Section 10 - Disorders of Secondary Hemostasis - Inhibitors
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
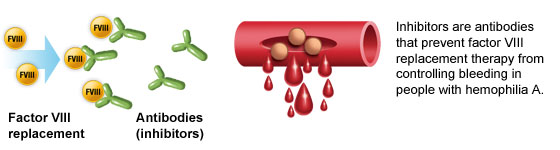
Inhibitors
Antibody directed against one or more coagulation factors
Interferes with normal coagulation
Can be specific (targeting a factor) or nonspecific (e.g. lupus anticoagulant)
True Autoantibody Inhibitors
Type: Specific inhibitors (e.g., anti-FVIII)
Mechanism: Bind and inactivate clotting factors or promote their clearance
Result:
↓ factor activity
Often leads to bleeding (acquired hemophilia if FVIII involved)
Mixing study: No correction of prolonged APTT
Associated with autoimmune disease, malignancy, pregnancy, elderly
Acquired Circulating Anticoagulants
Type: Nonspecific inhibitors
Mechanism: Interfere with phospholipid-dependent coagulation (e.g., lupus anticoagulant) or enhance natural anticoagulants (e.g., heparin → ↑ antithrombin activity)
Result:
Prolonged PT and/or APTT
Mixing study: No correction
Heparin: Prolongs TT, APTT, and often PT
Lupus anticoagulant: Prolonged APTT, but patient may clot, not bleed
Factor VIII:C Inhibitor
Mechanism
Autoantibody (usually IgG) directed against Factor VIII
Neutralizes infused or endogenous FVIII
Can occur in:
Hemophilia A patients (treatment complication)
Non-hemophiliacs ("Acquired hemophilia") due to autoimmune disorders, postpartum state, malignancy, or drugs
Factor VIII:C Inhibitor
Presentation
Bleeding usually spontaneous, soft tissue, or mucosal
Onset in previously healthy adults (50–80 years)
Mild to severe bleeding; may be fatal
No family history typically
Common triggers: SLE, RA, postpartum, drugs
Factor VIII:C Inhibitor
Laboratory Findings
