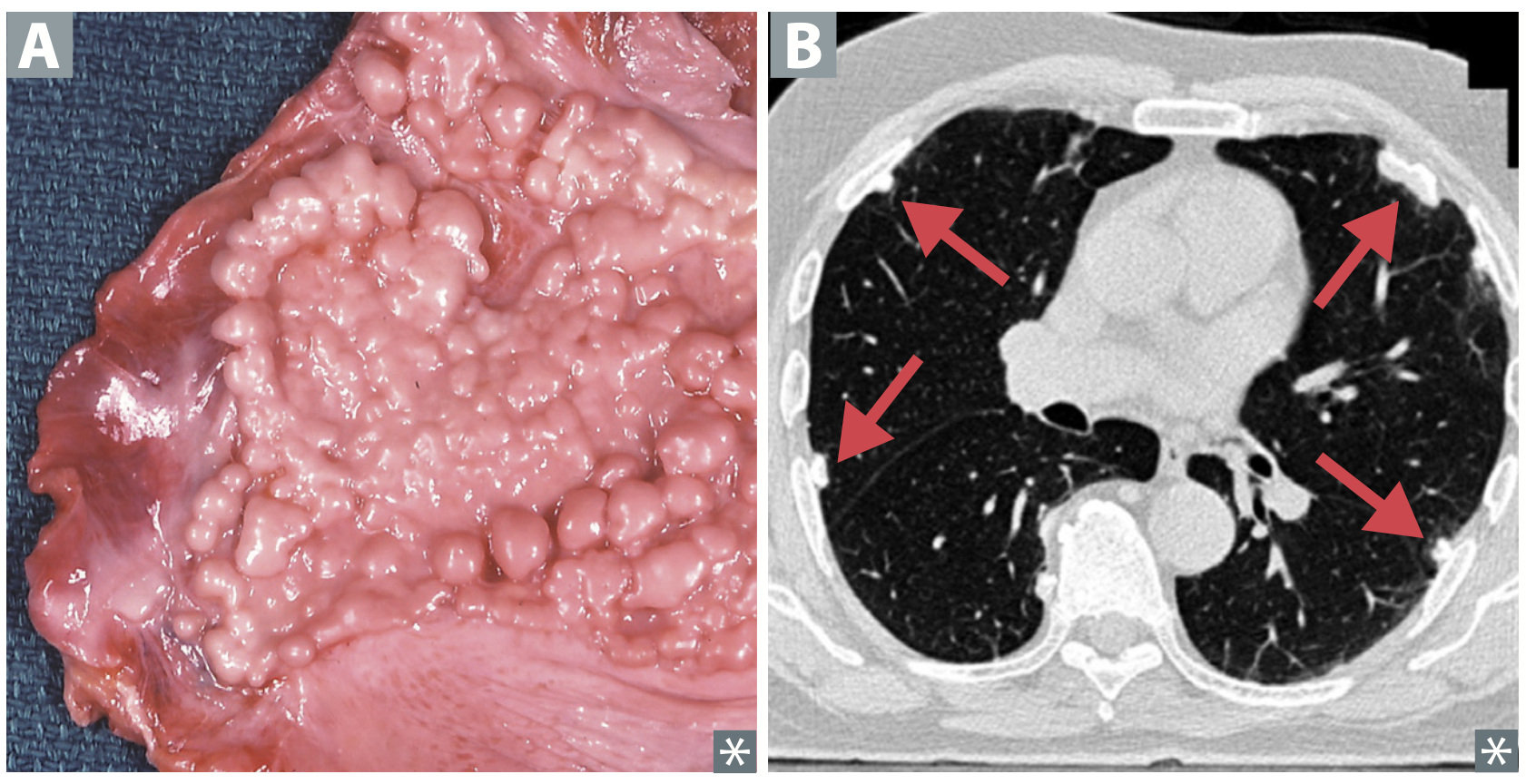
mesothelioma markers
Calretinin and cytokeratin 5/6 ⊕ in almost all
mesotheliomas
Mesothelioma is malignancy of
associated with what dissorder
how does it appear in Histology
may result in
Malignacy of pleura
asbestos predisposes
Histology may show psammoma bodies.
EM may show polygonal tumor cells with microvilli, desmosomes, tonofilamen
may cause pleural thickening and hemorraghic pleural effusion
“whitish cancer “
_____is from the roof ____, but affects the _____
______from the ____, but affect the ____
Asbestos is from the roof (was common in insulation), but affects the base (lower lobes).
Silica, coal, and berries are from the base (earth), but affect the roof (upper lobes).
Complications seen in Pneumoconioses
Cor pulmonale (right-sided HF secondary to pulmonary HTN)
Cancer
Caplan syndrome: rheumatoid arthritis and pneumoconioses with intrapulmonary nodules
Asbestosis
who
how does it present in lungs
Shipbuilding
roofing
plumbing
.
Ivory white calcified supra-diaphragmatic and pleural plaques
.
Asbestos bodies (ferruginous): golden-brown fusiform rods resembling dumbbells found in alveolar septum sputum sample
Asbestos bodies are visualized with Prussian blue stain and obtained via BAL