APTT: Prolonged
PT: Normal
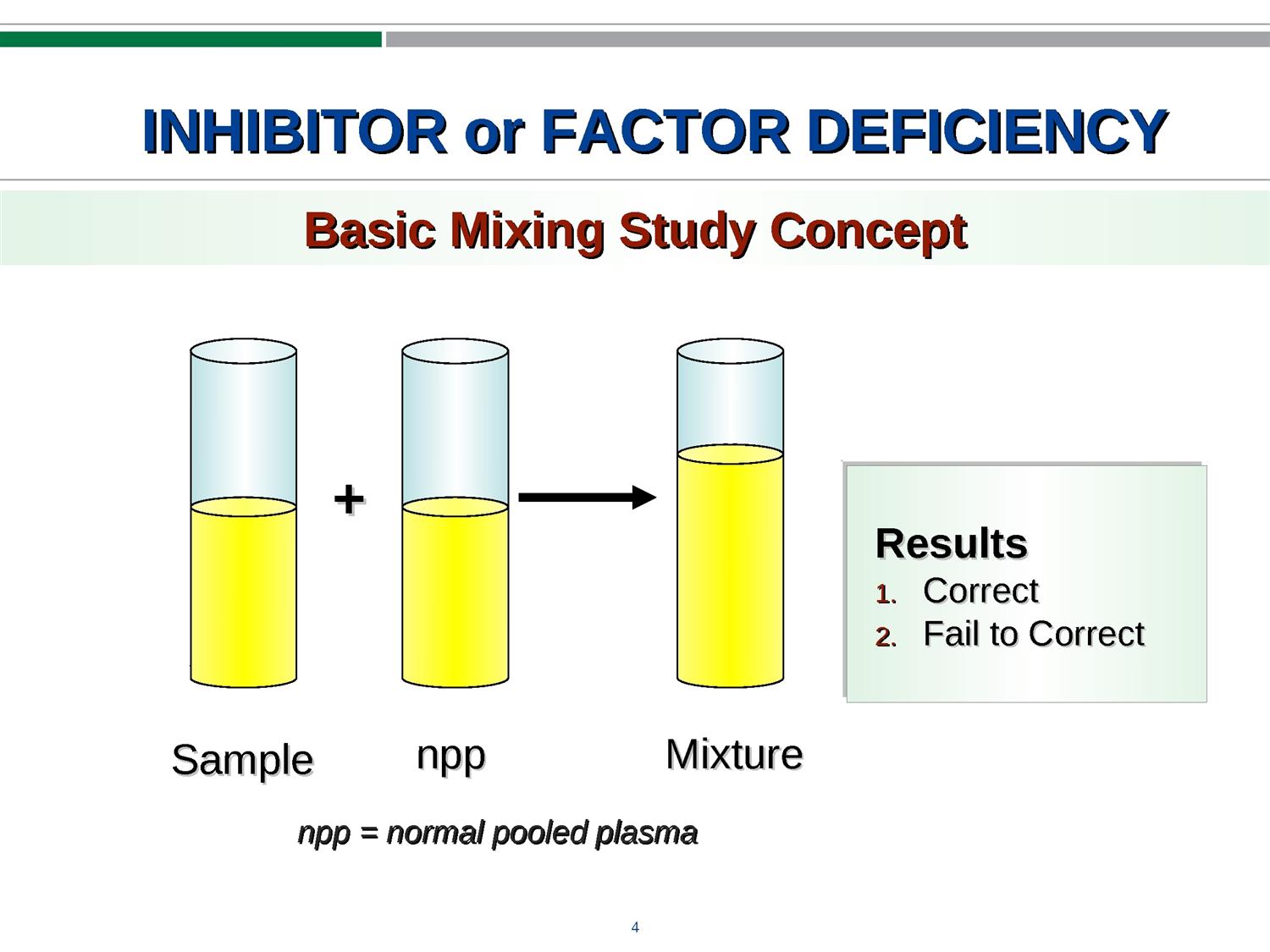
Mixing Study (50:50): Fails to correct APTT
Factor assay: Isolated low FVIII:C level
No other factor deficiencies
***This is the most important thing to remember diagnostically***
Factor VIII:C Inhibitor
Differential Diagnosis
Mixing Study Interpretation:
Corrects → Factor deficiency (e.g. Hemophilia A)
Fails to correct → Circulating inhibitor (e.g. FVIII:C inhibitor, lupus anticoagulant)
Distinction from Lupus Inhibitor: FVIII:C inhibitor causes clinical bleeding, not thrombosis
***Very importnant***
Factor VIII:C Inhibitor
Management
Depends on inhibitor titer
Bypass agents (e.g., rFVIIa, FEIBA) for bleeding
Immunosuppressive therapy (steroids, rituximab) to eradicate antibody
Rare spontaneous remission in acquired cases
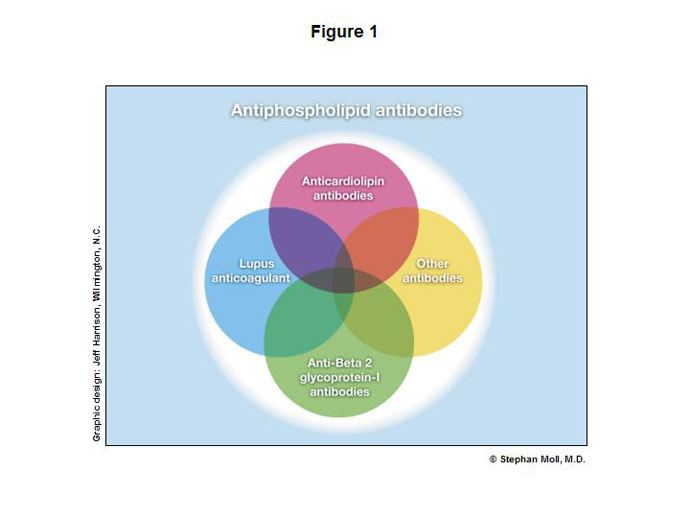
Antiphospholipid Antibodies
Definition
Group of immunoglobulins that bind protein–phospholipid complexes
Includes:
• Lupus anticoagulant (LA) or LI Lupus inhibitor
• Anticardiolipin antibodies
• Anti–β2 glycoprotein I antibodies
• Other less defined antibodies
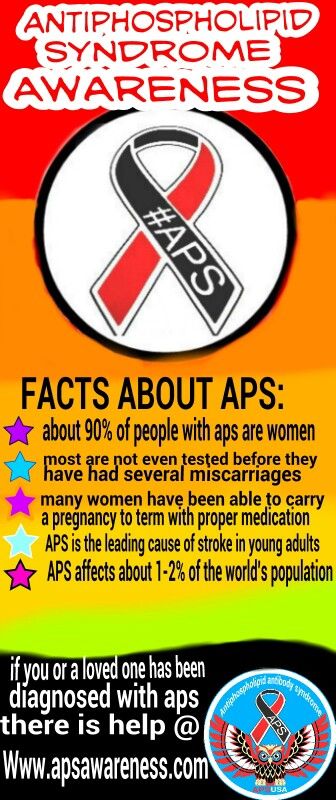
Antiphospholipid Syndrome (APS)
Clinical Presentation
Recurrent arterial or venous thrombosis
Pregnancy complications (e.g., miscarriage, preeclampsia)
Unexplained skin/circulatory changes
Thrombocytopenia
Hemolytic anemia
Nonbacterial thrombotic endocarditis
Lupus Anticoagulant (LA)
Mechanism
Not factor-specific; interferes with phospholipid-dependent coag reagents
Binds phospholipid in test systems (reagents) but not to platelets themselves
Prolongs APTT in vitro
Not associated with bleeding
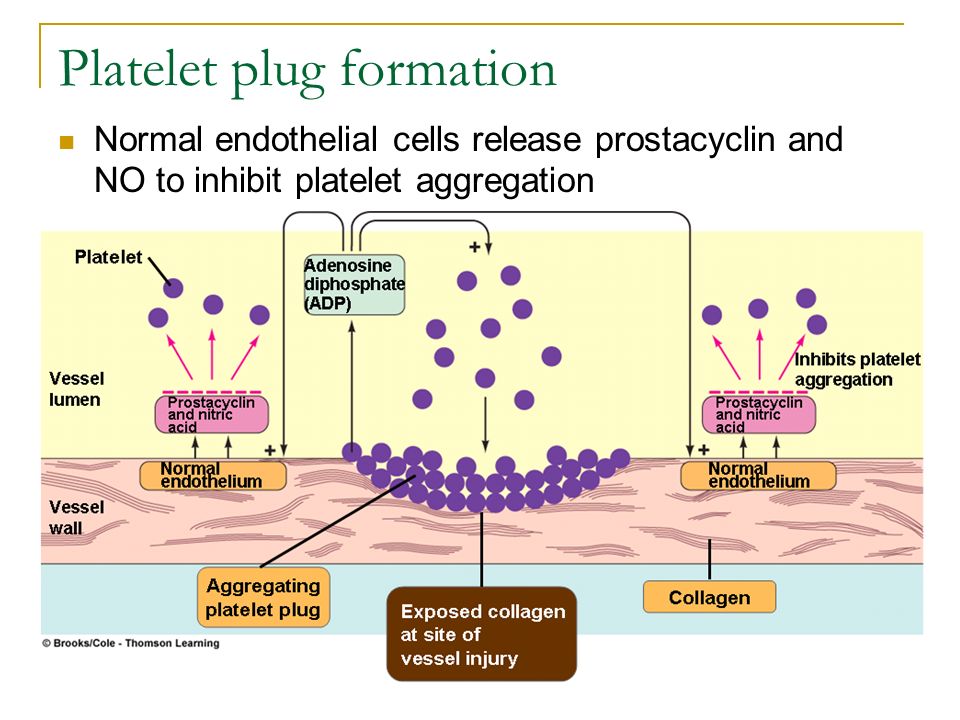
Lupus Anticoagulant (LA)
Clinical Manifestations
Prothrombotic despite “anticoagulant” name
Inhibits prostacyclin from endothelium
• Prostacyclin normally prevents platelet adhesionPlatelets are adhering at increased rates → aggregations → clotting → cascade
Increased risk of clot formation → THROMBOSIS
No bleeding tendency
Antiphospholipid Antibodies
Prevalence and Context
Present in 1–2% of healthy individuals (often transient)
• Post-infection or drug exposure5–15% of patients with recurrent thrombosis test positive
Associated with autoimmune diseases:
• SLE, RA, Sjögren’s syndrome
PT/INR and APTT in the Presence of Inhibitors
LI
APTT prolonged in most acquired inhibitors (e.g., factor VIII inhibitor, lupus anticoagulant)
PT/INR typically normal in lupus anticoagulant and factor VIII inhibitors
Both PT and APTT prolonged in inhibitors targeting common pathway or multiple factors
50:50 Mixing Study
LI
Purpose: Distinguish factor deficiency from inhibitor
Correction = factor deficiency
No correction = inhibitor present
Time-dependent inhibition may show initial correction with prolongation upon incubation (e.g., acquired factor VIII inhibitor)
Silica Clotting Time (SCT)
LI
Contact pathway-based APTT analog (uses silica as activator)
Prolonged SCT with no correction on mix = possible lupus anticoagulant
If a patients has a LI their SCT will be prolonged more than normal plasma
Often run in tandem with dRVVT in LA panels
Dilute Russell Viper Venom Time (dRVVT)
LI
Activates factor X directly (bypasses VIII and IX)
Sensitive and specific for lupus anticoagulant
Prolonged screen + correction with confirm reagent = LA present
Kaolin Clotting Time (KCT)
LI
Kaolin activates contact factors/Intrinsic Pathway
Prolonged KCT with no correction = consistent with lupus anticoagulant
Often included in LA-sensitive testing panels
Dilute Thromboplastin Time (dTT or dPTT)
LI
Test the extrinsic Pathway
Uses diluted tissue factor; sensitive to phospholipid-dependent inhibitors
Prolonged result without correction = LA
Especially useful when dRVVT is equivocal
Platelet Neutralization Procedure (PNP)
LI
Confirms lupus anticoagulant
Replaces reagent phospholipids with PL-rich platelet lysate
Shortened APTT with platelet lysate = LA confirmed
Helps distinguish LA from factor inhibitors
Only run after a prolonged DRVVT or KCT
Anti-cardiolipin Antibody (aCL)
Autoantibody against phospholipid-bound proteins
Positive IgG or IgM aCL = antiphospholipid syndrome
Does not prolong clot-based assays, but supports diagnosis
Anti-β2 Glycoprotein I Antibody
Autoantibody against β2-glycoprotein I-phospholipid complex
Confirms antiphospholipid syndrome when present
Measured by ELISA; does not interfere with clot-based testing
Can be a cause of Thrombosis
Antiphospholipid Syndrome (APS)
Mechanism
Autoantibodies against phospholipid-protein complexes (e.g., β2-glycoprotein I)
Promote thrombosis despite in vitro prolongation of clotting times
APS
Lab Findings
↑ APTT
dRVVT screen: prolonged
dRVVT confirm: corrects
50:50 mix: no correction
Anti-cardiolipin or β2GP1 Ab
APS
Clinical Features
Venous and arterial thrombosis
Recurrent miscarriage
Stroke in young adults
Often asymptomatic until thrombotic event
APS
Treatment
No treatment if asymptomatic
Steroids may reduce antibody activity
Plasmapheresis in emergencies
Antithrombotic therapy for active thrombosis